Abstract
Cervical oesophageal cancer (CEC) is a relatively uncommon malignancy. The biological behaviour and treatment have not been well studied. This retrospective study reviewed the clinicopathological features of 28 patients with CEC who underwent surgical resection to investigate the biological behaviour, treatment and prognosis of CEC. The long-term outcomes of these patients were compared with those of the CEC patients who received definitive chemoradiotherapy and those of thoracic or abdominal oesophageal cancer patients who underwent surgery. The study group contained 21 men and 7 women, ranging in age from 41 to 67 years (median: 56.5 years). The median survival time and the 1-, 3-, and 5-year overall survival rates were 25.0 months, 83.8%, 48.8%, and 41.9%, respectively. Only salvage surgery was found to affect the overall survival (P = 0.007). The long-term outcomes for CEC patients who underwent surgery were significantly better than those who received definitive chemoradiotherapy (P = 0.045) but were similar to those of thoracic or abdominal oesophageal cancer patients. In summary, CEC is an uncommon and aggressive malignancy. The malignant potential of CEC is similar to that of thoracic or abdominal oesophageal cancer. Surgical resection is an important therapeutic strategy and may be associated with better survival rates than definitive chemoradiotherapy.
Similar content being viewed by others
Introduction
Cervical oesophageal cancer (CEC) is a relatively uncommon malignancy, accounting for less than 5% of all oesophageal cancers1. Treatment options for CEC include primary resection, chemoradiotherapy (CRT), or a combination of the two2,3,4,5,6,7,8,9,10,11,12,13,14. Historically, surgery has been regarded as the standard treatment for CEC, but the overall survival is rather disappointing5. As the proximal cervical oesophagus is adjacent to the larynx, laryngectomy has often been considered to be necessary to achieve radical resection of CEC, but this procedure is not easily tolerated by patients and has a huge impact on the quality of life4, 15. Definitive CRT is now the mainstay treatment for CEC according to the National Comprehensive Cancer Network (NCCN) guidelines. However, locoregional disease persists or recurs in 40–60% of the patients who undergo CRT16, 17. Due to the low incidence of CEC, their biological behaviour and response to therapies have not been well studied.
Definitive CRT was the standard treatment for CEC patients in our hospital. However, we also performed surgical resection for patients who were willing to undergo surgery since 2001. In the current study, we retrospectively reviewed the clinical characteristics and surgical results of 28 patients with CEC who underwent surgical resection and compared their survival with that of CEC patients who received definitive CRT and that of thoracic or abdominal oesophageal cancer patients who underwent surgery.
Results
Patient characteristics
This study group contained 21 men and 7 women, ranging in age from 41 to 67 years (median: 56.5 years). The median length of the primary lesion was 4.0 cm (2.0~7.0 cm). Five patients had multiple lesions in the oesophagus, including two cases of pT1a tumour and one case of pT1b tumour in the middle third of the thoracic oesophagus; and one case of pT1b tumour and one case of pTis tumour in the lower third of the thoracic oesophagus. An R0 resection (complete tumour resection) was achieved in 26 patients (92.9%), and an R2 resection (macroscopic residual tumour) was performed in 2 patients (7.1%). Fifteen patients underwent transhiatal oesophagectomy without thoracotomy, and the other 13 patients underwent thoracoscopic surgery. A mean of 21.4 (range 2–49) lymph nodes was dissected from each specimen, and 14 patients (50%) were confirmed to have lymph node metastases. The postoperative complication rate was 21.4% (6 patients), including one case of wound infection, two cases of anastomotic leakage and three cases of pulmonary complications. No patients died during treatment in the hospital or within 30 days after surgery.
Survival and prognosis factors
The mean follow-up time of the 28 CEC patients who underwent surgical resection was 34.6 months (range, 2.0–182.0 months). During follow-up, 15 patients died, and no cases were lost to follow-up. The 1-, 3-, and 5-year overall survival (OS) rates for the entire population were 83.8%, 48.8%, and 41.9%, respectively, with a median survival time (MST) of 25.0 months (95% confidence interval (CI) 0.8–49.2 months).
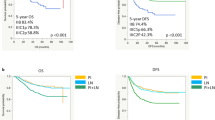
The variables related to survival in univariate analysis are shown in Table 1. Only salvage surgery was found to affect the overall survival (P = 0.007, Fig. 1). The MST and 5-year OS rate for patients who underwent salvage surgery were 15.0 months (95% CI 10.5–19.5) and 0%, respectively, which were significantly lower than those of 97.0 months (95% CI 0.1–193.9) and 54.0%, respectively, for patients who underwent non-salvage surgery. Gender, age, tumour length, tumour cell differentiation, pT category, pN category, pTNM stage, and surgical procedure did not show statistically significant differences in survival (P > 0.05). In multivariate analysis, none of these factors were found to be independent factors (P > 0.05).
Comparison of the survival curves for patients with cervical oesophageal cancer who underwent salvage surgery and non-salvage surgery. The MST and 5-year OS rate for patients who underwent salvage surgery were 15.0 months (95% CI 10.5–19.5) and 0%, respectively, which were significantly lower than those of 97.0 months (95% CI 0.1–193.9) and 54.0%, respectively, for patients who underwent non-salvage surgery (P = 0.007).
Comparison of outcomes based on treatment
The definitive CRT group of patients with CEC included 278 men and 82 women, ranging in age from 36 to 79 years (median: 55.0 years). A total dose of 50–70 Gy (median 60 Gy) was delivered at a daily dose of 1.8 to 2 Gy. Concurrent chemotherapy with cisplatin plus 5-fluorouracil or docetaxel was repeated every 3 weeks for 2 to 4 cycles. The median length of the primary lesion was 4.0 cm (1.5~8.0 cm). According to the sixth edition of the American Joint Committee on Cancer (AJCC) staging system for oesophageal cancer, this cohortincluded 15 cases of clinical TNM (cTNM) stage I, 102 cases of cTNM stage II, and 243 cTNM stage III. No significant differences in clinicopathological features were found when compared with those of the surgery group (P > 0.05).
The MST and the1-, 3-, and 5-year OS rates for the definitive CRT group were 19.0 months (95% CI 16.6–21.4 months), 67.4%, 32.5%, and 21.0%, respectively. The long-term outcomes for CEC patients who received definitive CRT were significantly worse than those who underwent surgery (P = 0.045, Fig. 2).
Comparisons of the survival curves for patients with cervical oesophageal cancer who received surgery and definitive chemoradiotherapy. The MST and the1-, 3-, and 5-year OS rates for patients who underwent surgery were 25.0 months (95% confidence interval (CI) 0.8–49.2 months), 83.8%, 48.8%, and 41.9%, respectively, which were significantly better compared with those of 19.0 months (95% CI 16.6–21.4 months), 67.4%, 32.5%, and 21.0%, respectively, for patients who received definitive chemoradiotherapy (P = 0.045).
Comparison of outcomes based on tumour location
The clinicopathological features of the 3,950 patients with thoracic or abdominal oesophageal cancer who underwent surgical resection are shown in Table 2. All factors were similar to those of the patients with CEC, except for preoperative therapy. More patients with CEC underwent preoperative chemoradiotherapy. The MST and the 1-, 3-, and 5-year OS rates were 49.0 months (95% CI 43.9–54.1 months), 84.3%, 56.2%, and 46.4%, respectively. No significant differences were observed in the long-term outcomes between the CEC patients and the thoracic or abdominal oesophageal cancer patients (P = 0.429, Fig. 3). We further compared the long-term outcomes between the CEC patients and the thoracic or abdominal oesophageal cancer patients who did not receive preoperative therapy. The MST and the 1-, 3-, and 5-year OS rates for CEC patients were 97.0 months (95% CI 10.0–184.0 months), 93.8%, 63.9%, and 53.3%, respectively, compared with those of 50.0 months (95% CI 44.1–55.9 months), 84.3%, 56.5%, and 46.8%, respectively, for patients with thoracic or abdominal oesophageal cancer. The survival difference was not significant between these two groups (P = 0.748, Fig. 4).
Comparisons of the survival curves for patients with cervical oesophageal cancer and patients with thoracic or abdominal oesophageal cancer who underwent surgery. The median survival time (MST) and the1-, 3-, and 5-year OS rates for CEC patients were 25.0 months (95% confidence interval (CI) 0.8–49.2 months), 83.8%, 48.8%, and 41.9%, respectively, compared with those of 49.0 months (95% CI 43.9–54.1 months), 84.3%, 56.2%, and 46.4% for patients with thoracic or abdominal oesophageal cancer. The survival differences were not statistically significant (P = 0.429).
Comparisons of the survival curves for patients with cervical oesophageal cancer and patients with thoracic or abdominal oesophageal cancer who did not receive preoperative therapy. The MST and the1-, 3-, and 5-year OS rates for CEC patients were 97.0 months (95% CI 10.0–184.0 months), 93.8%, 63.9%, and 53.3%, respectively, compared with those of 50.0 months (95% CI 44.1–55.9 months), 84.3%, 56.5%, and 46.8% for patients with thoracic or abdominal oesophageal cancer. The survival differences were not significant (P = 0.748).
Discussion
Oesophageal cancer is one of the most aggressive malignancies, and it usually occurs in the thoracic oesophagus. CEC is a very rare disease and is often locally advanced at the time of diagnosis, resulting in limited locoregional disease control and poor survival14. Due to the low incidence of this disease, the biological characteristics, treatment, and prognosis were not well studied.
In the current study, we retrospectively analysed the clinicopathological characteristics and outcomes of 28 patients with CEC who underwent pharyngo-laryngo-esophagectomy (PLE) and compared their prognosis with that of the patients with CEC who received definitive CRT and the patients with thoracic or abdominal oesophageal cancer who underwent surgical resection. To our knowledge, few studies have evaluated the outcomes of CEC patients treated with definitive CRT and surgery and even fewer studies have compared the prognosis between patients with CEC and patients with thoracic oesophageal cancer. Only one study by Saeki et al.4 evaluated the malignant potential between CEC and thoracic oesophageal cancers and found that CEC was not more aggressive. Our study also confirmed that the long-term outcomes were similar between the patients with CEC and patients with thoracic or abdominal oesophageal cancer who underwent surgery. We think that more studies are needed to elucidate the biological characteristics of this cancer.
Historically, surgery has been the standard treatment for CEC. Generally, a PLE is carried out, which includes the resection of the larynx and is considered to have a great risk of major complications as well as a huge impact on quality of life18. Nonetheless, novel surgical strategies and improved perioperative management of oesophageal surgery have been developed during the last decades, such as minimally invasive surgery, which might decrease the operative morbidity and mortality. In this study, only 6 patients (21.4%) developed postoperative complications, and no patients died during treatment in the hospital. We think that more careful preoperative evaluation, postoperative critical care, and nutritional support are important in reducing complications in these patients.
Less invasive surgeries such as pharyngo-laryngo-cervical oesophagectomy (PLCE) and larynx-preserving surgery were also performed in patients with CEC in recent years4, 19. These types of surgery might achieve functional preservation and improve the quality of life. However, a previous study showed that oesophageal cancer might be a multicentric disease, with a heightened risk of synchronous or metachronous lesions ranging from 12% to 30%20, 21. We also found that 17.9% (5/28) of patients had multiple lesions in the thoracic oesophagus in this study, and all of them were pTis or pT1 diseases. The thoracic lesions in two cases were even misdiagnosed in the preoperative examination, as the endoscopy could not be passed across the malignant strictures into the distal oesophagus. This would, therefore, cast serious doubt on the advisability of performing segmental oesophageal resection.
Most of the previous studies have reported disappointing outcomes for patients with CEC due to a delayed diagnosis and the poor performance status of many patients14. Definitive CRT is now recommended for CEC to preserve functional upper respiratory and alimentary tracts. However, the reported 5-year overall survival rates ranged only from 18.6% to 37.9%12, 13, 22,23,24. In our study groups, the 5-year OS rate was 21.0% for patients who received definitive CRT, which was similar to that reported in previous studies. Although surgical resection is a more aggressive strategy and has a huge impact on the quality of life, it may provide the best chance of curing oesophageal cancer25.
The reported 5-year overall survival rates ranged from 24% to 47.0% for patients with CEC who underwent surgical resection2, 8, 26,27,28,29,30,31. In the current study, the 5-year OS rate was 41.9% for patients who underwent surgical resection. We also found that the long-term outcomes for patients with CEC who underwent surgery were significantly better than those who received definitive CRT. Due to the low number of these studies, more data are needed to confirm our findings. Moreover, neoadjuvant CRT has been increasingly used for the treatment of oesophageal cancer patients, and it has shown a significant survival benefit32. We think that further research should be conducted to establish the value of this new therapeutic approach for patients with CEC.
In conclusion, CEC is an uncommon and aggressive malignancy. The malignant potential of CEC is similar to that of thoracic or abdominal oesophageal cancer. Surgical resection is an important therapeutic strategy and may be associated with better survival rates than definitive CRT. As randomized controlled trials for this rare disease are currently impractical, we think that a prospective, multinational database to track these cases will enable a better investigation of the biological behaviour, treatment and prognosis of this disease.
Materials and Methods
Patient population
This study was undertaken at the Cancer Hospital of Shantou University Medical College and was approved by the Ethics Committee of that hospital. All methods were carried out in accordance with the approved guideline, and written informed consent from the patients or their family was not deemed necessary for this kind of retrospective study by the Cancer Hospital of Shantou University Medical College.
A total of 3,978 patients with oesophageal carcinoma underwent surgical resection between January 2001 and September 2016, including 28 patients with CEC and 3,950 patients with thoracic or abdominal oesophageal cancer. Three hundred and sixty CEC patients without distant metastasis received definitive CRT in the same period. In this study, CEC was defined as a tumour with its centre located between the oesophageal orifice and the sternal notch. Patients with CEC who had concurrent tumours in other segments of the oesophagus were also included in our study.
Medical history was obtained from all patients, and then, they underwent a physical examination. A chest radiograph, Doppler ultrasound examination of the neck; barium meal; contrast-enhanced computed tomography scan of the neck, chest and upper abdomen; oesophagoscopic biopsy; complete blood count; blood biochemistry analyses; and liver and renal function evaluations were also performed. Tumours were staged according to the sixth edition of the American Joint Committee on Cancer (AJCC) staging system for oesophageal cancer.
Surgical procedure
All patients underwent a total PLE. A transhiatal oesophagectomy without thoracotomy was performed before 2010, while thoracoscopic surgery was used for the thoracic procedures after 2011. Pharyngo-laryngectomy and cervical lymphadenectomy were performed by head and neck surgeons, while thoracoscopic surgery and laparotomy or laparoscopic surgery were conducted by the thoracic surgeons. The reconstruction was simultaneously performed by thoracic surgeons. A gastric tube, which was principally elevated through the posterior mediastinal route, was used for oesophageal reconstruction. In all patients, standard abdominal lymphadenectomy and selective cervical lymphadenectomy were performed. Mediastinal lymphadenectomy was performed for one patient who underwent a thoracoscopic surgery.
Preoperative therapy
Of the 28 patients with CEC who underwent surgical resection, only 2 patients received scheduled neoadjuvant radiotherapy of a total dose of 40 Gy and underwent oesophagectomy 4 weeks after the radiotherapy. Radiotherapy was delivered using an MV linear accelerator in 2 Gy fractions 5 days a week. Another 8 patients received definitive CRT and underwent salvage surgery after the recurrence of the tumour. A total dose of 60–68 Gy (median 60 Gy) was delivered. Chemotherapy with cisplatin plus 5-fluorouracil was repeated every 3 weeks for 2 to 4 cycles. The time from the termination of CRT to failure was 5 months to 7 years (median, 7 months).
Postoperative therapy
None of the 10 patients who received preoperative therapy underwent postoperative chemotherapy or radiotherapy. For the other 18 patients who chose surgery as their primary treatment, six of them received adjuvant radiotherapy with a total dose of 50 Gy.
Follow-up
Patients were followed with a clinical examination every 3 months for the first year, every 6 months for the second year and every 6 to 12 months thereafter. During each follow-up visit, the patients received a clinical evaluation, blood biochemistry examination, ultrasonography exam, and X-ray examination. Computed tomography was performed every 6 months. Endoscopic examinations were performed when necessary. Follow-up was continued up to November 2016 or until death, whichever occurred earlier.
Statistical analysis
Statistical analyses were performed using the SPSS 18.0 software (SPSS Inc., Chicago, IL, USA). Clinicopathological data between different groups were statistically compared by means of the χ2 test or Fisher’s exact test. Univariate analysis of survival was performed using the Kaplan-Meier method to estimate the survival probabilities, and the log-rank test was used for statistical comparisons. Multivariate analysis was performed to investigate prognostic factors for CEC patients using the Cox proportional hazard regression model with the entry factors of gender, age (≤60 years versus > 60 years), tumour length (≤4 cm versus > 4 cm), tumour cell differentiation, pT category, pN category, pTNM stage, surgical procedure and salvage surgery. All statistical tests performed were two-sided, and a P-value less than 0.05 was considered to be statistically significant.
References
Mendenhall, W. M. et al. Management of cervical esophageal carcinoma. Semin Radiat Oncol. 4, 179–191, doi:10.1053/SRAO00400179 (1994).
Triboulet, J. P., Mariette, C., Chevalier, D. & Amrouni, H. Surgical management of carcinoma of the hypopharynx and cervical esophagus: analysis of 209 cases. Arch Surg. 136, 1164–1170, doi:10.1001/archsurg.136.10.1164 (2001).
Nishimaki, T. et al. Outcomes and prognostic factors after surgical resection of hypopharyngeal and cervical esophageal carcinomas. Int Surg 87, 38–44 (2002).
Saeki, H. et al. Clinicopathological features of cervical esophageal cancer: retrospective analysis of 63 consecutive patients who underwent surgical resection. Ann Surg. 265, 130–136, doi:10.1097/SLA.0000000000001599 (2017).
Tong, D. K. et al. Current management of cervical esophageal cancer. World J Surg. 35, 600–607, doi:10.1007/s00268-010-0876-7 (2011).
Zhang, P. et al. Clinical efficacy and failure pattern in patients with cervical esophageal cancer treated with definitive chemoradiotherapy. Radiother Oncol. 116, 257–261, doi:10.1016/j.radonc.2015.07.011 (2015).
Cao, C. et al. Definitive radiotherapy for cervical esophageal cancer. Head Neck. 37, 151–155, doi:10.1002/hed.23572 (2015).
Cao, C. N. et al. Intensity-modulated radiotherapy for cervical esophageal squamous cell carcinoma: clinical outcomes and patterns of failure. Eur Arch Otorhinolaryngol. 273, 741–747, doi:10.1007/s00405-015-3576-y (2016).
Chou, S. H. et al. Radical resection or chemoradiotherapy for cervical esophageal cancer? World J Surg. 34, 1832–1839, doi:10.1007/s00268-010-0595-0 (2010).
Cao, C. N. et al. Primary radiotherapy compared with primary surgery in cervical esophageal cancer. JAMA Otolaryngol Head Neck Surg. 140, 918–926, doi:10.1001/jamaoto.2014.2013 (2014).
Suzuki, G. et al. Multimodal approach for cervical esophageal carcinoma: role of neoadjuvant chemotherapy. Anticancer Res. 34, 1989–1992 (2014).
Huang, S. H. et al. Effect of concurrent high-dose cisplatin chemotherapy and conformal radiotherapy on cervical esophageal cancer survival. Int J Radiat Oncol Biol Phys. 71, 735–740, doi:10.1016/j.ijrobp.2007.10.022 (2008).
Wang, S. et al. Esophageal cancer located at the neck and upper thorax treated with concurrent chemoradiation: a single-institution experience. J Thorac Oncol. 1, 252–259, doi:10.1016/S1556-0864(15)31576-8 (2006).
Hoeben, A. et al. Cervical esophageal cancer: a gap in cancer knowledge. Ann Oncol. 27, 1664–1674, doi:10.1093/annonc/mdw183 (2016).
Takebayashi, K. et al. Comparison of curative surgery and definitive chemoradiotherapy as initial treatment for patients with cervical esophageal cancer. Dis Esophagus. 30, 1–5, doi:10.1111/dote.12502 (2017).
Nakahara, R. et al. Treatment outcomes of definitive chemoradiotherapy for patients with hypopharyngeal cancer. J Radiat Res. 53, 906–915, doi:10.1093/jrr/rrs052 (2012).
Cooper, J. S. et al. Chemoradiotherapy of locally advanced esophageal cancer: long-term follow-up of a prospective randomized trial (RTOG 85-01). Radiation Therapy Oncology Group. JAMA. 281, 1623–1627, doi:10.1001/jama.281.17.1623 (1999).
Archibald, S., Young, J. E. & Thoma, A. Pharyngo-cervical esophageal reconstruction. Clin Plast Surg. 32, 339–346, vi, doi:10.1016/j.cps.2005.01.002 (2005).
Makino, T. et al. Short- and Long-Term Outcomes of Larynx-Preserving Surgery for Cervical Esophageal Cancer: Analysis of 100 Consecutive Cases. Ann Surg Oncol. 23, 858–865, doi:10.1245/s10434-016-5511-x (2016).
Mariette, C. et al. Oesophageal cancer in patients with head and neck cancers: therapeutic implications. Ann Chir. 127, 757–764 (2002).
Law, S. Y. et al. Thoracoscopic esophageal mobilization for pharyngolaryngoesophagectomy. Ann Thorac Surg. 70, 418–422 (2000).
Gkika, E. et al. Long-term results of definitive radiochemotherapy in locally advanced cancers of the cervical esophagus. Dis Esophagus. 27, 678–684, doi:10.1111/dote.12146 (2014).
Grass, G. D., Cooper, S. L., Armeson, K., Garrett-Mayer, E. & Sharma, A. Cervical esophageal cancer: a population-based study. Head Neck. 37, 808–814, doi:10.1002/hed.23678 (2015).
Yamada, K. et al. Treatment results of radiotherapy for carcinoma of the cervical esophagus. Acta Oncol. 45, 1120–1125, doi:10.1080/02841860600609768 (2006).
Lin, J., Akhter, S. A. & Iannettoni, M. D. Carcinoma of the esophagus In General Thoracic Surgery. 6th ed (eds Shields, T. W.) 2265–2298 (Lippincott Williams & Wilkins, 2005).
Kadota, H. et al. Larynx-preserving esophagectomy and jejuna transfer for cervical esophageal carcinoma. Laryngoscope. 119, 1274–1280, doi:10.1002/lary.20493 (2009).
Miyata, H. et al. Larynx-preserving limited resection and free jejunal graft for carcinoma of the cervical esophagus. World J Surg. 37, 551–557, doi:10.1007/s00268-012-1875-7 (2013).
Sun, F. et al. Surgical management of cervical esophageal carcinoma with larynx preservation and reconstruction. Int J Clin Exp Med. 7, 2771–2778, eCollection 2014 (2014).
Ott, K. et al. Limited resection and free jejunal graft interposition for squamous cell carcinoma of the cervical oesophagus. Br J Surg. 96, 258–266, doi:10.1002/bjs.6437 (2009).
Daiko, H. et al. Surgical management of carcinoma of the cervical esophagus. J Surg Oncol. 96, 166–172, doi:10.1002/jso.20795 (2007).
Jiang, M. et al. Reconstruction techniques for hypopharyngeal and cervical esophageal carcinoma. J Thorac Dis. 7, 449–454, doi:10.3978/j.issn.2072-1439.2015.02.12 (2015).
van Hagen, P. et al. Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med. 366, 2074–2084, doi:10.1056/NEJMoa1112088 (2012).
Acknowledgements
We thank Prof. Hao Zhang for his insightful comments on a previous version of this article.
Author information
Authors and Affiliations
Contributions
Chen S.B., Weng H.R. and Yang X.H. contributed equally to this work; Chen Y.P. designed the research; Chen S.B., Weng H.R., Yang X.H., Liu D.T., Li H. and Chen Y.P. performed the operation; Chen S.B., Weng H.R. and Yang X.H. analyzed the data and wrote the paper. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, Sb., Yang, Xh., Weng, Hr. et al. Clinicopathological features and surgical treatment of cervical oesophageal cancer. Sci Rep 7, 3272 (2017). https://doi.org/10.1038/s41598-017-03593-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-03593-0
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.