Abstract
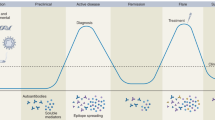
Systemic lupus erythematosus (SLE) is an autoimmune disease that has diverse clinical manifestations, ranging from restricted cutaneous involvement to life-threatening systemic organ involvement. The heterogeneity of pathomechanisms that lead to SLE contributes to between-patient variation in clinical phenotype and treatment response. Ongoing efforts to dissect cellular and molecular heterogeneity in SLE could facilitate the future development of stratified treatment recommendations and precision medicine, which is a considerable challenge for SLE. In particular, some genes involved in the clinical heterogeneity of SLE and some phenotype-related loci (STAT4, IRF5, PDGF genes, HAS2, ITGAM and SLC5A11) have an association with clinical features of the disease. An important part is also played by epigenetic varation (in DNA methylation, histone modifications and microRNAs) that influences gene expression and affects cell function without modifying the genome sequence. Immune profiling can help to identify an individual’s specific response to a therapy and can potentially predict outcomes, using techniques such as flow cytometry, mass cytometry, transcriptomics, microarray analysis and single-cell RNA sequencing. Furthermore, the identification of novel serum and urinary biomarkers would enable the stratification of patients according to predictions of long-term outcomes and assessments of potential response to therapy.
Key points
-
Systemic lupus erythematosus (SLE) has heterogeneous clinical presentation, disease course and treatment response.
-
Several new treatments targeting various pathways have gained approval or are under investigation, and a precision-medicine approach to treatment choice is needed.
-
Precision medicine is an emerging approach for disease treatment and prevention that uses individual variability (genomic, transcriptomic, proteomic and metabolomic) to identify patient subgroups that can benefit from specific treatments.
-
Disease-relevant immune subsets identified by immune profiling (helped by recent technological advances) are now shedding light on the cellular and molecular basis of clinical symptoms in individual patients with SLE.
-
Peripheral blood immunophenotyping is identifying molecular networks associated with disease activity, subtype and future relapse, which might provide biomarkers to facilitate the development of stratified treatment recommendations and SLE precision medicine.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Lisnevskaia, L., Murphy, G. & Isenberg, D. A. Systemic lupus erythematosus. Lancet 384, 1878–1888 (2014).
Morand, E. F. et al. Trial of anifrolumab in active systemic lupus erythematosus. N. Engl. J. Med. 382, 211–221 (2020).
Arriens, C. et al. AURORA phase 3 study demonstrates voclosporin statistical superiority over standard of care in lupus nephritis (LN). Ann. Rheum. Dis. 79, 172–173 (2020).
Fanouriakis, A. et al. 2019 update of the EULAR recommendations for the management of systemic lupus erythematosus. Ann. Rheum. Dis. 78, 736–745 (2019).
Van Vollenhoven, R. F. et al. 2021 DORIS definition of remission in SLE: final recommendations from an international task force. Lupus Sci. Med. 8, e000538 (2021).
Lorenzo-Vizcaya, A. & Isenberg, D. A. Clinical trials in systemic lupus erythematosus – the dilemma. Why have phase III trials failed to confirm the promising results of phase II trials. Ann. Rheum. Dis. 82, 169–174 (2023).
Pitzalis, C., Choy, E. H. S. & Buch, M. H. Transforming clinical trials in rheumatology: towards patient-centric precision medicine. Nat. Rev. Rheumatol. 16, 590–599 (2020).
Furie, R. A. et al. Type I interferon inhibitor anifrolumab in active systemic lupus erythematosus (TULIP-1): a randomised, controlled, phase 3 trial. Lancet Rheumatol. 1, 11 (2019).
Postal, M. et al. Type I interferon in the pathogenesis of systemic lupus erythematosus. Curr. Opin. Immunol. 67, 87–94 (2020).
Weckerle, C. E. et al. Network analysis of associations between serum interferon-α activity, autoantibodies, and clinical features in systemic lupus erythematosus. Arthritis Rheum. 63, 1044–1053 (2011).
Baechler, E. C. et al. Interferon-inducible gene expression signature in peripheral blood cells of patients with severe lupus. Proc. Natl Acad. Sci. USA 100, 2610–2615 (2003).
Crow, M. K., Kirou, K. A. & Wohlgemuth, J. Microarray analysis of interferon-regulated genes in SLE. Autoimmunity 36, 481–490 (2003).
Isenberg, D. et al. Efficacy and safety of atacicept for prevention of flares in patients with moderate-to-severe systemic lupus erythematosus (SLE): 52-week data (APRIL-SLE randomised trial). Ann. Rheum. Dis. 74, 2006–2015 (2015).
Merrill, J. T. et al. Efficacy and safety of atacicept in patients with systemic lupus erythematosus: results of a twenty-four-week, multicenter, randomized, double-blind, placebo-controlled, parallel-arm, phase IIb study. Arthritis Rheumatol. 70, 266–276 (2018).
Gordon, C. et al. Post hoc analysis of the phase II/III APRIL-SLE study: association between response to atacicept and serum biomarkers including BLyS and APRIL. Arthritis Rheumatol. 69, 122–130 (2017).
Morand, E. F. et al. Attainment of treat-to-target endpoints in SLE patients with high disease activity in the atacicept phase 2b ADDRESS II study. Rheumatology 59, 2930–2938 (2020).
Wallace, D. J. et al. Safety and clinical activity of atacicept in the long-term extension of the phase 2b ADDRESS II study in systemic lupus erythematosus. Rheumatology 60, 5379–5389 (2021).
Furie, R. A. et al. Cell depletion with obinutuzumab for the treatment of proliferative lupus nephritis: a randomised, double-blind, placebo-controlled trial. Ann. Rheum. Dis. 81, 100–107 (2022).
Rovin, B. H. et al. Efficacy and safety of rituximab in patients with active proliferative lupus nephritis: the lupus nephritis assessment with rituximab (LUNAR) study. Arthritis Rheum. 64, 1215–1226 (2012).
Reddy, V. et al. Obinutuzumab induces superior B-cell cytotoxicity to rituximab in rheumatoid arthritis and systemic lupus erythematosus patient samples. Rheumatology 56, 1227–1237 (2017).
Rivas-Larrauri, F. & Yamazaki-Nakashimada, M. A. Systemic lupus erythematosus: is it one disease? Reumatol. Clin. 12, 274–281 (2016).
Delgado-Vega, A. et al. Recent findings on genetics of systemic autoimmune diseases. Curr. Opin. Immunol. 22, 698–705 (2011).
Alarcon-Segovia, D. et al. Familial aggregation of systemic lupus erythematosus, rheumatoid arthritis, and other autoimmune diseases in 1,177 lupus patients from the GLADEL cohort. Arthritis Rheum. 52, 1138–1147 (2005).
International Consortium for Systemic Lupus Erythematosus Genetics (SLEGEN). Genome-wide association scan in women with systemic lupus erythematosus identifies susceptibility variants in ITGAM, PXK, KIAA1542 and other loci. Nat. Genet. 40, 204–210 (2008).
Hom, G. et al. Association of systemic lupus erythematosus with C8orf13-BLK and ITGAM-ITGAX. N. Engl. J. Med. 358, 900–909 (2008).
Buniello, A. et al. The NHGRI-EBI GWAS Catalog of published genome-wide association studies, targeted arrays and summary statistics 2019. Nucleic Acids Res. 47, D1005–D1012 (2019).
Deng, Y. & Tsao, B. P. Advances in lupus genetics and epigenetics. Curr. Opin. Rheumatol. 26, 482–492 (2014).
Kamitaki, N. et al. Complement genes contribute sex-biased vulnerability in diverse disorders. Nature 582, 577–581 (2020).
Manolio, T. A. Bringing genome-wide association findings into clinical use. Nat. Rev. Genet. 14, 549–558 (2013).
Brown, G. J. et al. TLR7 gain-of-function genetic variation causes human lupus. Nature 605, 349–356 (2022).
Brierley, M. M. & Fish, E. N. IFN-alpha/beta receptor interactions to biologic outcomes: understanding the circuitry. J. Interferon Cytokine Res. 22, 835–845 (2022).
Taylor, K. E. et al. Specificity of the STAT4 genetic association for severe disease manifestations of systemic lupus erythematosus. PLoS Genet. 4, e1000084 (2008).
Sigurdsson, S. et al. A risk haplotype of STAT4 for systemic lupus erythematosus is over-expressed, correlates with anti-dsDNA and shows additive effects with two risk alleles of IRF5. Hum. Mol. Genet. 17, 2868–2876 (2008).
Svenungsson, E. et al. A STAT4 risk allele is associated with ischaemic cerebrovascular events and anti-phospholipid antibodies in systemic lupus erythematosus. Ann. Rheum. Dis. 69, 834–840 (2010).
Restivo, V. et al. Systematic review and meta-analysis of cardiovascular risk in rheumatological disease: symptomatic and non-symptomatic events in rheumatoid arthritis and systemic lupus erythematosus. Autoimmun. Rev. 21, 102925 (2022).
Barnes, B., Lubyova, B. & Pitha, P. M. On the role of IRF in host defense. J. Interferon Cytokine Res. 22, 59–71 (2022).
Feng, D. et al. Irf5-deficient mice are protected from pristane-induced lupus via increased Th2 cytokines and altered IgG class switching. Eur. J. Immunol. 42, 1477–1487 (2012).
Song, S. et al. Inhibition of IRF5 hyperactivation protects from lupus onset and severity. J. Clin. Invest. 130, 6700–6717 (2020).
Watkins, A. A. et al. IRF5 deficiency ameliorates lupus but promotes atherosclerosis and metabolic dysfunction in a mouse model of lupus-associated atherosclerosis. J. Immunol. 194, 1467–1479 (2015).
Ostendorf, T., Eitner, F. & Floege, J. The PDGF family in renal fibrosis. Pediatr. Nephrol. 27, 1041–1050 (2011).
Chung, S. A. et al. International Consortium for Systemic Lupus Erythematosus Genetics. Lupus nephritis susceptibility loci in women with systemic lupus erythematosus. J. Am. Soc. Nephrol. 25, 2859–2870 (2014).
Kurogi, Y. Mesangial cell proliferation inhibitors for the treatment of proliferative glomerular disease. Med. Res. Rev. 23, 15–31 (2003).
Zoja, C. et al. Imatinib ameliorates renal disease and survival in murine lupus autoimmune disease. Kidney Int. 70, 97–103 (2006).
Feusi, E. et al. Enhanced hyaluronan synthesis in the MRL-Fas(lpr) kidney: role of cytokines. Nephron 83, 66–73 (1999).
Fagerholm, S. C. et al. The CD11b-integrin (ITGAM) and systemic lupus erythematosus. Lupus 22, 657–663 (2013).
Järvinen, T. M. et al. Polymorphisms of the ITGAM gene confer higher risk of discoid cutaneous than of systemic lupus erythematosus. PLoS ONE 5, e14212 (2010).
Kim-Howard, X. et al. ITGAM coding variant (rs1143679) influences the risk of renal disease, discoid rash and immunological manifestations in patients with systemic lupus erythematosus with European ancestry. Ann. Rheum. Dis. 69, 1329–1332 (2010).
Taylor, K. E. et al. Risk alleles for systemic lupus erythematosus in a large case-control collection and associations with clinical subphenotypes. PLoS Genet. 7, e1001311 (2011).
Chung, S. A. et al. Differential genetic associations for systemic lupus erythematosus based on anti-dsDNA autoantibody production. PLoS Genet. 7, e1001323 (2011).
Ho, R. C. et al. Genetic variants that are associated with neuropsychiatric systemic lupus erythematosus. J. Rheumatol. 43, 541–551 (2016).
Tsai, L. J. et al. The sodium-dependent glucose cotransporter SLC5A11 as an autoimmune modifier gene in SLE. Tissue Antigens 71, 14–26 (2008).
Zan, H. Epigenetics in lupus. Autoimmunity 47, 213–214 (2014).
De Oliveira, N. F. P., de Souza, B. F. & de Castro Coêlho, M. UV radiation and its relation to DNA methylation in epidermal cells: a review. Epigenomes 4, 23 (2020).
Sawalha, A. H. et al. Defective T-cell ERK signaling induces interferon-regulated gene expression and overexpression of methylation-sensitive genes similar to lupus patients. Genes Immun. 9, 368–378 (2008).
Adams, D. E. & Shao, W. H. Epigenetic alterations in immune cells of systemic lupus erythematosus and therapeutic implications. Cells 11, 506 (2022).
Esteller, M. Non-coding RNAs in human disease. Nat. Rev. Genet. 12, 861–874 (2011).
Perez-Hernandez, J. et al. Increased urinary exosomal microRNAs in patients with systemic lupus erythematosus. PLoS ONE 10, e0138618 (2015).
So, B. Y. F., Yap, D. Y. H. & Chan, T. M. MicroRNAs in lupus nephritis—role in disease pathogenesis and clinical applications. Int. J. Mol. Sci. 22, 10737 (2021).
Chi, M. et al. Immunological involvement of microRNAs in the key events of systemic lupus erythematosus. Front. Immunol. 12, 699684 (2021).
Yang, R., Hu, Y. & Bo, L. Genome variation and precision medicine in systemic lupus erythematosus. Methods Mol. Biol. 2204, 193–203 (2020).
Nelson, M. R. et al. The support of human genetic evidence for approved drug indications. Nat. Genet. 47, 856–860 (2015).
Bennett, L. et al. Interferon and granulopoiesis signatures in systemic lupus erythematosus blood. J. Exp. Med. 197, 711–723 (2003).
Banchereau, R. et al. Personalized immunomonitoring uncovers molecular networks that stratify lupus patients. Cell 165, 551–565 (2016).
Shobha, V. et al. Identification and stratification of systemic lupus erythematosus patients into two transcriptionally distinct clusters based on IFN-I signature. Lupus 30, 762–774 (2021).
Haynes, W. A. et al. Integrated, multicohort analysis reveals unified signature of systemic lupus erythematosus. JCI Insight 5, e122312 (2020).
Piga, M. et al. Risk factors of damage in early diagnosed systemic lupus erythematosus: results of the Italian multicentre Early Lupus Project inception cohort. Rheumatology 59, 2272–2281 (2020).
Morgan, C. et al. Individuals living with lupus: findings from the LUPUS UK Members Survey 2014. Lupus 27, 681–687 (2018).
Billi, A. C. et al. Nonlesional lupus skin contributes to inflammatory education of myeloid cells and primes for cutaneous inflammation. Sci. Transl Med. 14, eabn2263 (2022).
Fava, A. et al. Integrated urine proteomics and renal single-cell genomics identify an IFN-γ response gradient in lupus nephritis. JCI Insight 5, e138345 (2020).
Wang, M. et al. Diverse roles of NETosis in the pathogenesis of lupus. Front. Immunol. 13, 895216 (2022).
Decout, A. et al. The cGAS–STING pathway as a therapeutic target in inflammatory diseases. Nat. Rev. Immunol. 21, 548–569 (2021).
Merrill, J. T. et al. Efficacy and safety of rituximab in moderately-to-severely active systemic lupus erythematosus: the randomized, double-blind, phase II/III systemic lupus erythematosus evaluation of rituximab trial. Arthritis Rheum. 62, 222–233 (2010).
Petri, M. et al. Association between changes in gene signatures expression and disease activity among patients with systemic lupus erythematosus. BMC Med. Genomics 12, 4 (2019).
Northcott, M. et al. Glucocorticoid gene signatures in systemic lupus erythematosus and the effects of type I interferon: a cross-sectional and in-vitro study. Lancet Rheumatol. 3, e357–e370 (2021).
Northcott, M. et al. Type 1 interferon status in systemic lupus erythematosus: a longitudinal analysis. Lupus Sci. Med. 9, e000625 (2022).
Dörner, T. et al. Abnormalities of B cell subsets in patients with systemic lupus erythematosus. J. Immunol. Methods 363, 187–197 (2011).
Md Yusof, M. Y. et al. Predicting and managing primary and secondary non-response to rituximab using B-cell biomarkers in systemic lupus erythematosus. Ann. Rheum. Dis. 76, 1829–1836 (2017).
Von Spee-Mayer, C. et al. Low-dose interleukin-2 selectively corrects regulatory T cell defects in patients with systemic lupus erythematosus. Ann. Rheum. Dis. 75, 1407–1415 (2016).
Scalapino, K. J. et al. Suppression of disease in New Zealand Black/New Zealand White lupus-prone mice by adoptive transfer of ex vivo expanded regulatory T cells. J. Immunol. 177, 1451–1459 (2006).
Kubo, S. et al. Peripheral immunophenotyping identifies three subgroups based on T cell heterogeneity in lupus patients. Arthritis Rheumatol. 69, 2029–2037 (2017).
Sasaki, T. et al. Longitudinal immune cell profiling in early systemic lupus erythematosus. Arthritis Rheumatol. 74, 1808–1821 (2022).
O’Gorman, W. E. et al. Mass cytometry identifies a distinct monocyte cytokine signature shared by clinically heterogeneous pediatric SLE patients. J. Autoimmun. 81, 74–89 (2017).
Panousis, N. I. et al. Combined genetic and transcriptome analysis of patients with SLE: distinct, targetable signatures for susceptibility and severity. Ann. Rheum. Dis. 78, 1079–1089 (2019).
Nehar-Belaid, D. et al. Mapping systemic lupus erythematosus heterogeneity at the single-cell level. Nat. Immunol. 21, 1094–1106 (2020).
Perez, R. K. et al. Single-cell RNA-seq reveals cell type-specific molecular and genetic associations to lupus. Science 376, eabf1970 (2022).
Der, E. et al. Single cell RNA sequencing to dissect the molecular heterogeneity in lupus nephritis. JCI Insight 2, e93009 (2017).
Dunlap, G. S. et al. Single-cell transcriptomics reveals distinct effector profiles of infiltrating T cells in lupus skin and kidney. JCI Insight 7, e156341 (2022).
Robinson, G. A. et al. Disease-associated and patient-specific immune cell signatures in juvenile-onset systemic lupus erythematosus: patient stratification using a machine-learning approach. Lancet Rheumatol. 2, e485–e496 (2020).
Nakano, M. et al. Distinct transcriptome architectures underlying lupus establishment and exacerbation. Cell 185, 3375–3389 (2022).
Yu, H., Nagafuchi, Y. & Fujio, K. Clinical and immunological biomarkers for systemic lupus erythematosus. Biomolecules 11, 928 (2021).
Aringer, M. et al. 2019 European League Against Rheumatism/American College of Rheumatology classification criteria for systemic lupus erythematosus. Ann. Rheum. Dis. 78, 1151–1159 (2019).
Zhang, R. et al. Increased expression of hub gene CXCL10 in peripheral blood mononuclear cells of patients with systemic lupus erythematosus. Exp. Ther. Med. 18, 4067–4075 (2019).
Narumi, S. et al. Serum levels of ifn-inducible PROTEIN-10 relating to the activity of systemic lupus erythematosus. Cytokine 12, 1561–1565 (2000).
Capecchi, R. et al. New biomarkers in SLE: from bench to bedside. Rheumatology 59, v12–v18 (2020).
Fragoso-Loyo, H. et al. Interleukin-6 and chemokines in the neuropsychiatric manifestations of systemic lupus erythematosus. Arthritis Rheum. 56, 1242–1250 (2007).
Matsuoka, N. et al. Galectin-9 as a biomarker for disease activity in systemic lupus erythematosus. PLoS ONE 15, e0227069 (2020).
Van den Hoogen, L. L. et al. Galectin-9 is an easy to measure biomarker for the interferon signature in systemic lupus erythematosus and antiphospholipid syndrome. Ann. Rheum. Dis. 77, 1810–1814 (2018).
Oliveira, J. J. et al. The plasma biomarker soluble SIGLEC-1 is associated with the type I interferon transcriptional signature, ethnic background and renal disease in systemic lupus erythematosus. Arthritis Res. Ther. 20, 152 (2018).
El-Sherbiny, Y. M. et al. B cell tetherin: a flow cytometric cell-specific assay for response to type I interferon predicts clinical features and flares in systemic lupus erythematosus. Arthritis Rheumatol. 72, 769–779 (2020).
Zollars, E. et al. BAFF (B cell activating factor) transcript level in peripheral blood of patients with SLE is associated with same-day disease activity as well as global activity over the next year. Lupus Sci. Med. 2, e000063 (2015).
Theodorou, E. et al. B-cell activating factor and related genetic variants in lupus related atherosclerosis. J. Autoimmun. 92, 87–92 (2018).
Chun, H. Y. et al. Cytokine IL-6 and IL-10 as biomarkers in systemic lupus erythematosus. J. Clin. Immunol. 27, 461–466 (2007).
Zhang, Q., Sun, L. & Jin, L. Spot urine protein/creatinine ratio is unreliable estimate of 24 h proteinuria in lupus nephritis when the histological scores of activity index are higher. Lupus 24, 943–947 (2015).
Guedes Marques, M. et al. Random spot urine protein/creatinine ratio: a reliable method for monitoring lupus nephritis? Clin. Kidney J. 6, 590–594 (2013).
Lee, Y. H. & Song, G. G. Urinary MCP-1 as a biomarker for lupus nephritis: a meta-analysis. Z. Rheumatol. 76, 357–363 (2017).
Campbell, S. et al. Proinflammatory effects of TWEAK/Fn14 interactions in glomerular mesangial cells. J. Immunol. 176, 1889–1898 (2006).
Xuejing, Z. et al. Urinary TWEAK level as a marker of lupus nephritis activity in 46 cases. J. Biomed. Biotechnol. 2012, 359647 (2012).
Suttichet, T. B. et al. Urine TWEAK level as a biomarker for early response to treatment in active lupus nephritis: a prospective multicentre study. Lupus Sci. Med. 6, e000298 (2019).
Zhao, Z. et al. TWEAK/Fn14 interactions are instrumental in the pathogenesis of nephritis in the chronic graft-versus-host model of systemic lupus erythematosus. J. Immunol. 179, 7949–7958 (2007).
Supavekin, S. et al. Differential gene expression following early renal ischemia/reperfusion. Kidney Int. 63, 1714–1724 (2003).
Rubinstein, T. et al. Urinary neutrophil gelatinase-associated lipocalin as a novel biomarker for disease activity in lupus nephritis. Rheumatology 49, 960–971 (2010).
Mok, C. C. et al. Urinary angiostatin, CXCL4 and VCAM-1 as biomarkers of lupus nephritis. Arthritis Res. Ther. 20, 6 (2018).
Fasano, S. et al. Biomarker panels may be superior over single molecules in prediction of renal flares in systemic lupus erythematosus: an exploratory study. Rheumatology 59, 3193–3200 (2020).
Garantziotis, P. et al. Molecular taxonomy of systemic lupus erythematosus through data-driven patient stratification: molecular endotypes and cluster-tailored drugs. Front. Immunol. 13, 860726 (2022).
Wang, Y. F. et al. Identification of ST3AGL4, MFHAS1, CSNK2A2 and CD226 as loci associated with systemic lupus erythematosus (SLE) and evaluation of SLE genetics in drug repositioning. Ann. Rheum. Dis. 77, 1078–1084 (2018).
Toro-Domínguez, D., Carmona-Sáez, P. & Alarcón-Riquelme, M. E. Support for phosphoinositol 3 kinase and mTOR inhibitors as treatment for lupus using in-silico drug-repurposing analysis. Arthritis Res. Ther. 19, 54 (2017).
Lai, Z. W. et al. Sirolimus in patients with clinically active systemic lupus erythematosus resistant to, or intolerant of, conventional medications: a single-arm, open-label, phase 1/2 trial. Lancet 391, 1186–1196 (2018).
Toro-Domínguez, D. et al. Differential treatments based on drug-induced gene expression signatures and longitudinal systemic lupus erythematosus stratification. Sci. Rep. 9, 15502 (2019).
Hubbard, E. L. et al. Analysis of gene expression from systemic lupus erythematosus synovium reveals myeloid cell-driven pathogenesis of lupus arthritis. Sci. Rep. 10, 17361 (2020).
Author information
Authors and Affiliations
Contributions
S.F. and A.M. researched data for the article. S.F., A.M., D.A.I. and F.C. contributed substantially to the discussion of content. S.F. wrote the article. All authors contributed to review and/or editing of the manuscript before submission.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Rheumatology thanks Antonis Fanouriakis, Mariele Gatto and Keishi Fujio for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fasano, S., Milone, A., Nicoletti, G.F. et al. Precision medicine in systemic lupus erythematosus. Nat Rev Rheumatol 19, 331–342 (2023). https://doi.org/10.1038/s41584-023-00948-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41584-023-00948-y
This article is cited by
-
SLE serum induces altered goblet cell differentiation and leakiness in human intestinal organoids
EMBO Molecular Medicine (2024)