Abstract
Virtual reality (VR) technology can be a supporting tool to enhance mindfulness. Recently, many research using VR-based mindfulness (VBM) has been carried out in various psychiatric disorders but not in psychosis. We investigated safety and effects of virtual reality-based mindfulness (VBM) in patients with psychosis as a pilot study. Sixty-four patients were randomly assigned to VBM or to VR control. For VBM, education and meditation videos were provided. For VR control, 3-dimensional natural scenes were shown. Both programs consisted of 8 weekly sessions, each lasting about 30 min. Pre- and post-assessments were performed using the experiences questionnaire (EQ), psychotic symptom rating scales-delusion (PSYRATS-D), PSYRATS-auditory hallucinations (AH), motivation and pleasure scale-self rating (MAP-SR) and etc. The safety questionnaire was also surveyed after 1st and 8th session. Physiological measures such as skin conductance level (SCL), heart rate (HR) and RR interval, were collected during the VR interventions. Limited individuals participated in the safety questionnaire and physiological measures. All the results were presented in mean and standard deviation. We did not observe significant results in group x time interaction and main effects of group and time in the decentering and clinical scales. However, within group comparison showed that patients randomized to VBM showed increased decentering (p = 0.029) and decreased amount (p = 0.032) and duration of preoccupation (p = 0.016) in the PSYRATS-D. For the feelings and motivations about close caring relationships of the MAP-SR, we observed a significant group x time interaction (p = 0.027). The frequency of VR sickness was high but its severity was mild. There were significant differences only in HR over time in the VBM group (p = 0.01). These results suggest that VBM was not more effective in reducing decentering and psychiatric symptoms than VR control but its adversity was modest.
Similar content being viewed by others
Introduction
Virtual reality (VR) involves computer technology that enables the perception of multisensory stimuli within immersive, 3D, complex environments. With VR, patients can practice functioning in familiar settings, which may allow them to develop skills that are more generalizable to real-world situations1. As it also provides a realistic and immersive environment tailored to the individual’s needs, patients with mental health problems would feel more engaging and safer trying things in VR. Because of these beneficial features, VR therapy has emerged as a successful solution for a wide range of psychiatric disorders. Studies have shown that VR can be a promising add-on in the treatment, as well as assessment of many psychiatric disorders, such as substance use disorders2, specific phobias3, posttraumatic stress disorder (PTSD)4, stress and anxiety5,6,7 as well as an array of other diagnosis such as Alzheimer’s disease8. Although research using this technology in schizophrenia is recent, promising results were shown in the treatment of delusions9 and in the evaluation and training of cognitive and social skills10,11,12,13. All these studies incorporated various components of cognitive-behavioral therapy, exposure therapy or psychoeducation into VR technology.
Mindfulness has been defined as the act of consciously focusing the mind in the present moment without judgment and without attachment to the moment14. Mindfulness based interventions (MBIs) have been found effective for the treatment of psychological morbidities and emotional distress in physical and mental illness, including recurrent major depressive disorder, bipolar disorder, chronic pain, stress, anxiety disorders, chronic physical illness, eating disorders, cancer and substance use disorders15. The proposed mechanisms of MBI based on the Buddhist psychological model16 are acceptance/compassion, attention regulation, ethical practices, nonattachment and nonaversion, and decreased mental proliferation17. Historically, clinical literature has warned against the use of meditation with people experiencing symptoms of psychosis18. However, growing evidence have suggested the MBIs can be safe and effective with some modification in patients with psychosis15,19. One meta-analysis study reported that MBIs were moderately effective in pre-post studies but found to have small-to-moderate effect sizes when studies included a comparison group20. They were moderately effective in reducing negative and affective symptoms and in increasing functioning and quality of life. For positive symptoms, results suggested smaller effects.
However, mindfulness requires conscious effort and can be difficult to maintain, particularly for patients with psychosis having cognitive impairment. In recent years there has been an interest in using VR to support mindfulness practice. As VR is a very attention-grabbing technology in terms of providing a set of images and sounds of real-life situations and can be experienced without the constraints of time and space, VR-based mindfulness (VBM) may help patients focus their attention on achieving a state of mindfulness more easily and more conveniently. Moreover, it can be more attractive and compelling to young people with strong sense of adventure and desire for new technology. The VBM has already demonstrated positive outcomes in patients with depression21, panic disorder22, post-traumatic stress disorder23, methamphetamine use disorder24, borderline personality disorder25, severe burn26, and spinal cord injury27. In addition, VR-based guided meditation was found to have beneficial effect on heart rate variability28. Nevertheless, to the best of our knowledge, no study was undertaken in the field of psychosis using VBM. This stress the need of conducting a pilot study in psychosis in terms of feasibility of the study protocol, acceptability of the VBM, selection of the most appropriate primary outcome measure and sample size calculation for a full-scale trial.
Therapeutic effects of mindfulness intervention (MI) are known to be related to decentering29 Decentering is described as the capacity to take a detached view of one’s thoughts and emotions with a present-focused, nonjudgmental stance30,31. Based on this, we hypothesized that VBM would help attain decentering stance about themselves or situations in patients with psychosis which in turn may lead to a reduction of psychopathology. The present pilot study sought to investigate safety and effects of VBM in patients with psychosis. In addition, for an exploratory purpose, physiological measures such as skin conductance level (SCL), hear rate (HR) and RR interval, were collected during the VR intervention in some individuals.
Methods
Participants
Patients were recruited from outpatient clinics of psychiatry at four hospitals: Jeonbuk National University Hospital, Chonnam National University Hospital, Inje University Haeundae Paik Hospital, and Kyungpook National University Hospital from April 2020 to Feb 2022. Inclusion criteria were as follows: (a) schizophrenia spectrum disorders (schizophrenia, schizoaffective disorder, schizophreniform disorder) or psychotic disorder not otherwise specified (NOS), (b) between 18 and 59 years of age, and (c) stable outpatients with no change of medication during past 2 months. Diagnoses were established using the criteria of the Diagnostic and Statistical Manual of Mental Disorders fourth edition32. Two experienced psychiatrists from each institute participated in the diagnostic evaluation and reached a consensus on final diagnosis through discussion. The exclusion criteria were as follows: (a) IQ ≤ 70, (b) acute, unstable, or severe medical/neurological conditions, or (c) pregnant or lactating.
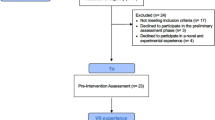
Initially eighty-five individuals were approached but 18 declined to participate. To sixty-seven patients, information about the study objectives and procedure was provided and informed consents were obtained. In the process, three were excluded due to the violation of inclusion/exclusion criteria. The remaining sixty-four patients were randomized to VBM or VR control group within blocks such that similar numbers were assigned to each group. During the trial, three were dropped out (Fig. 1). The authors assert that all procedures contributing to this work comply with the ethical standards of relevant national and institutional Human Experimental Commissions and the 1975 Declaration of Helsinki as amended in 2008. All procedures involving human subjects/patients were approved by Ethics Jeonbuk National University Hospital Committee (approval number CUH 2020-01-042). Trial was registered at the Clinical Research Information Service (KCT0007718).
Measures
Data on sociodemographic variables (sex, age and education), clinical data and medications were collected. The clinical data included duration of untreated psychosis (DUP) and duration of illness (DI). The total daily dose of antipsychotics at the time of baseline assessment was converted to chlorpromazine (CPZ) dose equivalents based on a defined daily dose33. For the evaluation of psychopathology, the Positive and Negative Syndrome Scale34 (PANSS), Psychotic Symptom Rating Scale-Delusions & Auditory hallucinations35 (PSYRATS-D and PSYRATS-AH) and Columbia-Suicide Severity Rating Scale36 (C-SSRS) were performed. The raters were psychiatrists with at least 2-year experience on these measures and blind to the type of intervention randomized to the patients. For self-rating scale, the Experiences Questionnaire (EQ) measuring decentering37, Beck Depression Inventory38 and Motivation and Pleasure Scale-Self Report39 were administered. The MAP-SR is a 15-item scale measuring the motivation and pleasure domain of negative symptoms rated on a 5-point Likert scale. Based on the previous studies demonstrating effects of decentering in depression40,41,42, we considered the EQ as a primary outcome measure. All measures were performed within one-week before and after the intervention. Safety was operationalized as no triggering of significant levels of simulator or VR sickness, and no adverse experiences in the following week. VR sickness refers to symptoms similar to motion sickness (e.g. nausea, dizziness). VR sickness was evaluated using the Simulator Sickness Questionnaire (SSQ)43. This was surveyed right after the first and final sessions. Only limited individuals participated in this survey because of its late inclusion in the research protocol and subsequently late IRB approval.
VR-based mindfulness and VR control
VBM was developed using 360 and 3 D camera. It consists of educational (4 min) and therapeutic (5–8 min) videos. The educational video has two parts. The first one is about general introduction of mindfulness and was used in the first four therapeutic sessions. It explains the origin of suffering (attachment and aversion) and emphasizes the importance of strengthening self-monitoring and self-perception to be aware of it. As a first step, focusing on breathing is explained. The second one is about reemphasizing breathing meditation to calm one’s mind, concept of decentering, truth of impermanence and steady practice at home. This video was used in the last four therapeutic sessions. The therapeutic video has four different meditations such as five-sense awareness meditation, awareness meditation, looking back at myself meditation and loving-kindness meditation during which related instructions were given intermittently. The first two types of meditation are to enhance awareness of body sensation and internal thoughts/feelings and the third to improve non-reactive self-related processing44. The last one was included based on the recent interest in loving-kindness meditation as an extension of mindfulness constructs45,46. Educational material and guiding instructions during therapeutic sessions were developed and recorded by psychiatrists who has full experience and expertise in mindfulness (YH Park and YC Chung). To be tailored to patients with psychosis, formats were designed with short practice time, more guidance and short silence47. For shooting meditation videos, experts were recruited and recorded at different places in Jeju island, Korea. For VR control (10 min), 3D videos of nature scenes were selected from Google sites. The nature scenes with calm and relaxing contents were only selected. Screenshots of examples of VR-based MI are shown in Fig. 2. To experience VR, a head-mounted display (Oculus Rift CV1, Reality Labs, Menlo Park, United States) was used. The Head-mounted Display (HMD) has a 90 Hz refresh rate and a 110° field of view with high resolution (1080 × 1200). The VR environments were generated using the Unity engine (Unity Technologies, San Francisco, USA).
A range of physiological stress measures was taken during the VR exposure during the 1st and 8th sessions. Skin conductance level (SCL) was recorded using two gold coated flat and dry surface electrodes (about Ø = 10 mm) that were covered with isotonic electrode gel and placed on the forehead. The sampling rate was 100 Hz. Skin conductance was expressed as mean skin conductance level (μS) between the different data points. Heart rate (HR) was recorded using an earlobe-pulse-plethysmograph (FNIKorea Co., Ltd, Gwacheon, Korea). The sampling rate was 256 Hz. The time intervals between consecutive heart beats, RR intervals, were also measured. For VBM, physiological measures were collected during one educational and two therapeutic video exposures respectively. For VR control, physiologic measures were obtained one time during the whole exposure. Only limited individuals participated in measuring physiological signals because of the same reason with the VR sickness survey.
Procedures
Participants were randomized to VBM or VR control group via a web-based system (https://www.randomizer.org/). Raters and statistician were blind to group allocation. During the trial, discussion about the cases with names or other potentially identifying information was strictly prohibited. Regardless of the intervention assigned, they received 8 weekly sessions, each lasting 30 min at the digital therapy room of hospital. For every session, they randomly chose two different meditations or nature videos. After application of the equipment for the physiological measurements, participants put on the HMD and experienced the sessions. After the sessions, experiences and any adverse events were discussed. Especially to the participants receiving VBM, core principles of mindfulness and steady practice at home were re-emphasized. During the trial, treatment as usual (supportive psychotherapy, psychoeducation and maintained pharmacotherapy) was provided to all participants.
Statistical analysis
On the basis of the existing literature on mindfulness or decentering, a small to medium effect size (0.35) was expected48,49. A power analysis indicated that 44 subjects per group would give adequate power (0.80) to detect an effect of this size. Group characteristics at baseline between the two groups were compared with a two-sample t test or Chi-square test. A 2 × 2 mixed design was employed, comprising two factors with two levels each. The first factor was intervention type (VBM and VR control), and the second factor was time points (pre- and post-intervention). Effects on clinical variables were verified using two-way repeated measure (RM) ANCOVA and paired t test for between group and within group comparisons respectively. Because of exploratory nature of the study, multiple comparison was not controlled. For VR sickness, the McNemar test or Chi-square test was performed. One-way RM ANOVA was performed for SCL, HR and RR intervals collected during six time periods (one educational and two meditation videos in the first and 8th sessions) in VBM group. Two-way RM ANOVA was conducted to examine effects of VR interventions on three physiological measures between the VBM and VR control groups. Statistical analyses were performed using R Statistical Software (version 4.3.0, R Foundation for Statistical Computing, Vienna, Austria). All statistical analyses were two-sided, and p < 0.05 was considered statistically significant.
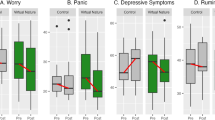
Results
There were no significant differences in demographic and clinical characteristics of the participants between the two groups (Table 1). The two-way RM ANCOVA showed significant group x time interaction only for feelings and motivation about close, caring relationships of the MAP-SR (p = 0.027). The post-hoc tests demonstrated a significant difference between the two groups at baseline (p = 0.015) but not at the endpoint (p = 0.48). For within group comparison, most of subscale scores of the PSYRATS-D were changed significantly in VBM group, and total score and subscale scores of the PANSS changed significantly in both VBM and VR control groups. The BDI score changed only in VR control group (P = 0.01) whereas score of the EQ differed only in VBM group (P = 0.03) (Table 2).
For VR sickness, most common symptoms in VBM group were difficulty with visual focus [10/13 (77 %)], blurred vision [9/13 (69%)] and eye fatigue [9/13 (69%)] whereas in the control group, blurred vision [10/15 (67%)], general discomfort [9/15 (60%)] and difficulty with visual focus [8/15 (53%)]. In the VBM group, percentage of fullness of head decreased after 8th session relative to after 1st session (P = 0.03). In the VR control group, opposite finding was found (P = 0.046). There were no significant differences in the incidence of symptoms of VR sickness between the two groups at both after 1st session and after 8th session (Table 3). The severity of symptoms of VR sickness was usually less than 2 (moderate) in both groups (Table S1).
We were able to collect physiological measures from 8 and 9 patients allocated to VBM and VR control groups. One-way RM ANOVA showed a significant main effect in time only for HR (F (5,35) = 3.10, P = 0.02) (Table S2). In the post-hoc test, significant differences were shown between T1 vs. T3 and T5 (Fig. S1). Two-way RM ANOVA showed a significant main effect in time only for HR (F (1,16) = 8.69, P = 0.01) (Table S3). Post-hoc test showed a significant difference of HR in the first session vs. HR in the 8th session only in VBM group (Fig. S2).
Discussion
VR technology can facilitate mindfulness learning by reducing the interference of distractors from the natural environment and providing a sense of presence in immersive environments. These qualities have great potential to benefit research in that extraneous variables that would otherwise be uncontrollable can be limited. There has been widespread use of VR-based MI in diverse clinical areas but surprisingly no study in psychosis. The present study is the first randomized controlled study exploring safety and effects of VBM in patients with psychosis. The VBM was tolerable but the frequency of VR sickness was high. We could not observe a significant effect of the VBM on the decentering, a primary outcome, between the two groups but on the change of feelings and motivations about close caring relationships in the MAP-SR.
We observed a significant reduction of decentering in the treatment group but not in the control group. Studies have shown that decentering reduced levels of depressive rumination by teaching patients more adaptive ways of relating to their thinking40 and was associated with less depressive symptoms41 or the lowest rates of relapse of depression in the 18-month follow-up period42. However, using keywords such as decentering, psychosis and/or schizophrenia, no studies were found. Instead, several studies investigated “decentration” in patients with schizophrenia50,51,52 along with self-reflectivity, understanding of others’ minds and mastery. It is defined as the ability to see others as having independent motives like theory of mind and could be considered as one component of social cognition whereas decentering is focused on self-awareness. However, we did not observe significant results in group x time interaction and main effects of group and time. In other words, these findings suggest that increased decentering in the treatment group was not enough to produce a significant difference compared to the control group. As the degree of presence could be influential in mindfulness research incorporating VR, causes for this negative finding may be interpreted that the setting or contents of our VBM were not good enough to produce a fully immersive feeling of presence. Or it may be related to a relatively small sample size of the participants.
Interestingly, we found significant reductions of the amount and duration of preoccupation in the PSYRATS-D in the treatment group but not in the control group. Also, between group difference for the duration of preoccupation was a trend toward significance. This may be related to increased decentering in the treatment group. This speculation may be supported by the results of additional correlation analysis that the score of the EQ was negatively associated with the duration of preoccupation (\(r\) = –0.43, P = 0.01) and amount of preoccupation (\(r\) = –0.34, P = 0.54) at the post-assessment. Given that effect of MI on positive symptoms is generally small20 and scores of the PSYRATS-D in the present study were very low, our finding is encouraging. During the trial, we felt that in order to enhance decentering stance more effectively in psychosis, guiding comments should be modified from typical approach, being aware of one’s own drive or attachment and acceptance of one’s own bad words and behaviors, to a new transformative approach, being aware of one’s own trauma/hurts coming from others drive or attachment and focusing more on self-compassion and self-kindness. This new approach may be more fit with patient mind status fully filled with fear/threatened feelings, anger, shame/guilt or mistrust. Additionally, it is of note that both education before the session and instructions given during the session were general explanations about stress and mindfulness, not mentioning specific symptoms. If we further incorporate specific mindfulness-based education or instruction on how to cope with positive symptoms in the program, this would yield more encouraging results on positive symptoms which need to be tested in future studies. Collectively, our results suggest that VBM is beneficial in enhancing decentering and decreasing preoccupation and distress related to delusion in patients with psychosis. As for the results on the PSYRATS-AH, there were no significant changes in any domains of the PSYRATS-AH after VR-based MI in both treatment and control groups. This indicates that VBM is not effective in reducing AHs even though baseline scores of the PSYRATS-AH in the treatment group were significantly higher compared to the control group. Psychological therapies for voices emphasize a decentered relationship with voices such as an awareness of experiences, maintenance of distance and disidentification from them53. It should be noted that in one randomized controlled trial with large sample size, AVATAR therapy for AH involves specifically how to cope with voices such as assertive responding and dialog with therapist54. In order to see positive results on AHs, it seems necessary to modify contents of VBM.
For the PANSS, there were no significant results in group x time interaction and main effect of group However, within group comparisons showed significant improvements in total, positive symptom and negative symptom scores of the PANSS in both groups. These findings suggest that both interventions are effective in reducing psychopathologies but effect of VBM is not superior to that of the VR control. One important controversial issue is what is the best and optimal control condition for VBM. Other studies adopted a wait-list approach, VR mental relaxation, or supportive counseling. We believe that our VR control condition is optimal in that every setting is the same except the contents of the VR. This may have contributed to the negative findings for between-group differences. Importantly, we observed a significant group x time interaction in the feelings and motivations about close caring relationships between the two groups. Considering that there were no within-group differences in both groups, this finding may be driven by the sum of little increase in the treatment group and little decrease in the control group. The decrease of the feelings and motivations about close caring relationships in the control group may be related to the increase in the negative symptoms in the control group. In other words, these findings collectively suggest that VBM might be beneficial in preventing aggravation of feelings and motivations about close caring relationships or negative symptoms compared to VR control. This possibility should be explored in future studies with a larger sample.
Regarding safety, most of the participants reported various symptoms of VR sickness: the most common symptoms in the treatment group were difficulty with visual focus, blurred vision and eye fatigue and in the control group, blurred vision, general discomfort and difficulty with visual focus. However, severity of symptoms was mostly mild level. In addition, there were no significant differences in the frequency of symptoms between the two groups. These findings indicate that VBM and VR control can be carried out safely in patients with psychosis which is in line with other studies in psychosis9,54. The safe profile of VR-based programs may be related to very low attrition rates (3.4 or 5.7%) in the two groups. This could be considered as a strength of using VR-based programs, especially in young individuals with psychosis. Analysis of physiological measures revealed that there were significant differences only in HR over time in the VBM group. Although the effects were not marked enough to produce a significant group difference, these findings suggest that VBM could decrease autonomic activity over time in patients with psychosis.
There are limitations to the study. First, as sample size was relatively small, type II error may exist. In addition, DI and education of the participants were relatively longer and higher. These factors limit the generalizability of our findings. Second, the duration of each session was about 30 min which is a little shorter55,56 or similar57 when compared to other studies. Third, as a short dialog with therapists was carried out after each session in the treatment group to enhance understanding of MI, the quality of therapists may have affected the results. Even though we had introductory online meetings about therapist roles, its control remains crucial in the multi-sites study. Fourth, we did not collect data on prior experiences of VR which may affected results differently. Fifth, the long-term effects of VBM should be explored further. Albeit these caveats, strengths of our study are that this is the first RCT using VBM in patients with psychosis and VR control was optimally designed.
In summary, we did not observe significant differences in decentering between the two groups but a significant difference in group x time interaction for feelings and motivations about close caring relationships of the MAP-SR. In addition, patients randomized to VBM showed increased decentering and decreased amount and duration of preoccupation in the PSYRATS-D although their changes were not enough to produce between-group difference. The frequency of VR sickness was high but its severity was mild and acceptable. These results suggest that VBM was not more effective in reducing decentering and psychiatric symptoms than VR control but its adversity was modest. Given the feasibility of the research design and procedures, acceptability and tolerability of the VBM, and possible type II error, it warrants a full-scale trial with a larger sample size and more rigorous methodology.
References
Cieślik, B. et al. Virtual reality in psychiatric disorders: A systematic review of reviews. Complement Ther. Med. 52, 102480 (2020).
Amista, N. F., Kim, J. J. & Kim, N. Trend and future of virtual reality for addiction treatment of substance use disorders: A systematic review. J. Digit. Contents Soc. 18, 1551–1560 (2017).
Miloff, A. et al. Automated virtual reality exposure therapy for spider phobia vs. in-vivo one-session treatment: A randomized non-inferiority trial. Behav. Res. Ther. 118, 130–140 (2019).
Gonçalves, R., Pedrozo, A. L., Coutinho, E. S., Figueira, I. & Ventura, P. Efficacy of virtual reality exposure therapy in the treatment of PTSD: a systematic review. PLoS One. 7, e48469 (2012).
Maples-Keller, J. L., Bunnell, B. E., Kim, S. J. & Rothbaum, B. O. The use of virtual reality technology in the treatment of anxiety and other psychiatric disorders. Harv. Rev. Psychiatry 25, 103–113 (2017).
Boeldt, D., McMahon, E., McFaul, M. & Greenleaf, W. Using virtual reality exposure therapy to enhance treatment of anxiety disorders: Identifying areas of clinical adoption and potential obstacles. Front Psychiatry 10, 773 (2019).
Freeman, D. et al. Virtual reality in the assessment, understanding, and treatment of mental health disorders. Psychol Med. 47, 2393–2400 (2017).
Clay, F. et al. Use of immersive virtual reality in the assessment and treatment of Alzheimer’s disease: A systematic review. J. Alzheimers Dis. 75, 23–43 (2020).
Fornells-Ambrojo, M. et al. Virtual reality and persecutory delusions: safety and feasibility. Schizophr Res. 104, 228–236 (2008).
Chan, C. L., Ngai, E. K., Leung, P. K. & Wong, S. Effect of the adapted Virtual Reality cognitive training program among Chinese older adults with chronic schizophrenia: a pilot study. Int. J. Geriatr. Psychiatry 25, 643–649 (2010).
Ku, J. et al. VR-based conversation training program for patients with schizophrenia: A preliminary clinical trial. Cyberpsychol Behav. 10, 567–574 (2007).
Park, K. M. et al. A virtual reality application in role-plays of social skills training for schizophrenia: a randomized, controlled trial. Psychiatry Res. 189, 166–172 (2011).
Tsang, M. M. & Man, D. W. A virtual reality-based vocational training system (VRVTS) for people with schizophrenia in vocational rehabilitation. Schizophr Res. 144, 51–62 (2013).
Linehan, M. DBT Skills training manual. Guilford Publications (2014).
Potes, A. et al. Mindfulness in severe and persistent mental illness: a systematic review. Int. J. Psychiatry Clin. Pract. 22, 253–261 (2018).
Grabovac, A., Lau, M. & Willett, B. Erratum to: Mechanisms of Mindfulness: A Buddhist Psychological Model. Mindfulness 2, 218–218 (2011).
Gu, J., Strauss, C., Bond, R. & Cavanagh, K. How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clin. Psychol Rev. 37, 1–12 (2015).
Kuijpers, H. J., van der Heijden, F. M., Tuinier, S. & Verhoeven, W. M. Meditation-induced psychosis. Psychopathology. 40, 461–464 (2007).
Chadwick, P., Taylor, K. N. & Abba, N. Mindfulness groups for people with psychosis. Behav. Cogn. Psychother. 33, 351–359 (2005).
Khoury, B., Lecomte, T., Gaudiano, B. A. & Paquin, K. Mindfulness interventions for psychosis: a meta-analysis. Schizophr Res. 150, 176–184 (2013).
Falconer, C. J. et al. Embodying self-compassion within virtual reality and its effects on patients with depression. BJPsych Open 2, 74–80 (2016).
Seol, E. et al. “Drop the beat” virtual reality based mindfulness and cognitive behavioral therapy for panic disorder–a pilot study. Proc. 23rd ACM Symp. Virtual Reality Softw. Technol. 57, 1–3 (2017).
Rice, V. J., Liu, B. & Schroeder, P. J. Impact of in-person and virtual world mindfulness training on symptoms of post-traumatic stress disorder and attention deficit and hyperactivity disorder. Mil. Med. 183, 413–420 (2018).
Chen, X. J. et al. Mindfulness-based relapse prevention combined with virtual reality cue exposure for methamphetamine use disorder: Study protocol for a randomized controlled trial. Contemp Clin. Trials 70, 99–105 (2018).
Nararro-Haro, M. V. et al. The use of virtual reality to facilitate mindfulness skills training in dialectical behavioral therapy for borderline personality disorder: A case study. Front Psychol 7, 1573 (2016).
Gomez, J. et al. The use of virtual reality facilitates dialectical behavior therapy® “Observing Sounds and Visuals” mindfulness skills training exercises for a latino patient with severe burns: A case study. Front Psychol 8, 1611 (2017).
Flores, A., Linehan, M. M., Todd, S. R. & Hoffman, H. G. The use of virtual reality to facilitate mindfulness skills training in dialectical behavioral therapy for spinal cord injury: A case study. Front Psychol 9, 531 (2018).
Pascual, K., Fredman, A., Naum, A., Patil, C. & Sikka, N. Should mindfulness for health care workers go virtual? A mindfulness-based intervention using virtual reality and heart rate variability in the emergency department. Workplace Health Saf 71, 188–194 (2023).
Hayes, A. M. & Feldman, G. Clarifying the construct of mindfulness in the context of emotion regulation and the process of change in therapy. Clin. Psychol: Sci. Pract. 11, 255 (2004).
Naragon-Gainey, K. & DeMarree, K. G. Structure and validity of measures of decentering and defusion. Psychol Assess 29, 935–954 (2017).
Safran, J. D. & Segal, Z. V. Interpersonal process in cognitive therapy. New York: Basic Books; 1996 sept. 1. ISBN: 1568218583.
American Psychiatric Association, D. S. & American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-4. Washington, DC: American psychiatric association (1994).
Leucht, S., Samara, M., Heres, S. & Davis, J. M. Dose equivalents for antipsychotic drugs: The DDD method. Schizophr Bull 42, S90–S94 (2016).
Kay, S. R., Fiszbein, A. & Opler, L. A. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 13, 261–276 (1987).
Haddock, G., McCarron, J., Tarrier, N. & Faragher, E. B. Scales to measure dimensions of hallucinations and delusions: the psychotic symptom rating scales (PSYRATS). Psychol Med. 29, 879–889 (1999).
Pai, D., Woo, J. M., Son, M. H. & Lee, C. The reliability and validity of the Korean version of Columbia-Suicide Severity Rating Scale in alcohol dependent patients. J. Korean Neuropsychiatric Assoc. 54, 222–227 (2015).
Fresco, D. M. et al. Initial psychometric properties of the experiences questionnaire: validation of a self-report measure of decentering. Behav. Ther. 38, 234–246 (2007).
Beck, A. T., Steer, R. A. & Brown, G. Beck Depression Inventory–II (BDI-II) [Database record]. APA PsycTests. https://doi.org/10.1037/t00742-000 (1996).
Llerena, K. et al. The Motivation and Pleasure Scale-Self-Report (MAP-SR): reliability and validity of a self-report measure of negative symptoms. Compr. Psychiatry 54, 568–574 (2013).
Segal, Z., Mark, W. & John T. Mindfulness-based cognitive therapy for depression. Guilford publications (2002).
Mori, M. & Tanno, Y. Mediating role of decentering in the associations between self-reflection, self-rumination, and depressive symptoms. Psychology. 6, 613 (2005).
Fresco, D. M., Segal, Z. V., Buis, T. & Kennedy, S. Relationship of posttreatment decentering and cognitive reactivity to relapse in major depression. J. Consult Clin. Psychol. 75, 447–455 (2007).
Kennedy, R. S., Lane, N. E., Berbaum, K. S. & Lilienthal, M. G. Simulator sickness questionnaire: An enhanced method for quantifying simulator sickness. Int. J. Aviat. Psychol. 3, 203–220 (1993).
Ngan, S. T. J. & Cheng, P. W. C. Classification of mindfulness meditation and its impact on neural measures in the clinical population. Front Psychol 13, 891004 (2022).
Hofmann, S. G., Grossman, P. & Hinton, D. E. Loving-kindness and compassion meditation: potential for psychological interventions. Clin. Psychol Rev. 31, 1126–1132 (2011).
Grossman, P. et al. MS quality of life, depression, and fatigue improve after mindfulness training: a randomized trial. Neurology. 75, 1141–1149 (2010).
Chadwick, P. Mindfulness for psychosis. Br. J. Psychiatry 204, 333–334 (2014).
Feldman, G., Greeson, J. & Senville, J. Differential effects of mindful breathing, progressive muscle relaxation, and loving-kindness meditation on decentering and negative reactions to repetitive thoughts. Behav. Res. Ther. 48, 1002–1011 (2010).
Orme-Johnson, D. W. & Dillbeck, M. C. Methodological concerns for meta-analyses of meditation: Comment on Sedlmeier et al. (2012). Psychol Bull 140, 610–616 (2014).
Ferrer-Quintero, M. et al. Persons with first episode psychosis have distinct profiles of social cognition and metacognition [published correction appears in Schizophrenia (Heidelb). NPJ Schizophr 7, 61 (2021).
Lysaker, P. H. et al. Metacognitive function and fragmentation in schizophrenia: Relationship to cognition, self-experience and developing treatments. Schizophr Res. Cogn. 19, 100142 (2019).
Semerari, A. et al. How to evaluate metacognitive functioning in psychotherapy? The metacognition assessment scale and its applications. Clin. Psychol. Psychother. 10, 238–261 (2003).
Thomas, N. et al. Psychological therapies for auditory hallucinations (voices): current status and key directions for future research. Schizophr Bull 40, S202–S212 (2014).
Craig, T. K. et al. AVATAR therapy for auditory verbal hallucinations in people with psychosis: a single-blind, randomised controlled trial. Lancet Psychiatry 5, 31–40 (2018).
Freeman, D. et al. Virtual reality in the treatment of persecutory delusions: randomised controlled experimental study testing how to reduce delusional conviction. Br. J. Psychiatry 209, 62–67 (2016).
Pot-Kolder, R. M. C. A. et al. Virtual-reality-based cognitive behavioural therapy versus waiting list control for paranoid ideation and social avoidance in patients with psychotic disorders: a single-blind randomised controlled trial. Lancet Psychiatry 5, 217–226 (2018).
Freeman, D. et al. Automated psychological therapy using virtual reality (VR) for patients with persecutory delusions: study protocol for a single-blind parallel-group randomised controlled trial (THRIVE). Trials. 20, 87 (2019).
Acknowledgements
The corresponding author would like to thank all participants in the study and father for guidance and support (SDG).
Funding
This study was supported by a grant of the Korean Mental Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (HL19C0015) and a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (HR18C0016).
Author information
Authors and Affiliations
Contributions
Y.-C.C. conceptualized the study. S.-W.K., B.J.L., S.-H.W., and Y.-C.C. performed the study and acquired data. B.M.L., C.Y.K., L.L., and F.Z.R. conducted statistical analyses. Y.-C.C. analyzed and interpreted the data. B.M.L. drafted the manuscript. Y.-C.C. critically revised the manuscript. Y.-C.C. received the grant. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, B.M., Kim, SW., Lee, B.J. et al. Effects and safety of virtual reality-based mindfulness in patients with psychosis: a randomized controlled pilot study. Schizophr 9, 57 (2023). https://doi.org/10.1038/s41537-023-00391-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41537-023-00391-8