Abstract
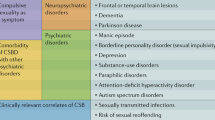
While the pathophysiology of several psychiatric disorders has become modestly elucidated in the last decade, comorbid sexual dysfunctions in such patients are frequently left apart from clinical and research interest. We aimed to address the malfunctioning neurocircuitry underlying sexual dysfunctions in depression, anxiety, schizophrenia and mania. We performed a comprehensive literature review, addressing any combination of the topics of “neurobiology”/“neural”, “sexual”/“desire”/“arousal”/“orgasm”/“ejaculation” and “depression”/“anxiety”/“schizophrenia”/“mania”/“bipolar”. Altered neurotransmitter levels or connectivity in patients are reported in sexual dysfunctions (either desire, arousal, orgasm and ejaculation) and main psychiatric disorders (depression, anxiety, mania and schizophrenia). Neuronal pathways responsible for the occurrence of sexual dysfunctions in psychiatric disorders can be figured out by overlap of their acknowledged pathophysiology. However, specific research in that group is scant, so future tailored studies are warranted to elucidate actual mechanisms.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Waldinger MD. Psychiatric disorders and sexual dysfunction. Handb Clin Neurol. 2015;130:469–89.
Waldinger MD. Not medical solutions, but overmedicalization by pharmaceutical company policies endanger both sexological care, science, and sexual medicine. A commentary. J Sex Marital Ther. 2008;34:179–83.
Freud S, Haute Pv, Westerink H, Freud S, Freud S. Three essays on the theory of sexuality: the1905 edition. London; New York: Verso; 2016. xc, p. 111.
Tharoor H, Kaliappan A, Gopal S. Sexual dysfunctions in schizophrenia: professionals and patients perspectives. Indian J Psychiatry. 2015;57:85–7.
Atlantis E, Sullivan T. Bidirectional association between depression and sexual dysfunction: a systematic review and meta-analysis. J Sex Med. 2012;9:1497–507.
Shabsigh R, Zakaria L, Anastasiadis AG, Seidman AS. Sexual dysfunction and depression: etiology, prevalence, and treatment. Curr Urol Rep. 2001;2:463–7.
Labbate LA, Lare SB. Sexual dysfunction in male psychiatric outpatients: validity of the Massachusetts General Hospital Sexual Functioning Questionnaire. Psychother Psychosom. 2001;70:221–5.
Harley EW, Boardman J, Craig T. Sexual problems in schizophrenia: prevalence and characteristics. A cross sectional survey. Soc Psychiatry Psychiatr Epidemiol. 2010;45:759–66.
Jonusiene G, Griffioen, T. Psychiatric disorders and sexual dysfunctions. In: Kirana PS, Tripodi, F, Reisman, Y, Porst, H, editors. The EFS and ESSM Syllabus of Clinical Sexology. Amsterdam: Medix; 2013.
Basson R. A model of women’s sexual arousal. J Sex Marital Ther. 2002;28:1–10.
McKenna KE. Neural circuitry involved in sexual function. J Spinal Cord Med. 2001;24:148–54.
Chapelle PA, Durand J, Lacert P. Penile erection following complete spinal cord injury in man. Br J Urol. 1980;52:216–9.
Dean RC, Lue TF. Physiology of penile erection and pathophysiology of erectile dysfunction. Urol Clin North Am. 2005;32:379–95.
Argiolas A, Melis MR. Central control of penile erection: role of the paraventricular nucleus of the hypothalamus. Prog Neurobiol. 2005;76:1–21.
Rubio-Aurioles E, Bivalacqua TJ. Standard operational procedures for low sexual desire in men. J Sex Med. 2013;10:94–107.
Cacioppo S, Bianchi-Demicheli F, Frum C, Pfaus JG, Lewis JW. The common neural bases between sexual desire and love: a multilevel kernel density fMRI analysis. J Sex Med. 2012;9:1048–54.
Seok JW, Sohn JH, Cheong C. Neural substrates of sexual arousal in heterosexual males: event-related fMRI investigation. J Physiol Anthropol. 2016;35:8.
Cheng JC, Secondary J, Burke WH, Fedoroff JP, Dwyer RG. Neuroimaging and sexual behavior: identification of regional and functional differences. Curr Psychiatry Rep. 2015;17:55.
Poeppl TB, Langguth B, Laird AR, Eickhoff SB. The functional neuroanatomy of male psychosexual and physiosexual arousal: a quantitative meta-analysis. Hum Brain Mapp. 2014;35:1404–21.
Georgiadis JR, Kringelbach ML. The human sexual response cycle: brain imaging evidence linking sex to other pleasures. Prog Neurobiol. 2012;98:49–81.
Georgiadis JR. Functional neuroanatomy of human cortex cerebri in relation to wanting sex and having it. Clin Anat. 2015;28:314–23.
Pfaus JG. Pathways of sexual desire. J Sex Med. 2009;6:1506–33.
Graf H, Walter M, Metzger CD, Abler B. Antidepressant-related sexual dysfunction—perspectives from neuroimaging. Pharmacol Biochem Behav. 2014;121:138–45.
Veening JG, de Jong TR, Waldinger MD, Korte SM, Olivier B. The role of oxytocin in male and female reproductive behavior. Eur J Pharmacol. 2015;753:209–28.
Rowland DL. Neurobiology of sexual response in men and women. CNS Spectr. 2006;11(8 Suppl 9):6–12.
Lorrain DS, Riolo JV, Matuszewich L, Hull EM. Lateral hypothalamic serotonin inhibits nucleus accumbens dopamine: implications for sexual satiety. J Neurosci. 1999;19:7648–52.
Argiolas A, Melis MR. Neuropeptides and central control of sexual behaviour from the past to the present: a review. Prog Neurobiol. 2013;108:80–107.
Jesulola E, Micalos P, Baguley IJ. Understanding the pathophysiology of depression: From monoamines to the neurogenesis hypothesis model—are we there yet? Behav Brain Res. 2018;341:79–90.
Laurent SM, Simons AD. Sexual dysfunction in depression and anxiety: conceptualizing sexual dysfunction as part of an internalizing dimension. Clin Psychol Rev. 2009;29:573–85.
Friedman A, Deri I, Friedman Y, Dremencov E, Goutkin S, Kravchinsky E, et al. Decoding of dopaminergic mesolimbic activity and depressive behavior. J Mol Neurosci. 2007;32:72–9.
Nestler EJ, Carlezon WA Jr.. The mesolimbic dopamine reward circuit in depression. Biol Psychiatry. 2006;59:1151–9.
Fitzgerald PB, Srithiran A, Benitez J, Daskalakis ZZ, Oxley TJ, Kulkarni J, et al. An fMRI study of prefrontal brain activation during multiple tasks in patients with major depressive disorder. Hum Brain Mapp. 2008;29:490–501.
Anand A, Li Y, Wang Y, Gardner K, Lowe MJ. Reciprocal effects of antidepressant treatment on activity and connectivity of the mood regulating circuit: an FMRI study. J Neuropsychiatry Clin Neurosci. 2007;19:274–82.
Opel N, Redlich R, Grotegerd D, Dohm K, Zaremba D, Meinert S, et al. Prefrontal brain responsiveness to negative stimuli distinguishes familial risk for major depression from acute disorder. J Psychiatry Neurosci. 2017;42:343–52.
Stoy M, Schlagenhauf F, Sterzer P, Bermpohl F, Hagele C, Suchotzki K, et al. Hyporeactivity of ventral striatum towards incentive stimuli in unmedicated depressed patients normalizes after treatment with escitalopram. J Psychopharmacol. 2012;26:677–88.
Yang JC. Functional neuroanatomy in depressed patients with sexual dysfunction: blood oxygenation level dependent functional MR imaging. Korean J Radiol. 2004;5:87–95.
Stoleru S, Redoute J, Costes N, Lavenne F, Bars DL, Dechaud H, et al. Brain processing of visual sexual stimuli in men with hypoactive sexual desire disorder. Psychiatry Res. 2003;124:67–86.
Serretti A, Chiesa A. Sexual side effects of pharmacological treatment of psychiatric diseases. Clin Pharmacol Ther. 2011;89:142–7.
Clayton AH, El Haddad S, Iluonakhamhe JP, Ponce Martinez C, Schuck AE. Sexual dysfunction associated with major depressive disorder and antidepressant treatment. Expert Opin Drug Saf. 2014;13:1361–74.
Duval ER, Javanbakht A, Liberzon I. Neural circuits in anxiety and stress disorders: a focused review. Ther Clin Risk Manag. 2015;11:115–26.
Hilbert K, Lueken U, Beesdo-Baum K. Neural structures, functioning and connectivity in Generalized Anxiety Disorder and interaction with neuroendocrine systems: a systematic review. J Affect Disord. 2014;158:114–26.
Pietrini F, Godini L, Lazzeretti L, Benni L, Pracucci C, Talamba GA, et al. [Neuroimaging and neurobiology of social anxiety]. Riv Psichiatr. 2010;45:349–60.
Shackman AJ, Stockbridge MD, Tillman RM, Kaplan CM, Tromp DP, Fox AS, et al. The neurobiology of dispositional negativity and attentional biases to threat: implications for understanding anxiety disorders in adults and youth. J Exp Psychopathol. 2016;7:311–42.
Barlow DH. Causes of sexual dysfunction: the role of anxiety and cognitive interference. J Consult Clin Psychol. 1986;54:140–8.
Beck JG, Barlow DH. The effects of anxiety and attentional focus on sexual responding—II. Cognitive and affective patterns in erectile dysfunction. Behav Res Ther. 1986;24:19–26.
Carvalho J, Nobre P. Biopsychosocial determinants of men’s sexual desire: testing an integrative model. J Sex Med. 2011;8:754–63.
Bancroft J, Janssen E, Strong D, Carnes L, Vukadinovic Z, Long JS. The relation between mood and sexuality in heterosexual men. Arch Sex Behav. 2003;32:217–30.
Corona G, Mannucci E, Petrone L, Ricca V, Balercia G, Giommi R, et al. Psycho-biological correlates of free-floating anxiety symptoms in male patients with sexual dysfunctions. J Androl. 2006;27:86–93.
Dvorak RD, Wray TB, Kuvaas NJ, Kilwein TM. Mania and sexual risk: associations with behavioral self-regulation. J Affect Disord. 2013;150:1076–81.
Dell’Osso L, Carmassi C, Carlini M, Rucci P, Torri P, Cesari D, et al. Sexual dysfunctions and suicidality in patients with bipolar disorder and unipolar depression. J Sex Med. 2009;6:3063–70.
Kopeykina I, Kim HJ, Khatun T, Boland J, Haeri S, Cohen LJ, et al. Hypersexuality and couple relationships in bipolar disorder: a review. J Affect Disord. 2016;195:1–14.
Strakowski SM, Eliassen JC, Lamy M, Cerullo MA, Allendorfer JB, Madore M, et al. Functional magnetic resonance imaging brain activation in bipolar mania: evidence for disruption of the ventrolateral prefrontal-amygdala emotional pathway. Biol Psychiatry. 2011;69:381–8.
Pomarol-Clotet E, Alonso-Lana S, Moro N, Sarro S, Bonnin MC, Goikolea JM, et al. Brain functional changes across the different phases of bipolar disorder. Br J Psychiatry. 2015;206:136–44.
Fleck DE, Eliassen JC, Durling M, Lamy M, Adler CM, DelBello MP, et al. Functional MRI of sustained attention in bipolar mania. Mol Psychiatry. 2012;17:325–36.
Blumberg HP, Stern E, Martinez D, Ricketts S, de Asis J, White T, et al. Increased anterior cingulate and caudate activity in bipolar mania. Biol Psychiatry. 2000;48:1045–52.
Seok JW, Sohn JH. Neural substrates of sexual desire in individuals with problematic hypersexual behavior. Front Behav Neurosci. 2015;9:321.
King R, Raese JD, Barchas JD. Catastrophe theory of dopaminergic transmission: a revised dopamine hypothesis of schizophrenia. J Theor Biol. 1981;92:373–400.
Heilbronner U, Samara M, Leucht S, Falkai P, Schulze TG. The longitudinal course of schizophrenia across the lifespan: clinical, cognitive, and neurobiological aspects. Harv Rev Psychiatry. 2016;24:118–28.
Drake CR, Pathe M. Understanding sexual offending in schizophrenia. Crim Behav Ment Health. 2004;14:108–20.
Phillips SL, Heads TC, Taylor PJ, Hill GM. Sexual offending and antisocial sexual behavior among patients with schizophrenia. J Clin Psychiatry. 1999;60:170–5.
de Boer MK, Castelein S, Wiersma D, Schoevers RA, Knegtering H. The facts about sexual (dys)function in schizophrenia: an overview of clinically relevant findings. Schizophr Bull. 2015;41:674–86.
Hocaoglu C, Celik FH, Kandemir G, Guveli H, Bahceci B. Sexual dysfunction in outpatients with schizophrenia in Turkey: a cross-sectional study. Shanghai Arch Psychiatry. 2014;26:347–56.
Dembler-Stamm T, Fiebig J, Heinz A, Gallinat J. Sexual dysfunction in unmedicated patients with schizophrenia and in healthy controls. Pharmacopsychiatry. 2018. https://doi.org/10.1055/s-0044-100627.
Baggaley M. Sexual dysfunction in schizophrenia: focus on recent evidence. Hum Psychopharmacol. 2008;23:201–9.
Kirino E. Serum prolactin levels and sexual dysfunction in patients with schizophrenia treated with antipsychotics: comparison between aripiprazole and other atypical antipsychotics. Ann Gen Psychiatry. 2017;16:43.
Zhang XR, Zhang ZJ, Zhu RX, Yuan YG, Jenkins TA, Reynolds GP. Sexual dysfunction in male schizophrenia: influence of antipsychotic drugs, prolactin and polymorphisms of the dopamine D2 receptor genes. Pharmacogenomics. 2011;12:1127–36.
Mete D, Dafreville C, Paitel V, Wind P. [Aripiprazole, gambling disorder and compulsive sexuality]. Encephale. 2016;42:281–3.
Cheon E, Koo BH, Seo SS, Lee JY. Two cases of hypersexuality probably associated with aripiprazole. Psychiatry Investig. 2013;10:200–2.
Ucok A, Incesu C, Aker T, Erkoc S. Do psychiatrists examine sexual dysfunction in schizophrenia patients? J Sex Med. 2008;5:2000–1.
Rademacher L, Schulte-Ruther M, Hanewald B, Lammertz S. Reward: from basic reinforcers to anticipation of social cues. Curr Top Behav Neurosci. 2017;30:207–21.
Williams DR, Burkner PC. Effects of intranasal oxytocin on symptoms of schizophrenia: a multivariate Bayesian meta-analysis. Psychoneuroendocrinology. 2017;75:141–51.
Peeters M, Giuliano F. Central neurophysiology and dopaminergic control of ejaculation. Neurosci Biobehav Rev. 2008;32:438–53.
Veening JG, Coolen LM. Neural mechanisms of sexual behavior in the male rat: emphasis on ejaculation-related circuits. Pharmacol Biochem Behav. 2014;121:170–83.
Alwaal A, Breyer BN, Lue TF. Normal male sexual function: emphasis on orgasm and ejaculation. Fertil Steril. 2015;104:1051–60.
Clement P, Giuliano F. Physiology and pharmacology of ejaculation. Basic Clin Pharmacol Toxicol. 2016;119(Suppl 3):18–25.
Stoneham MD, Everitt BJ, Hansen S, Lightman SL, Todd K. Oxytocin and sexual behaviour in the male rat and rabbit. J Endocrinol. 1985;107:97–106.
Waldinger MD. Ejaculatio praecox, erectio praecox, and detumescentia praecox as symptoms of a hypertonic state in lifelong premature ejaculation: a new hypothesis. Pharmacol Biochem Behav. 2014;121:189–94.
Agmo A, Berenfeld R. Reinforcing properties of ejaculation in the male rat: role of opioids and dopamine. Behav Neurosci. 1990;104:177–82.
Kennedy SH, Rizvi S. Sexual dysfunction, depression, and the impact of antidepressants. J Clin Psychopharmacol. 2009;29:157–64.
Fabre LF, Clayton AH, Smith LC, Goldstein IM, Derogatis LR. Association of major depression with sexual dysfunction in men. J Neuropsychiatry Clin Neurosci. 2013;25:308–18.
Waldinger MD. Pharmacotherapy for premature ejaculation. Expert Opin Pharmacother. 2015;16:2615–24.
Bijlsma EY, Chan JS, Olivier B, Veening JG, Millan MJ, Waldinger MD, et al. Sexual side effects of serotonergic antidepressants: mediated by inhibition of serotonin on central dopamine release? Pharmacol Biochem Behav. 2014;121:88–101.
Waldinger MD, Berendsen HH, Blok BF, Olivier B, Holstege G. Premature ejaculation and serotonergic antidepressants-induced delayed ejaculation: the involvement of the serotonergic system. Behav Brain Res. 1998;92:111–8.
Corona G, Petrone L, Mannucci E, Jannini EA, Mansani R, Magini A, et al. Psycho-biological correlates of rapid ejaculation in patients attending an andrologic unit for sexual dysfunctions. Eur Urol. 2004;46:615–22.
Mourikis I, Antoniou M, Matsouka E, Vousoura E, Tzavara C, Ekizoglou C, et al. Anxiety and depression among Greek men with primary erectile dysfunction and premature ejaculation. Ann Gen Psychiatry. 2015;14:34.
Rajkumar RP, Kumaran AK. The association of anxiety with the subtypes of premature ejaculation: a chart review. Prim Care Companion CNS Disord. 2014;16:4.
McMahon CG, Jannini EA, Serefoglu EC, Hellstrom WJ. The pathophysiology of acquired premature ejaculation. Transl Androl Urol. 2016;5:434–49.
Xia J, Chen T, Chen J, Han Y, Xu Z, Zhou L, et al. The sympathetic skin response located in the penis as a predictor of the response to sertraline treatment in patients with primary premature ejaculation. J Sex Med. 2014;11:2801–8.
Kempeneers P, Andrianne R, Cuddy M, Blairy S. Sexual cognitions, trait anxiety, sexual anxiety and distress in men with different subtypes of premature ejaculation and in their partners. J Sex Marital Ther. 2017;44:319–32.
Lyketsos GC, Sakka P, Mailis A. The sexual adjustment of chronic schizophrenics: a preliminary study. Br J Psychiatry. 1983;143:376–82.
Fan X, Henderson DC, Chiang E, Briggs LB, Freudenreich O, Evins AE, et al. Sexual functioning, psychopathology and quality of life in patients with schizophrenia. Schizophr Res. 2007;94:119–27.
Malik P, Kemmler G, Hummer M, Riecher-Roessler A, Kahn RS, Fleischhacker WW, et al. Sexual dysfunction in first-episode schizophrenia patients: results from European First Episode Schizophrenia Trial. J Clin Psychopharmacol. 2011;31:274–80.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Trovão, J.N., Serefoglu, E.C. Neurobiology of male sexual dysfunctions in psychiatric disorders: the cases of depression, anxiety, mania and schizophrenia. Int J Impot Res 30, 279–286 (2018). https://doi.org/10.1038/s41443-018-0077-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-018-0077-8
This article is cited by
-
Relationship between hyperuricemia with deposition and sexual dysfunction in males and females
Journal of Endocrinological Investigation (2022)
-
Frequency of etiological factors among patients with acquired premature ejaculation: prospective, observational, single-center study
International Journal of Impotence Research (2020)
-
Psychiatric Comorbidities and Sexual Health
Current Sexual Health Reports (2020)