Abstract
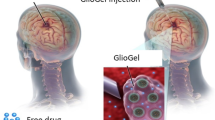
The poor transport of molecular and nanoscale agents through the blood–brain barrier together with tumour heterogeneity contribute to the dismal prognosis in patients with glioblastoma multiforme. Here, a biodegradable implant (μMESH) is engineered in the form of a micrometre-sized poly(lactic-co-glycolic acid) mesh laid over a water-soluble poly(vinyl alcohol) layer. Upon poly(vinyl alcohol) dissolution, the flexible poly(lactic-co-glycolic acid) mesh conforms to the resected tumour cavity as docetaxel-loaded nanomedicines and diclofenac molecules are continuously and directly released into the adjacent tumour bed. In orthotopic brain cancer models, generated with a conventional, reference cell line and patient-derived cells, a single μMESH application, carrying 0.75 mg kg−1 of docetaxel and diclofenac, abrogates disease recurrence up to eight months after tumour resection, with no appreciable adverse effects. Without tumour resection, the μMESH increases the median overall survival (∼30 d) as compared with the one-time intracranial deposition of docetaxel-loaded nanomedicines (15 d) or 10 cycles of systemically administered temozolomide (12 d). The μMESH modular structure, for the independent coloading of different molecules and nanomedicines, together with its mechanical flexibility, can be exploited to treat a variety of cancers, realizing patient-specific dosing and interventions.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
The data that support the plots within this paper and other findings of this study are available from the corresponding author upon reasonable request.
References
Delgado-Lopez, P. D. & Corrales-Garcia, E. M. Survival in glioblastoma: a review on the impact of treatment modalities. Clin. Transl. Oncol. 18, 1062–1071 (2016).
Omuro, A. & DeAngelis, L. M. Glioblastoma and other malignant gliomas: a clinical review. JAMA 310, 1842–1850 (2013).
Stupp, R. et al. Maintenance therapy with tumor-treating fields plus temozolomide vs temozolomide alone for glioblastoma: a randomized clinical trial. JAMA 314, 2535–2543 (2015).
Delgado‐Martín, B. & Medina, M. Á. Advances in the knowledge of the molecular biology of glioblastoma and its impact in patient diagnosis, stratification, and treatment. Adv. Sci. 7, 1902971 (2020).
Jackson, C. M., Choi, J. & Lim, M. Mechanisms of immunotherapy resistance: lessons from glioblastoma. Nat. Immunol. 20, 1100–1109 (2019).
Stupp, R. et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N. Engl. J. Med. 352, 987–996 (2005).
Aldape, K. et al. Challenges to curing primary brain tumours. Nat. Rev. Clin. Oncol. 16, 509–520 (2019).
Giese, A., Bjerkvig, R., Berens, M. E. & Westphal, M. Cost of migration: invasion of malignant gliomas and implications for treatment. J. Clin. Oncol. 21, 1624–1636 (2003).
Stummer, W. et al. Fluorescence-guided surgery with 5-aminolevulinic acid for resection of malignant glioma: a randomised controlled multicentre phase III trial. Lancet Oncol. 7, 392–401 (2006).
Lemee, J. M., Clavreul, A. & Menei, P. Intratumoral heterogeneity in glioblastoma: don’t forget the peritumoral brain zone. Neuro-Oncol. 17, 1322–1332 (2015).
D’Amico, R. S., Englander, Z. K., Canoll, P. & Bruce, J. N. Extent of resection in glioma—a review of the cutting edge. World Neurosurg. 103, 538–549 (2017).
Tanaka, S., Louis, D. N., Curry, W. T., Batchelor, T. T. & Dietrich, J. Diagnostic and therapeutic avenues for glioblastoma: no longer a dead end? Nat. Rev. Clin. Oncol. 10, 14–26 (2013).
Ballabh, P., Braun, A. & Nedergaard, M. The blood–brain barrier: an overview: structure, regulation, and clinical implications. Neurobiol. Dis. 16, 1–13 (2004).
Lesniak, M. S. & Brem, H. Targeted therapy for brain tumours. Nat. Rev. Drug Discov. 3, 499–508 (2004).
Arvanitis, C. D., Ferraro, G. B. & Jain, R. K. The blood–brain barrier and blood–tumour barrier in brain tumours and metastases. Nat. Rev. Cancer 20, 26–41 (2020).
The Cancer Genome Atlas Research Network Comprehensive genomic characterization defines human glioblastoma genes and core pathways. Nature 455, 1061–1068 (2008).
Network, T. C. Corrigendum: Comprehensive genomic characterization defines human glioblastoma genes and core pathways. Nature 494, 506 (2013).
Verhaak, R. G. et al. Integrated genomic analysis identifies clinically relevant subtypes of glioblastoma characterized by abnormalities in PDGFRA, IDH1, EGFR, and NF1. Cancer Cell 17, 98–110 (2010).
Wang, Q. et al. Tumor evolution of glioma-intrinsic gene expression subtypes associates with immunological changes in the microenvironment. Cancer Cell 33, 152 (2018).
Osuka, S. & Van Meir, E. G. Overcoming therapeutic resistance in glioblastoma: the way forward. J. Clin. Investig. 127, 415–426 (2017).
Neftel, C. et al. An integrative model of cellular states, plasticity, and genetics for glioblastoma. Cell 178, 835–849 (2019).
Chen, J. et al. A restricted cell population propagates glioblastoma growth after chemotherapy. Nature 488, 522–526 (2012).
Lee, A. et al. Spherical polymeric nanoconstructs for combined chemotherapeutic and anti-inflammatory therapies. Nanomedicine 12, 2139–2147 (2016).
Lam, F. C. et al. Enhanced efficacy of combined temozolomide and bromodomain inhibitor therapy for gliomas using targeted nanoparticles. Nat. Commun. 9, 1991 (2018).
Tamborini, M. et al. A combined approach employing chlorotoxin-nanovectors and low dose radiation to reach infiltrating tumor niches in glioblastoma. ACS Nano 10, 2509–2520 (2016).
Prados, M. D. et al. Phase II study of erlotinib plus temozolomide during and after radiation therapy in patients with newly diagnosed glioblastoma multiforme or gliosarcoma. J. Clin. Oncol. 27, 579–584 (2009).
Samal, J., Rebelo, A. L. & Pandit, A. A window into the brain: tools to assess pre-clinical efficacy of biomaterials-based therapies on central nervous system disorders. Adv. Drug Deliv. Rev. 148, 68–145 (2019).
Randall, E. C. et al. Integrated mapping of pharmacokinetics and pharmacodynamics in a patient-derived xenograft model of glioblastoma. Nat. Commun. 9, 4904 (2018).
Foley, C. P. et al. Intra-arterial delivery of AAV vectors to the mouse brain after mannitol mediated blood brain barrier disruption. J. Control. Release 196, 71–78 (2014).
Zou, Y. et al. Effective and targeted human orthotopic glioblastoma xenograft therapy via a multifunctional biomimetic nanomedicine. Adv. Mater. 30, e1803717 (2018).
Timbie, K. F., Mead, B. P. & Price, R. J. Drug and gene delivery across the blood–brain barrier with focused ultrasound. J. Control. Release 219, 61–75 (2015).
Aryal, M., Arvanitis, C. D., Alexander, P. M. & McDannold, N. Ultrasound-mediated blood–brain barrier disruption for targeted drug delivery in the central nervous system. Adv. Drug Deliv. Rev. 72, 94–109 (2014).
May, J. N. et al. Multimodal and multiscale optical imaging of nanomedicine delivery across the blood–brain barrier upon sonopermeation. Theranostics 10, 1948–1959 (2020).
Johnsen, K. B. et al. Modulating the antibody density changes the uptake and transport at the blood–brain barrier of both transferrin receptor-targeted gold nanoparticles and liposomal cargo. J. Control. Release 295, 237–249 (2019).
Lajoie, J. M. & Shusta, E. V. Targeting receptor-mediated transport for delivery of biologics across the blood–brain barrier. Annu. Rev. Pharmacol. Toxicol. 55, 613–631 (2015).
Bu, L. L. et al. Advances in drug delivery for post-surgical cancer treatment. Biomaterials 219, 119182 (2019).
Vogelbaum, M. A. & Aghi, M. K. Convection-enhanced delivery for the treatment of glioblastoma. Neuro-Oncol. 17, ii3–ii8 (2015).
Brem, H. et al. Placebo-controlled trial of safety and efficacy of intraoperative controlled delivery by biodegradable polymers of chemotherapy for recurrent gliomas. Lancet 345, 1008–1012 (1995).
Bota, D. A., Desjardins, A., Quinn, J. A., Affronti, M. L. & Friedman, H. S. Interstitial chemotherapy with biodegradable BCNU (Gliadel) wafers in the treatment of malignant gliomas. Ther. Clin. Risk Manag. 3, 707–715 (2007).
Shapira-Furman, T. et al. Biodegradable wafers releasing temozolomide and carmustine for the treatment of brain cancer. J. Control. Release 295, 93–101 (2019).
Song, E. et al. Surface chemistry governs cellular tropism of nanoparticles in the brain. Nat. Commun. 8, 15322 (2017).
Jahangiri, A. et al. Convection-enhanced delivery in glioblastoma: a review of preclinical and clinical studies. J. Neurosurg. 126, 191–200 (2017).
Conde, J., Oliva, N., Zhang, Y. & Artzi, N. Local triple-combination therapy results in tumour regression and prevents recurrence in a colon cancer model. Nat. Mater. 15, 1128–1138 (2016).
Talebian, S. et al. Biopolymers for antitumor implantable drug delivery systems: recent advances and future outlook. Adv. Mater. 30, e1706665 (2018).
Jain, A. et al. Guiding intracortical brain tumour cells to an extracortical cytotoxic hydrogel using aligned polymeric nanofibres. Nat. Mater. 13, 308–316 (2014).
Hosseinzadeh, R. et al. A drug‐eluting 3D‐printed mesh (GlioMesh) for management of glioblastoma. Adv. Ther. 2, 1900113 (2019).
Han, D. et al. Multi-layered core–sheath fiber membranes for controlled drug release in the local treatment of brain tumor. Sci. Rep. 9, 17936 (2019).
Ramachandran, R. et al. Theranostic 3-dimensional nano brain-implant for prolonged and localized treatment of recurrent glioma. Sci. Rep. 7, 43271 (2017).
Wang, C. et al. In situ formed reactive oxygen species-responsive scaffold with gemcitabine and checkpoint inhibitor for combination therapy. Sci. Transl. Med. 10, eaan3682 (2018).
Wang, T. et al. A cancer vaccine-mediated postoperative immunotherapy for recurrent and metastatic tumors. Nat. Commun. 9, 1532 (2018).
Lee, J. et al. Flexible, sticky, and biodegradable wireless device for drug delivery to brain tumors. Nat. Commun. 10, 5205 (2019).
Theruvath, J. et al. Locoregionally administered B7-H3-targeted CAR T cells for treatment of atypical teratoid/rhabdoid tumors. Nat. Med. 26, 712–719 (2020).
Donovan, L. K. et al. Locoregional delivery of CAR T cells to the cerebrospinal fluid for treatment of metastatic medulloblastoma and ependymoma. Nat. Med. 26, 720–731 (2020).
Sahoo, S. K., Panyam, J., Prabha, S. & Labhasetwar, V. Residual polyvinyl alcohol associated with poly (d,l-lactide-co-glycolide) nanoparticles affects their physical properties and cellular uptake. J. Control. Release 82, 105–114 (2002).
Zweers, M. L., Engbers, G. H., Grijpma, D. W. & Feijen, J. In vitro degradation of nanoparticles prepared from polymers based on dl-lactide, glycolide and poly(ethylene oxide). J. Control. Release 100, 347–356 (2004).
Skog, J. et al. Glioblastoma microvesicles transport RNA and proteins that promote tumour growth and provide diagnostic biomarkers. Nat. Cell Biol. 10, 1470–1476 (2008).
Dancy, J. G. et al. Non-specific binding and steric hindrance thresholds for penetration of particulate drug carriers within tumor tissue. J. Control. Release 238, 139–148 (2016).
Kalb, E. & Engel, J. Binding and calcium-induced aggregation of laminin onto lipid bilayers. J. Biol. Chem. 266, 19047–19052 (1991).
Wong, C. et al. Multistage nanoparticle delivery system for deep penetration into tumor tissue. Proc. Natl Acad. Sci. USA 108, 2426–2431 (2011).
Narayanan, A. et al. The proneural gene ASCL1 governs the transcriptional subgroup affiliation in glioblastoma stem cells by directly repressing the mesenchymal gene NDRG1. Cell Death Differ. 26, 1813–1831 (2019).
Acknowledgements
This project was partially supported by the European Research Council under the European Union’s Seventh Framework Programme (FP7/2007-2013)/ERC grant agreement 616695–POTENT (P.D.), and by the European Union’s Horizon 2020 Research and Innovation Programme under the Marie Sklodowska-Curie grant agreement 754490–MINDED (P.D.). We thank the laboratory of D. De Pietri Tonelli for providing the U-87 MG GFP+ cells. We thank the Clean Room Facility in IIT and M. Francardi. P.D. and G.A.G. are grateful to Professor Sanjiv Sam Gambhir of Stanford University for catalysing and supporting the collaboration between their laboratories. We dedicate this work to the memory and legacy of Professor Sanjiv Sam Gambhir, who passed away on 18 June 2020.
Author information
Authors and Affiliations
Contributions
D.D.M. and P.D. conceived the idea and designed the experiments. D.D.M. realized all the different platforms used, performed all the in vitro experiments, acquired optical and electron microscopy images, analysed all the data and performed statistical analyses. A.L.P. performed all the in vivo experiments. R.P. conducted the histological analyses and sample preparation. F.M. helped in the realization of the orthotopic tumour models. T.C. prepared samples for CLEM study. F.P. and R.S. helped with the in vivo experiments. A.L.G. and R.G. provided patient-derived GBM cells, transfected the cells with Luc+ and helped in developing the tumour model, and A.L.G. helped with cell inoculation. M.F. synthesized lipid-Cy5. R.M. performed cryo-EM analyses. A.A. performed liquid chromatography–mass spectrometry analyses. C.W. and G.A.G. performed time-course penetration experiments with µSPNs. D.D.M., P.D. and A.L.P. wrote the manuscript. P.D. supervised the whole project.
Corresponding author
Ethics declarations
Competing interests
D.D.M. and P.D. are the coinventors on the pending patent WO2019193524A1—‘An implantable device for localized drug delivery, uses thereof and a manufacturing method thereof’ filed by the Fondazione Istituto Italiano di Tecnologia. The remaining authors declare no competing interests.
Additional information
Peer review information Nature Nanotechnology thanks Manish Aghi, Ravi Bellamkonda and Abhay Pandit for their contribution to the peer review of this work.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Materials and Methods, Results and Discussion, and Figs. 1–40.
Rights and permissions
About this article
Cite this article
Di Mascolo, D., Palange, A.L., Primavera, R. et al. Conformable hierarchically engineered polymeric micromeshes enabling combinatorial therapies in brain tumours. Nat. Nanotechnol. 16, 820–829 (2021). https://doi.org/10.1038/s41565-021-00879-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41565-021-00879-3
This article is cited by
-
Breaking the boundaries of biological penetration depth: X-ray luminescence in light theranostics
Science China Chemistry (2024)
-
Chemotactic nanomotor for multimodal combined therapy of glioblastoma
Science China Chemistry (2024)
-
A nitric-oxide driven chemotactic nanomotor for enhanced immunotherapy of glioblastoma
Nature Communications (2023)
-
Local delivery of doxorubicin prodrug via lipid nanocapsule–based hydrogel for the treatment of glioblastoma
Drug Delivery and Translational Research (2023)
-
3D printed hydrogel scaffolds combining glutathione depletion-induced ferroptosis and photothermia-augmented chemodynamic therapy for efficiently inhibiting postoperative tumor recurrence
Journal of Nanobiotechnology (2022)