Abstract
Atherosclerotic plaque results from a complex interplay between lipid deposition, inflammatory changes, cell migration and arterial wall injury. Over the past two decades, clinical trials utilizing invasive arterial imaging modalities, such as intravascular ultrasonography, have shown that reducing levels of atherogenic lipoproteins, mainly serum LDL-cholesterol (LDL-C), to very low levels can safely reduce overall atherosclerotic plaque burden and favourably modify plaque composition. Classically, this outcome has been achieved with intensive statin therapy. Since 2016, newer and potent lipid-lowering strategies, such as proprotein convertase subtilisin–kexin type 9 inhibition, have shown incremental effects on plaque regression and risk of clinical events. Despite maximal reduction in plasma LDL-C levels, considerable residual cardiovascular risk remains in some patients. Therefore, there is a need to study therapeutic approaches that address residual risk beyond LDL-C reduction to promote plaque stabilization or regression. Contemporary imaging modalities, such as coronary computed tomography angiography, enable non-invasive assessment of the overall atherosclerotic plaque burden as well as of certain local plaque characteristics. This technology could allow further study of plaque stabilization and regression using novel therapeutic approaches. Non-invasive plaque assessment might also offer the potential to guide personalized management strategies if validated for this purpose.
Key points
-
Intravascular ultrasonography is the traditionally favoured imaging technique to evaluate plaque burden and morphology in clinical trials; newer and promising invasive techniques include optical coherence tomography and near-infrared spectroscopy.
-
Non-invasive plaque assessment is feasible with coronary computed tomography angiography, including the evaluation of plaque distribution and burden across all epicardial coronary arteries and the identification of high-risk plaque features.
-
The strongest evidence for plaque regression and stabilization comes from clinical trials of intensive reductions of plasma LDL-cholesterol (LDL-C) with statin therapy and the use of intravascular ultrasonography to track coronary atherosclerosis over time.
-
Emerging evidence has shown that plasma LDL-C reduction with proprotein convertase subtilisin–kexin type 9 inhibitors leads to additional plaque regression.
-
Evidence to support non-LDL-C and non-lipid targeting to promote additional plaque regression is inconsistent and less robust than for LDL-C reduction.
-
Future trials should leverage non-invasive plaque assessment through coronary computed tomography angiography and focus on achieving residual risk reduction through effects on plaque regression and stabilization by modifying other targets such as plasma lipoprotein(a) levels.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Change history
12 January 2024
In the version of the article initially published, the name of a peer reviewer, Matthew Budoff, was mispelled in the reviewer acknowledgements, and has now been amended in the HTML and PDF versions of the article.
References
Libby, B. et al. Atherosclerosis. Nat. Rev. Dis. Prim. 16, 56 (2019).
Stary, H. C. et al. A definition of advanced types of atherosclerotic lesions and a histological classification of atherosclerosis: a report from the Committee on Vascular Lesions of the Council on Arteriosclerosis, American Heart Association. Arterioscler. Thromb. Vasc. Biol. 15, 1512–1531 (1995).
Moreno, P. R. The high-risk thin-cap fibroatheroma: a new kid on the block. Circ. Cardiovasc. Interv. 2, 500–502 (2009).
Libby, P. The changing landscape of atherosclerosis. Nature 592, 524–533 (2021).
Stone, P. H., Libby, P. & Boden, W. E. Fundamental pathobiology of coronary atherosclerosis and clinical implications for chronic ischemic heart disease management-the plaque hypothesis. A narrative review. JAMA Cardiol. 8, 192–201 (2023).
Dawson, L. P., Lum, M., Nerleker, N., Nicholls, S. J. & Layland, J. Coronary atherosclerotic plaque regression: JACC state-of-the-art review. J. Am. Coll. Cardiol. 79, 66–82 (2022).
Schuurman, A. et al. Prognostic value of intravascular ultrasound in patients with coronary artery disease. J. Am. Coll. Cardiol. 72, 2003–2011 (2018).
Zing, L. et al. Clinical significance of lipid-rich plaque detected by optical coherence tomography: a 4-year follow-up study. J. Am. Coll. Cardiol. 69, 2502–2513 (2017).
Budoff, M. J. et al. When does a calcium score equate to secondary prevention? Insights from the multicational CONFIRM registry. JACC Cardiovasc. Imaging 16, 1181–1189 (2023).
D’Ascenzo, F. et al. Atherosclerotic coronary plaque regression and the risk of adverse cardiovascular events: a meta-regression of randomized clinical trials. Atherosclerosis 226, 178–185 (2013).
Nissen, S. E. & Yock, P. Intravascular ultrasound: novel pathophysiological insights and current clinical applications. Circulation 103, 604–616 (2001).
Garcia-Garcia, H. M., Costa, M. A. & Serruys, P. W. Imaging of coronary atherosclerosis: intravascular ultrasound. Eur. Heart J. 31, 2456–2469 (2010).
Treusdell, A. G. et al. Intravascular imaging during percutaneous coronary intervention: JACC state-of-the-art review. J. Am. Coll. Cardiol. 81, 590–605 (2023).
Nair, A. et al. Coronary plaque classification with intravascular ultrasound radiofrequency data analysis. Circulation 106, 2200–2206 (2002).
Virmani, R., Burke, A. P., Farb, A. & Kolodgie, F. D. Pathology of the vulnerable plaque. J. Am. Coll. Cardiol. 47, C13–C18 (2006).
Araki, M. et al. Optical coherence tomography in coronary atherosclerosis assessment and intervention. Nat. Rev. Cardiol. 19, 684–703 (2022).
Yonetsu, T. et al. In vivo critical fibrous cap thickness for rupture-prone coronary plaques assessed by optical coherence tomography. Eur. Heart J. 32, 1251–1259 (2011).
Gerbaud, E. et al. Plaque burden can be assessed using intravascular optical coherence tomography and a dedicated automated processing algorithm: a comparison study with intravascular ultrasound. Eur. Heart J. Cardiovasc. Imaging 21, 640–652 (2020).
Jaguszewski, M., Klingenberg, R. & Landmesser, U. Intracoronary near-infrared spectroscopy (NIRS) imaging for detection of lipid content of coronary plaques: current experience and future perspectives. Curr. Cardiovasc. Imaging Rep. 6, 426–430 (2013).
Madder, R., Smith, J. L. & Dixon, S. R. Composition of target lesions by near-infrared spectroscopy in patients with acute coronary syndrome versus stable angina. Circ. Cardiovasc. Interv. 5, 55–61 (2012).
Sandfort, V., Lima, J. A. C. & Bluemke, D. A. Noninvasive imaging of atherosclerotic plaque progression: status of coronary computed tomography angiography. Circ. Cardiovasc. Imaging 8, e003316 (2015).
Voros, S. et al. Coronary atherosclerosis imaging by coronary CT angiography: current status, correlation with intravascular interrogation and meta-analysis. JACC Cardiovasc. Imaging 4, 537–548 (2011).
Saremi, F. & Achenbach, S. Coronary plaque characterization using CT. Am. J. Roentgenol. 204, W249–W260 (2015).
Einstein, A. J., Henzlova, M. J. & Rajagopalan, S. Estimating risk of cancer associated with radiation exposure from 64-slice computed tomography coronary angiography. JAMA 298, 317–323 (2007).
He, Y. et al. Accuracy of MRI to identify the coronary artery plaque: a comparative study with intravascular ultrasound. J. Magn. Reason. Imaging 35, 72–78 (2012).
Evans, N. R., Tarkin, J. M., Chowdhury, M. M., Warburton, E. A. & Rudd, J. H. F. PET imaging of atherosclerotic disease: advancing plaque assessment from anatomy to physiology. Curr. Atheroscler. Rep. 18, 30 (2016).
Fayad, Z. A. et al. Safety and efficacy of dalcetrapib on atherosclerotic disease using novel non-invasive multimodality imaging (dal-PLAQUE): a randomised clinical trial. Lancet 378, 1547–1559 (2011).
Grundy, S. M. et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Circulation 13, e1082–e1143 (2019).
Ornish, D. et al. Can lifestyle changes reverse coronary heart disease? The Lifestyle Heart Trial. Lancet 336, 129–133 (1990).
Ornish, D. et al. Intensive lifestyle changes for reversal of coronary heart disease. JAMA 280, 2001–2007 (1998).
Watts, G. F. et al. Effects on coronary artery disease of lipid-lowering diet, or diet plus cholestyramine, in the St Thomas’ Atherosclerosis Regression Study (STARS). Lancet 339, 563–569 (1992).
Henzel, J. et al. High-risk coronary plaque regression after intensive lifestyle intervention in nonobstructive coronary disease: a randomized study. JACC Cardiovasc. Imaging 14, 1192–1202 (2021).
Nissen, S. E. et al. Effect of intensive compared with moderate lipid-lowering therapy on progression of coronary atherosclerosis: a randomized controlled trial. JAMA 291, 1071–1080 (2004).
Nissen, S. E. et al. Statin therapy, LDL cholesterol, C-reactive protein, and coronary artery disease. N. Engl. J. Med. 352, 29–38 (2005).
Nicholls, S. J. et al. Effect of two intensive statin regimens on progression of coronary disease. N. Engl. J. Med. 365, 2078–2087 (2011).
Park, S. et al. Effect of statin treatment on modifying plaque composition: a double-blind, randomized study. J. Am. Coll. Cardiol. 67, 1772–1783 (2016).
Hiro, T. et al. Effect of intensive statin therapy on regression of coronary atherosclerosis in patients with acute coronary syndrome: a multicenter randomized trial evaluated by volumetric intravascular ultrasound using pitavastatin versus atorvastatin (JAPAN-ACS [Japan assessment of pitavastatin and atorvastatin in acute coronary syndrome] study). J. Am. Coll. Cardiol. 54, 293–302 (2009).
Nissen, S. E. et al. Effect of very high-intensity statin therapy on regression of coronary atherosclerosis: the ASTEROID trial. JAMA 295, 1556–1565 (2006).
Takayma, T. et al. Effect of rosuvastatin on coronary atheroma in stable coronary artery disease: multicenter coronary atherosclerosis study measuring effects of rosuvastatin using intravascular ultrasound in Japanese subjects (COSMOS). Circ. J. 73, 2110–2117 (2009).
Raber, L. et al. Effect of high-intensity statin therapy on atherosclerosis in non-infarct-related coronary arteries (IBIS-4): a serial intravascular ultrasonography study. Eur. Heart J. 21, 490–500 (2015).
Raber, L. et al. Changes in coronary plaque composition in patients with acute myocardial infarction treated with high-intensity statin therapy (IBIS-4): a serial optical coherence tomography study. JACC Cardiovasc. Imaging 12, 1518–1528 (2019).
Nishiguchi, T. et al. Effect of early pitavastatin therapy on coronary fibrous-cap thickness assessed by optimal coherence tomography in patients with acute coronary syndrome: the ESCORT study. JACC Cardiovasc. Imaging 11, 829–838 (2018).
Komukai, K. et al. Effect of atorvastatin therapy on fibrous cap thickness in coronary atherosclerotic plaque as assessed by optical coherence tomography: the EASY-FIT study. J. Am. Coll. Cardiol. 64, 2207–2217 (2014).
Kini, A. S. et al. Changes in plaque lipid content after short-term intensive versus standard statin therapy: the YELLOW trial (reduction in yellow plaque by aggressive lipid-lowering therapy). J. Am. Coll. Cardiol. 62, 21–29 (2013).
Lee, S. et al. Effects of statins on coronary atherosclerotic plaques: the PARADIGM study. JACC Cardiovasc. Imaging 11, 1475–1484 (2018).
Cannon, C. P. et al. Ezetimibe added to statin therapy after acute coronary syndromes. N. Engl. J. Med. 372, 2387–2397 (2015).
Kovarnik, T. et al. Virtual histology evaluation of atherosclerosis regression during atorvastatin and ezetimibe administration: HEAVEN study. Circ. J. 76, 176–183 (2012).
Nakajima, N. et al. Effect of combination of ezetimibe and a statin on coronary plaque regression in patients with acute coronary syndrome: ZEUS trial (eZEtimibe Ultrasound Study). IJC Metab. Endocr. 2, 8–13 (2014).
Tsujita, K. et al. Impact of dual lipid-lowering strategy with ezetimibe and atorvastatin on coronary plaque regression in patients with percutaneous coronary intervention: the multicenter randomized PRECISE-IVUS trial. J. Am. Coll. Cardiol. 66, 495–507 (2015).
Ueda, Y. et al. Effect of ezetimibe on stabilization and regression of intracoronary plaque — the ZIPANGU study. Circ. J. 11, 1611–1619 (2017).
Hougaard, M. et al. Influence of ezetimibe in addition to high-dose atorvastatin therapy on plaque composition in patients with ST-segment elevation myocardial infarction assessed by serial: Intravascular ultrasound with iMap: the OCTIVUS trial. Cardiovasc. Revasc. Med. 18, 110–117 (2017).
Hibi, K. et al. Effects of ezetimibe-statin combination therapy on coronary atherosclerosis in acute coronary syndrome. Circ. J. 82, 757–766 (2018).
Lloyd-Jones, D. M. et al. 2022 ACC expert consensus decision pathway on the role of nonstatin therapies for LDL-cholesterol lowering in the management of atherosclerotic cardiovascular disease risk: a report of the American College of Cardiology Solution Set Oversight Committee. J. Am. Coll. Cardiol. 80, 1366–1418 (2022).
Sabatine, M. S. et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N. Engl. J. Med. 18, 1713–1722 (2017).
O’Donoghue, M. L. et al. Long-term evolocumab in patients with established atherosclerotic cardiovascular disease. Circulation 146, 1109–1119 (2022).
Schwartz, G. G. et al. Alirocumab and cardiovascular outcomes after acute coronary syndrome. N. Engl. J. Med. 379, 2097–2107 (2018).
Blom, D. J. et al. Efficacy and safety of alirocumab in adults with homozygous familial hypercholesterolemia: the ODYSSEY HoFH trial. J. Am. Coll. Cardiol. 76, 131–132 (2020).
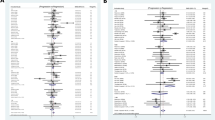
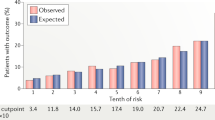
Nicholls, S. J. et al. Effect of evolocumab on progression of coronary disease in statin-treated patients: the GLAGOV randomized clinical trial. JAMA 316, 2373–2384 (2016).
Nicholls, S. J. et al. Effect of evolocumab on coronary plaque composition. J. Am. Coll. Cardiol. 72, 2012–2021 (2018).
Raber, L. et al. Effect of alirocumab added to high-intensity statin therapy on coronary atherosclerosis in patients with acute myocardial infarction: the PACMAN-AMI randomized clinical trial. JAMA 327, 1771–1781 (2022).
Biccire, F. G. et al. Concomitant coronary atheroma regression and stabilization in response to lipid-lowering therapy. J. Am. Coll. Cardiol. 82, 1737–1747 (2023).
Nicholls, S. J. et al. Effect of evolocumab on coronary plaque phenotype and burden in statin-treated patients following myocardial infarction. JACC Cardiovasc. Imaging 15, 1308–1321 (2022).
Ako, J. et al. Effect of alirocumab on coronary atheroma volume in Japanese patients with acute coronary syndrome — the ODYSSEY J-IVUS trial. Circ. J. 25, 2025–2033 (2019).
Ray, K. K. et al. Two phase 3 trials of inclisiran in patients with elevated LDL cholesterol. N. Engl. J. Med. 382, 1507–1519 (2020).
Nissen, S. E. et al. Bempedoic acid and cardiovascular outcomes in statin-intolerant patients. N. Engl. J. Med. 388, 1353–1364 (2023).
Raal, F. J. et al. Familial hypercholesterolemia treatments: guidelines and new therapies. Atherosclerosis 277, 483–492 (2018).
Wang, A. et al. Systematic review of low-density lipoprotein cholesterol apheresis for the treatment of familial hypercholesterolemia. J. Am. Heart Assoc. 5, e003294 (2016).
Lau, F. D. & Guigliano, R. P. Lipoprotein(a) and its significance in cardiovascular disease: a review. JAMA Cardiol. 7, 760–769 (2022).
Matsuzaki, M. et al. Intravascular ultrasound evaluation of coronary plaque regression by low density lipoprotein-apheresis in familial hypercholesterolemia: the Low Density Lipoprotein-Apheresis Coronary Morphology and Reserve Trial (LACMART). J. Am. Coll. Cardiol. 40, 220–227 (2002).
Banerjee, S. et al. Plaque regression and endothelial progenitor cell mobilization with intensive lipid elimination regimen (PREMIER). Circ. Cardiovasc. Interv. 13, e008933 (2020).
Wong, N. D. et al. Residual atherosclerotic cardiovascular disease risk in statin-treated adults: the Multi-Ethnic Study of Atherosclerosis. J. Clin. Lipidol. 11, 1223–1233 (2017).
Matsuura, Y., Kanter, J. E. & Bornfeldt, K. E. Highlighting residual atherosclerotic cardiovascular disease risk. Arterioscler. Thromb. Vasc. Biol. 39, e1–e9 (2019).
Gurdasani, D. et al. Lipoprotein(a) and risk of coronary, cerebrovascular, and peripheral artery disease: the EPIC-Norfolk prospective population study. Arterioscler. Thromb. Vasc. Biol. 32, 3058–3065 (2012).
Lee, J. M. S. et al. Effects of high-dose modified-release nicotinic acid on atherosclerosis and vascular function: a randomized, placebo-controlled, magnetic resonance imaging study. J. Am. Coll. Cardiol. 19, 1787–1794 (2009).
The AIM-HIGH Investigators. Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N. Engl. J. Med. 365, 2255–2267 (2011).
The HPS2-THRIVE Collaborative Group. Effects of extended-release niacin with laropiprant in high-risk patients. N. Engl. J. Med. 371, 203–212 (2014).
Barter, P. J. et al. Effects of torcetrapib in patients at high risk for coronary events. N. Engl. J. Med. 357, 2109–2122 (2007).
Forrest, M. J. et al. Torcetrapib-induced blood pressure elevation is independent of CETP inhibition and is accompanied by increased circulating levels of aldosterone. Br. J. Pharmacol. 154, 1465–1473 (2008).
Vergeer, M. et al. Cholesteryl ester transfer protein inhibitor torcetrapib and off-target toxicity: a pooled analysis of the rating atherosclerotic disease change by imaging with a new CETP inhibitor (RADIANCE) trials. Circulation 118, 2515–2522 (2008).
Nissen, S. E. et al. Effect of torcetrapib on the progression of coronary atherosclerosis. N. Engl. J. Med. 356, 1304–1316 (2007).
Schwartz, G. G. et al. Effects of dalcetrapib in patients with a recent acute coronary syndrome. N. Engl. J. Med. 367, 2089–2099 (2012).
Lincoff, A. M. et al. Evacetrapib and cardiovascular outcomes in high-risk vascular disease. N. Engl. J. Med. 376, 1933–1942 (2017).
Bowman, L. et al. Effects of anacetrapib in patients with atherosclerotic vascular disease. N. Engl. J. Med. 377, 1217–1227 (2017).
Ballantyne, C. M. et al. Obicetrapib plus ezetimibe as an adjunct to high-intensity statin therapy: a randomized phase 2 trial. J. Clin. Lipidol. 17, 491–503 (2023).
Angelantonio, E. D. et al. Major lipids, apolipoproteins, and risk of vascular disease. JAMA 302, 1993–2000 (2009).
Tardif, J. et al. Effects of the high-density lipoprotein mimetic agent CER-001 on coronary atherosclerosis in patients with acute coronary syndromes: a randomized trial. Eur. Heart J. 35, 3277–3286 (2014).
Nicholls, S. J. et al. Effect of serial infusions of CER-001, a pre-β high-density lipoprotein mimetic, on coronary atherosclerosis in patients following acute coronary syndromes in the CER-001 Atherosclerosis Regression Acute Coronary Syndrome Trial: a randomized clinical trial. JAMA Cardiol. 3, 815–822 (2018).
Nicholls, S. J. et al. Effect of infusion of high-density lipoprotein mimetic containing recombinant apolipoprotein A-I Milano on coronary disease in patients with an acute coronary syndrome in the MILANO-PILOT trial: a randomized clinical trial. JAMA Cardiol. 3, 806–814 (2018).
Nissen, S. E. et al. Effect of recombinant ApoA-I Milano on coronary atherosclerosis in patients with acute coronary syndromes: a randomized controlled trial. JAMA 290, 2292–2300 (2003).
Tardif, J. et al. Effects of reconstituted high-density lipoprotein infusions on coronary atherosclerosis: a randomized controlled trial. JAMA 297, 1675–1682 (2007).
Virani, S. S. et al. 2021 ACC expert consensus decision pathway on the management of ASCVD risk reduction in patients with persistent hypertriglyceridemia: a report of the American College of Cardiology Solution Set Oversight Committee. J. Am. Coll. Cardiol. 78, 960–993 (2021).
Pradhan, A. S. et al. Triglyceride lowering with pemafibrate to reduce cardiovascular risk. N. Engl. J. Med. 387, 1923–1934 (2022).
Budoff, M. J. et al. Effect of icosapent ethyl on progression of coronary atherosclerosis in patients with elevated triglycerides on statin therapy: final results of the EVAPORATE trial. Eur. Heart J. 41, 3925–3932 (2020).
Ridker, P. M. et al. Effects of randomized treatment with icosapent ethyl and a mineral oil comparator on interleukin-1β, interleukin-6, C-reactive protein, oxidized low-density lipoprotein cholesterol, homocysteine, lipoprotein(a), and lipoprotein-associated phospholipase A1: A REDUCE-IT biomarker substudy. Circulation 146, 372–379 (2022).
Lakshmanan, S. et al. Comparison of mineral oil and non-mineral oil placebo on coronary plaque progression by coronary computed tomography angiography. Cardiovasc. Res. 116, 479–482 (2020).
Watanabe, T. et al. A randomized controlled trial of eicosapentaenoic acid in patients with coronary heart disease on statins. J. Cardiol. 70, 537–544 (2017).
Reyes-Soffer, G. et al. Lipoprotein(a): a genetically determined, causal, and prevalent risk factor for atherosclerotic cardiovascular disease: a scientific statement from the American Heart Association. Arterioscler. Thromb. Vasc. Biol. 42, e48–e60 (2022).
Kaiser, Y. et al. Association of lipoprotein(a) with atherosclerotic plaque progression. J. Am. Coll. Cardiol. 79, 223–233 (2022).
Kronenberg, F. et al. Frequent questions and responses on the 2022 lipoprotein(a) consensus statement of the European Atherosclerosis Society. Atherosclerosis 374, 107–120 (2023).
US National Library of Medicine. ClinicalTrials.gov https://www.clinicaltrials.gov/study/NCT04023552 (2023).
US National Library of Medicine. ClinicalTrials.gov https://www.clinicaltrials.gov/study/NCT05581303 (2023).
Kovarnik, T. et al. Plaque volume and plaque risk profile in diabetic vs. non-diabetic patients undergoing lipid-lowering therapy: a study based on 3D intravascular ultrasound and virtual histology. Cardiovasc. Diabetol. 16, 156 (2017).
Fukushima, Y. et al. Relationship between advanced glycation end products and plaque progression in patients with acute coronary syndrome: the JAPAN-ACS sub-study. Cardiovasc. Diabetol. 12, 5 (2013).
Nissen, S. E. et al. Comparison of pioglitazone vs glimepiride on progression of coronary atherosclerosis in patients with type 2 diabetes: the PERISCOPE randomized controlled trial. JAMA 299, 1561–1573 (2008).
Nicholls, S. J. et al. Lowering the triglyceride/high-density lipoprotein cholesterol ratio is associated with the beneficial impact of pioglitazone on progression of coronary atherosclerosis in diabetic patients: insights from the PERISCOPE (Pioglitazone Effect on Regression of Intravascular Sonographic Coronary Obstruction Prospective Evaluation) study. J. Am. Coll. Cardiol. 57, 153–159 (2011).
Gerstein, H. C. et al. Effect of rosiglitazone on progression of coronary atherosclerosis in patients with type 2 diabetes mellitus and coronary artery disease: the assessment on the prevention of progression by rosiglitazone on atherosclerosis in diabetes patients with cardiovascular history trial. Circulation 121, 1176–1187 (2010).
Sardu, C. et al. SGLT2-inhibitors effects on the coronary fibrous cap thickness and MACEs in diabetic patients with inducible myocardial ischemia and multi vessels non-obstructive coronary artery stenosis. Cardiovasc. Diabetol. 22, 80 (2023).
Nissen, S. E. et al. Effect of antihypertensive agents on cardiovascular events in patients with coronary disease and normal blood pressure — the CAMELOT study: a randomized controlled trial. JAMA 292, 2217–2225 (2004).
Hirohata, A. et al. Impact of olmesartan on progression of coronary atherosclerosis a serial volumetric intravascular ultrasound analysis from the OLIVUS (impact of OLmesarten on progression of coronary atherosclerosis: evaluation by intravascular ultrasound) trial. J. Am. Coll. Cardiol. 55, 976–982 (2010).
Rodriguez-Granillo, G. A. et al. Long-term effect of perindopril on coronary atherosclerosis progression (from the perindopril’s prospective effect on coronary atherosclerosis by angiography and intravascular ultrasound evaluation [PERSPECTIVE] study). Am. J. Cardiol. 100, 159–163 (2007).
Nicholls, S. J. et al. Effect of aliskiren on progression of coronary disease in patients with prehypertension: the AQUARIUS randomized clinical trial. JAMA 310, 1135–1144 (2013).
Nidorf, S. M. et al. Colchicine in patients with chronic coronary disease. N. Engl. J. Med. 383, 1838–1847 (2020).
Tardif, J. et al. Efficacy and safety of low-dose colchicine after myocardial infarction. N. Engl. J. Med. 381, 2497–2505 (2019).
Vaidya, K. et al. Colchicine therapy and plaque stabilization in patients with acute coronary syndrome: a CT coronary angiography study. JACC Cardiovasc. Imaging 11, 305–315 (2018).
Budoff, M. J. et al. Testosterone treatment and coronary plaque volume in older men with low testosterone. JAMA 317, 708–716 (2017).
Nissen, S. E. et al. Effect of rimonabant on progression of atherosclerosis in patients with abdominal obesity and coronary artery disease: the STRADIVARIUS randomized controlled trial. JAMA 299, 1547–1560 (2008).
Nicholls, S. J. et al. Effect of the BET protein inhibitor, RVX-208, on progression of coronary atherosclerosis: results of the phase 2b, randomized, double-blind, multicenter, ASSURE trial. Am. J. Cardiovasc. Drugs 16, 55–65 (2016).
Ko, Y. et al. Effects of combination therapy with cilostazol and probucol versus monotherapy with cilostazol on coronary plaque, lipid and biomarkers: SECURE study, a double-blind randomized controlled clinical trial. J. Atheroscler. Thromb. 21, 816–830 (2014).
Tardif, J. et al. Effects of the antioxidant succinobucol (AGI-1067) on human atherosclerosis in a randomized clinical trial. Atherosclerosis 197, 480–486 (2008).
Eikelboom, J. W. et al. Rivaroxaban with or without aspirin in stable cardiovascular disease. N. Engl. J. Med. 377, 1319–1330 (2017).
Lee, J. et al. Randomized trial of rivaroxaban versus warfarin in the evaluation of progression of coronary atherosclerosis. Am. Heart J. 206, 127–130 (2018).
Author information
Authors and Affiliations
Contributions
Both authors contributed substantially to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Cardiology thanks William Boden, Matthew Budoff, Hector Garcia-Garcia and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sarraju, A., Nissen, S.E. Atherosclerotic plaque stabilization and regression: a review of clinical evidence. Nat Rev Cardiol (2024). https://doi.org/10.1038/s41569-023-00979-8
Accepted:
Published:
DOI: https://doi.org/10.1038/s41569-023-00979-8
This article is cited by
-
The serum soluble ASGR1 concentration is elevated in patients with coronary artery disease and is associated with inflammatory markers
Lipids in Health and Disease (2024)