Abstract
Patients with schizophrenia (SCZ) smoke up to three times more than general people. However, there are conflicting results regarding the relationship between tobacco smoke and clinical symptom severity in SCZ. The aim of this study was to assess the impact of smoking on clinical symptoms after antipsychotic treatment in a 12-week cohort study after controlling for confounding factors. One hundred and forty-five male patients with drug-naïve first-episode (DNFE) SCZ received antipsychotic monotherapy for 12 weeks. Symptom severity was assessed at baseline and at week 12 by the Positive and Negative Syndrome Scale (PANSS). We found no differences in clinical symptoms among male smokers with SCZ compared with male nonsmokers. However, male smokers showed greater improvement in negative symptoms after 12 weeks of treatment, controlling for age, years of education, onset age, and baseline body mass index (BMI). Our study showed that after 12 weeks of treatment with antipsychotics, male smokers showed greater improvement in negative symptoms than male nonsmokers.
Similar content being viewed by others
Introduction
Schizophrenia (SCZ) is a chronic and severe mental disorder that affects 1% of the world’s population. People with schizophrenia experience hallucinations, and disorganized thinking, and are prone to false and paranoid beliefs1. The symptoms of SCZ are classified as positive symptoms and negative symptoms.
The negative symptoms are defined as a reduction or lack of normal behaviors associated with normal functioning, such as social functioning, motivation, and personal expression. Negative symptoms can be primary symptoms inherent to the underlying pathophysiology of SCZ or secondary symptoms related to psychiatric or medical comorbidities, or adverse treatment effects2. The negative symptom domain consists of 5 key constructs: blunted affect, alogia (reduction in the number of words spoken), avolition (reduced goal-directed activity due to decreased motivation), asociality, and anhedonia (reduced experience of pleasure)3,4. Negative symptoms are one of the core symptoms of SCZ and are strongly associated with long-term morbidity and poor functional outcomes in patients5,6. While positive symptoms can often be effectively improved with available antipsychotic medications, current treatment options for negative symptoms are relatively limited in effectiveness, and they remain an unmet medical need7. Interestingly, some studies have shown evidence of fewer negative symptoms in SCZ patients who smoke, which contributes to the self-treatment of negative symptoms8.
Patients with SCZ have a high rate of smoking compared to the general population9. Previous studies have reported a smoking rate of ~60% in SCZ patients and a strong association between smoking and SCZ (OR = 6:0; 95% CI, 3.0–12.0)10,11. In particular, studies have shown that patients with SCZ are also more likely to be heavy smokers compared to the general population12. A study by our group showed that in China, the prevalence of heavy smoking was higher in SCZ patients (28.3%) than in the general population (14.5%)13.
Previous studies have shown that smoking can act as self-medication for clinical symptoms of SCZ through the neurobiological basis of nicotine14. A meta-analysis also reported that nicotine could enhance cognitive functioning, including motor abilities, attention and immediate memory15. Longitudinal studies have also reported that smoking may be an independent protective factor for the development of SCZ16. Nicotine is the main addictive component of cigarettes17,18, which has been reported to ameliorate the abnormalities in dopaminergic, glutamatergic, and GABAergic pathways19 and has been linked to the mechanism of symptom improvements.
However, the link between smoking and SCZ has been a complex issue. Some studies reported that smoking was associated with more severe negative symptoms in patients with psychiatric disorders20. A cross-sectional study of SCZ patients showed that mildly dependent smokers had more severe negative symptoms than nonsmokers21. A 4 to 16-year follow-up study including 14,248 healthy adolescents without any psychiatric disorder showed that those who smoked <9 cigarettes per day were 1.38 times more likely to be later hospitalized for SCZ and those who smoked >10 cigarettes per day were 2.28 times more likely to develop SCZ than nonsmokers (95% CI = 1:19–4.34)22. Another cohort study of 1,413,849 women and 233,879 men with first-episode SCZ showed a hazard ratio of 3.5 for women and 3.8 for men for smoking23, suggesting that cigarette smoking causes SCZ. Some confounding factors that were not controlled for, such as antipsychotic types, disease duration and demographic characteristics of patients could explain the discrepancy in a variety of studies.
To better understand the relationship between smoke and SCZ, in this study, we recruited male drug-naïve first-episode (DNFE) patients to exclude the potential effects of antipsychotic medication, duration of illness and sex. In clinical studies in the SCZ, patients with DNFE are particularly advantageous because the effects of confounding factors, including medication efficacy, duration of illness, and physical comorbidity, can be minimized24. In addition, to control for the effects of different antipsychotics, all patients in our study received antipsychotics as monotherapy. We hypothesized that smoking might alleviate negative symptoms in SCZ patients after treatment with antipsychotic monotherapy in male patients with DNFE SCZ. Because smoking is substantially more common among Chinese men than in women with SCZ25, as well as sex differences in smoking behaviors26, we recruited only male patients. Therefore, in this study, we aimed to compare the severity of negative symptoms in male smokers and nonsmokers before and after 12 weeks of treatment and to investigate whether smoking might affect drug efficacy.
Materials and methods
Subjects
One hundred and forty-five male patients with SCZ were recruited from Hebei Province Veterans hospital, Beijing Huilongguan Hospital and Wenzhou kangning hospital. Of all the 145 male patients, 60 were smokers and 85 were nonsmokers. Inclusion and exclusion criteria were described in a previous study27. Male first-episode inpatients, aged 16–45 years, diagnosed with SCZ by SCID-IV, were recruited for this study. Patients had a disease duration of no more than 5 years, cumulative duration of antipsychotic medication of no more than 2 weeks, and no significant medical comorbidities. The first episode was defined as a previous study28. Patients were excluded from this study if they had any other current categorical diagnosis of psychiatric disorders. All patients were treated with a flexible dose of antipsychotics for 12 weeks. In this 12-week observational study, patients were hospitalized and nurses monitored adherence to treatment.
The study protocol was approved by the Ethics Committee of Beijing Huilongguan Hospital, and written informed consent was obtained from all patients.
Assessment
All patients were treated with flexible doses of oral antipsychotics for 12 weeks. The study consisted of three visits, conducted on day 1 (visit 1, screening), day 1 (visit 2, assessment of baseline), and at week 12 or after early discontinuation of the trial drug (visit 3, assessment of follow-up).
Six experienced psychiatrists assessed the severity of psychiatric symptoms using the Positive and Negative Syndrome Scale (PANSS)29. The PANSS scale was assessed at baseline and at week 12. The primary outcome was the change from baseline in the PANSS total score or subscores at week 12. After training, the repeated assessment showed that the inter-observer correlation coefficient was maintained at >0.8 for the PANSS total score.
Statistical analysis
For patients who discontinued this clinical trial medication, the last observation carried forward (LOCF) was used. Analysis of variance (ANOVA) was performed to compare baseline demographic characteristics of the SCZ in smokers and nonsmokers. A repeated measures ANOVA was performed to analyze the different changes in PANSS total score and their subscale scores between smokers and non-smokers at baseline and the LOCF endpoint at week 12. Pearson correlation coefficients between symptom changes and demographic characteristics were calculated for smokers and nonsmokers, respectively. p values were adjusted using Bonferroni correction (B-adjusted p) as reported in previous studies30,31,32,33. Linear regression analyses were performed to identify factors associated with symptom improvement in SCZ patients. Regression analyses were performed to determine the relative contribution of smoking and other demographic variables (e.g., age, years of education, baseline BMI and onset age) to explain the variance in negative symptom improvement.
All data were analyzed with SPSS statistical analysis software (version 22.0; SPSS Inc., Chicago, IL), and significance thresholds were determined at p < 0.05.
Results
At baseline, male smokers with SCZ were older, had a later age of onset and had a shorter education year than male nonsmokers with SCZ (all p < 0.05) (Table 1). Correlation analysis showed that clinical symptoms at baseline were associated with age, BMI, age at onset, and years of education (all p < 0.05). However, we did not find any differences in positive, negative symptoms, general psychopathology and PANSS total scores between smokers and nonsmokers in male patients with SCZ (p = 0.71, p = 0.11, p = 0.38, and p = 0.92).
After 12 weeks of treatment, the PANSS total score and each subscale score decreased significantly (all p < 0.01). The mean reduction in PANSS total score was 29.4 (95% CI 27.1–31.8) and the mean reductions in their subscale scores were 12.0 (95% CI 11.1–12.9) for positive symptoms, 4.9 (95% CI 4.2–5.6) for negative symptoms, and 12.7 (95% CI 11.5–13.9) for general psychopathology.
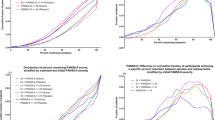
In addition, we found significant differences in the improvement of negative symptoms, general psychopathology and total scores between smokers and nonsmokers with SCZ (all p < 0.05) (Table 2 and Fig. 1). After Bonferroni correction, only the improvements in negative symptoms and total score were significant between smoking and nonsmoking patients (all B-adjusted p < 0.05). The further paired t-test indicated that smokers showed greater improvement in negative symptoms than non-smokers [5.5 (95% CI 3.6–7.4) vs. 3.7 (95% CI 2.6–4.7), p < 0.05]. Additionally, the number of cigarettes was positively associated with negative symptom improvement (r = 0.57, p < 0.001).
Further regression analysis confirmed that smoking was a predictor of improvement in negative symptoms in male patients with SCZ (Beta = 0.26, t = 2.7, p = 0.008) (adjusted R2 = 0.15).
Discussion
In this study, we found that male smokers with SCZ had greater clinical symptom improvement than male nonsmokers after 12 weeks of treatment, controlling for age, onset age, baseline BMI and education years.
Notably, in our study, negative symptoms of SCZ patients were slightly more severe at baseline. We hypothesize that the toxic component of cigarette plays a worsening role in clinical symptoms during the early and onset stages of SCZ, and therefore smokers per se have higher scores on negative symptom. A growing body of evidence suggests a common genetic predisposition and overlapping genetic roots for the development of smoking and SCZ34,35. The overlapping genetic risks combine with other risk factors for SCZ to exacerbate negative symptoms in smokers. However, the differences in negative symptoms between smokers and nonsmokers were not significant, although smokers had more than 2 points higher scores on negative symptoms than those of nonsmokers.
Consistent with our hypothesis, we found that after 12 weeks of treatment, male smokers with SCZ had more improvement in negative symptoms than male nonsmokers with SCZ. Many previous studies have focused on the relationship between smoking and the beneficial effects of antipsychotic medication on negative symptoms after treatment36,37,38,39. However, there is no consistent evidence that smoking has a beneficial effect on symptoms in SCZ40. In particular, there are few longitudinal and cohort studies on the relationship between smoking and clinical symptoms in DNFE patients with SCZ. Our prospective cohort study of first-episode drug naïve patients after a relatively short period (12 weeks) of treatment showed that smoking is associated with improvement in negative symptoms in male patients with SCZ. However, our results are inconsistent with previous studies, which reported that smoking was associated with more negative clinical outcomes41. These inconsistent results may be due to the type of antipsychotic, duration of treatment (12 weeks vs. 24 months), the severity of smoking dependence, and severity of psychotic symptoms at baseline.
Potential mechanisms for differential treatment response and symptom improvement between male smokers and non-smokers may be related to the interactive modulation of antipsychotics and smoking. The negative symptoms in SCZ may be the result of abnormalities in multiple neural networks (e.g., frontal-cortical-temporal, cortical-striatal; Millan et al.42). Current evidence supports the dopaminergic hypothesis as one of the pathophysiological hypotheses for negative symptoms in SCZ, which proposes that positive symptoms are the result of overactive dopaminergic neurotransmission in the limbic pathway, whereas negative symptoms are thought to be caused by low dopaminergic function in the frontal lobes and other limbic structures of the midbrain7,43. Nicotine is known to bind to nAChRs in the brain and alter neurotransmitter transmission44,45. Smoking can attenuate negative symptoms by reducing dopamine degradation and enhancing the effects of nicotine-mediated dopamine release in male SCZ patients, particularly in the inferior prefrontal cortex circuit40,46,47,48,49. Overall, our findings support a strong relationship between smoking and the improvement of negative symptoms after treatment with antipsychotics in male patients with first-episode SCZ. However, the number of smokers in SCZ patients was low (n = 60) due to the limited sample size and the low prevalence of smoking in first-episode SCZ patients. We also do not know whether the severity of dependence is associated with improvement in negative symptoms because we did not assess it with the Fagerstrom Test for Nicotine Dependence (FTND) in the present study. Therefore, the current study is preliminary and further longitudinal studies with large sample sizes are needed to investigate the role of smoking in the response of SCZ patients to treatment with various antipsychotic medications.
A previous study from our group investigated the association between smoking, oxidative stress and alleviation of clinical symptoms in patients with SCZ50, which demonstrated that smokers showed greater improvement in negative symptoms compared with nonsmokers. The present study recruited only male patients with SCZ and focused on the relationship between smoking and improvements in negative symptoms in SCZ after excluding the potential influence of gender on the findings.
There are some major limitations of the present study. First, due to the observational design of this study, we could not draw clear causal conclusions. Second, the smoking status collected by the self-report questionnaire used to measure smoking status may be a source of differential assessment error that may bias the association between smoking and negative symptoms. In addition, the dose of antipsychotics is flexible depending on the patient’s symptoms, and the daily dose of anitpsychotics used in each patient was not recorded in this study. We also did not measure the serum levels of antipsychotics. Therefore, we did not add the dose as a covariate. Third, the observation points after treatment were limited. Clinical symptoms were only assessed at two time points (baseline and week 12). In addition, the follow-up period is quite short (12 weeks). It would be better to extend this period and carry out a study with a longer period (minimum, 12 months) in the future. Fourth, we only examined the influence of smoking on the improvements in the severity of clinical symptoms. Further studies should extend the test to other broader tests such as the cognitive functions as assessed by MATRICS. Fifth, the number of non-smoking subjects is small compared to nonsmokers, which is different to real clinical practice, where the data indicate a higher prevalence of smokers. This may be due to the fact that all recruited patients were DNFE and were hospitalized during the 12 weeks of treatment.
In conclusion, our study showed that male smokers showed greater improvement in negative symptoms than male nonsmokers after 12 weeks of treatment with antipsychotics. Our findings provide further evidence for the relationship between smoking and negative symptoms in male patients with SCZ in the early stages of this disorder and after treatment with antipsychotics. However, it should be noted that the number of male smokers was small in this study. Further studies with a large sample size of male SCZ patients who smoke, with a longitudinal design of various antipsychotics, are needed to establish this relationship between smoking and the alleviation of negative symptoms in SCZ patients.
References
Barnett, R. Schizophrenia. Lancet 391, 648 (2018).
Mosolov, S. N. & Yaltonskaya, P. A. Primary and secondary negative symptoms in schizophrenia. Front. Psychiatry 12, 766692 (2022).
Correll, C. U. & Schooler, N. R. Schooler, and treatment, negative symptoms in schizophrenia: a review and clinical guide for recognition, assessment, and treatment. Neuropsychiatr. Dis. Treat. 16, 519–534 (2020).
Boutros, N. N., Mucci, A., Diwadkar, V. & Tandon, R. Negative symptoms in schizophrenia. Clin. Schizophr. Relat. Psychoses 8, 28–35b (2014).
Kirkpatrick, B. & Galderisi, S. Deficit schizophrenia: an update. World Psychiatry 7, 143–147 (2008).
Galderisi, S., Mucci, A. & Maj, M. Untangling the factors contributing to functional outcome in schizophrenia—reply. JAMA Psychiatry 75, 754–755 (2018).
Correll, C. U. & Schooler, N. R. Negative symptoms in schizophrenia: a review and clinical guide for recognition, assessment, and treatment. Neuropsychiatr. Dis. Treat. 16, 519–534 (2020).
Smith, R. C., Singh, A., Infante, M., Khandat, A. & Kloos, A. Effects of cigarette smoking and nicotine nasal spray on psychiatric symptoms and cognition in schizophrenia. Neuropsychopharmacology 27, 479–497 (2002).
Ding, J. B. & Hu, K. Cigarette smoking and schizophrenia: etiology, clinical, pharmacological, and treatment implications. Schizophr. Res. Treat. 2021, 7698030 (2021).
Winterer, G. Why do patients with schizophrenia smoke? Curr. Opin. Psychiatry 23, 112–119 (2010).
Myles, N. et al. Tobacco use before, at, and after first-episode psychosis: a systematic meta-analysis. J. Clin. Psychiatry 73, 468–475 (2012).
Williams, J. M. et al. Increased nicotine and cotinine levels in smokers with schizophrenia and schizoaffective disorder is not a metabolic effect. Schizophr. Res. 79, 323–335 (2005).
Wei, S. et al. Demographics, clinical characteristics and cognitive symptoms of heavy smokers and non-heavy smokers in Chinese male patients with chronic schizophrenia. Eur. Arch. Psychiatry Clin. Neurosci. 272, 1325–1333 (2022).
Addington, J., el-Guebaly, N., Campbell, W., Hodgins, D. C. & Addington, D. Smoking cessation treatment for patients with schizophrenia. Am. J. Psychiatry 155, 974–976 (1998).
Heishman, S. J., Kleykamp, B. A. & Singleton, E. G. Meta-analysis of the acute effects of nicotine and smoking on human performance. Psychopharmacology 210, 453–469 (2010).
Zammit, S. et al. Investigating the association between cigarette smoking and schizophrenia in a cohort study. Am. J. Psychiatry 160, 2216–2221 (2003).
Changeux, J. P. Nicotine addiction and nicotinic receptors: lessons from genetically modified mice. Nat. Rev. Neurosci. 11, 389–401 (2010).
Dome, P., Lazary, J., Kalapos, M. P. & Rihmer, Z. Smoking, nicotine and neuropsychiatric disorders. Neurosci. Biobehav. Rev. 34, 295–342 (2010).
Lucatch, A. M., Lowe, D. J. E., Clark, R. C., Kozak, K. & George, T. P. Neurobiological determinants of tobacco smoking in schizophrenia. Front. Psychiatry 9, 672 (2018).
Cooper, J. et al. Tobacco smoking among people living with a psychotic illness: the second Australian Survey of Psychosis. Aust. N. Z. J. Psychiatry 46, 851–863 (2012).
Krishnadas, R., Jauhar, S., Telfer, S., Shivashankar, S. & McCreadie, R. G. Nicotine dependence and illness severity in schizophrenia. Br. J. Psychiatry 201, 306–312 (2012).
Weiser, M. et al. Higher rates of cigarette smoking in male adolescents before the onset of schizophrenia: a historical-prospective cohort study. Am. J. Psychiatry 161, 1219–1223 (2004).
Kendler, K. S., Lönn, S. L., Sundquist, J. & Sundquist, K. Smoking and schizophrenia in population cohorts of Swedish women and men: a prospective co-relative control study. Am. J. Psychiatry 172, 1092–1100 (2015).
Buckley, P. E. & Evans, D. First-episode schizophrenia. A window of opportunity for optimizing care and outcomes. Postgrad. Med. 5–19 (2006).
Zhang, X. Y. et al. Sex difference in the prevalence of smoking in Chinese schizophrenia. J. Psychiatr. Res. 44, 986–988 (2010).
de Leon, J. & Diaz, F. J. A meta-analysis of worldwide studies demonstrates an association between schizophrenia and tobacco smoking behaviors. Schizophr. Res. 76, 135–157 (2005).
Liu, H. et al. Sex-specific association between antioxidant defense system and therapeutic response to risperidone in schizophrenia: a prospective longitudinal study. Curr. Neuropharmacol. 20, 1793–1803 (2021).
Lieberman, J. A. et al. Atypical and conventional antipsychotic drugs in treatment-naive first-episode schizophrenia: a 52-week randomized trial of clozapine vs chlorpromazine. Neuropsychopharmacology 28, 995–1003 (2003).
Kay, S. R., Fiszbein, A. & Opler, L. A. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr. Bull. 13, 261–276 (1987).
Alameda, L. et al. Exploring the mediation of DNA methylation across the epigenome between childhood adversity and First Episode of Psychosis-findings from the EU-GEI study. Mol. Psychiatry 28, 2095–2106 (2023).
Niculescu, A. B. et al. Understanding and predicting suicidality using a combined genomic and clinical risk assessment approach. Mol. Psychiatry 20, 1266–1285 (2015).
Vermeulen, J. M. et al. Association between smoking behavior and cognitive functioning in patients with psychosis, siblings, and healthy control subjects: results from a prospective 6-year follow-up study. Am. J. Psychiatry 175, 1121–1128 (2018).
Luykx, J. J. et al. Interrogating associations between polygenic liabilities and electroconvulsive therapy effectiveness. Biol. Psychiatry 91, 531–539 (2022).
Ohi, K. et al. Polygenic risk scores for late smoking initiation associated with the risk of schizophrenia. NPJ Schizophr. 6, 36 (2020).
Peterson, R. E. et al. Genome-wide analyses of smoking behaviors in schizophrenia: findings from the Psychiatric Genomics Consortium. J. Psychiatr. Res. 137, 215–224 (2021).
Awad, A. G. & Voruganti, L. L. Revisiting the ‘self-medication’ hypothesis in light of the new data linking low striatal dopamine to comorbid addictive behavior. Ther. Adv. Psychopharmacol. 5, 172–178 (2015).
Oleson, E. B. & Cheer, J. F. A brain on cannabinoids: the role of dopamine release in reward seeking. Cold Spring Harb. Perspect. Med. 2, a012229 (2012).
Sabe, M., Zhao, N. & Kaiser, S. Cannabis, nicotine and the negative symptoms of schizophrenia: Systematic review and meta-analysis of observational studies. Neurosci. Biobehav. Rev. 116, 415–425 (2020).
Yang, Y., Marder, S. R. & Green, M. F. Repurposing drugs for cognition in schizophrenia. Clin. Pharmacol. Ther. 101, 191–193 (2017).
Šagud, M. et al. Smoking in schizophrenia: an updated review. Psychiatr. Danub 30, 216–223 (2018).
Oluwoye, O. et al. Impact of tobacco, alcohol and cannabis use on treatment outcomes among patients experiencing first episode psychosis: data from the national RAISE-ETP study. Early Interv. Psychiatry 13, 142–146 (2019).
Millan, M. J., Fone, K., Steckler, T. & Horan, W. P. Negative symptoms of schizophrenia: clinical characteristics, pathophysiological substrates, experimental models and prospects for improved treatment. Eur. Neuropsychopharmacol. 24, 645–692 (2014).
Abi-Dargham, A. Do we still believe in the dopamine hypothesis? New data bring new evidence. Int. J. Neuropsychopharmacol. 7, S1–S5 (2004).
Müller Herde, A. et al. Chronic nicotine exposure alters metabotropic glutamate receptor 5: longitudinal PET study and behavioural assessment in rats. Neurotox Res. 36, 806–816 (2019).
Whitton, A. E. et al. Potent dopamine D2 antagonists block the reward-enhancing effects of nicotine in smokers with schizophrenia. Schizophr. Bull. 45, 1300–1308 (2019).
Glassman, A. H. Cigarette smoking: implications for psychiatric illness. Am. J. Psychiatry 150, 546–553 (1993).
Drew, A. E., Derbez, A. E. & Werling, L. L. Nicotinic receptor-mediated regulation of dopamine transporter activity in rat prefrontal cortex. Synapse 38, 10–16 (2000).
Nomikos, G. G. et al. Role of alpha7 nicotinic receptors in nicotine dependence and implications for psychiatric illness. Behav. Brain Res. 113, 97–103 (2000).
Sagud, M., Mihaljevic Peles, A. & Pivac, N. Smoking in schizophrenia: recent findings about an old problem. Curr. Opin. Psychiatry 32, 402–408 (2019).
Chen, N. et al. Smoke, GPx activity and symptoms improvement in patients with drug-naive first-episode schizophrenia: a large-scale 12-week follow-up study. Asian J. Psychiatr. 77, 103267 (2022).
Acknowledgements
This study was funded by the Natural Science Foundation of Guangdong Province (2023A1515011728), Plan on enhancing scientific research in GMU (02-410-230221XM), Project of Guangzhou Municipal Science and Technology Bureau (2023A03J0835), the Guangzhou Municipal Health Commission (2023C-TS26), Opening Foundation of Jiangsu Key Laboratory of Neurodegeneration, Nanjing Medical University (KF202202), Open Project Program of State Key Laboratory of Virtual Reality Technology and Systems, Beihang University (VRLAB2022 B02), and Shanghai Key Laboratory of Psychotic Disorders Open Grant (21-K03), Guangzhou Key R&D Program Agriculture and Social Development Science and Technology Project (202206010034), Guangzhou Municipal Basic Research Project jointly funded by municipal schools (institutes) (2023A03J0834), Guangzhou High-level Clinical Key Specialty, and Guangzhou Research-oriented Hospital. All funding had no role in study design, data analysis, paper submission and publication. The funding for this study had no further role in study design, data analysis, and the decision to submit the paper for publication.
Author information
Authors and Affiliations
Contributions
X.M. and Z.L. were responsible for study design, statistical analysis and manuscript preparation. X.M., W.W., X.S., H.G., S.W., and X.G. were responsible for recruiting the patients, performing the clinical rating and collecting the clinical data. X.M., X.L., and Z.L. were evolving the ideas and editing the manuscript. X.M., X.L., and Z.L. were involved in writing the protocol, and cowrote the paper. All authors have contributed to and have approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mu, X., Wu, W., Wang, S. et al. Smoking affects symptom improvement in schizophrenia: a prospective longitudinal study of male patients with first-episode schizophrenia. Schizophr 10, 34 (2024). https://doi.org/10.1038/s41537-024-00449-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41537-024-00449-1