Abstract
Cognition and social cognition anomalies in patients with bipolar disorder (BD) and schizophrenia (SCZ) have been largely documented, but the degree of overlap between the two disorders remains unclear in this regard. We used machine learning to generate and combine two classifiers based on cognitive and socio-cognitive variables, thus delivering unimodal and multimodal signatures aimed at discriminating BD and SCZ from two independent groups of Healthy Controls (HC1 and HC2 respectively). Multimodal signatures discriminated well between patients and controls in both the HC1-BD and HC2-SCZ cohorts. Although specific disease-related deficits were characterized, the HC1 vs. BD signature successfully discriminated HC2 from SCZ, and vice-versa. Such combined signatures allowed to identify also individuals at First Episode of Psychosis (FEP), but not subjects at Clinical High Risk (CHR), which were classified neither as patients nor as HC. These findings suggest that both trans-diagnostic and disease-specific cognitive and socio-cognitive deficits characterize SCZ and BD. Anomalous patterns in these domains are also relevant to early stages of disease and offer novel insights for personalized rehabilitative programs.
Similar content being viewed by others
Introduction
Schizophrenia and bipolar disorder are two severe brain diseases that heavily compromise quality of life and personal functioning1,2. Despite their traditional nosological discrimination3, cross-domain evidence suggests a quite large degree of clinical overlap. Indeed, patients often do not fit completely within the boundaries of a single disorder and show a mixture of psychopathological features traditionally associated with both these illnesses4,5. Therefore, rather than considering schizophrenia and bipolar disorder as two separate diagnostic entities, recent views have hypothesized that they lie on a psychopathological continuum6. This view is further supported by growing evidence highlighting partially shared genetic risk between the two diseases7,8. Thus, partially-shared phenotypes9 may characterize these brain disorders, under the influence of partially-shared genetic risk factors.
Among phenotypes in common between patients with schizophrenia (SCZ) and with bipolar disorder (BD), those related to cognitive and socio-cognitive impairments10,11 play a key role. Indeed, such correlates are crucially associated with both the diseases12. Univariate literature13,14 is relatively consistent in showing more quantitative (i.e., in terms of severity of impairments) than qualitative (i.e., in terms of differentially impaired domains) cognitive differences between bipolar disorder and schizophrenia. Typically, SCZ exhibit more severe and pervasive core cognitive deficits, which affect multiple domains including processing speed15, verbal fluency16, episodic and working memory17, and cognitive flexibility18. These alterations usually emerge in the context of a global intellectual impairment10,19 and are tightly associated with negative symptoms and disorganization, crucially contributing to the typical increased functional disability in SCZ20.
Also BD experience specific alterations affecting different cognitive domains13,14,21, but to a lesser extent and within a framework of relatively preserved general intelligence, likely reflecting better premorbid functioning2. This pattern of milder cognitive impairment in bipolar disorder emerges across a broad range of domains, including attention, verbal memory, working memory, and executive functioning10,22. This body of evidence suggests that BD and SCZ could be differentiated at the cognitive level only quantitatively, and not qualitatively. Interestingly, this seems to be the case also for social cognition. In this regard, meta-analytic findings reveal a stable pattern of socio-cognitive deficits across domains, including recognition and perception of basic socio-emotional cues, social inference23 as well as theory of mind11, with SCZ showing the same socio-cognitive abnormalities of BD, but to a greater extent11,23. Taken together, this literature suggests that SCZ and BD are difficult to distinguish based on cognitive and socio-cognitive characteristics. Indeed, these impairments define a dimensional phenotype occurring among psychosis spectrum disorders24. Furthermore, subclinical signs identifying risk conditions for psychosis spectrum disorders are paralleled by both cognitive and socio-cognitive deficits22. In this regard, previous studies have highlighted that individuals at clinical high risk for psychosis (i.e., at-risk mental state for psychosis—ARMS)25 and bipolar disorder (i.e., bipolar at-risk—BAR)26 show a large extent of quantitative and qualitative similarities in the occurrence of early cognitive27 and socio-cognitive impairments28.
However, all this literature is based on univariate statistical approaches. Compared with these methods, which may leverage knowledge only at the group-level29, techniques based on multivariate approaches, like Machine learning (ML), use information from multiple data sources to classify groups of subjects30 based on parsimonious sets of variables (i.e., signatures). This approach allows classification of individuals at the single-subject level, avoiding a group vs. group perspective31,32. Thus, it may contribute to successfully identify individualized and fine-grained patterns of cognitive and socio-cognitive anomalies in SCZ and BD, as well as to investigate their diagnosis-related or trans-diagnostic relevance.
This study aimed to identify at the single-subject level data-driven cognitive and socio-cognitive signatures of BD and SCZ, and to investigate their trans-diagnostic or diagnosis-specific relevance. Another aim was to investigate if such signatures are also relevant to risk conditions for these diseases or their early stages. With this purpose, we devised a “reversal discovery-validation” ML strategy (Fig. 1—Phase 1 & 2). First, we generated three ML algorithms, hereby called “classifiers”. The first classifier was based on cognition (unimodal classifier), the second on social cognition (unimodal classifier), and the third was a higher-order classifier that learned from the combined decisions of the cognitive and socio-cognitive classifiers (multimodal classifier). Then, we tested the classifiers’ accuracy in predicting the membership of each individual (i) within a cohort including a group of healthy controls (Healthy Controls - group 1: HC1) and BD as well as (ii) within an independent cohort including another group of healthy controls (Healthy Controls - group 2: HC2) and SCZ (Fig. 1—Phase 1; Methods, “Phase 1: generation of unimodal and multimodal classifiers”). Thus, to test the degree of overlaps and specificities of BD- and SCZ-related models, we applied the uni- and multimodal classifiers predicting HC1 and BD memberships to the HC2-SCZ cohort, and vice-versa (Fig. 1—Phase 2; Methods, “Phase 2: reciprocal validation of the generated unimodal and multimodal classifiers”). Finally, to investigate the generalization of our unimodal and multimodal classifiers to earlier stages of disease and psychosis risk, models were applied to independent cohorts of individuals at clinical risk for psychosis (Clinical High Risk—CHR) or earlier stages of disease (First Episode of Psychosis—FEP) via Out Of sample Cross-Validation (OOCV) (Fig. 1—Phase 3; Methods, “Phase 3: investigating the generalization of unimodal and multimodal classifiers”).
To detect cognitive and socio-cognitive similarities and differences between schizophrenia and bipolar disorder, we employed a “reversal discovery-validation strategy”, consisting of two phases: (i) in Phase 1, we generated unimodal and multimodal signatures based on cognitive and socio-cognitive features aimed at discriminating two independent groups of Healthy Controls from two groups of patients suffering from Bipolar Disorder and Schizophrenia, respectively; (ii) in Phase 2, we applied the disease-related models generated in Phase 1 in each cohort to the other one data. In Phase 3, to test the generalizability of disease-related signatures on populations at risk or at early stages of psychosis, we applied the discovery models generated in Phase 1 also to cognitive and socio-cognitive data collected on Clinical High-Risk and First Episode of Psychosis individuals. BD = patients with Bipolar Disorder; CHR = participants with Clinical High Risk for psychosis; FEP = participants at First Episode of Psychosis; HC1 = Healthy Controls (group 1); HC2 = Healthy Controls (group 2); SCZ = patients with Schizophrenia.
Results
Demographic and clinical differences between healthy controls and patients
T-test and χ2 revealed that HC1 differed from BD in terms of age, socio-economic status, current and premorbid IQ (all p < 0.001) (Table 1A). On the other hand, HC2 differed from SCZ in terms of gender, age, socio-economic status, current and premorbid IQ (all p < 0.001) (Table 1B). Furthermore, ANOVAs indicated that CHR and FEP differed from patients and control groups of both HC1-BD and HC2-SCZ cohorts in terms of age, socio-economic status, current and premorbid IQ (all p < 0.05) (Table 2).
Machine learning
Phase 1: classification models between Healthy Controls (group 1) and Bipolar Disorder patients
In order to classify HC1 vs. BD, we built three separate within-cohort Support Vector Machine (SVM) algorithms. SVM is a margin-based statistical technique of supervised learning able to discriminate individuals into two (or more) groups by establishing a linear space of classification (i.e., a hyperplane) on the basis of specific cases called support vectors29. The first algorithm was based on performance at cognitive tests, whereas the second incorporated socio-cognitive measures. The third was a multimodal SVM, i.e., stacking-based, which allows to combine the unimodal classifiers33, integrating their multiple learned decision values and then learning again from this meta-information (Methods, “Phase 1: generation of unimodal and multimodal classifiers”). All the generated classifiers correctly discriminated BD from HC1 better than chance with a permuted significance of p < 0.05. In particular, we used balanced accuracy (BAC) as a measure of model performance, which refers to accuracy calculated in terms of true positive and negative cases, balanced by the sample size of each positive and negative group. BAC is used to optimize performance in models with unbalanced sample sizes29. According to this measure, the stacking-based model had the best classification performance, assigning membership of each individual to BD and HC1 with 80.0% BAC (p = 0.02). The cognitive classifier revealed a cross-validated BAC of 79.8% (p = <0.001), while BAC of the socio-cognitive classifier was 74.4% (p = <0.001) (for detailed classification results, see Table 3A and Fig. 2). To investigate putative association of predicted membership with psychopharmacological treatment or symptom scores, we extracted decision scores from the best-performing classifier (i.e., the stacking-based). Decision scores represent the individual geometric distance from the decision boundary. This resulted in a decision value and a predicted classification label per participant32. Spearman’s test revealed no significant associations between decision scores extracted from the stacking-based classifier and lithium carbonate equivalent dose (Spearman’s rho = −0.103, p = 0.44) or mania as assessed by Young Mania Rating Scale (YMRS)34 (Spearman’s rho = 0.062, p = 0.641) for BD.
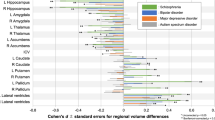
Then, we looked at the features with the highest probability of being selected for HC1 vs. BD classification. With regard to the cognitive classifier, they were the mean accuracy (as the correct response percentage) between loads at the N-back working memory task35, and the global memory IQ score36 (Fig. 3). With regard to the socio-cognitive classifier, they were the total score for the ability to infer paradoxical sarcasm during videotaped interactions, assessed by The Awareness of Social Inference Test (TASIT)37, the accuracy in identifying anger facial expressions, assessed by the Facial Emotion Identification Test (FEIT)38, and the total reaction time at the FEIT (Fig. 3).
Scores closer to 1 represent a higher probability of being selected for decisions by the Support Vector Machine algorithm. Only features with a selection probability >0.5 are shown (complete selection probability results for the whole pool of cognitive and socio-cognitive features are available in SF1A and 1B, respectively). FEIT = Facial Emotion Identification Test; N = number; TASIT II = The Awareness of Social Inference Test – Section II; WMS = Wechsler Memory Scale.
Phase 1: classification models between Healthy Controls (group 2) and Schizophrenia patients
We used the same method described for HC1 vs. BD discrimination to build two unimodal and one stacking-based SVM algorithms for HC2 vs. SCZ classification. Here, all the generated models correctly classified each individual as SCZ or HC2 better than chance with a permuted significance <0.001. As in the HC1 vs. BD analysis, the stacking-based model performed better than the two unimodal classifiers with 84.9% BAC (p = <0.001), while cross-validated BAC was 83.4% (p = <0.001) for the cognitive classifier, and 78.6% (p = <0.001) for the socio-cognitive classifier (for detailed classification results, see Table 3B and Fig. 4). Spearman’s test revealed no significant associations between decision scores extracted from the best-performing classifier (i.e., the stacking-based) and chlorpromazine equivalents (Spearman’s rho = 0.019, p = 0.83) or psychosis-related psychopathology as assessed by Positive And Negative Symptoms Scale (PANSS)39 total score (Spearman’s rho = 0.020, p = 0.828) for SCZ.
Further investigations of the cognitive classifier revealed that the features that mostly contributed to HC2 vs. SCZ discrimination were the 0-back accuracy, the global memory IQ score, the total score of immediate recall for verbal learning40,41, the total score for semantic fluency41 and 1-back efficiency, computed as the ratio between accuracy and reaction times (Fig. 5). With regard to the socio-cognitive classifier, the most relevant features for the HC2 vs. SCZ classification were the TASIT total score of ability to infer lie, global sarcasm, and paradoxical sarcasm, the FEIT accuracy in identifying surprise facial expressions, as well as the FEIT total average response time (Fig. 5).
Scores closer to 1 represent a higher probability of being selected for decisions by the Support Vector Machine algorithm. Only features with a selection probability >0.5 are shown (complete selection probability results for the whole pool of cognitive and socio-cognitive features are available in SF2A and 2B, respectively). FEIT = Facial Emotion Identification Test; N = number; RAVLT = Rey Auditory Verbal Learning Test; SEM. FLUENCY = Semantic Fluency; TASIT II/III = The Awareness of Social Inference Test – Section II/Section III; WMS = Wechsler Memory Scale.
Phase 2: reciprocal validation of the models discriminating between healthy controls and patients
To investigate whether the disease-related signatures built independently for each cohort (i.e., HC1 vs. BD and HC2 vs. SCZ) were disease-specific or able to correctly categorize individuals of the other cohort, we employed an OOCV to apply HC1 vs. BD discriminative models to the HC2-SCZ cohort, and vice-versa (Methods, “Phase 2: reciprocal validation of the generated unimodal and multimodal classifiers”), as already done previously42. OOCV is a technique used when discovery models previously generated by an algorithm are applied to a new set of data collected on independent groups of unseen individuals, with the aim to test signatures’ generalizability31. The application of the models discriminating HC1 vs. BD to the HC2-SCZ cohort revealed that all unimodal and multimodal classifiers assigned group memberships within the HC2-SCZ cohort better than chance, with the highest validation performance for the cognitive classifier (BAC: 78.3%), followed by the stacking-based model (BAC: 77.4%) and the socio-cognitive classifier (BAC: 66.2%) (for detailed classification results, Table 4A).
Applying the models discriminating HC2 vs. SCZ to the HC1-BD cohort indicated that both unimodal and multimodal classifiers assigned group memberships within the HC1-BD cohort better than chance, with the stacking-based model as the best-performing classifier (BAC: 83.1%), followed by the cognitive (BAC: 82.4%) and the socio-cognitive classifier (BAC: 77.9%) (for detailed classification results, Table 4B).
For supplementary models aimed at classifying BD and SCZ using a direct comparison of the two groups of patients, please see Supplementary Information - SI, Section 5.
Phase 3: application of the multimodal classifiers discriminating between healthy controls and patients to First Episode of Psychosis and Clinical High-Risk individuals
Then, we explored the possible generalization of the best-performing HC1 vs. BD and HC2 vs. SCZ classifiers (i.e., stacking-based) to earlier stages of disease and psychosis risk. Specifically, we first applied both the disease-related stacking-based models to CHR and FEP cognitive and socio-cognitive data via OOCV. Then, we used decision scores based on such classifiers as the dependent variable in an ANOVA model (between factor: membership to HC1/HC2, CHR, FEP, BD or SCZ groups) (see Methods, “Phase 3: investigating the generalization of unimodal and multimodal classifiers” for details). The application of the HC1 vs. BD model revealed that decision scores for FEP significantly differed from those for HC1 (p = <0.001), but not from those for BD (p = 0.97), while CHR decision scores differed from both those for HC1 (p < 0.001) and for BD (p = 0.02) (Fig. 6A). When the HC2 vs. SCZ model was applied, FEP decision scores were different from those for HC2 (p < 0.001), but not from those for SCZ (p = 0.95). Differently, CHR decision scores differed from both those for SCZ (p < 0.001) and for HC2 (p < 0.001) (Fig. 6B). In summary, after the application of the HC1 vs. BD and HC2 vs. SCZ stacking models, FEP individuals showed both a BD- and an SCZ-like classification pattern, whereas neither a control nor a patient-like pattern emerged for CHR individuals.
ANOVA analysis were conducted to compare decision scores from the stacking-based models discriminating Healthy Controls (group 1) vs. Bipolar Disorder patients (panel 6A) and Healthy Controls (group 2) vs. Schizophrenia patients (panel 6B) and decision scores extracted for Clinical High Risk and First Episode of Psychosis individuals after the Out-Of-sample-Cross-Validation procedure. Error bars represent standard error.
Discussion
Our results suggest that cognitive and socio-cognitive deficits are relevant to the multimodal categorization of SCZ or BD vs. HC, and that anomalies contributing to such discrimination are mostly disease-specific, with some overlap. On the other hand, multivariate models taking into account the entire set of these cognitive and socio-cognitive impairments are not predictive for differentiation between patients with these two brain disorders. Furthermore, the present findings also suggest a generalization of cognitive and socio-cognitive classifiers categorizing SCZ and BD vs. HC only to first episode of the illness, but not to conditions of clinical liability.
Classification models between healthy controls and patients (Phase 1)
We found that unimodal models based on either cognitive or socio-cognitive characteristics significantly and accurately assigned membership of BD and SCZ to the respective diagnostic groups. Indeed, the combination of these unimodal classifiers in a single stacking model led to the highest discriminative power between classes. These results suggest that cognitive and socio-cognitive profiles of alterations contribute to the phenotypical characterization of schizophrenia and bipolar disorder23.
Analysis of the cognitive and socio-cognitive features contributing the most to the discrimination between BD or SCZ from the respective HC cohorts allows to further characterize this contention. In particular, the most reliable cognitive features for the discrimination of BD were related to overall working memory accuracy and global memory quotient, suggesting a memory-related pattern of alterations consisting of load-independent working memory impairments and multi-domain memory disruptions at the core of the disorder. On the other hand, disruptions within the domain of memory, namely the global memory quotient and load-dependent working memory efficiency, contributed to discriminate SCZ from HC, together with other cognitive deficits related to information processing (0-back accuracy), incidental immediate learning, and semantic fluency. Therefore, a broader pattern of multi-domain cognitive anomalies, already reported by previous literature10,19 and mainly related to basic information processing and verbal-executive components of cognition, emerged for schizophrenia. Taken together, these results suggest that cognitive abnormalities differentiating either BD or SCZ from HC are generally qualitatively different, but commonalities are also present. Interestingly, findings from univariate literature primarily implicate quantitative rather than qualitative differences in cognitive anomalies between BD and SCZ10,43, which may be consistent with the view that a data-driven, multivariate approach is more sensitive to a fine-grained disentanglement of the cognitive asset of these two disorders.
Our results from the socio-cognitive domain may be inserted in a similar explanatory framework. We found that the socio-cognitive variables contributing the most to BD discrimination were the accuracy in identifying angry facial expressions and the global time needed to identify facial emotion expressions. These results appear to delineate a pattern of alterations mainly related to emotion identification processes and are partially consistent with previous univariate literature reporting slower reaction times in BD during emotion recognition44 and decreased accuracy in identifying45 and distinguishing46 anger from other emotions44,47. Results in SCZ indicate that the most reliable features selected to classify between patients and controls were the ability to properly infer both lie and global sarcasm, the ability in identifying surprise facial expressions, and the average response time to correctly identify emotions on faces. Previous literature already reported deficits in enriched social inference in schizophrenia. In particular, a previous study indicated lower performance in SCZ at both lie and sarcasm TASIT subscales when compared with BD and HC individuals, with the latter two groups having similar performance23. Similarly, surprise was already reported as the most misinterpreted emotion by SCZ patients, although within a frame of disrupted emotion recognition48.
Overall, these findings suggest that socio-cognitive features reveal a key discriminative power in discriminating BD or SCZ from HC, which is mostly related to the emotion recognition and social inference broader domains, consistently with previous literature reporting their alteration in both these brain disorders11. Furthermore, as for the cognitive domain discussed above, our findings also suggest both qualitative differences and overlaps in discriminant socio-cognitive features in BD and SCZ vs. HC. Specifically, a broad spectrum of socio-cognitive anomalies, encompassing basic facial emotion identification and both minimal and enriched social inference, emerged for schizophrenia. Differently, BD were discriminated from HC by a prevalent occurrence of emotion identification deficits. A possible interpretation of these results is that SCZ are discriminated by alterations of complex social processes as well as by minimal social inference abilities, while discrimination of BD is mainly supported by the latter. However, it should be noted that also the ability to properly infer paradoxical sarcasm was highly discriminant for classifying both BD and SCZ. Sarcasm comprehension has been previously associated with ToM abilities49 and impairments in this social ability are reported for both disorders, although a greater deficit appears to be present in schizophrenia50. Thus, we may speculate that ToM deficits could trans-diagnostically affect the ability to make judgments on the meaning of conversational remarks both in schizophrenia and bipolar disorder. However, hierarchical models able to better specify the reciprocal relationships among paradoxical sarcasm and ToM abilities need to be developed in the future to validate this view.
Reciprocal validation of the models discriminating between healthy controls and patients (Phase 2)
Results from the between-cohort application of within-cohort generated models indicate high performance of classification for the cognitive, the socio-cognitive, and the stacking-based classifiers, with high discriminative power of all the HC1 vs. BD generated models in the HC2 vs. SCZ comparison, and vice-versa. These results suggest that the overall signatures generated for each disorder are not disease-specific. On the other hand, we found that some of the cognitive and socio-cognitive features discriminating the most between BD vs. HC1 and SCZ vs. HC2 do not overlap, which seems at odds with the generalizability of the overall models between diagnoses. A possible explanation of these seemingly discrepant findings is that the variables selected as most reliably discriminating between HC1 and BD, and between HC2 and SCZ, respectively, were different because our ML pipeline identified deficits that are more “at the core” of each disease at the single-subject level, and therefore representing “hub” cognitive and socio-cognitive diagnosis-related deficits. Despite the identification of these “core”, diagnosis-related alterations, the high generalization of each model to unseen individuals with a different diagnosis proved the non-specificity of the overall bipolar and schizophrenia signatures, suggesting how, at the level of the entire pool of variables, our algorithm may have caught further cognitive and socio-cognitive deficits relevant for both the disorders. Based on this interpretation, our results may support the notion that schizophrenia and bipolar patients are characterized by similar cognitive and socio-cognitive deficits, consistently with previous univariate literature10,11. However, within these deficits, those that are more at the core of each disease are different. Therefore, personalized programs targeted at chronic patients should be oriented to primarily manage disease-related “hub” alterations, but always within a broader framework of intervention aimed to monitor also to the “side”, less central, trans-diagnostic deficits. According to this interpretation, our findings might be considered as a starting evidence corroborating the existence of a psychopathological continuum between schizophrenia and bipolar disorder, emerging at the level of cognitive-behavioral phenotypes. However, as widely reported by previous literature conceptualizing bipolar disorder and schizophrenia as different brain diseases51, cognitive and socio-cognitive deficits in both the disorders might be underpinned by multiple structural and functional abnormalities52,53. Thus, delivering classification models based also on brain features is needed to more deeply investigate—and potentially corroborate—the bipolar disorder-schizophrenia continuum hypothesis. For instance, to build new knowledge useful to better refine current nosology, future machine learning studies generating models based on both behavioral and structural/functional brain data should aim at combining this multivariate information to grasp the possible between-domains latent interactions at the single-subject level.
Application of the multimodal classifiers discriminating between healthy controls and patients to First Episode of Psychosis and Clinical High-Risk individuals (Phase 3)
As a final step, we tested the generalization of each stacking-based signature (i.e., HC1 vs. BD and HC2 vs. SCZ) to earlier stages of diseases and to psychosis risk. Here, FEP decision scores did not differ from those of BD or SCZ when the respective predictive models were applied, while such scores diverged from those of HC individuals. These patterns indicate that, for both HC1 vs. BD and HC2 vs. SCZ models, the algorithm recognizes FEP more as “BD-like” or “SCZ-like”, rather than “HC-like”, suggesting that both BD-related and SCZ-related multimodal signatures generalized to early stages of disease irrespectively from diagnostic boundaries, thus showing trans-diagnostical prognostic relevance.
A different pattern of results was present when both HC1 vs. BD and HC2 vs. SCZ models were separately applied to CHR. Here, CHR decision scores differed from both those of BD and SCZ as well as from those of HC individuals. In other words, for both HC1 vs. BD and HC2 vs. SCZ models, neither patient- nor control-like patterns emerged for CHR, suggesting that cognitive and socio-cognitive features of individuals at clinical risk diverge from those of HC, consistently with the notion that these individuals may be affected by anomalies related to these domains; however, such cognitive and socio-cognitive impairments may not be shaped as those present in full-blown schizophrenia or bipolar disorder yet.
Limitations
Our results should be interpreted considering several limitations. Although we carefully controlled for potential confounding factors including age and sex (see SI, Section 4 for further details about ML preprocessing pipeline), their nonlinear interaction with other external confounds, like medication itself, onset of disease and duration of illness or premorbid intelligence quotient, cannot be ultimately ruled out. However, considering that no significant associations emerged between decision scores extracted from our best models and psychopharmacological treatment or symptoms, it is less likely that these confounders might have affected our results. Moreover, because of the lack of information about non-pharmacological interventions that patients may have undertaken, we could not explore their putative effects on cognitive and socio-cognitive performance. Future studies are warranted to shed light on this possibility.
Although we have employed a stringent double cycle nested Cross-Validation (CV) strategy which should enforce unbiased estimations, further validations of our results in external wider groups of individuals with completely different demographic and geographic profiles are needed to fulfil requirements for generalizability. Indeed, this further evidence would strengthen the potential for translation of our findings into clinical practice and is particularly warranted for the at-risk and FEP cohorts, whereas validation results may have been affected by the small sample size.
Conclusions and future directions
We delivered ML algorithms highlighting that, despite “hub” cognitive and socio-cognitive alterations specifically related to each full-blown diagnosis can be identified, bipolar disorder and schizophrenia share in both domains an overall common pattern of impairments that should therefore be trans-diagnostically approached. Therefore, effective remediation strategies for BD or SCZ individuals should be tailored both on these specific cognitive and socio-cognitive deficits at the core of each disorder, and on less central behavioral alterations. Furthermore, our findings support the potential translation of such trans-diagnostic intervention strategies at earlier stages of diseases (i.e., first-episode individuals). In this framework, we think our results are potentially relevant from a clinical perspective, as they provide ready-to-use information to refine individualized intervention focused on cognitive and socio-cognitive impairments for both the earlier and the chronic phases of the diseases32. Nevertheless, future studies are warranted to further validate our findings and investigate more deeply the relationship between the identified cognitive and socio-cognitive alterations from a trans-diagnostic perspective as well as their potential associations with brain structural and functional underpinnings.
Methods
Sample determination
A total of 546 individuals, all Caucasians native of the Apulia region, Italy, participated in the study. Inclusion and exclusion criteria and full details about sample determination are reported in SII, Section 1. Specifically, our sample included 290 HC and 177 patients, of which 118 were SCZ and 59 were BD, according to the Diagnostic and Statistical Manual of Mental Diseases-5 criteria3. To obtain two cohorts with a proportion between healthy subjects and patients of about 2:1, 95 HC (Healthy Controls - group 1: HC1) randomly entered the first cohort with the BD group (Table 1A), while the remaining 195 HC (Healthy Controls - group 2: HC2) entered the second cohort with the SCZ group (Table 1B).
Moreover, individuals at risk for psychosis or at early stages of disease were also included (Table 2). Specifically, 35 were CHR individuals (i.e., at clinical risk for a first episode of psychosis54,55) and 29 were FEP individuals (i.e., individuals at first episode of psychosis). A detailed description of the clinical characteristics of these cohorts is reported in SI, Section 1.
For all participants, we assessed socio-economic status with the Hollingshead scale56 and the Intelligence Quotient (IQ) using the Wechsler Adult Intelligence Scale-Revised (WAIS-R)57. Furthermore, the Italian version of the Wide Reading Achievement Test (WRAT)58 was employed to measure premorbid IQ. In clinical populations, the Global Assessment of Functioning Scale (GAF)59, the PANSS, and the YMRS were administered to evaluate patients’ global functioning, positive and negative symptoms, global psychiatric symptoms, and manic symptoms.
Two sample t-tests, χ2 tests, and ANOVA were used to investigate group differences in terms of demographic and clinical characteristics, both within (Table 1A, B) and between cohorts (Table 2).
Machine Learning: definition of unimodal classifiers
All participants underwent an extensive assessment protocol, aimed at collecting data about cognitive and socio-cognitive abilities in adult healthy and clinical populations, through different standardized tools (SI, Sections 2–3). Using these cognitive and socio-cognitive measures, we trained:
-
a.
a “cognitive” classifier based on variables from different target cognitive domains previously associated with bipolar disorder2 and schizophrenia60. Specifically, we fed the algorithm with 52 variables, reflecting individual abilities based on psychometric norms from different pen-and-pencil neuropsychological tools, capturing attention (AX Continuous Performance Task – CPT61, TMT – Part A and B), global memory (WMS), incidental (RAVLT) and episodic (Babcock Story Recall Test - BSRT62,63) auditory verbal learning, working memory (N-back), verbal fluency (Phonological and Semantic Fluency Test) and abstract reasoning (Wisconsin Card Sorting Test – WCST64) performance.
-
b.
a “socio-cognitive” classifier based on variables from three social cognition domains of interest, i.e., identification of emotions, social inference, and emotion management, reported as frequently altered in both schizophrenia and bipolar disorder65. In particular, the algorithm was fed by 37 variables, which included domains measured with: (1) the FEIT, which allowed quantifying the individual ability to correctly identify and process emotions from facial expression; (2) the TASIT, which measures the higher-level ability to infer other people’s emotions and thoughts using contextual information during social interactions; the Mayer-Salovey-Caruso Emotional Intelligence Test (MSCEIT)66 which measured the ability to efficiently manage emotional reactions during fictional every-day situations.
SI reports detailed descriptions of the tools administered (Sections 3 and 4), a complete list of the variables which fed ML models (Supplementary Table-ST1), as well as mean and standard deviation performance values of each of these variables (ST2A and ST2B).
Machine Learning: analysis pipeline
Our overall ML analytic strategy consisted of three phases and was carried out using the NeuroMiner software, version 1.05 (www.pronia.eu/neurominer/)30. In particular, to properly detect cognitive and socio-cognitive similarities and differences between schizophrenia and bipolar disorder, we employed a “reversal discovery-validation strategy”, as already done in previous publications42, consisting in two phases, i.e., Phases 1 and 2. In a third step (Phase 3), we investigated how discriminative models generated and validated in the previous phases applied to patients at early stages of disease and at-risk populations.
Phase 1: generation of unimodal and multimodal classifiers
We first generated parsimonious unimodal and multimodal classification models based on our cognitive and socio-cognitive domains of variables to build disease-related signatures, that could discriminate BD and SCZ clinical groups from HC1 and HC2, respectively (see Results, “Phase 1: classification models between Healthy Controls (group 1) and Bipolar Disorder patients” and “Phase 1: classification models between Healthy Controls (group 2) and Schizophrenia patients”).
In our ML pipeline (full details in SI, Section 4) we implemented a double-cycle, repeated nested CV30,42,67, to allow for unbiased estimation of the model’s generalizability, preventing information leaking throughout the strict separation between subjects used for training the models and independent individuals used for testing decisions68. According to this strategy, models trained at the inner CV cycle (CV1) of each unimodal classifier (i.e., cognitive and socio-cognitive) that contributed most to the discriminative pattern between HC1 vs. BD and HC2 vs. SCZ, were then applied to independent test data at the outer CV cycle (CV2). We implemented a 10-fold CV cycle both in the inner CV1 and in the outer CV2 levels, employing a repeated nested CV29. In particular, we permuted the participants within their groups (number of permutations = 5) and repeated the CV cycle for each of these permutations. Thus, within our nested CV framework, we built an ensemble of 50 models (n = 5 repetition × k = 10 folds) for each CV2 partition30,31. All model training steps of parameter optimization, that use group-level statistical procedures for features’ preprocessing, occur only in CV1 training data. Instead, CV1 test data are used to pick hyperparameter combinations that provide potentially good model generalization capacity. Specifically, all the features entering our classifiers underwent three preprocessing steps within CV1:
-
i.
feature-wise scaling was performed to remove between-features differences effect from the training sample information;
-
ii.
scaled data entered a k-Nearest Neighbor imputation step, aimed at filling the missing values for each given subject in the data, using the feature-specific median value computed in the 7 more similar nearest neighbors on the basis of Euclidean distance;
-
iii.
partial correlations were finally performed to regress out the variance associated with age and gender and control for their confounding effect, given the reported association between these variables and the heterogeneity and severity of cognitive69,70 and socio-cognitive71,72 alterations in schizophrenia and bipolar disorder (see SI-Section 4.3 for details).
To assess the discriminative utility of the input variables within each unimodal classifier, we performed a feature selection procedure within the CV1 loop29,42,73. More specifically, after the data entering in a greedy forward search wrapper73, we computed the feature-related probability of being selected for classification purposes within the inner CV loop for each variable, providing maximum prognostic performance with the smallest amount of predictors. This way, we then applied the trained model to CV2 cycle, where generalization error estimation is performed68. Indeed, CV2 validation data, as derived from unseen study participants (i.e., they were not used for training the classification algorithm)68, serve exclusively the purpose to measure the models’ generalizability. With this procedure, we finally obtained parsimonious SVM decision models based on preprocessed cognitive and socio-cognitive features, determining each validation individual’s outcome class (i.e., HC1/HC2 vs. BD/SCZ) through a majority voting procedure across all ensemble models. Classification performance was measured using BAC, sensitivity, specificity, Area-Under-the Curve, Positive Predictive Value, Negative Predictive Value, and Positive Likelihood Ratio. A stacking procedure was further implemented to build a third multimodal classifier74, aimed at combining the unimodal classifiers within the ML environment. Specifically, stacking used the decisions models from our lower-level cognitive and socio-cognitive unimodal classifiers to generate a new, higher-level algorithm that did not learn from domain-specific raw data (i.e., cognition and social cognition performance scores), but from the decisions scores of the unimodal classifiers29. The stacking generalization was performed to investigate whether using all the information coming from both cognition and social cognition would have led to an increase in HC1 vs. BD and HC2 vs. SCZ classification accuracy, compared with the classification ability of single domains-related unimodal classifiers. Permutation analyses were performed to assign statistical significance to the observed classification performance of our models30,75. Specifically, for each permutation, we performed 1000 random permutations of the outcome labels and we retrained all linear SVM models in the repeated nested CV design, using the respective feature subsets resulted from the observed-label analyses. For each permutation, we collected the predictions of the random models into a permuted prediction ensemble for each outer cycle subject. Thus, we built a BAC-based null distribution of out-of-training classification performance. The final calculated significance of the observed out-of-training BAC consisted in the number of events with a permuted out-of-training BAC higher or equal to the observed BAC divided by the number of performed permutations. We set the model significance at α = 0.05. To explore a possible relationship between classification and medication or symptoms severity, we performed non-parametric correlation analyses between decision scores extracted from the best-performing classifiers in both the cohorts and drugs dosages, scores of mania (as assessed by YMRS) and psychosis-related psychopathology (as assessed by PANSS) (α = 0.05, not corrected).
Phase 2: reciprocal validation of the generated unimodal and multimodal classifiers
We applied (i) HC1 vs. BD models to the HC2-SCZ cohort, and vice-versa, (ii) HC2 vs. SCZ models to the HC1-BD cohort using OOCV31,33, without any re-in-between training. Specifically, OOCV is usually required in an ML framework for a thorough generalizability assessment and usually involves the application of the trained models used to predict targets in the CV2 data folds (i.e., HC1 vs. BD and HC2 vs. SCZ models) to a separate dataset that has been independently collected (i.e., HC2-SCZ and HC1-BD data, respectively). Thus, this method allowed us to investigate whether the disease-related signatures built independently for each cohort were disease-specific or had discriminative power also for the other (see Results, “Phase 2: reciprocal validation of the models discriminating between healthy controls and patients”).
Phase 3: investigating the generalization of unimodal and multimodal classifiers
To explore the generalization of the independently generated HC1 vs. BD and HC2 vs. SCZ ML signatures to earlier stages of diseases and to psychosis risk, we compared the performance of the best classifier in assigning membership to HC or patient groups with those obtained applying such classifier to CHR and FEP. With this aim, we performed an OOCV without any in-between retraining as done in Phase 2 (see Methods, “Phase 2: reciprocal validation of the generated unimodal and multimodal classifiers”). Then, we employed an ANOVA to compare the OOCV-based ML decision scores of each of these cohorts, with, respectively, the HC1 vs. BD and the HC2 vs. SCZ decision scores (see Results, “Phase 3: application of the multimodal classifiers discriminating between healthy controls and patients to First Episode of Psychosis and Clinical High-Risk individuals”). Therefore, in terms of decision scores comparison, the presence of a significant difference between CHR or FEP and any other clinical group would suggest that the OOCV-ed algorithm did not classify them as patients. On the other hand, the presence of a significant difference between CHR or FEP and any control group would suggest that the algorithm did not classify them as controls. Finally, the presence of significant differences between CHR or FEP and both controls and clinical cohorts would suggest that CHR and FEP individuals were not comparable either to controls or to patients, based on the rule generated by the OOCV-ed algorithm.
References
Vancampfort, D. et al. Sedentary behavior and physical activity levels in people with schizophrenia, bipolar disorder and major depressive disorder: a global systematic review and meta-analysis. World Psychiatry 16, 308–315 (2017).
Harvey, P. D., Wingo, A. P., Burdick, K. E. & Baldessarini, R. J. Cognition and disability in bipolar disorder: lessons from schizophrenia research. Bipolar Disord. 12, 364–375 (2010).
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596 (2013).
Pearlson, G. D. Etiologic, phenomenologic, and endophenotypic overlap of schizophrenia and bipolar disorder. Annu. Rev. Clin. Psychol. 11, 251–281 (2015).
Lake, C. Schizophrenia and bipolar disorder: No dichotomy, a continuum, or one disease? Psychiatr. Ann. 40, 129–131. (2010).
Crow, T. J. The continuum of psychosis and its implication for the structure of the gene. Br. J. Psychiatry 149, 419–429 (1986).
Moskvina, V. et al. Gene-wide analyses of genome-wide association data sets: evidence for multiple common risk alleles for schizophrenia and bipolar disorder and for overlap in genetic risk. Mol. Psychiatry 14, 252–260 (2009).
International Schizophrenia C, Purcell, S. M. et al. Common polygenic variation contributes to risk of schizophrenia and bipolar disorder. Nature 460, 748–752 (2009).
Craddock, N. & Owen, M. J. The beginning of the end for the Kraepelinian dichotomy. Br. J. Psychiatry 186, 364–366 (2005).
Bortolato, B., Miskowiak, K. W., Kohler, C. A., Vieta, E. & Carvalho, A. F. Cognitive dysfunction in bipolar disorder and schizophrenia: a systematic review of meta-analyses. Neuropsychiatr. Dis. Trea.t 11, 3111–3125 (2015).
Bora, E. & Pantelis, C. Social cognition in schizophrenia in comparison to bipolar disorder: a meta-analysis. Schizophr. Res. 175, 72–78 (2016).
Jiménez-López, E. et al. Neurocognition and functional outcome in patients with psychotic, non-psychotic bipolar I disorder, and schizophrenia. A five-year follow-up. Eur. Psychiatry 56, 60–68 (2019).
Daban, C. et al. Specificity of cognitive deficits in bipolar disorder versus schizophrenia. A systematic review. Psychother. Psychosom. 75, 72–84 (2006).
Reichenberg, A. et al. Neuropsychological function and dysfunction in schizophrenia and psychotic affective disorders. Schizophr. Bull. 35, 1022–1029 (2009).
Trivedi, J. K. et al. Cognitive functions in stable schizophrenia & euthymic state of bipolar disorder. Indian J. Med. Res. 126, 433–439 (2007).
Henry, J. D. & Crawford, J. R. A meta-analytic review of verbal fluency deficits in schizophrenia relative to other neurocognitive deficits. Cogn. Neuropsychiatry 10, 1–33 (2005).
Ragland, J. D. et al. Prefrontal activation deficits during episodic memory in schizophrenia. Am. J. Psychiatry 166, 863–874 (2009).
Laws, K. R. A meta-analytic review of Wisconsin Card Sort studies in schizophrenia: general intellectual deficit in disguise? Cogn Neuropsychiatry 4, 1–30 (1999).
Szoke, A. et al. Longitudinal studies of cognition in schizophrenia: meta-analysis. Br. J. Psychiatry 192, 248–257 (2008).
Bowie, C. R. & Harvey, P. D. Cognition in schizophrenia: impairments, determinants, and functional importance. Psychiatr. Clin. North. Am. 28, 613–633 (2005). 626.
Vohringer, P. A. et al. Cognitive impairment in bipolar disorder and schizophrenia: a systematic review. Front. Psychiatry 4, 87 (2013).
Sheffield, J. M., Karcher, N. R. & Barch, D. M. Cognitive deficits in psychotic disorders: a lifespan perspective. Neuropsychol. Rev. 28, 509–533 (2018).
Lee, J. et al. Social and nonsocial cognition in bipolar disorder and schizophrenia: relative levels of impairment. Am. J. Psychiatry 170, 334–341 (2013).
Barch, D. M. & Sheffield, J. M. Cognitive impairments in psychotic disorders: common mechanisms and measurement. World Psychiatry 13, 224–232 (2014).
Fusar-Poli, P. et al. Heterogeneity of psychosis risk within individuals at clinical high risk: a meta-analytical stratification. JAMA Psychiatry 73, 113–120 (2016).
Bechdolf, A. et al. The predictive validity of bipolar at-risk (prodromal) criteria in help-seeking adolescents and young adults: a prospective study. Bipolar Disord. 16, 493–504 (2014).
Bauer, I. E., Kazimi, I. F., Zeni, C. P. & Soares, J. C. Bipolar Disorder Vulnerability 139–156 (Elsevier, 2018).
Lee, T. Y., Hong, S. B., Shin, N. Y. & Kwon, J. S. Social cognitive functioning in prodromal psychosis: a meta-analysis. Schizophr Res 164, 28–34 (2015).
Dwyer, D. B., Falkai, P. & Koutsouleris, N. Machine learning approaches for clinical psychology and psychiatry. Annu. Rev. Clin. Psychol. 14, 91–118 (2018).
Koutsouleris, N. et al. Multisite prediction of 4-week and 52-week treatment outcomes in patients with first-episode psychosis: a machine learning approach. Lancet Psychiatry 3, 935–946 (2016).
Antonucci, L. A. et al. A pattern of cognitive deficits stratified for genetic and environmental risk reliably classifies patients with schizophrenia from healthy control subjects. Biol. Psychiatry 87, 697–707 (2020).
Antonucci, L. A. et al. Machine learning-based ability to classify psychosis and early stages of disease through parenting and attachment-related variables is associated with social cognition. BMC Psychol. 9, 47 (2021).
Koutsouleris, N. et al. Prediction models of functional outcomes for individuals in the clinical high-risk state for psychosis or with recent-onset depression: a multimodal, multisite machine learning analysis. JAMA Psychiatry 75, 1156–1172 (2018).
Young, R. C., Biggs, J. T., Ziegler, V. E. & Meyer, D. A. A rating scale for mania: reliability, validity and sensitivity. Br. J. Psychiatry 133, 429–435 (1978).
Kirchner, W. K. Age differences in short-term retention of rapidly changing information. J. Exp. Psychol. 55, 352–358 (1958).
Uttl, B., & Graf, P. The Wechsler memory scale-III: validity and reliability. Arch. Clin. Neuropsychol. 8, 705–706 (1999).
McDonald, S. et al. Reliability and validity of The Awareness of Social Inference Test (TASIT): a clinical test of social perception. Disabil. Rehabil. 28, 1529–1542 (2006).
Erol, A., Putgul, G., Kosger, F. & Ersoy, B. Facial emotion recognition in schizophrenia: the impact of gender. Psychiatry Investig. 10, 69–74 (2013).
Kay, S. R., Fiszbein, A. & Opler, L. A. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr. Bull. 13, 261–276 (1987).
Rey, A. L'examen clinique en psychologie. [The clinical examination in psychology]. (Presses Universitaries De France, 1958).
Carlesimo, G. A., Caltagirone, C., Gainotti, G. & Nocentini, U. Batteria per la valutazione del deterioramento mentale: II. Standardizzazione e affidabilità diagnostica nell’identificazione di pazienti affetti da sindrome demenziale. [The Mental Deterioration Battery: II. Standardization and diagnostic reliability in the identification of demented patients.]. Arch. Psicol. Neurol. Psichiatr. 56, 471–488 (1995).
Antonucci, L. A. et al. Multivariate classification of schizophrenia and its familial risk based on load-dependent attentional control brain functional connectivity. Neuropsychopharmacology 45, 613–621 (2020).
Bora, E. & Ozerdem, A. Meta-analysis of longitudinal studies of cognition in bipolar disorder: comparison with healthy controls and schizophrenia. Psychol. Med. 47, 2753–2766 (2017).
Altamura, M. et al. Facial emotion recognition in bipolar disorder and healthy aging. J. Nerv. Ment. Dis. 204, 188–193 (2016).
Bozorg, B., Tehrani-Doost, M., Shahrivar, Z., Fata, L. & Mohamadzadeh, A. Facial emotion recognition in adolescents with bipolar disorder. Iran J. Psychiatry 9, 20–24 (2014).
Goghari, V. M. & Sponheim, S. R. More pronounced deficits in facial emotion recognition for schizophrenia than bipolar disorder. Compr. Psychiatry 54, 388–397 (2013).
Furlong, L. S. et al. Characterization of facial emotion recognition in bipolar disorder: focus on emotion mislabelling and neutral expressions. J. Neuropsychol. 16, 353–372 (2022).
Lee, S. C. et al. Error patterns of facial emotion recognition in patients with schizophrenia. J. Affect. Disord. 300, 441–448 (2022).
Zhu, N. & Wang, Z. The paradox of sarcasm: theory of mind and sarcasm use in adults. Pers. Individ. Differ. 163, 110035 (2020).
Mitchell, R. L. & Young, A. H. Theory of mind in bipolar disorder, with comparison to the impairments observed in schizophrenia. Front. Psychiatry 6, 188 (2015).
Yamada, Y., Matsumoto, M., Iijima, K. & Sumiyoshi, T. Specificity and continuity of schizophrenia and bipolar disorder: relation to biomarkers. Curr. Pharm. Des. 26, 191–200 (2020).
Fernandez-Linsenbarth, I. et al. Neurobiological underpinnings of cognitive subtypes in psychoses: a cross-diagnostic cluster analysis. Schizophr. Res. 229, 102–111 (2021).
Wenzel, J. et al. Cognitive subtypes in recent onset psychosis: distinct neurobiological fingerprints? Neuropsychopharmacology 46, 1475–1483 (2021).
Yung, A. R. et al. Mapping the onset of psychosis: the Comprehensive Assessment of At-Risk Mental States. Aust. N. Z. J. Psychiatry 39, 964–971 (2005).
Fusar-Poli, P. The clinical high-risk state for psychosis (CHR-P), version II. Schizophr. Bull. 43, 44–47 (2017).
Hollingshead, A. B. Four Factor Index of Social Status (1975).
Wechsler D. WAIS-R Manual: Wechsler Adult Intelligence Scale-Revised (Psychological Corporation, 1981).
Colombo, L., Sartori, G. & Brivio, C. J. G. Id. P. Stima del quoziente intellettivo tramite l'applicazione del TIB (test breve di Intelligenza). G. Ital. Psicol. 29, 613–638 (2002).
Hall, R. C. Global assessment of functioning. A modified scale. Psychosomatics 36, 267–275 (1995).
Fioravanti, M., Bianchi, V. & Cinti, M. E. Cognitive deficits in schizophrenia: an updated metanalysis of the scientific evidence. BMC Psychiatry 12, 64 (2012).
Conners, C. K. The computerized continuous performance test. Psychopharmacol. Bull. 21, 891–892 (1985).
Spinnler, H. & Tognoni, G. Standardizzazione e Taratura Italiana di Test Neuropsicologici (Masson Italia Periodici Press, 1987).
Babcock, H. & Levy, L. Test and Manual of Directions; the Revised Examination for the Measurement of Efficiency of Mental Functioning (Stoelting, 1940).
Grant, D. A. & Berg, E. A behavioral analysis of degree of reinforcement and ease of shifting to new responses in a Weigl-type card-sorting problem. J. Exp. Psychol. 38, 404–411 (1948).
Martino, D. J., Samamé, C. & Strejilevich, S. A. Social cognition in schizophrenia and bipolar disorder: Just quantitative differences.? Schizophr. Res. 183, 164–165 (2017).
Mayer, J. & Caruso, D. Mayer-Salovey-Caruso Emotional Intelligence Test (MSCEIT) (2002).
Antonucci, L. A. et al. Using combined environmental-clinical classification models to predict role functioning outcome in clinical high-risk states for psychosis and recent-onset depression. Br. J. Psychiatry 220, 229–245 (2022).
Ruschhaupt, M., Huber, W., Poustka, A. & Mansmann, U. A compendium to ensure computational reproducibility in high-dimensional classification tasks. Stat. Appl. Genet. Mol. Biol. 3, 37 (2004).
Perlick, D., Mattis, S., Stastny, P. & Teresi, J. Gender differences in cognition in schizophrenia. Schizophr. Res. 8, 69–73 (1992).
Rajji, T. K., Ismail, Z. & Mulsant, B. H. Age at onset and cognition in schizophrenia: meta-analysis. Br. J. Psychiatry 195, 286–293 (2009).
Navarra-Ventura, G. et al. Gender differences in social cognition: a cross-sectional pilot study of recently diagnosed patients with schizophrenia and healthy subjects. Can. J. Psychiatry 63, 538–546 (2018).
Green, M. F. et al. Social cognition in schizophrenia, Part 1: performance across phase of illness. Schizophr. Bull. 38, 854–864 (2012).
Saeys, Y., Inza, I. & Larranaga, P. A review of feature selection techniques in bioinformatics. Bioinformatics 23, 2507–2517 (2007).
Wolpert, D. H. Stacked generalization. Neural Netw. 5, 241–259 (1992).
Golland, P. & Fischl, B. Permutation tests for classification: towards statistical significance in image-based studies. Inf. Process. Med. Imaging 18, 330–341 (2003).
Author information
Authors and Affiliations
Consortia
Corresponding authors
Ethics declarations
Competing interests
A.B. reported receiving grants and personal fees from Lundbeck and receiving personal fees from Janssen and from Otsuka during the conduct of the study. G.B. reported receiving personal fees from Lundbeck outside the submitted work. All other authors declare no biomedical financial interests and no potential conflicts of interest. This paper reflects only the authors’ views. The funding bodies had no role in study design, data collection, and analysis, decision to publish, or preparation of the manuscript.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Raio, A., Pergola, G., Rampino, A. et al. Similarities and differences between multivariate patterns of cognitive and socio-cognitive deficits in schizophrenia, bipolar disorder and related risk. Schizophr 9, 11 (2023). https://doi.org/10.1038/s41537-023-00337-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41537-023-00337-0