Abstract
Toll-like receptors (TLR) are crucial components in the initiation of innate immune responses to a variety of pathogens, triggering the production of pro-inflammatory cytokines and type I and II interferons, which are responsible for innate antiviral responses. Among the different TLRs, TLR7 recognizes several single-stranded RNA viruses including SARS-CoV-2. We and others identified rare loss-of-function variants in X-chromosomal TLR7 in young men with severe COVID-19 and with no prior history of major chronic diseases, that were associated with impaired TLR7 signaling as well as type I and II IFN responses. Here, we performed RNA sequencing to investigate transcriptome variations following imiquimod stimulation of peripheral blood mononuclear cells isolated from patients carrying previously identified hypomorphic, hypofunctional, and loss-of-function TLR7 variants. Our investigation revealed a profound impairment of the TLR7 pathway in patients carrying loss-of-function variants. Of note, a failure in IFNγ upregulation following stimulation was also observed in cells harboring the hypofunctional and hypomorphic variants. We also identified new TLR7 variants in severely affected male patients for which a functional characterization of the TLR7 pathway was performed demonstrating a decrease in mRNA levels in the IFNα, IFNγ, RSAD2, ACOD1, IFIT2, and CXCL10 genes.
Similar content being viewed by others
Introduction
Coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [1], has rapidly developed into a global pandemic of enormous consequences. COVID-19 is characterized by a broad spectrum of clinical manifestations in humans, ranging from asymptomatic to mild symptomatic to severe pneumonia accompanied by multiorgan failure [2]. Older age, male sex, hypertension, diabetes, and obesity are all indicators identified as risk factors predisposing to severe disease [2]. In addition, and perhaps underlying some of these indicators, specific genetic factors may more precisely explain the predisposition of some individuals to develop severe disease requiring hospitalization and even admission to intensive care units [2]. Increasing evidence suggests that defects in responsiveness to type I interferons (IFN-I) are of prime importance. Indeed, genetic variants that decrease IFN-I production and the development of anti-IFN-I autoantibodies have been associated with more severe COVID-19 [3,4,5,6,7]. Recently, two studies in young men with severe COVID-19 and no history of major chronic diseases identified rare loss-of-function (LOF) variants in X-chromosomal TLR7 that were associated with impaired TLR7 signaling as well as type I and II IFN responses [4, 5]. Another study revealed that at least 3.5% of patients with life-threatening COVID-19 pneumonia had genetic mutations at candidate loci known to be involved in TLR3- and IRF7-dependent induction and amplification of IFN-I [7].
Interferons are rapidly produced following viral infection and induce potent first-line defense mechanisms against viruses that are key in host–virus standoff [8]. The initial sensing of pathogens is mediated by innate pattern recognition receptors that include Toll-like receptors (TLRs). The intracellular signaling cascades triggered by TLRs lead to the transcriptional expression of inflammatory mediators that coordinate the elimination of pathogens and infected cells. Interestingly, among the different TLRs, TLR7 binds to single-stranded RNA viruses, such as influenza A virus, HIV-1, hepatitis C virus, HBV RNA intermediates, and SARS-CoV-2 as well as binding to synthetic guanine-rich RNA sequence analogs such as imiquimod (IMQ) [9,10,11,12,13]. Upon virus infection or agonist stimulation, TLR7 dimerizes in the endosome to initiate TLR7-mediated MyD88 signal transduction, resulting in the activation of mitogen-activated protein kinase cascades and NF-κB [14]. Signaling in human immune cells by TLR7 has been documented to trigger production of pro-inflammatory cytokines, including tumor necrosis factor α (TNF-α), interleukin (IL)-6, IL-1β, and IL-12 as well as IFN-I. IFN-I regulates a range of immune responses through the IFN-I receptor, resulting in the transcription of hundreds of IFN-stimulated genes (ISGs) whose joint action leads to the generation of an “antiviral state” [8, 14].
To gain insight into TLR7-linked mechanisms of severe COVID-19, we performed RNA sequencing (RNA-Seq) to carefully characterize transcriptome variations following IMQ stimulation of peripheral blood mononuclear cells (PBMC) isolated from patients carrying previously identified LOF TLR7 variants [5]. In addition, we found new TLR7 variants in severely affected males for which functional characterization of the pathway was also performed.
Results and discussion
To study more deeply the functional effects of TLR7 variants, after TLR7 stimulation with IMQ in comparison with unstimulated cells, we performed RNA-Seq experiments on PBMC from healthy donors (HDs) and from patients carrying the functionally hypomorphic variants Ala288Val and Ala448Val, the hypofunctional variant Val219Ile, and the LOF variants Ala1032Thr and Ser301Pro. As shown in Fig. 1A, B, we observed several differentially expressed genes (DEGs) in the HDs as well as in the patients carrying hypomorphic and hypofunctional variants. In contrast, when LOF variants were analyzed, no DEGs were found (Fig. 1C). Specifically, TLR7 stimulation induced a strong response in HDs with 211 genes significantly upregulated (log2 fold change (FC) ≥ 1.5; adjusted p value ≤ 0.05) and 19 downregulated genes (log2FC ≤ −1.5; adjusted p value ≤ 0.05) compared with unstimulated PBMC. The genes displaying the top 50 absolute FC are listed in Fig. 1A. We used the Gene Ontology (GO) database to perform GO-biological process enrichment analysis of DEGs. Cytokine-mediated signaling and cellular response to interferons were upregulated pathways in HDs (Fig. 1A, lower panel). Patients carrying hypomorphic or hypofunctional variants displayed 108 upregulated genes (log2FC ≥ 1.5; adjusted p value ≤ 0.05) and 5 downregulated genes (log2FC ≤ −1.5; adjusted p value ≤ 0.05), most of which were the same observed in HDs (Fig. 1B). The GO-biological process enrichment analysis identified the same upregulated pathways (Fig. 1B, lower panel). Interestingly, RNA-seq analysis in patients carrying LOF variants showed that none had genes with an adjusted p value ≤ 0.05 (Fig. 1C), suggesting a profound impairment of the TLR7 pathway. As shown in the heat map (Fig. 1D), for most of the 50 genes with the highest FC in HDs after IMQ stimulation we noticed a significant upregulation in patients carrying hypomorphic and hypofunctional variants but not in patients with LOF variants. A notable exception was IFNγ for which a failure to induce upregulation following stimulation was also observed in cells harboring the hypofunctional and hypomorphic variants. It has been shown that at around day 10 in subjects with COVID-19, IFN-I decreased while IFNγ remained stable [15], promoting the resolution of lung inflammation. Therefore, administration of IFN-I might be considered a therapeutic option for TLR7 mutated patients. The efficacy of IFN-I therapy would depend on whether it is administered early in the course of the disease. Patients with a severe course of COVID-19 are usually admitted to the hospital after a few days at home making it difficult to identify those in need of IFN-I treatment. Indeed, inappropriate administration of IFN-I to the wrong patients or at the wrong time point could be counterproductive by triggering the cytokine storm. A more attractive therapeutic option would be IFNγ, which is not only useful in patients with hypomorphic mutations but, in addition, can stabilize the inflammatory response and does not require timely administration.
A–C Volcano plots showing DEGs. Red dots show upregulated genes (log2FC ≥ 1.5 with adjusted p value ≤ 0.05) and blue dots represent downregulated genes (log2FC ≤ −1,5; adjusted p value ≤ 0.05). The DEGs with the top 50 absolute FC are reported. A Three healthy donors. B Patients (n = 3) carrying the Ala288Val, Ala488Val, and Val219 Ile variants. C Patients carrying Ala1032Thr (n = 1) and Ser301Pro (n = 1) variants. Gene Ontology biological process terms significantly overrepresented among the genes increased by IMQ are shown in the lower panel in (A, B, D). Heatmap of logCPM values for the top DEGs in HDs and patients carrying TLR7 variants after IMQ stimulation. IMQ imiquimod, NS non stimulated.
As shown in Fig. 1, in HDs and in patients carrying hypomorphic and hypofunctional variants, but not in patients carrying LOF variants, TLR7 engagement triggered an antiviral response upregulating typical antiviral ISGs (RSAD2, APOBEC3A, HERC5, OASs, MXs, IFITs, and IFITMs family genes) as well as proinflammatory cytokine and chemokine genes (IL6, CXCL10, CXCL11, CCL8, CCL2, CCL7) [8]. Interestingly, IL6 and CXCL10 were found to be involved in the mechanisms sustaining the cytokine-storm, a peculiar aspect of SARS-COV-2 infection which, at least in severe cases, is responsible for diffuse alveolar damage and multi-organ failure [16]. Furthermore, IFITMs inhibit cellular entry of SARS-CoV and MERS-CoV [17]. We also observed upregulation of CCL2 and CCL7, two pivotal chemokines for monocyte recruitment, both of which were found enriched in bronchoalveolar fluid (BALF) from patients with severe COVID-19 [18, 19]. Moreover, the TNFSF10 gene (TRAIL), an apoptosis-related gene that was previously found to be upregulated in BALF and PBMC from COVID-19 patients [20], was also upregulated after IMQ stimulation in HD and in patients carrying hypomorphic and hypofunctional variants. Meanwhile, we observed a marked induction of negative regulators (such as USP18, IL1RN, and ACOD1), suggesting stimulation of negative feedback loops. The functional status of the cells was evaluated by stimulating PBMC from patients and HDs with the TLR4 agonist lipopolysaccharide (LPS). Intracellular production of IL6 was evaluated in monocytes (as shown in Supplementary Fig. 1). The frequencies of CD3−CD14+IL6+ cells were comparable in patients and HDs, indicating that cells from patients harboring TLR7 variants were functionally active. IFNα and IFNγ protein production was evaluated in the supernatant of PBMC from HDs and from a small number of patients after TLR7 engagement. The data showed a trend toward a lower production of IFNα as well as IFNγ proteins in patients carrying LOF TLR7 variants. The patient carrying the hypomorphic variant Ala288Val showed a reduced, though not statistically significant, production of IFNα protein after TLR7 engagement (Supplementary Fig. 2). Overall, the transcriptomic profile of cells harboring LOF TLR7 variants showed a wide deficiency of ISGs while both hypomorphic and LOF mutations displayed a reduction of IFNγ transcription.
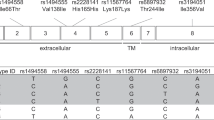
We next extended the analysis to two additional rare TLR7 variants: the already reported Arg920Lys variant (P6) [5], and the new Asp41Glu (P10) variant predicted to be deleterious from in silico analysis (Fig. 2A). The two variants were identified in two severely affected male patients aged 49 and 79 years, one in each. In order to functionally characterize the TLR7 pathway, we performed a gene expression profile analysis of PBMC from patient P6 and from two relatives of patient P10 following stimulation with IMQ. We found a statistically significant decrease in mRNA levels for IFNα and IFNγ genes in P6, P10-II-I, and P10-II-III compared with HDs (Fig. 2B, C). We further analyzed some of the genes showing the highest FC in the HDs transcriptomic profile and observed a significant decrease of mRNAs encoding for RSAD2, ACOD1, and IFIT2 genes in P6, demonstrating a profound impairment of the TLR7 signaling pathway in response to TLR7 stimulation (Fig. 2D–F). Of note, it was reported that RSAD2, in addition to the role of direct suppressor of viral replication, promotes TLR7- and TLR9-mediated production of IFNα. [21]. Moreover, we observed that CXCL10 mRNA was markedly reduced in P6, P10-II-I, and P10-II-III compared with HDs (Fig. 2G). Overall, our data expand previous findings on the TLR7 role in rare Mendelian forms of COVID-19 and provide further insights into the altered pathways that might contribute to disease severity.
A Pedigree of P6 (A upper panel) and P10 (A lower panel) shows the segregation of the variant within the family. Squares represent male family members; circles, females. Black symbols indicate individuals harboring the TLR7 variant. Individuals infected by SARS-CoV-2 are indicated by a virus symbol () close to the individual symbol. B–G PBMC from COVID-19 patients and four unaffected male controls (HDs) were stimulated with IMQ at 5 μg/mL or cell culture medium. A quantitative PCR assay was performed and 2−ΔΔCt was calculated using HPRT1 as the housekeeping gene. Fold change in mRNA expression of genes induced by IMQ with respect to cell culture medium was calculated: *p < 0.05; **p < 0.01; ***p < 0.001.
Materials and methods
Male COVID-19 patients were selected from the Italian GEN-COVID cohort [5]. Cases were selected according to the following inclusion criteria: (i) male gender; (ii) young age (<60 years); and (iii) detection of rare variants in TLR7. Exclusion criteria were: (i) SARS-CoV-2 infection not confirmed by PCR. Relatives of patients 6 and 10 were contacted to obtain a blood sample. Segregation analysis of the variants was performed with Sanger sequencing on an ABI3130 Genetic Analyzer. PBMC isolation, IMQ stimulation, and qPCR were performed as previously described [5]. The primers used are listed in Supplementary Table 1. Supernatants of PBMCs stimulated with IMQ, LPS, or medium alone were measured for IFNα (Invitrogen) and IFNγ production (Bio-Techne) according to the manufacturer’s instructions. PBMC were stimulated in vitro with LPS at 1 µg/ml for 4 h, then IL6 production was examined in CD3− CD14+ cells by flow cytometry. Briefly, 3 × 105 PBMC were stained with anti-CD3 BV605 and anti-CD14 BB700 mAbs, fixed and permeabilized with the BD Cytofix/Cytoperm kit in the presence of anti-IL6 BV421 (Becton Dickinson) according to the manufacturer’s instructions. RNA quality was assessed by Fragment Bioanalyzer (Agilent); all samples exhibited RNA quality numbers greater than 8. The libraries for RNA-seq were performed according to the Illumina TruSeq Stranded mRNA Library preparation protocol and sequenced in multiplex with HiSeq 2500 platform (Illumina) in 50 nucleotides, paired-end read configuration. Sequencing data were analyzed using the BioJupies platform [22].
WES and Genotype (GWAS) data were generated within the GEN-COVID Data Repository (GCGDR). In order to be able to store and analyze the massive amount of genomic data generated with the analysis of the entire cohort of samples populating the biobank, we relied on the NIG. External users can upload and analyze data using the NIG pipeline by registering and creating a specific project. A section dedicated to COVID-19 samples has been created within the NIG database (http://nigdb.cineca.it/) that provides variant frequencies as a free tool for both clinicians and researchers.
References
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. China Novel Coronavirus Investigating and Research Team. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020;382:727–33.
Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. J Am Med Assoc. 2020;323:2052–9.
Park A, Iwasaki A. Type I and Type III interferons—induction, signaling, evasion, and application to combat COVID-19. Cell Host Microbe. 2020;27:870–8.
van der Made CI, Simons A, Schuurs-Hoeijmakers J, van den Heuvel G, Mantere T, Kersten S, et al. Presence of genetic variants among young men with severe COVID-19. J Am Med Assoc. 2020;324:1–11.
Fallerini C, Daga S, Mantovani S, Benetti E, Picchiotti N, Francisci D, et al. Association of Toll-like receptor 7 variants with life-threatening COVID-19 disease in males: findings from a nested case-control study. Elife. 2021;10:e67569.
Bastard P, Rosen LB, Zhang Q, Michailidis E, Hoffmann HH, Zhang Y, et al. Autoantibodies against type I IFNs in patients with life-threatening COVID-19. Science. 2020;370:eabd4585.
Zhang Q, Bastard P, Liu Z, Le Pen J, Moncada-Velez M, Chen J, et al. Inborn errors of type I IFN immunity in patients with life-threatening COVID-19. Science. 2020;370:eabd4570.
Grandvaux N, tenOever B. R, Servant M. J, Hiscott J. The interferon antiviral response: from viral invasion to evasion. Curr Opin Infect Dis. 2002;15(Jun):259–67.
Lee J, Wu CC, Lee KJ, Chuang TH, Katakura K, Liu YT, et al. Activation of anti-hepatitis C virus responses via Toll-like receptor 7. Proc Natl Acad Sci USA. 2006;103:1828–33.
Heil F, Hemmi H, Hochrein H, Ampenberger F, Kirschning C, Akira S, et al. Species-specific recognition of single-stranded RNA via toll-like receptor 7 and 8. Science. 2004;303:1526–9.
Isogawa M, Robek MD, Furuichi Y, Chisari FV. Toll-like receptor signaling inhibits hepatitis B virus replication in vivo. J Virol. 2005;79:7269–72.
Poulas K, Farsalinos K, Zanidis C. Activation of TLR7 and innate immunity as an efficient method against COVID-19 pandemic: imiquimod as a potential therapy. Front Immunol. 2020;11:1373.
Mele D, Mantovani S, Oliviero B, Grossi G, Ludovisi S, Mondelli MU, et al. Hepatitis C virus inhibits CD4 T cell function via binding to Toll-like receptor 7. Antiviral Res. 2017;137:108–11.
Petes C, Odoardi N, Gee K. The Toll for trafficking: Toll-like receptor 7 delivery to the endosome. Front Immunol. 2017;8:1075.
Galani IE, Rovina N, Lampropoulou V, Triantafyllia V, Manioudaki M, Pavlos E, et al. Untuned antiviral immunity in COVID-19 revealed by temporal type I/III interferon patterns and flu comparison. Nat Immunol. 2021 Jan;22:32–40.
Coperchini F, Chiovato L, Croce L, Magri F, Rotondi M. The cytokine storm in COVID-19: an overview of the involvement of the chemokine/chemokine-receptor system. Cytokine Growth Factor Rev. 2020;53:25–32.
Huang IC, Bailey CC, Weyer JL, Radoshitzky SR, Becker MM, Chiang JJ, et al. Distinct patterns of IFITM-mediated restriction of filoviruses, SARS coronavirus, and influenza A virus. PLoS Pathog. 2011;7:e1001258.
Shi C, Pamer EG. Monocyte recruitment during infection and inflammation. Nat Rev Immunol. 2011;11:762–74.
Zhou Z, Ren L, Zhang L, Zhong J, Xiao Y, Jia Z, et al. Heightened innate immune responses in the respiratory tract of COVID-19 patients. Cell Host Microbe. 2020;27:883–890.e2.
Xiong Y, Liu Y, Cao L, Wang D, Guo M, Jiang A, et al. Transcriptomic characteristics of bronchoalveolar lavage fluid and peripheral blood mononuclear cells in COVID-19 patients. Emerg Microbes Infect. 2020;9:761–70.
Saitoh T, Satoh T, Yamamoto N, Uematsu S, Takeuchi O, Kawai T, et al. Antiviral protein Viperin promotes Toll-like receptor 7- and Toll-like receptor 9-mediated type I interferon production in plasmacytoid dendritic cells. Immunity. 2011;34:352–63.
Torre D, Lachmann A, Ma'ayan A. BioJupies: automated generation of interactive notebooks for RNA-seq data analysis in the cloud. Cell Syst. 2018;7:556–561.
Acknowledgements
This study is part of the GEN-COVID Multicenter Study, https://sites.google.com/dbm.unisi.it/gen-covid, the Italian multicenter study aimed at identifying the COVID-19 host genetic bases. Specimens were provided by the COVID-19 Biobank of Siena, which is part of the Genetic Biobank of Siena, member of BBMRI-IT, of Telethon Network of Genetic Biobanks (project No. GTB18001), of EuroBioBank, and of RD-Connect. We thank the CINECA consortium for providing computational resources and the Network for Italian Genomes (NIG; http://www.nig.cineca.it) for its support. We thank private donors for the support provided to AR (Department of Medical Biotechnologies, University of Siena) for the COVID-19 host genetics research project (D.L n.18 of March 17, 2020). We also thank the COVID-19 Host Genetics Initiative (https://www.covid19hg.org/), MIUR project “Dipartimenti di Eccellenza 2018–2020” to the Department of Medical Biotechnologies University of Siena, Italy, and “Bando Ricerca COVID-19 Toscana” project to Azienda Ospedaliero-Universitaria Senese. We thank Intesa San Paolo for the 2020 charity fund dedicated to the project N B/2020/0119 “Identificazione delle basi genetiche determinanti la variabilità clinica della risposta a COVID-19 nella popolazione italiana”. Generous support was also received from private donations by Mrs. Maurizio Traglio, Enzo Cattaneo, and Alberto Borella. We thank Francis P. Crawley for revising the paper. We thank the CINECA consortium for providing computational resources and the Network for Italian Genomes (NIG) http://www.nig.cineca.it for its support. We thank private donors for the support provided to A.R. (Department of Medical Biotechnologies, University of Siena) for the COVID-19 host genetics research project (D.L n.18 of March 17, 2020). We also thank the COVID-19 Host Genetics Initiative (https://www.covid19hg.org/); MIUR project “Dipartimenti di Eccellenza 2018–2020” to the Department of Medical Biotechnologies University of Siena, Italy. We also thank Intesa San Paolo for the 2020 charity fund dedicated to the project N. B/2020/0119 “Identificazione delle basi genetiche determinanti la variabilità clinica della risposta a COVID-19 nella popolazione italiana” and the Tuscany Region for funding within “Bando Ricerca COVID-19 Toscana” project supporting research at the Azienda Ospedaliero-Universitaria Senese. We also thank Mrs. Maurizio Traglio, Enzo Cattaneo and Alberto Borella for private donations.
Author information
Authors and Affiliations
Consortia
Contributions
Conceptualization: SM, SD, CF, IM, MUM, and AR. Data curation: SM, SD, CF, IM, FM, AR, MUM, and GEN‐COVID Multicenter Study. Formal analysis: SM, SD, CF, EB, NP, and SF. Funding acquisition: AR. Investigation: MB, SA, IM, EF, FM, and AR. Methodology: MB, FF, AG, SZ, MB, MP, SC, SA, DA, and KC. Resources: AR and MUM; Software: SM, SD, EB, NP, and SF; Supervision: EF, IM, FM, AR, and MUM. Validation: IM, AR, and MUM. Visualization: CG, CF, MB, FF, CF, AR, and RM. Writing-original draft: SM, SD, CF, EF, IM, AR, and MUM. All authors have reviewed and approved the paper.
Corresponding authors
Ethics declarations
Ethics
The GEN-COVID study was performed in accordance with the relevant international, EU, national, and institutional guidelines and approved in advance by the University Hospital (Azienda Ospedaliero-Universitaria Senese) Ethical Review Board, Siena, Italy (Prot n. 16917, dated March 16, 2020). Clinical trial registration NCT04549831. Patients or legally authorized representatives provided informed consent for participating in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mantovani, S., Daga, S., Fallerini, C. et al. Rare variants in Toll-like receptor 7 results in functional impairment and downregulation of cytokine-mediated signaling in COVID-19 patients. Genes Immun 23, 51–56 (2022). https://doi.org/10.1038/s41435-021-00157-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41435-021-00157-1
This article is cited by
-
COVID-19 annual update: a narrative review
Human Genomics (2023)
-
The dynamic interface of genetics and immunity: toward future horizons in health & disease
Genes & Immunity (2023)
-
The role of TLR7 agonists in modulating COVID-19 severity in subjects with loss-of-function TLR7 variants
Scientific Reports (2023)
-
A comprehensive SARS-CoV-2–human protein–protein interactome reveals COVID-19 pathobiology and potential host therapeutic targets
Nature Biotechnology (2023)
-
Rare predicted loss-of-function variants of type I IFN immunity genes are associated with life-threatening COVID-19
Genome Medicine (2023)