Abstract
Obesity and type 2 diabetes mellitus (T2DM) are widespread, non-communicable diseases that are responsible for considerable levels of morbidity and mortality globally, primarily in the form of cardiovascular disease (CVD). Changes to lifestyle and behaviour have insufficient long-term efficacy in most patients with these diseases; metabolic surgery, although effective, is not practically deliverable on the scale that is required. Over the past two decades, therapies based on incretin hormones, spearheaded by glucagon-like peptide 1 (GLP1) receptor agonists (GLP1RAs), have become the treatment of choice for obesity and T2DM, and clinical evidence now suggests that these agents have benefits for CVD. We review the latest advances in incretin-based pharmacotherapy. These include ‘GLP1 plus’ agents, which combine the known advantages of GLP1RAs with the activity of additional hormones, such as glucose-dependent insulinotropic peptide, glucagon and amylin, to achieve desired therapeutic goals. Second-generation non-peptidic oral GLP1RAs promise to extend the benefits of GLP1 therapy to those who do not want, or cannot have, subcutaneous injection therapy. We conclude with a discussion of the knowledge gaps that must be addressed before incretin-based therapies can be properly deployed for maximum benefit in the treatment of obesity and T2DM.
Key points
-
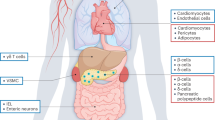
The incretins glucagon-like peptide 1 (GLP1) and glucose-dependent insulinotropic peptide (GIP) and related hormones such as glucagon and amylin regulate metabolism, gastrointestinal motility, appetite and body weight.
-
GLP1 receptor agonists (GLP1RAs) are established treatments for type 2 diabetes mellitus (T2DM) and obesity, with data that support positive effects on hard clinical end points such as cardiovascular events and renal outcomes.
-
‘GLP1 plus’ treatments go beyond GLP1RAs by combining GLP1 activity with complementary activities such as those of GIP, glucagon and amylin; these treatments are beginning to reach clinical practice.
-
People with T2DM and obesity have varying presentations with differing metabolic and organ involvement, so ‘GLP1 plus’ treatments might offer differential advantages, depending on the clinical picture.
-
Oral GLP1RAs are also beginning to reach clinical practice, and will open up access for those who do not want, or cannot have, injections; oral GLP1RAs can also be made at lower cost.
-
Evidence on the duration of treatment for obesity, on the treatment of children <12 years of age and women of reproductive age, on rare adverse effects and on how we can target treatment to subgroups needs to be developed.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Lean, M. E. et al. Primary care-led weight management for remission of type 2 diabetes (DiRECT): an open-label, cluster-randomised trial. Lancet 391, 541–551 (2018).
Taheri, S. et al. Effect of intensive lifestyle intervention on bodyweight and glycaemia in early type 2 diabetes (DIADEM-I): an open-label, parallel-group, randomised controlled trial. Lancet 6, 477–489 (2020).
Look AHEAD Research Group. Eight-year weight losses with an intensive lifestyle intervention: the look AHEAD study. Obesity 22, 5–13 (2014).
Diabetes Prevention Program Research Group. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet 374, 1677–1686 (2009).
Schauer, P. R. et al. Bariatric surgery versus intensive medical therapy for diabetes – 5-year outcomes. N. Engl. J. Med. 376, 641–651 (2017).
Perdomo, C. M., Cohen, R. V., Sumithran, P., Clément, K. & Frühbeck, G. Contemporary medical, device, and surgical therapies for obesity in adults. Lancet 401, 1116–1130 (2023).
Ikramuddin, S. et al. Lifestyle intervention and medical management with vs without Roux-en-Y gastric bypass and control of hemoglobin A1c, LDL cholesterol, and systolic blood pressure at 5 years in the Diabetes Surgery study. JAMA 319, 266–278 (2018).
Mingrone, G. et al. Bariatric-metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 year follow-up of an open-label, single-centre, randomised controlled trial. Lancet 386, 964–973 (2015).
World Health Organization. WHO European regional obesity report. (WHO, 2022).
Cohen, R. V. et al. Gastric bypass versus best medical treatment for diabetic kidney disease: 5 years follow up of a single-centre open label randomised controlled trial. EClinicalMedicine 53, e200420 (2022).
Tan, T. M. M. Co-agonist therapeutics come of age for obesity. Nat. Rev. Endocrinol. 19, 66–67 (2022).
Hinke, S. A. et al. Identification of a bioactive domain in the amino-terminus of glucose-dependent insulinotropic polypeptide (GIP). Biochim. Biophys. Acta Protein Struct. Mol. Enzymol. 1547, 143–155 (2001).
Mojsov, S., Weir, G. C. & Habener, J. F. Insulinotropin: glucagon-like peptide I (7-37) co-encoded in the glucagon gene is a potent stimulator of insulin release in the perfused rat pancreas. J. Clin. Invest. 79, 616–619 (1987).
Gribble, F. M. & Reimann, F. Function and mechanisms of enteroendocrine cells and gut hormones in metabolism. Nat. Rev. Endocrinol. 15, 226–237 (2019).
Nauck, M. A., Homberger, E., Eberghard, S. G., Allen, R. C. & Eaton, P. Incretin effects of increasing glucose loads in man calculated from venous insulin and C-peptide responses. J. Clin. Endocrinol. Metab. 63, 492–498 (1986).
Gasbjerg, L. S. et al. Evaluation of the incretin effect in humans using GIP and GLP-1 receptor antagonists. Peptides 125, 170183 (2020).
Nauck, M., Stöckmann, F., Ebert, R. & Creutzfeldt, W. Reduced incretin effect in type 2 (non-insulin-dependent) diabetes. Diabetologia 29, 46–52 (1986).
Højberg, P. V. et al. Four weeks of near-normalisation of blood glucose improves the insulin response to glucagon-like peptide-1 and glucose-dependent insulinotropic polypeptide in patients with type 2 diabetes. Diabetologia 52, 199–207 (2009).
Vilsbøll, T., Agersø, H., Krarup, T. & Holst, J. J. Similar elimination rates of glucagon-like peptide-1 in obese type 2 diabetic patients and healthy subjects. J. Clin. Endocrinol. Metab. 88, 220–224 (2003).
Kjems, L. L., Holst, J. J., Vølund, A. & Madsbad, S. The influence of GLP-1 on glucose-stimulated insulin secretion: effects on β-cell sensitivity in type 2 and nondiabetic subjects. Diabetes 52, 380–386 (2003).
Mentis, N. et al. GIP does not potentiate the antidiabetic effects of GLP-1 in hyperglycemic patients with type 2 diabetes. Diabetes 60, 1270–1276 (2011).
Kimball, C. & Murlin, J. R. Aqueous extracts of pancreas: III. Some precipitation reactions of insulin. J. Biol. Chem. 58, 337–346 (1923).
Wewer Albrechtsen, N. J. et al. 100 years of glucagon and 100 more. Diabetologia 66, 1378–1394 (2023).
Svendsen, B. et al. Insulin secretion depends on intra-islet glucagon signaling. Cell Rep. 25, 1127–1134.e2 (2018).
Kim, T. et al. Hepatic glucagon receptor signaling enhances insulin-stimulated glucose disposal in rodents. Diabetes 67, 2157–2166 (2018).
Cegla, J. et al. Coinfusion of low-dose GLP-1 and glucagon in man results in a reduction in food intake. Diabetes 63, 3711–3720 (2014).
Flint, A., Raben, A., Astrup, A. & Holst, J. J. Glucagon-like peptide 1 promotes satiety and suppresses energy intake in humans. J. Clin. Invest. 101, 515–520 (1998).
Turton, M. et al. A role for glucagon-like peptide-1 in the central regulation of feeding. Nature 379, 69–72 (1991).
Verdich, C. et al. A meta-analysis of the effect of glucagon-like peptide-1 (7-36) amide on ad libitum energy intake in humans. J. Clin. Endocrinol. Metab. 86, 4382–4389 (2001).
Drucker, D. J. GLP-1 physiology informs the pharmacotherapy of obesity. Mol. Metab. 57, 101351 (2022).
Varin, E. M. et al. Distinct neural sites of GLP-1R expression mediate physiological versus pharmacological control of incretin action. Cell Rep. 27, 3371–3384.e3 (2019).
Sisley, S. et al. Neuronal GLP1R mediates liraglutide’s anorectic but not glucose-lowering effect. J. Clin. Invest. 124, 2456–2463 (2014).
Meyer-Gerspach, A. C. et al. Endogenous GLP-1 alters postprandial functional connectivity between homeostatic and reward-related brain regions involved in regulation of appetite in healthy lean males: a pilot study. Diabetes Obes. Metab. 20, 2330–2338 (2018).
Ten Kulve, J. S. et al. Elevated postoperative endogenous GLP-1 levels mediate effects of Roux-en-Y gastric bypass on neural responsivity to food cues. Diabetes Care 40, 1522–1529 (2017).
De Silva, A. et al. The gut hormones PYY 3-36 and GLP-1 7-36 amide reduce food intake and modulate brain activity in appetite centers in humans. Cell Metab. 14, 700–706 (2011).
Steinert, R. E. et al. Effect of glucagon-like peptide-1 receptor antagonism on appetite and food intake in healthy men. Am. J. Clin. Nutr. 100, 514–523 (2014).
Borgmann, D. et al. Gut-brain communication by distinct sensory neurons differently controls feeding and glucose metabolism. Cell Metab. 33, 1466–1482.e7 (2021).
Asmar, M. et al. On the role of glucose-dependent insulintropic polypeptide in postprandial metabolism in humans. Am. J. Physiol. Endocrinol. Metab. 298, 614–621 (2010).
Bergmann, N. C. et al. Effects of combined GIP and GLP-1 infusion on energy intake, appetite and energy expenditure in overweight/obese individuals: a randomised, crossover study. Diabetologia 62, 665–675 (2019).
Bergmann, N. C. et al. No acute effects of exogenous glucose-dependent insulinotropic polypeptide on energy intake, appetite, or energy expenditure when added to treatment with a long-acting glucagon-like peptide 1 receptor agonist in men with type 2 diabetes. Diabetes Care 43, 588–596 (2020).
Mroz, P. A. et al. Optimized GIP analogs promote body weight lowering in mice through GIPR agonism not antagonism. Mol. Metab. 20, 51–62 (2019).
Andriaenssens, A.E. et al. Glucose-dependent insulinotropic polypeptide receptor-expressing cells in the hypothalamus regulate food intake. Cell Metab. 30, 987–996.e6 (2019).
Knop, F. K. et al. A long-acting glucose-dependent insulinotropic polypeptide receptor agonist shows weight loss without nausea or vomiting [abstract]. Diabetes 72 (Suppl. 1), 56-OR (2023).
Davies, I. & Tan, T. M. M. Design of novel therapeutics targeting the glucose-dependent insulinotropic polypeptide receptor (GIPR) to aid weight loss. Expert. Opin. Drug. Discov. 18, 659–669 (2023).
Müller, T. D., Finan, B., Clemmensen, C., Dimarchi, R. D. & Tschöp, M. H. The new biology and pharmacology of glucagon. Physiol. Rev. 97, 721–766 (2017).
Kissileff, H. R., Xavier Pi-sunyer, F., Hinton, V. & Xavier Pi-Sunyer, F. Individual, but not simultaneous, glucagon and cholecystokinin infusions inhibit feeding in men. Am. J. Physiol. 262, R975–R980 (1992).
Schulman, J. L., Carleton, J. L., Whitney, G. & Whitehorn, J. C. Effect of glucagon on food intake and body weight in man. J. Appl. Physiol. 11, 419–421 (1957).
Geary, N. & Smith, G. P. Selective hepatic vagotomy blocks pancreatic glucagon’s satiety effect. Physiol. Behav. 31, 391–394 (1983).
Müller, T. D. et al. Glucagon-like peptide 1 (GLP-1). Mol. Metab. 30, 72–130 (2019).
Salem, V. et al. Glucagon increases energy expenditure independently of brown adipose tissue activation in humans. Diabetes Obes. Metab. 18, 72–81 (2016).
Tan, T. M. et al. Coadministration of glucagon-like peptide-1 during glucagon infusion in humans results in increased energy expenditure and amelioration of hyperglycemia. Diabetes 62, 1131–1138 (2013).
Hope, D. C. D. et al. Hypoaminoacidemia underpins glucagon-mediated energy expenditure and weight loss. Cell Rep. Med. 3, 100810 (2022).
Godoy-Matos, A. F., Silva Júnior, W. S. & Valerio, C. M. NAFLD as a continuum: from obesity to metabolic syndrome and diabetes. Diabetol. Metab. Syndr. 12, 60 (2020).
Reda, T. K., Geliebter, A. & Pi-Sunyer, F. X. Amylin, food intake, and obesity. Obes. Res. 10, 1087–1091 (2002).
Boccia, L. et al. Amylin brain circuitry. Peptides 132, 170366 (2020).
Asmar, M., Bache, M., Knop, F. K., Madsbad, S. & Holst, J. J. Do the actions of glucagon-like peptide-1 on gastric emptying, appetite, and food intake involve release of amylin in humans? J. Clin. Endocrinol. Metab. 95, 2367–2375 (2010).
Roth, J. D. et al. Leptin responsiveness restored by amylin agonism in diet-induced obesity: evidence from nonclinical and clinical studies. Proc. Natl Acad. Sci. USA 105, 7257–7262 (2008).
Batterham, R. L. et al. Inhibition of food intake in obese subjects by peptide YY 3-36. N. Engl. J. Med. 349, 941–948 (2003).
Sloth, B., Holst, J. J., Flint, A., Gregersen, N. T. & Astrup, A. Effects of PYY 1-36 and PYY 3-36 on appetite, energy intake, energy expenditure, glucose and fat metabolism in obese and lean subjects. Am. J. Physiol. Endocrinol. Metab. 292, 1062–1068 (2007).
Behary, P. et al. Combined GLP-1, oxyntomodulin and peptide YY improves body weight and glycaemia in obesity and prediabetes/type 2 diabetes: a randomized single-blinded placebo-controlled study. Diabetes Care 42, 1446–1453 (2019).
Nauck, M. A., Kemmeries, G., Holst, J. J. & Meier, J. J. Rapid tachyphylaxis of the glucagon-like peptide 1-induced deceleration of gastric emptying in humans. Diabetes 60, 1561–1565 (2011).
Pironi, L. et al. Fat-induced ileal brake in humans: a dose-dependent phenomenon correlated to the plasma levels of peptide YY. Gastroenterology 105, 733–739 (1993).
Macconell, L., Pencek, R., Li, Y., Maggs, D. & Porter, L. Exenatide once weekly: sustained improvement in glycemic control and cardiometabolic measures through 3 years. Diabetes Metab. Syndr. Obes. 6, 31–41 (2013).
Nauck, M. et al. Efficacy and safety comparison of liraglutide, glimepiride, and placebo, all in combination with metformin, in type 2 diabetes. Diabetes Care 32, 84–90 (2009).
Buse, J. B. et al. Effects of exenatide (exendin-4) on glycemic control over 30 weeks in sulfonylurea-treated patients with type 2 diabetes. Diabetes Care 28, 1083–1091 (2004).
Jelsing, J. et al. Liraglutide: short-lived effect on gastric emptying – long lasting effects on body weight. Diabetes Obes. Metab. 14, 531–538 (2012).
Gutzwiller, J.-P. et al. Glucagon-like peptide-1 promotes satiety and reduces food intake in patients with diabetes mellitus type 2. Am. J. Physiol. 276, R151–R154 (1999).
Mentlein, R., Gallwitz, B. & Schmidt, W. E. Dipeptidyl‐peptidase IV hydrolyses gastric inhibitory polypeptide, glucagon‐like peptide‐1(7–36)amide, peptide histidine methionine and is responsible for their degradation in human serum. Eur. J. Biochem. 214, 829–835 (1993).
Deacon, C. F., Johnsen, A. H. & Holst, J. J. Degradation of glucagon-like peptide-1 by human plasma in vitro yields an N-terminally truncated peptide that is a major endogenous metabolite in vivo. J. Clin. Endocrinol. Metab. 80, 952–957 (1995).
Glaesner, W. et al. Engineering and characterization of the long-acting glucagon-like peptide-1 analogue LY2189265, an Fc fusion protein. Diabetes Metab. Res. Rev. 26, 287–296 (2010).
Lau, J. et al. Discovery of the once-weekly glucagon-like peptide-1 (GLP-1) analogue semaglutide. J. Med. Chem. 58, 7370–7380 (2015).
Umpierrez, G., Povedano, S. T., Manghi, F. P., Shurzinske, L. & Pechtner, V. Efficacy and safety of dulaglutide monotherapy versus metformin in type 2 diabetes in a randomized controlled trial (AWARD-3). Diabetes Care 37, 2168–2176 (2014).
Dungan, K. M. et al. Once-weekly dulaglutide versus once-daily liraglutide in metformin-treated patients with type 2 diabetes (AWARD-6): a randomised, open-label, phase 3, non-inferiority trial. Lancet 384, 1349–1357 (2014).
Chen, Y. H. et al. Efficacy and safety of dulaglutide monotherapy compared with glimepiride in East-Asian patients with type 2 diabetes in a multicentre, double-blind, randomized, parallel-arm, active comparator, phase III trial. Diabetes Obes. Metab. 20, 2121–2130 (2018).
Wysham, C. et al. Efficacy and safety of dulaglutide added onto pioglitazone and metformin versus exenatide in type 2 diabetes in a randomized controlled trial (AWARD-1). Diabetes Care 37, 2159–2167 (2014).
Giorgino, F., Benroubi, M., Sun, J. H., Zimmermann, A. G. & Pechtner, V. Efficacy and safety of once-weekly dulaglutide versus insulin glargine in patients with type 2 diabetes on metformin and glimepiride (AWARD-2). Diabetes Care 38, 2241–2249 (2015).
Blonde, L. et al. Once-weekly dulaglutide versus bedtime insulin glargine, both in combination with prandial insulin lispro, in patients with type 2 diabetes (AWARD-4): a randomised, open-label, phase 3, non-inferiority study. Lancet 385, 2057–2066 (2015).
Frias, J. P. et al. Efficacy and safety of dulaglutide 3.0 mg and 4.5 mg vs dulaglutide 1.5 mg in metformin-treated patients with type 2 diabetes in a randomised controlled trial. Diabetes Care 44, 765–773 (2021).
Frías, J. P. et al. Efficacy and safety of once-weekly semaglutide 2·0 mg versus 1·0 mg in patients with type 2 diabetes (SUSTAIN FORTE): a double-blind, randomised, phase 3B trial. Lancet Diabetes Endocrinol. 9, 563–574 (2021).
Pratley, R. E. et al. Semaglutide versus dulaglutide once weekly in patients with type 2 diabetes (SUSTAIN 7): a randomised, open-label, phase 3b trial. Lancet Diabetes Endocrinol. 6, 275–286 (2018).
Capehorn, M. S. et al. Efficacy and safety of once-weekly semaglutide 1.0 mg vs once-daily liraglutide 1.2 mg as add-on to 1–3 oral antidiabetic drugs in subjects with type 2 diabetes (SUSTAIN 10). Diabetes Metab. 46, 100–109 (2020).
Marso, S. P. et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N. Engl. J. Med. 375, 1834–1844 (2016).
Kapitza, C., Dahl, K., Jacobsen, J. B., Axelsen, M. B. & Flint, A. Effects of semaglutide on beta cell function and glycaemic control in participants with type 2 diabetes: a randomised, double-blind, placebo-controlled trial. Diabetologia 60, 1390–1399 (2017).
Wilding, J. P. H. et al. Once-weekly semaglutide in adults with overweight or obesity. N. Engl. J. Med. 384, 989–1002 (2021).
Rubino, D. M. et al. Effect of weekly subcutaneous semaglutide vs daily liraglutide on body weight in adults with overweight or obesity without diabetes: the STEP 8 randomized clinical trial. JAMA 327, 138–150 (2022).
Wadden, T. A. et al. Effect of subcutaneous semaglutide vs placebo as an adjunct to intensive behavioral therapy on body weight in adults with overweight or obesity: the STEP 3 randomized clinical trial. JAMA 325, 1403–1413 (2021).
Rubino, D. et al. Effect of continued weekly subcutaneous semaglutide vs placebo on weight loss maintenance in adults with overweight or obesity: the STEP 4 randomized clinical trial. JAMA 325, 1414–1425 (2021).
Kadowaki, T. et al. Semaglutide once a week in adults with overweight or obesity, with or without type 2 diabetes in an east Asian population (STEP 6): a randomised, double-blind, double-dummy, placebo-controlled, phase 3a trial. Lancet Diabetes Endocrinol. 10, 193–206 (2022).
Garvey, W. T. et al. Two-year effects of semaglutide in adults with overweight or obesity: the STEP 5 trial. Nat. Med. 28, 2083–2091 (2022). The first phase III trial demonstrating that once-weekly subcutaneous semaglutide can maintain moderate weight loss with a favourable tolerability and safety profile.
Wilding, J. P. H. et al. Weight regain and cardiometabolic effects after withdrawal of semaglutide: the STEP 1 trial extension. Diabetes Obes. Metab. 24, 1553–1564 (2022). In this trial, participants had regained two-thirds of their prior weight loss 1 year after withdrawal of semaglutide, confirming the chronicity of obesity and the need for ongoing treatment.
Weghuber, D. et al. Once-weekly semaglutide in adolescents with obesity. N. Engl. J. Med. 387, 2245–2257 (2022).
Davies, M. et al. Semaglutide 2·4 mg once a week in adults with overweight or obesity, and type 2 diabetes (STEP 2): a randomised, double-blind, double-dummy, placebo-controlled, phase 3 trial. Lancet 397, 971–984 (2021).
Russell-Jones, D. & Khan, R. Insulin-associated weight gain in diabetes – causes, effects and coping strategies. Diabetes Obes. Metab. 9, 799–812 (2007).
Gerstein, H. C. et al. Dulaglutide and cardiovascular outcomes in type 2 diabetes (REWIND): a double-blind, randomised placebo-controlled trial. Lancet 394, 121–130 (2019).
Lincoff, A. M. et al. Semaglutide and cardiovascular outcomes in obesity without diabetes. N. Engl. J. Med. 389, 2221–2232 (2023). The SELECT trial demonstrated a reduced incidence of cardiovascular outcomes in people with obesity and pre-existing CVD but without T2DM treated once weekly with semaglutide compared with those treated with placebo.
Finan, B. et al. Unimolecular dual incretins maximize metabolic benefits in rodents, monkeys, and humans. Sci. Transl. Med. 5, 209ra151 (2013).
Rosenstock, J. et al. Efficacy and safety of a novel dual GIP and GLP-1 receptor agonist tirzepatide in patients with type 2 diabetes (SURPASS-1): a double-blind, randomised, phase 3 trial. Lancet 398, 143–155 (2021).
Frías, J. P. et al. Tirzepatide versus semaglutide once weekly in patients with type 2 diabetes. N. Engl. J. Med. 385, 503–515 (2021).
Dahl, D. et al. Effect of subcutaneous tirzepatide vs placebo added to titrated insulin glargine on glycemic control in patients with type 2 diabetes: the SURPASS-5 randomized clinical trial. JAMA 327, 534–545 (2022).
Inagaki, N., Takeuchi, M., Oura, T., Imaoka, T. & Seino, Y. Efficacy and safety of tirzepatide monotherapy compared with dulaglutide in Japanese patients with type 2 diabetes (SURPASS J-mono): a double-blind, multicentre, randomised, phase 3 trial. Lancet Diabetes Endocrinol. 10, 623–633 (2022).
Kadowaki, T., Chin, R., Ozeki, A., Imaoka, T. & Ogawa, Y. Safety and efficacy of tirzepatide as an add-on to single oral antihyperglycaemic medication in patients with type 2 diabetes in Japan (SURPASS J-combo): a multicentre, randomised, open-label, parallel-group, phase 3 trial. Lancet Diabetes Endocrinol. 10, 634–644 (2022).
Del Prato, S. et al. Tirzepatide versus insulin glargine in type 2 diabetes and increased cardiovascular risk (SURPASS-4): a randomised, open-label, parallel-group, multicentre, phase 3 trial. Lancet 398, 1811–1824 (2021).
Ludvik, B. et al. Once-weekly tirzepatide versus once-daily insulin degludec as add-on to metformin with or without SGLT2 inhibitors in patients with type 2 diabetes (SURPASS-3): a randomised, open-label, parallel-group, phase 3 trial. Lancet 398, 583–598 (2021).
Sorli, C. et al. Efficacy and safety of once-weekly semaglutide monotherapy versus placebo in subjects with type 2 diabetes (SUSTAIN 1): a randomised, placebo-controlled phase 3a trial. Diabetes Obes. Metab. 23, 404–414 (2021).
Aroda, V. R. et al. PIONEER 1: randomized clinical trial of the efficacy and safety of oral semaglutide monotherapy in comparison with placebo in patients with type 2 diabetes. Diabetes Care 42, 1724–1732 (2019).
Jastreboff, A. M. et al. Tirzepatide once weekly for the treatment of obesity. N. Engl. J. Med. 387, 205–216 (2022). This trial demonstrated that an incretin co-agonist (GLP1RA–GIPRA) represents an advance over the ‘monoagonist’ GLP1RA semaglutide in terms of weight loss benefit without an increase in gastrointestinal adverse events.
Mesinovic, J., Zengin, A., De Courten, B., Ebeling, P. R. & Scott, D. Sarcopenia and type 2 diabetes mellitus: a bidirectional relationship. Diabetes Metab. Syndr. Obes. 12, 1057 (2019).
Sattar, N. et al. Tirzepatide cardiovascular event risk assessment: a pre-specified meta-analysis. Nat. Med. 28, 591–598 (2022).
Holst, J. J. & Rosenkilde, M. M. GIP as a therapeutic target in diabetes and obesity: insight from incretin co-agonists. J. Clin. Endocrinol. Metab. 105, e2710–e2716 (2020).
Jones, B. The therapeutic potential of GLP-1 receptor biased agonism. Br. J. Pharmacol. 179, 492–510 (2022).
Willard, F. S. et al. Tirzepatide is an imbalanced and biased dual GIP and GLP-1 receptor agonist. JCI Insight 5, e140532 (2020).
Samms, R. J., Coghlan, M. P. & Sloop, K. W. How may GIP enhance the therapeutic efficacy of GLP-1? Trends Endocrinol. Metab. 31, 410–421 (2020).
Strande, J. L. et al. A phase 1, randomized, double-blind, placebo-controlled single and multiple ascending dose study of AMG 133 in subjects with obesity: late breaking: a phase 1 study of AMG 133 in subjects with obesity. Metabolism 142, 155433 (2023).
Hare, K. J. et al. The glucagonostatic and insulinotropic effects of glucagon-like peptide 1 contribute equally to its glucose-lowering action. Diabetes 59, 1765–1770 (2010).
Hope, D. C. D., Vincent, M. L. & Tan, T. M. M. Striking the balance: GLP-1/glucagon co-agonism as a treatment strategy for obesity. Front. Endocrinol. 12, 735019 (2021).
Galsgaard, K. D., Pedersen, J., Knop, F. K., Holst, J. J. & Albrechtsen, N. J. W. Glucagon receptor signaling and lipid metabolism. Front. Physiol. 10, 413 (2019).
Day, J. W. et al. A new glucagon and GLP-1 co-agonist eliminates obesity in rodents. Nat. Chem. Biol. 5, 749–757 (2009).
Nahra, R. et al. Effects of cotadutide on metabolic and hepatic parameters in adults with overweight or obesity and type 2 diabetes: a 54-week randomized phase 2b study. Diabetes Care 44, 1433–1442 (2021).
Le Roux, C. W. et al. A phase 2, randomized, double-blind, placebo-controlled, dose-finding study of survodutide (BI 456906) in people with overweight/obesity [abstract]. Diabetes 72 (Suppl. 1), 51-OR (2023).
Finan, B. et al. A rationally designed monomeric peptide triagonist corrects obesity and diabetes in rodents. Nat. Med. 21, 27–36 (2015).
Jastreboff, A. M. et al. Triple-hormone-receptor agonist retatrutide for obesity – a phase 2 trial. N. Engl. J. Med. 389, 514–526 (2023). This trial demonstrated that once-weekly administration of the highest dose of a unimolecular triple-agonist (GLP1RA–GIPRA–GCGRA) by subcutaneous injection in people with obesity and T2DM induces weight loss that appears comparable to that achieved with bariatric surgery, with a favourable safety and tolerability profile.
American Diabetes Assocation. American Diabetes Association highlights novel agent retatrutide which results in substantial weight reduction in people with obesity or type 2 diabetes during late breaking symposium. American Diabetes Association https://www2.diabetes.org/newsroom/press-releases/2023/american-diabetes-association-highlights-novel-agent-retatrutide-results-substantial-weight-reduction-people-with-obesity-type-2-diabetes-during-late-breaking-symposium (2023).
Quek, J. et al. Global prevalence of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in the overweight and obese population: a systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 8, 20–30 (2023).
Younossi, Z. M. et al. The global epidemiology of NAFLD and NASH in patients with type 2 diabetes: a systematic review and meta-analysis. J. Hepatol. 71, 793–801 (2019).
Sanyal, A. J. et al. Prospective study of outcomes in adults with nonalcoholic fatty liver disease. N. Engl. J. Med. 385, 1559–1569 (2021).
Fletcher, M. M. et al. AM833 is a novel agonist of calcitonin family G protein-coupled receptors: pharmacological comparison with six selective and nonselective agonists. J. Pharmacol. Exp. Ther. 377, 417–440 (2021).
Lau, D. C. W. et al. Once-weekly cagrilintide for weight management in people with overweight and obesity: a multicentre, randomised, double-blind, placebo-controlled and active-controlled, dose-finding phase 2 trial. Lancet 398, 2160–2172 (2021).
Frias, J. P. et al. Efficacy and safety of co-administered once-weekly cagrilintide 2·4 mg with once-weekly semaglutide 2·4 mg in type 2 diabetes: a multicentre, randomised, double-blind, active-controlled, phase 2 trial. Lancet 402, 720–730 (2023). In this trial, a fixed dose combination of once-weekly subcutaneous cagrilintide and semaglutide (a different approach to the unimolecular co-agonists tirzepatide, cotadutide and retatrutide) elicited impressive reductions in HbA1c and body weight over a short period in people with obesity and T2DM.
Field, B. C. T. et al. PYY3-36 and oxyntomodulin can be additive in their effect on food intake in overweight and obese humans. Diabetes 59, 1635–1639 (2010).
Neary, N. M. et al. Peptide YY3-36 and glucagon-like peptide-17-36 inhibit food intake additively. Endocrinology 146, 5120–5127 (2005).
Gantz, I. et al. Efficacy and safety of intranasal peptide YY3-36 for weight reduction in obese adults. J. Clin. Endocrinol. Metab. 92, 1754–1757 (2007).
Tan, T. M. M. et al. Safety and efficacy of an extended-release peptide YY analogue for obesity: a randomized, placebo-controlled, phase 1 trial. Diabetes Obes. Metab. 23, 1471–1483 (2021).
Overgaard, R. V., Navarria, A., Ingwersen, S. H., Bækdal, T. A. & Kildemoes, R. J. Clinical pharmacokinetics of oral semaglutide: analyses of data from clinical pharmacology trials. Clin. Pharmacokinet. 60, 1335–1348 (2021).
Buckley, S. T. et al. Transcellular stomach absorption of a derivatized glucagon-like peptide-1 receptor agonist. Sci. Transl. Med. 10, eaar7047 (2018).
Overgaard, R. V., Hertz, C. L., Ingwersen, S. H., Navarria, A. & Drucker, D. J. Levels of circulating semaglutide determine reductions in HbA1c and body weight in people with type 2 diabetes. Cell Rep. Med. 2, 100387 (2021).
Aroda, V. R. et al. Efficacy and safety of once-daily oral semaglutide 25 mg and 50 mg compared with 14 mg in adults with type 2 diabetes (PIONEER PLUS): a multicentre, randomised, phase 3b trial. Lancet 402, 693–704 (2023).
Thethi, T. K., Pratley, R. & Meier, J. J. Efficacy, safety and cardiovascular outcomes of once-daily oral semaglutide in patients with type 2 diabetes: the PIONEER programme. Diabetes Obes. Metab. 22, 1263–1277 (2020).
Knop, F. K. et al. Oral semaglutide 50 mg taken once per day in adults with overweight or obesity (OASIS 1): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 402, 705–719 (2023). This trial demonstrated that an oral formulation of semaglutide can result in double-digit weight loss with a favourable safety and tolerability profile in people with obesity.
Wharton, S. et al. Daily oral GLP-1 receptor agonist orforglipron for adults with obesity. N. Engl. J. Med. 389, 877–888 (2023). Orforglipron is a novel, oral, once-daily G protein-biased non-peptidic GLP1RA that resulted in impressive weight loss over a short-period in a phase II trial in people with obesity.
Frias, J. P. et al. Efficacy and safety of oral orforglipron in patients with type 2 diabetes: a multicentre, randomised, dose-response, phase 2 study. Lancet 402, 472–483 (2023).
Kelly, A. S. et al. A randomized, controlled trial of liraglutide for adolescents with obesity. N. Engl. J. Med. 382, 2117–2128 (2020).
Tamborlane, W. V. et al. Liraglutide in children and adolescents with type 2 diabetes. N. Engl. J. Med. 381, 637–646 (2019).
Simmonds, M., Llewellyn, A., Owen, C. G. & Woolacott, N. Predicting adult obesity from childhood obesity: a systematic review and meta-analysis. Obes. Rev. 17, 95–107 (2016).
Alorfi, N. M. & Alshehri, F. S. Usage of glucagon-like peptide-1 for obesity in children; updated review of Clinicaltrials.gov. J. Multidiscip. Healthc. 16, 2179–2187 (2023).
Mastrandrea, L. D. et al. Liraglutide effects in a paediatric (7-11 y) population with obesity: a randomized, double-blind, placebo-controlled, short-term trial to assess safety, tolerability, pharmacokinetics, and pharmacodynamics. Pediatr. Obes. 14, e12495 (2019).
Kelly, A. S. et al. Exenatide as a weight-loss therapy in extreme pediatric obesity: a randomized, controlled pilot study. Obesity 20, 364–370 (2012).
Food and Drug Administration. Highlights of prescribing information: Wegovy (semaglutide) injection for subcutaneous use. FDA http://www.accessdata.fda.gov/drugsatfda_docs/label/2021/215256s000lbl.pdf (2021).
Aubry, E. M., Oelhafen, S., Fankhauser, N., Raio, L. & Cignacco, E. L. Adverse perinatal outcomes for obese women are influenced by the presence of comorbid diabetes and hypertensive disorders. Sci. Rep. 9, 9793 (2019).
Bone, J. N., Joseph, K. S., Mayer, C., Platt, R. & Lisonkova, S. The association between pre-pregnancy body mass index and perinatal death and the role of gestational age at delivery. PLoS One 17, e0264565 (2022).
Vernini, J. M. et al. Maternal and fetal outcomes in pregnancies complicated by overweight and obesity. Reprod. Health 13, 100 (2016).
Godfrey, K. M. et al. Influence of maternal obesity on the long-term health of offspring. Lancet Diabetes Endocrinol. 5, 53–64 (2017).
Patro Golab, B. et al. Influence of maternal obesity on the association between common pregnancy complications and risk of childhood obesity: an individual participant data meta-analysis. Lancet Child. Adolesc. Health 2, 812–821 (2018).
Cesta, C. E. et al. Safety of GLP-1 receptor agonists and other second-line antidiabetics in early pregnancy. JAMA Intern Med. 184, 144–152 (2024).
Parker, V. E. R. et al. Efficacy, safety, and mechanistic insights of cotadutide, a dual receptor glucagon-like peptide-1 and glucagon agonist. J. Clin. Endocrinol. Metab. 105, 803–820 (2020).
Simonsen, L. et al. Preclinical evaluation of a protracted GLP-1/glucagon receptor co-agonist: translational difficulties and pitfalls. PLoS ONE 17, e0264974 (2022).
Hope, D. C. D. & Tan, T. M. M. Glucagon and energy expenditure; revisiting amino acid metabolism and implications for weight loss therapy. Peptides 162, 170962 (2023).
Wang, W. et al. Association of semaglutide with risk of suicidal ideation in a real-world cohort. Nat. Med. 30, 168–176 (2024).
Author information
Authors and Affiliations
Contributions
All authors researched data for the article, contributed substantially to discussion of the content, wrote the article and reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
T.T. is a shareholder and consultant for Zihipp Ltd., an Imperial College spinout company developing gut hormone-based analogues for obesity. The other authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Endocrinology thanks Jonathan Campbell and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ansari, S., Khoo, B. & Tan, T. Targeting the incretin system in obesity and type 2 diabetes mellitus. Nat Rev Endocrinol (2024). https://doi.org/10.1038/s41574-024-00979-9
Accepted:
Published:
DOI: https://doi.org/10.1038/s41574-024-00979-9