Abstract
Anhedonia is a common symptom in schizophrenia and is closely related to poor functional outcomes. Several lines of evidence reveal that the orbitofrontal cortex plays an important role in anhedonia. In the present study, we aimed to investigate abnormalities in structural covariance within the orbitofrontal subregions, and to further study their role in anticipatory and consummatory anhedonia in schizophrenia. T1 images of 35 schizophrenia patients and 45 healthy controls were obtained. The cortical thickness of 68 cerebral regions parcellated by the Desikan-Killiany (DK) atlas was calculated. The structural covariance within the orbitofrontal subregions was calculated in both schizophrenia and healthy control groups. Stepwise linear regression was performed to examine the relationship between structural covariance and anhedonia in schizophrenia patients. Patients with schizophrenia exhibited higher structural covariance between the left and right medial orbitofrontal thickness, the left lateral orbitofrontal thickness and left pars orbitalis thickness compared to healthy controls (p < 0.05, FDR corrected). This results imply that the increased structural covariance in orbitofrontal thickness may be involved in the process of developing anhedonia in schizophrenia. The result indicated that the increased structural covariance between the left and right medial orbitofrontal thickness might be a protective factor for anticipatory pleasure (B’ = 0.420, p = 0.012).
Similar content being viewed by others
Introduction
Schizophrenia is a severe mental disorder that affects 0.5–1% of the population worldwide1, and mainly manifests as positive symptoms, negative symptoms, and cognitive impairments. Negative symptoms tend to be residual after treatment and are associated with poor functional outcomes of schizophrenia2,3. Anhedonia is one of the most common negative symptoms in schizophrenia, with an estimated prevalence rate arranging from 45 to ~80%4,5. Anhedonia refers to the reduced capacity to experience pleasure in activities that individuals would normally enjoy6 and is considered to be a vital aspect of psychiatric disorders. The Measurement and Treatment Research to Improve Cognition in Schizophrenia (MATRICS) consensus conference on negative symptoms suggests that anhedonia is one of the five categories of negative symptoms in schizophrenia7. In the “Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition” (DSM-5), anhedonia is defined as “Lack of enjoyment from, engagement in, or energy for life’s experiences; deficits in the capacity to feel pleasure and take interests in things.” Anhedonia has also been divided into consummatory anhedonia and anticipatory anhedonia based on the components of pleasure8. The former refers to the reduction in experiencing pleasure when engaging in an enjoyable activity, while the latter refers to the reduction in experiencing pleasure related to future activities. It was assumed that the two different components of anhedonia may involve distinct biological mechanisms. The presence of anhedonia usually suggests an unfavorable situation, such as treatment resistance and low quality of life in patients with depression9, and poor outcomes and disability in patients with schizophrenia10. Moreover, anhedonia may be responsible for a higher risk of suicidal ideation and suicide attempts in schizophrenia11,12. It was also observed that social anhedonia is closely related to poorer neurocognitive functioning13. This highlights a crucial need to elucidate how anhedonia develops.
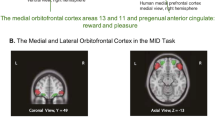
The literature, while still incomplete, has revealed, part of the biological underpinnings of anhedonia. Research into the mechanisms underlying anhedonia plays an important role in potentially mapping the brain abnormalities in anhedonia. Recently, evidence has emerged that the orbitofrontal cortex (OFC) is linked to anhedonia14. The OFC is located on the ventral side of the frontal lobe and receives projections from visual, olfactory, taste, and somatosensory regions15. Evidence has shown that the OFC and the anterior cingulate gyrus are both related to the pleasure sensation brought by taste16. It has been reported that higher levels of physical anhedonia resulted in atypical OFC sulcogyral patterns17, whose activity was found to be negatively correlated with anhedonia14. Evidence indicates that different subregions of the OFC are involved. The medial orbitofrontal cortex (mOFC) is responsible for measuring the reward value of stimuli, while the lateral orbitofrontal cortex (lOFC) is responsible for measuring the punishment component in ongoing activities and provides a basis for a change in behavior18. However, the role of the OFC in reward has mainly been studied in patients with depression. Evidence in schizophrenia patients is relatively rare. Given that many other brain regions have also been reported to be involved in anhedonia, the relationship of the intercortical region may provide new insights into the mechanism of anhedonia.
Structural covariance analysis is an important approach for mapping intercorrelation between brain regions and is promising for investigating neurodevelopmental abnormalities. There is evidence that significant differences in structural covariance exist between schizophrenia patients and healthy controls19. However, whether structural covariance alteration contributes to the pathology of anhedonia is still unclear. Given that human functional magnetic resonance imaging (MRI) studies and animal studies have emphasized the crucial role of cortical regions, especially frontal regions in anhedonia, we hypothesized that anhedonia is related to structural covariance within the OFC. The present study set out to delineate the cortical region abnormalities within the OFC related to anhedonia in the construct of consummatory and anticipatory pleasure in schizophrenia using structure covariance analysis.
Results
Demographic and clinical variables
A total of 80 subjects were included (35 patients with schizophrenia and 45 healthy controls). There were no significant differences in age, sex, marital status, and education level (p > 0.05) between the schizophrenia group and the healthy control group. The schizophrenia group showed significantly lower score of the Temporal Experience of Pleasure Scale (TEPS) (p < 0.05). The results are present in Table 1.
Structural covariance of brain regions within the OFC in patients with schizophrenia and healthy controls
In schizophrenia group, 13 brain structural covariance were significant. In healthy control group, there were 3 brain structural covariance being significant. Finally, 13 brain structural covariance were selected for between-group analysis (see more details in Supplementary Material A). Significantly increased structural covariance between the left and right mOFC thickness (p = 0.012, FDR-corrected) and the left lOFC thickness and left pars orbitalis cortical thickness (p = 0.032, FDR-corrected) were found in patients with schizophrenia (see more details in Fig. 1 and Table 2).
Structural covariance related to anhedonia in schizophrenia
The stepwise regression analysis showed that structural covariance between the left and right mOFC was positively related to anticipatory pleasure (B’ = 0.420, p = 0.012) and the sum of anticipatory and consummatory pleasure (B’ = 0.429, p = 0.010) (see more details in Table 3).
Discussion
It has been proposed that cortical regions, especially the frontal cortex, control higher-order brain functions and exert control over subcortical regions20,21. In this study, we investigated the structural covariance abnormalities underlying anhedonia, and there were several major findings. First, compared to healthy controls, patients with schizophrenia manifested both consummatory and anticipatory anhedonia. Second, patients with schizophrenia showed increased structural covariance in cortical thickness. Third, the increased structural covariance between the left and right medial orbitofrontal thickness was negatively correlated with anhedonia in schizophrenia.
Anhedonia in patients with schizophrenia compared to healthy controls
We found that patients with schizophrenia showed reduced anticipatory and consummatory pleasure, which was congruent with a recent meta-analysis indicating that patients with first-episode or chronic schizophrenia experienced less consummatory and anticipatory pleasure on average than healthy controls22. It is assumed that anticipatory pleasure requires cognitive functions that entail predicting future feelings of pleasure. Therefore, anticipatory anhedonia might be associated with cognitive impairments that commonly occur in patients with schizophrenia. In addition, demotivating beliefs in schizophrenia patients with negative symptoms may also impede anticipatory pleasure23. Consummatory pleasure is more related to in-the-moment pleasure and is thought to have a strong association with the reward system24. However, consummatory pleasure in schizophrenia has long been a debated topic. Many studies have found that consummatory pleasure is intact in schizophrenia patients, even in those with pronounced negative symptoms25,26. The inconsistent results from other studies may result from differences in patient characteristics. For example, most of the studies included patients who were administered with antipsychotics. Antipsychotics mostly exert treatment effects by regulating dopaminergic systems, which are closely related to feelings of pleasure and thereby influence the study results.
Increased structural covariance in cortical thickness in schizophrenia
The regions exhibiting increased structural covariance in the present study included the left and right mOFC, left lateral orbitofrontal cortex and left pars orbitalis cortex.
Schizophrenia typically has an occult onset and exhibits a protracted clinical course. Biological changes, including brain structural and functional alterations, can occur during disease progression or even before illness onset27,28,29. These alterations may relate to the causes, features, or compensatory processes of the disease. Network analysis has shown reorganization patterns of brain function and structure30,31,32 and disturbances in regional correlations such as the frontal regions in schizophrenia33,34. Structural changes in brain regions usually appear in a pattern of concomitant loss and thereby exhibit increased structural covariance in schizophrenia35. Therefore, we expected a highly organized change in key brain regions. Our observation supports this conjecture.
The specific brain regions involved in the altered structural covariance are promising for providing clues regarding the mechanism of the disease. The OFC is a subdivision of the prefrontal cortex that has been proved to be vital in schizophrenia. It has been reported that the activation of apoptosis in the OFC might contribute to the development of schizophrenia36. The OFC volume has also been found to be correlated with negative symptom severity in schizophrenia37. In addition, the OFC is responsible for emotional and executive functioning, decision-making, and reward-related behavior, and is associated with emotional disturbances such as social withdrawal, apathy, and depressed mood, which are commonly seen in schizophrenia38,39. Regional specificity within the OFC further suggests that the mOFC is activated by emotional stimuli40. The lOFC is involved in the process of evaluation, learning of risky bias41,42 and emotions such as regret43. Although studies on the pars orbitalis are scarce, the role of pars orbitalis in semantic deficits has been demonstrated44. The present study suggests that the left and right mOFC, the left lOFC, and the left pars orbitalis were essential regions involved in schizophrenia. Although the literature indicates that these regions might be related to cognitive and emotional disorganization in schizophrenia, longitudinal studies are necessary to fully interpret how these alterations correlate with the characterization, staging, and development of the disease.
Increased structural covariance in cortical thickness correlated with anhedonia in schizophrenia
As discussed above, we found that schizophrenia patients had significantly lower TEPS score (more severe anhedonia) and increased structural covariance compared to normal controls. What this may indicate is that increased structural covariance may associate with lower TEPS score in schizophrenia patients. However, our further analysis reached the opposite conclusion that the increased structural covariance was positively correlated with higher TEPS score (more mild anhedonia) in these patients. In view of this opposite finding, we reasoned that the phenomenon of increased structural covariance in patients might be a protective effect in patients with schizophrenia against anhedonia. Anhedonia is one of the most important symptoms of schizophrenia and has a high prevalence rate. In biochemical terms, ample evidence supports that dopamine dysregulation is involved in the pathological mechanism of anhedonia45. In addition, the association between anhedonia and dopamine dysregulation in the OFC has been reported. Previous positron emission tomography studies recruited healthy volunteers and showed that reward learning processes were correlated with dopamine release in the mOFC and dorsal anterior cingulate cortex (ACC)46. Studies including attention deficit hyperactivity disorder or cocaine-dependent subjects also indicated that OFC dysfunction was related to altered dopamine function47,48.
On the brain functional and structural level, the OFC is considered to play a crucial role in anhedonia. In major depressive disorder, lower OFC gamma activity was correlated with blunted reward learning49, and neural reward prediction error signals in the mOFC were negatively correlated with anhedonia using computational modeling50. In schizophrenia, diffusion tensor imaging studies showed that reduced fractional anisotropy in the left posterior mOFC-ACC was associated with anhedonia39,51.
In summary, the association between the OFC and anhedonia is multifaceted and interconnected (dopamine function, regional structure and function), although further studies are needed to measure dopamine activity in the OFC. What we found in the structural covariance category has added new evidence for the role of the mOFC in anhedonia in schizophrenia patients. The increased structural covariance between the left mOFC and right mOFC may be a compensatory process for anhedonia in schizophrenia. However, in order to obtain stronger evidence, a longitudinal study design to identify a clear relationship between structural covariance and anhedonia is required.
Limitations
Several limitations should be addressed here. First, this is a cross-sectional study. Hence, the change in anhedonia, as well as the structural covariance over the stages of schizophrenia, is unknown. Second, we must admit that the evidence of the protective function of increased structural covariance between the left and right mOFC is relatively weak. As such, prospective studies are needed to provide a more convincing result. Third, the present study aimed to reveal the structural covariance between cortical thickness; therefore, the role of cortical-subcortical interaction cannot be determined. Forth, due to the relatively small sample size, we were unable to perform stratified analysis to exclude the influence of the duration of illness and the medication history.
Conclusion
In the present study, we identified an increased structural covariance mainly in frontal regions, and the increased structural covariance between left and right mOFC might exert a protective effect on anhedonia in schizophrenia.
Methods
Subjects
We recruited 80 subjects altogether (35 patients with schizophrenia and 45 healthy volunteers). The inclusion criteria of the schizophrenia group were as follows: (1) met the diagnostic criteria of schizophrenia in the “Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition” (DSM-IV); (2) a minimum education year of 9; (3) was aged from 18 to 50; (3) was Han Chinese and right-handed; (4) did not take antipsychotic medicine within the last 2 weeks; (5) did not have severe somatic diseases such as brain disease; (6) did not have contraindications for MRI; (7) did not receive physical therapy such as transcranial magnetic stimulation or transcranial direct current stimulation within the last 6 months; and (8) did not have any history of psychiatric comorbidity. Schizophrenia patients were recruited from the Shanghai Mental Health Center as outpatients. Every individual was interviewed by two independent and experienced psychiatrists using the “Mini-International Neuropsychiatric Interview” (MINI). We recruited healthy volunteers through advertisement, and each of them was interviewed by an experienced psychiatrist using the MINI. The inclusion criteria for healthy controls were as follows: (1) a minimum education year of 9; (2) aged from 18 to 50; (3) Han Chinese and right-handed; (4) no history or family history of mental illness; (5) no contraindications for MRI; and (6) no severe somatic diseases. All participants were asked to provide written informed consent. The present study was reviewed and approved by the Review Board of the Shanghai Mental Health Center.
Demographic, clinical, and anhedonic assessments
Demographic information was collected from all participants, including age, sex, education level, duration of illness, marital status, duration of antipsychotic medication, and total antipsychotic dose (olanzapine equivalent) calculated based on defined daily doses. Assessment of clinical symptoms of schizophrenia was performed by trained researchers using the Chinese version of the Positive and Negative Syndrome Scale (PANSS)52. The Temporal Experience of Pleasure Scale (Chinese version)53 was used to assess anhedonia. The TEPS consists of the anticipatory pleasure subscale (TEPS-ANT) and the consummatory pleasure subscale (TEPS-CON), which reflect anticipatory pleasure and consummatory pleasure, respectively.
Imaging data acquisition
Brain image data were collected on a 3 Tesla Siemens Prisma magnetic resonance image (MRI) system equipped with a 64-channel radiofrequency coil. All participants underwent high-resolution T1-weighted anatomical imaging. The parameters were: TR = 2000 ms, TE = 2.32 ms, flip = 8°, 208 slices with thickness = 0.9 mm, FOV = 230 mm * 230 mm; and matrix = 256 * 256. Each subject was instructed to lie still in a supine position during scanning.
Data preprocessing
FreeSurfer v6.0 (https://surfer.nmr.mgh.harvard.edu) was used for imaging preprocessing. The Recon-all command in FreeSurfer was chosen to process whole-brain segmentation automatically. Then each individual’s cortical thickness data were mapped to FreeSurfer’s fsaverage. Next, each hemisphere was parcellated into 34 cortical regions using the Desikan-Killiany (DK) atlas54, and cortical thickness was measured for 3 subregions (the lateral orbitofrontal, medial orbitofrontal and pars orbitalis) within the OFC.
Statistical analysis
All statistical analyses were performed in R3.6.3. All tests were two-sided, and the significance level was set as p < 0.05. The differences in demographic and clinical information between the schizophrenia group and healthy control group were analyzed using either the independent Student’s t test or Pearson’s chi-square test as appropriate. Then, we compared the differences in structural covariance between the two groups. First, we calculated the correlation coefficient between each subregion of the OFC with sex, age, and education level as covariates in the schizophrenia and healthy control groups, respectively. Significant structural covariance in either the schizophrenia or healthy control group was selected for further analysis. Secondly, between-group differences in structural covariance networks within the OFC were assessed using the z-test55 (see more details in Supplementary Material A). We performed a false discovery rate (FDR) correction for multiple comparisons (FDR < 0.05). The Pearson correlation coefficient (r) can be considered the normalized inner product of standard scores (z score) as follows:
X and Y correspond to the thickness of two cortical brain regions across subjects. N represents the sample size of each group (the schizophrenia group and healthy control group). \(\bar X\) and \(\bar Y\) denote the means of X and Y, respectively. s stands for the sample standard deviation. zYi and zYi equal to \(\frac{{{{{\boldsymbol{X}}}}_{{{\boldsymbol{i}}}} - {{{\bar{\boldsymbol X}}}}}}{{{{{\boldsymbol{s}}}}_{{{\boldsymbol{X}}}}}}\) and \(\frac{{{{{\boldsymbol{Y}}}}_{{{\boldsymbol{i}}}} - {{{\bar{\boldsymbol Y}}}}}}{{{{{\boldsymbol{s}}}}_{{{\boldsymbol{Y}}}}}}\), respectively. r can be regarded as the sum of partial_p56. partial_p can be written as follows:
Finally, stepwise linear regression analysis was used to explore the relationship between structural covariance and anhedonia in schizophrenia. The structural covariance of any two brain regions that differed significantly was included in the regression analysis. Moreover, illness duration, sex, age, education level, the score of the positive/negative/general psychopathology subscale of the PANSS, duration of antipsychotic medication, and total antipsychotic dose were also included in the regression analysis to exclude their influence as confounding factors.
References
Perälä, J. et al. Lifetime prevalence of psychotic and bipolar I disorders in a general population. Arch. Gen. Psychiatry 64, 19–28 (2007).
Rabinowitz, J. et al. Negative symptoms have greater impact on functioning than positive symptoms in schizophrenia: analysis of CATIE data. Schizophr. Res. 137, 147–150 (2012).
Robertson, B. R. et al. Social competence versus negative symptoms as predictors of real world social functioning in schizophrenia. Schizophr. Res. 160, 136–141 (2014).
Horan, W. P., Kring, A. M. & Blanchard, J. J. Anhedonia in schizophrenia: a review of assessment strategies. Schizophr. Bull. 32, 259–273 (2006).
Pelizza, L. & Ferrari, A. Anhedonia in schizophrenia and major depression: state or trait? Ann. Gen. Psychiatry 8, 22 (2009).
Andreasen, N. C. & Olsen, S. Negative v positive schizophrenia. Definition and validation. Arch. Gen. Psychiatry 39, 789–794 (1982).
Kirkpatrick, B., Fenton, W. S., Carpenter, W. T. & Marder, S. R. The NIMH-MATRICS consensus statement on negative symptoms. Schizophr. Bull. 32, 214–219 (2006).
Gard, D. E., Kring, A. M., Gard, M. G., Horan, W. P. & Green, M. F. Anhedonia in schizophrenia: distinctions between anticipatory and consummatory pleasure. Schizophr. Res. 93, 253–260 (2007).
Spijker, J., Bijl, R. V., de Graaf, R. & Nolen, W. A. Determinants of poor 1-year outcome of DSM-III-R major depression in the general population: results of the Netherlands Mental Health Survey and Incidence Study (NEMESIS). Acta Psychiatr. Scand. 103, 122–130 (2001).
Kiwanuka, J. N., Strauss, G. P., McMahon, R. P. & Gold, J. M. Psychological predictors of functional outcome in people with schizophrenia. Schizophr. Res. 157, 299–304 (2014).
Loas, G., Azi, A., Noisette, C., Legrand, A. & Yon, V. Fourteen-year prospective follow-up study of positive and negative symptoms in chronic schizophrenic patients dying from suicide compared to other causes of death. Psychopathology 42, 185–189 (2009).
Winer, E. S. et al. Anhedonia predicts suicidal ideation in a large psychiatric inpatient sample. Psychiatry Res. 218, 124–128 (2014).
Cohen, A. S., Couture, S. M. & Blanchard, J. J. Neuropsychological functioning and social anhedonia: three-year follow-up data from a longitudinal community high risk study. J. Psychiatr. Res. 46, 898–904 (2012).
Ursu, S. et al. Prefrontal cortical deficits and impaired cognition-emotion interactions in schizophrenia. Am. J. Psychiatry 168, 276–285 (2011).
Rolls, E. T. The functions of the orbitofrontal cortex. Brain Cogn. 55, 11–29 (2004).
de Araujo, I. E. T., Rolls, E. T., Kringelbach, M. L., McGlone, F. & Phillips, N. Taste-olfactory convergence, and the representation of the pleasantness of flavour, in the human brain. Eur. J. Neurosci. 18, 2059–2068 (2003).
Zhang, H., Harris, L., Split, M., Troiani, V. & Olson, I. R. Anhedonia and individual differences in orbitofrontal cortex sulcogyral morphology. Hum. Brain Mapp. 37, 3873–3881 (2016).
Kringelbach, M. L. & Rolls, E. T. The functional neuroanatomy of the human orbitofrontal cortex: evidence from neuroimaging and neuropsychology. Prog. Neurobiol. 72, 341–372 (2004).
Zugman, A. et al. Structural covariance in schizophrenia and first-episode psychosis: an approach based on graph analysis. J. Psychiatr. Res. 71, 89–96 (2015).
Gläscher, J., Adolphs, R. & Tranel, D. Model-based lesion mapping of cognitive control using the Wisconsin Card Sorting Test. Nat. Commun. 10, 20 (2019).
Stuss, D. T. Functions of the frontal lobes: relation to executive functions. J. Int. Neuropsychol. Soc. 17, 759–765 (2011).
Visser, K. F., Chapman, H. C., Ruiz, I., Raugh, I. M. & Strauss, G. P. A meta-analysis of self-reported anticipatory and consummatory pleasure in the schizophrenia-spectrum. J. Psychiatr. Res. 121, 68–81 (2020).
Pillny, M., Schlier, B. & Lincoln, T. M. “I just don’t look forward to anything”. How anticipatory pleasure and negative beliefs contribute to goal-directed activity in patients with negative symptoms of psychosis. Schizophr. Res. 222, 429–436 (2020).
Meehl, P. E. Schizotaxia, schizotypy, schizophrenia. Am. Psychol. 17, 827–838 (1962).
Barch, D. M., Pagliaccio, D. & Luking, K. Mechanisms underlying motivational deficits in psychopathology: similarities and differences in depression and schizophrenia. Curr. Top. Behav. Neurosci. 27, 411–449 (2016).
Mote, J., Minzenberg, M. J., Carter, C. S. & Kring, A. M. Deficits in anticipatory but not consummatory pleasure in people with recent-onset schizophrenia spectrum disorders. Schizophr. Res. 159, 76–79 (2014).
Cui, L.-B. et al. Baseline structural and functional magnetic resonance imaging predicts early treatment response in schizophrenia. Eur. J. Neurosci. https://doi.org/10.1111/ejn.15046 (2020).
Curtis, M. T., Coffman, B. A. & Salisbury, D. F. Parahippocampal area three gray matter is reduced in first-episode schizophrenia spectrum: discovery and replication samples. Hum. Brain Mapp. https://doi.org/10.1002/hbm.25256 (2020).
Rodriguez-Perez, N. et al. Long term cortical thickness changes after a first episode of non-affective psychosis: the 10 year follow-up of the PAFIP cohort. Prog. Neuropsychopharmacol. Biol. Psychiatry 110180 https://doi.org/10.1016/j.pnpbp.2020.110180 (2020).
Griffa, A. et al. Characterizing the connectome in schizophrenia with diffusion spectrum imaging. Hum. Brain Mapp. 36, 354–366 (2015).
Lo, C.-Y. Z. et al. Randomization and resilience of brain functional networks as systems-level endophenotypes of schizophrenia. Proc. Natl. Acad. Sci. USA 112, 9123–9128 (2015).
Palaniyappan, L. Progressive cortical reorganisation: a framework for investigating structural changes in schizophrenia. Neurosci. Biobehav. Rev. 79, 1–13 (2017).
Bassett, D. S. et al. Hierarchical organization of human cortical networks in health and schizophrenia. J. Neurosci. Off. J. Soc. Neurosci. 28, 9239–9248 (2008).
Zhang, Y. et al. Abnormal topological organization of structural brain networks in schizophrenia. Schizophr. Res. 141, 109–118 (2012).
Palaniyappan, L. et al. Structural covariance and cortical reorganisation in schizophrenia: a MRI-based morphometric study. Psychol. Med. 49, 412–420 (2019).
Velásquez, E. et al. Synaptosomal proteome of the orbitofrontal cortex from schizophrenia patients using quantitative label-free and iTRAQ-based shotgun proteomics. J. Proteome Res. 16, 4481–4494 (2017).
Lacerda, A. L. T. et al. Morphology of the orbitofrontal cortex in first-episode schizophrenia: relationship with negative symptomatology. Prog. Neuropsychopharmacol. Biol. Psychiatry 31, 510–516 (2007).
Jackowski, A. P. et al. The involvement of the orbitofrontal cortex in psychiatric disorders: an update of neuroimaging findings. Rev. Bras. Psiquiatr9 34, 207–212 (2012).
Ohtani, T. et al. Abnormalities in white matter connections between orbitofrontal cortex and anterior cingulate cortex and their associations with negative symptoms in schizophrenia: a DTI study. Schizophr. Res. 157, 190–197 (2014).
Phan, K. L., Wager, T., Taylor, S. F. & Liberzon, I. Functional neuroanatomy of emotion: a meta-analysis of emotion activation studies in PET and fMRI. NeuroImage 16, 331–348 (2002).
Constantinople, C. M. et al. Lateral orbitofrontal cortex promotes trial-by-trial learning of risky, but not spatial, biases. eLife 8 (2019).
Kennerley, S. W., Behrens, T. E. J. & Wallis, J. D. Double dissociation of value computations in orbitofrontal and anterior cingulate neurons. Nat. Neurosci. 14, 1581–1589 (2011).
Steiner, A. P. & Redish, A. D. Behavioral and neurophysiological correlates of regret in rat decision-making on a neuroeconomic task. Nat. Neurosci. 17, 995–1002 (2014).
Catani, M. et al. A novel frontal pathway underlies verbal fluency in primary progressive aphasia. Brain 136, 2619–2628 (2013).
Szczypinski, J. J. & Gola, M. Dopamine dysregulation hypothesis: the common basis for motivational anhedonia in major depressive disorder and schizophrenia? Rev. Neurosci. 29, 727–744 (2018).
Vrieze, E. et al. Measuring extrastriatal dopamine release during a reward learning task. Hum. Brain Mapp. 34, 575–586 (2013).
Lin, S.-H. et al. A pilot study on the association between the blood oxygen level-dependent signal in the reward system and dopamine transporter availability in adults with attention deficit hyperactivity disorder. CNS Spectr. 1–8 https://doi.org/10.1017/S1092852920001133 (2020).
Moeller, F. G. et al. Increased orbitofrontal brain activation after administration of a selective adenosine A(2A) antagonist in cocaine dependent subjects. Front. Psychiatry 3, 44 (2012).
Webb, C. A. et al. Neural correlates of three promising endophenotypes of depression: evidence from the EMBARC study. Neuropsychopharmacology 41, 454–463 (2016).
Rothkirch, M., Tonn, J., Köhler, S. & Sterzer, P. Neural mechanisms of reinforcement learning in unmedicated patients with major depressive disorder. Brain 140, 1147–1157 (2017).
Ohtani, T. et al. Abnormal white matter connections between medial frontal regions predict symptoms in patients with first episode schizophrenia. Cortex 71, 264–276 (2015).
He, Y. L. & Zhang, M. Y. The Chinese norm and factor analysis of PANSS. Chin. J. Clin. Psychol. 8, 65–69 (2000).
Chan, R. C. K. et al. The Temporal Experience of Pleasure Scale (TEPS): exploration and confirmation of factor structure in a healthy Chinese sample. PLoS ONE 7, e35352 (2012).
Desikan, R. S. et al. An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. NeuroImage 31, 968–980 (2006).
Diedenhofen, B. & Musch, J. cocor: a comprehensive solution for the statistical comparison of correlations. PLoS ONE 10, e0121945 (2015).
Eisenberg, I. W., Wallace, G. L., Kenworthy, L., Gotts, S. J. & Martin, A. Insistence on sameness relates to increased covariance of gray matter structure in autism spectrum disorder. Mol. Autism 6, 54 (2015).
Acknowledgements
This work was supported by National Key Research and Development Program of China (grant number 2018YFC1314302), National Natural Science Foundation of China (grant numbers 81471358 and 81771450), Western Medicine Guide Project of Shanghai Municipal Commission of Science and Technology (grant number 14411969000), and Top Talent Support Program for Young and Middle-aged People of Wuxi Health Committee (WX18IIAN032).
Author information
Authors and Affiliations
Contributions
C.Z. designed the study and revised the manuscript. L.Y. and Z.W. managed the literature searches, data acquisition, data analysis and drafting the article. D.W. made contributions to literature searches and data collection. C.G., X.T. and G.Z. made contributions to data acquisition. X.F. designed the study and revised the article. All authors contributed to and have approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was reviewed and approved by the Review Board of the Shanghai Mental Health Center.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yu, L., Wu, Z., Wang, D. et al. Increased cortical structural covariance correlates with anhedonia in schizophrenia. Schizophr 9, 19 (2023). https://doi.org/10.1038/s41537-023-00350-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41537-023-00350-3