Abstract
We present a novel comprehensive literature review of studies of the psychosocial functioning (PF) and quality of life (QoL) of patients with childhood glaucoma and their caregivers. Our findings demonstrate variable study quality and approach, as well as inconsistent results relating to the association of glaucoma-specific factors and sociodemographic variables with measured PF and QoL. Future studies should focus on the development of culturally cognizant and standardized assessment tools, execution of multi-center longitudinal studies with global representation, evaluation of PF and QoL among siblings and childhood glaucoma providers, and implementation of interventions to improve patient and caregiver PF and QoL.
摘要
我们对儿童青光眼患者和其监护人的心理功能 (PF) 和生活质量 (QoL) 进行了全新以及具有深度的文献回顾。研究结果表明, 该方面研究的质量和方法各不相同, 而且关于青光眼特定因素和社会人口变量与测定的PF和QoL之间的关系的结果也不一致。未来的研究应集中于开发具有文化认知并经过标准化的评估工具, 开展具有全球代表性的多中心纵向研究, 评估兄弟姐妹和儿童青光眼病例提供者的PF和QoL, 以及实施干预措施来改善患者及监护人的PF和QoL。
Similar content being viewed by others
Introduction
While literature exists on the effects of childhood glaucoma on psychosocial functioning (PF) and quality of life (QoL) from the perspective of the patient or family, there is no consensus on the magnitude of the impact of this diagnosis on patients and family members. Extrapolations from studies on other pediatric vision disorders [1,2,3,4,5,6,7,8,9] and chronic pediatric conditions [10,11,12,13] imply that childhood glaucoma may have significant outcomes on the QoL of the patient, caregivers, and siblings [14]. Patient-reported outcome measures (PROMs) allow clinicians to better understand the patient’s perception of their own well-being and functioning with regard to their disease [15]. Increased clinical implementation of PROMs and other psychosocial tools in recent years has revealed an association between pediatric patient or caregiver QoL and treatment adherence and disease outcome [16,17,18,19]. We review the literature regarding PF and QoL in childhood glaucoma, and the tools available for their assessment. This review will provide a synthesis of existing literature, highlight the relevance of these factors in the holistic care of patients with glaucoma and their families, and emphasize the importance of including this type of data in studies of clinical and surgical outcomes in childhood glaucoma. We hope to motivate further research in this area with the goal of improving overall health outcomes for patients with childhood glaucoma and their caregivers.
Childhood glaucoma
Childhood or pediatric glaucoma (henceforth referred to as “childhood glaucoma”) is classified into two diagnostic categories: primary glaucoma and secondary glaucoma [20]. Primary glaucoma is not associated with other ocular or systemic diseases and is classified by age of onset into primary congenital glaucoma (PCG) and juvenile open-angle glaucoma (JOAG). Secondary glaucoma may be associated with either a non-acquired systemic disease, syndrome, or ocular anomaly or with acquired conditions such as trauma or inflammation. A separate category exists for glaucoma following cataract surgery [20, 21]. In this review, “childhood glaucoma” will encompass all childhood glaucoma diagnoses.
Prevalence and incidence
Due to a lack of data, an accurate estimate of the global prevalence or incidence of childhood glaucoma cannot be determined. Ethnicity and consanguinity are believed to influence rates of glaucoma [22], further complicating the global approximation of cases. Glaucoma accounts for 0–7% of pediatric blindness depending on the region [23, 24], and it is estimated that one in 10,000 babies in the United States is born with PCG [25], and that a general ophthalmologist may encounter one new case of PCG every five years [26, 27]. In one U.S. county with an incidence of 2.29 cases of childhood glaucoma per 100,000 residents under age 20, most cases were secondary, either non-acquired or acquired, while PCG and JOAG were rare [28].
Health outcomes
Childhood glaucoma is characterized by elevated intraocular pressure (IOP) and its effects on the structures of the young eye. These will vary depending on the age of onset and the severity and duration of the elevated IOP. If left untreated, elevated pressure damages the optic nerve, leading to loss of the optic nerve fibers and producing “cupping” of the nerve head; these structural changes manifest functionally as progressive and irreversible vision loss including blindness [29]. Other clinical features include progressive myopia, photosensitivity, eye enlargement (buphthalmos), watery eyes (epiphora), and cloudiness (corneal edema). Thus, not only does childhood glaucoma cause visual disability, it can also involve cosmetic changes which may impact the patient’s emotional adjustment or self-esteem as has been reported in pediatric cases such as skin disorders [30, 31] and Marfan syndrome [32].
Because childhood glaucoma is rare with sometimes subtle or unfamiliar clinical presentations, it can be diagnosed late or misdiagnosed altogether [26]. In many areas, access to ophthalmologists with training or expertise in childhood glaucoma is limited, compounding delays in diagnosis and treatment [26, 33]. In addition to negative ocular health outcomes, childhood glaucoma and its associated management and follow-up can significantly impact the patient and immediate family members’ PF and QoL, which will be the focus of the rest of the review.
Defining key concepts
Psychosocial functioning
Although the term lends itself to variable interpretations, PF is defined by Ro and Clark according to four domains: well-being, basic functioning, self-mastery, and interpersonal and social relationships. In general, it is the ability of an individual to engage in daily activity, partake in societal roles, and develop social relationships.
Well-being refers to an individual’s life satisfaction and self-acceptance while basic functioning encompasses mobility, participation in society, and physical ability. Self-mastery relates to internal self-control, and lastly, interpersonal, and social relationships pertain to empathy and agreeableness [34].
Quality of life
QoL is an individual’s subjective perception of life in the context of their culture, society, environment, and expectations, as defined by the World Health Organization, and encompasses physical, psychological, and social health [35]. Studies sometimes refer to QoL as it pertains to vision in three ways: health-related (HR-QoL) [36, 37], vision-related (VR-QoL) [38], and functional vision (FV) [36] (also referred to as functional visual ability or visual functioning). However, it is important to note that these are distinct, though related, constructs.
HR-QoL is the subset of QoL and refers to the individual’s perception of their physical or mental health status [39, 40]. VR-QoL, similar to HR-QoL, defines an individual’s perception of their well-being as it pertains to their vision [38, 41]. FV is a different and distinct concept that measures an individual’s visual ability to perform daily activities or tasks [42, 43], rather than the impact of the individual’s vision on their well-being, which is assessed by QoL measures. Unfortunately, many studies and published instruments conflate QoL and FV [44].
Patient-reported outcome measures
PROMs assess the patient’s own perception of their status with respect to their health or specific diagnosis and can measure any of the following different concepts: HR-QoL, functional status, symptoms, or health behavior [45].
Caregiver
Caregiver encompasses both formal (i.e., ophthalmologist) and informal caregivers (i.e., parents and siblings) and refers to any person who helps an individual with childhood glaucoma with their disease management or activities of daily living [46].
Because the current review encompasses no study involving caregivers other than parents, “caregivers” hereafter solely describes parents of individuals with childhood glaucoma.
Most relevant to this review is the caregiver burden; the multidimensional, self-perceived strain a person may feel for caring for their family member, loved one, or patient over time [47].
Disease and psychosocial function/quality of life
Relationship between chronic pediatric conditions and PF or QoL
The effects of the physical limitations and treatment demands from various chronic pediatric conditions extend beyond the patient’s physical health status. For instance, children and young people with chronic health conditions are at higher risk for mental health problems (e.g., anxiety and depression), and psychosocial, behavioral, and academic impairment as compared to their peers without the chronic disease [10, 11, 48,49,50,51].
From an early age, children with chronic disease depend on their caregivers for support with treatment, medical appointments, and activities of daily living, resulting in caregivers experiencing physical and mental health complications [52,53,54,55,56], extensive time demands [55], financial burden [55, 57], family stress or patient-caregiver tension [58], and low QoL [59, 60]. The caregivers’ QoL may impact the care they provide, affecting patient medication adherence and, in turn, disease outcome, patient QoL, and psychosocial adjustment [16, 18, 19]. Everhart et al. [16] report that this relationship can operate in the reverse direction as well, where improved medication adherence results in the improved health status of the child, minimizing caregiver anxiety.
Disease factors of childhood glaucoma that may affect PF or QoL
Childhood glaucoma and visual impairment may physically limit the patient, restricting their academic, social, and extracurricular activities. It is a lifelong disease demanding routine visits or procedures with a physician that, extrapolating from chronic pediatric diseases previously mentioned, may impose a financial, timewise, and personal opportunity cost for the patient, caregivers, and family unit [14]. Almost all cases of childhood glaucoma require chronic eye drop use, prescription glasses, and/or surgery, with more than a third (39.4%) needing more than one procedure [61]. Prescription glasses negatively affect children’s self-esteem [62] and administering eye drops in pediatric patients may be distressing for the child and caregiver because of discomfort and patient resistance [62, 63], hindering therapy compliance and potentially impacting disease progression. Such progression leads to impaired vision, which studies link to higher levels of depression [64,65,66] and a greater independent risk factor for suicide [67] than neurological disorders and malignant disease [68].
Furthermore, the progressive nature of vision disorders such as glaucoma leads to illness and prognosis uncertainty, which correlates positively with patient depression and anxiety [69]. Although limited literature exists on this relationship for caregivers of individuals with vision disorders, studies performed on other pediatric conditions report a negative impact of illness uncertainty on caregiver well-being [58, 70]. This risk can be mitigated by improving health literacy (e.g., knowledge and expectations of disease, treatment, or other health factors) for patients and caregivers, which decreases patient anxiety [71] and improves medication adherence [72]. By enhancing patient and caregiver understanding of childhood glaucoma, individuals are more likely to comply with treatment, potentially improving their physical and mental health outcomes.
By reviewing the current literature and exploring assessment tools available on childhood glaucoma, the authors hope to encourage PF and QoL support initiatives in an effort to improve childhood glaucoma outcomes.
Method of literature search
Database and search terms
The authors performed the initial literature search through the PubMed database in August 2021 and repeated the search twice more (in March and April 2022). One author (DEM) performed the database search and screened papers by inclusion criteria, which was later verified by two subsequent authors (AS and HM). The authors used the following combinations of search terms or closely related ones: “Childhood glaucoma OR pediatric glaucoma OR glaucoma” AND “quality of life OR life experience OR caregiver burden OR mental health OR psychology OR psychosocial OR family psychology OR cognitive development OR academic function”.
The authors conducted the search in two stages: once without an age filter to capture caregivers, parents, immediate family member participants, and adults who were diagnosed with glaucoma at a pediatric age and a second time with an age filter to include only newborn, infant, preschool child, child, and adolescent patients. For both stages, authors screened articles by topic based on their titles or abstract. The authors excluded papers pertaining to eye diseases other than glaucoma or papers on topics unrelated to PF or QoL. The search with the age filter did not contribute any articles not previously captured by the unfiltered search.
Inclusion and exclusion criteria
The authors used the following inclusion criteria when selecting literature: (1) original abstracts available in English; (2) research studies of any methodology; (3) studies from any country of publication; (4) studies from any year of publication; (5) study participants who were diagnosed with glaucoma at a pediatric age or study participants who were considered to be parent, caregiver, or immediate family member of a patient with childhood glaucoma; and (6) studies on the topic of PF or QoL. The authors excluded literature if (1) the paper was on any disease not relevant to childhood glaucoma, (2) the paper was on any topic not relevant to PF or QoL, and (3) it was a literature review and/or meta-analysis paper.
All identified papers included an English language abstract. The authors used Google Translate for papers with an English abstract and non-English articles.
Results
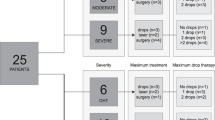
The initial database search yielded 2396 papers (Fig. 1) and, following the inclusion and exclusion criteria previously outlined, the database search resulted in the identification of 22 papers.
This outlines the number of papers included in the review (“n”) after screening sequentially by titles, abstracts, and full texts (white boxes on the left). It also includes the number of papers removed (“n”) due to an irrelevant topic or population identified through each screening step (grey boxes on the right).
Out of 22 papers, 2 [73, 74] focused solely on questionnaire development and validation, while the remaining 20 measured aspects of PF and QoL in patients with childhood glaucoma and their caregivers with two studies also assessing the psychometric properties of the questionnaire used [37, 75]. Alternatively, one study measured the agreement between the patients’ and caregivers’ report of the patient’s HR-QoL [76]. Most studies (n = 13) focused on children and young people with glaucoma [36,37,38, 71, 75,76,77,78,79,80,81,82], while others (n = 9) studied caregivers of these patients [38, 73, 83,84,85,86,87,88,89].
Many of the included papers investigated associations between the main outcomes (i.e., QoL or FV) and at least one clinical, treatment, or disease-specific factor. For instance, the studies most frequently compared PF or QoL findings to glaucoma type or laterality [36,37,38, 75, 77, 78, 83, 85, 88, 90], visual acuity (VA) [36,37,38, 75, 77,78,79, 82, 83, 88, 90], age at or duration since diagnosis [36, 38, 77, 79, 83, 86, 87], medication or treatment practices [36, 71, 75, 77,78,79, 81,82,83, 88], and number and outcomes of glaucoma surgeries [36, 38, 75, 77,78,79, 81,82,83, 85,86,87,88]. In relation to family and broader sociodemographic characteristics, researchers most frequently compared outcome measures to age, gender, marital status, parental education level, employment status, household income, socioeconomic status, and presence of another child with glaucoma in the family [36,37,38, 75, 77,78,79, 81, 83, 85,86,87,88, 90].
The findings of the present literature review are discussed from the perspective of patients with childhood glaucoma and their caregivers.
The impact of childhood glaucoma on patients
The summary of studies on patients with childhood glaucoma is outlined in Table 1, with correlates and predictors of QoL and/or FV presented in Table 2. Most studies investigated associations between different clinical and sociodemographic factors and QoL and/or FV, with only one study measuring other factors.
Psychosocial functioning and quality of life of individuals with childhood glaucoma: associated clinical, management, treatment, and glaucoma-specific factors
The majority of studies reported possible differences in patient’s QoL and FV in relation to their VA. The results across the studies measuring VR-QoL were mostly consistent, with seven papers reporting worse QoL in cases of increasing visual field deviation [79, 81], worse VA [36, 38, 77,78,79, 82], or worse postoperative VA [75]. Though, one study found the association with VA not to be important [81]. Conversely, studies measuring HR-QoL [37] or generic QoL and life satisfaction [90] did not find their association with the level of VA and visual field mean deviation to be significant. Similar to VR-QoL, worse FV was also related to worse VA [36, 38, 77].
As for glaucoma factors, some studies found children with bilateral glaucoma to have significantly worse VR-QoL [77], HR-QoL [36], as well as satisfaction with life [90] and FV [36, 38] compared to children with unilateral glaucoma. One study [38] also found laterality to be a significant independent predictor of FV scores. Five papers reported laterality not to be associated with VR-QoL [36, 38, 78], HR-QoL [37], or generic QoL [90]. Type of glaucoma did not play an important role in QoL or in FV [77] in most cases [37, 75, 77]. One study observed that children with secondary childhood glaucoma reported significantly worse VR-QoL and FV than children with PCG despite comparable VA [38].
Children’s age at diagnosis or duration since diagnosis did not have a significant impact on either FV [38, 77] or QoL [38, 77, 79]. QoL was not associated with age at surgery [90] or time since the last surgery [37, 79], though children reported better self-care scores after a successful surgery compared to children with an unsuccessful surgery [75]. Most studies did not find a connection between number of glaucoma surgeries and patient QoL [38, 78, 79, 81, 82], except for one study that reported worse VR-QoL in children who underwent three or more surgeries [77]. Two studies observed poor FV (self-reported difficulty to complete an activity due to vision) in children who underwent one or more surgeries [38] and more than three surgeries [77]. Consistently, other types of medical treatment or application of medication (e.g., eye drops, antiglaucoma medication, number of clinic visits) were not associated with QoL in children with glaucoma [36, 77,78,79, 81, 82]. With regard to FV, one study observed that children who required less daily eye drops had better FV scores [77].
Glaucoma knowledge and expectations of eye care significantly impact family’s PF and well-being [71, 82]. In one study [71], an educational program on glaucoma resulted in participants reporting more accurate knowledge about glaucoma and disease causes. Patients also improved their attitudes and practices toward glaucoma care and future health. Importantly, participants demonstrated significantly fewer difficulties with activities of daily living, higher self-esteem, and improved mental health. In another study [82], patient and family QoL factors were evaluated. Significant psychosocial indicators included knowledge of glaucoma, treatment adherence, present social support, future expectations from the point of optimism, and uncertainty surrounding the child’s diagnosis.
Psychosocial functioning and quality of life of individuals with childhood glaucoma: associated sociodemographic factors and characteristics of patient and family
Studies assessed the relationship between PF and QoL measures and sociodemographic factors, such as age, gender, and ethnicity. The majority of these studies did not find age or gender to be associated with QoL [36,37,38, 75, 77,78,79, 90] or FV scores [36, 38]. However, one study found patients of young age (8–11 years old) and female gender to report worse HR-QoL and showed greater disagreement with parental reports than adolescent and male patients, respectively [76]. Only one study looked at potential ethnicity-related differences, but did not find an association with VR-QoL scores [78]. In a study on young adults with childhood glaucoma [90], married adults reported higher life satisfaction, and marital status explained 8.8% of the variance in the participants’ life satisfaction scores. The authors also found that adults living in rural environments and with higher education levels reported better overall QoL, together explaining the 13% of the variance in the participants’ QoL scores. Interestingly, the socioeconomic status of these participants did not play a role in their QoL or life satisfaction. Parental education level was not associated with children’s VR-QoL or FV [77]. A cross-sectional study measuring personality characteristics found introverted children to report significantly lower scores on social and mental domains of VR-QoL compared to those of extroverted children [75]. However, it is important to note that the authors did not specify how these personality traits were measured and categorized in the two groups.
The impact of childhood glaucoma on caregivers
The summary of studies on caregivers to patients with childhood glaucoma is outlined in Table 3 and correlates and predictors of QoL and/or FV for those caregivers are presented in Table 4. Caregiver outcomes related to PF were measured as mental health, caregiver burden, positive aspects of caregiving, and QoL, with most studies also assessing their relationship to different clinical and sociodemographic factors.
Psychosocial functioning and quality of life of caregivers of individuals with childhood glaucoma: the impact of the diagnosis
In contrast to the results of studies focusing on the patient, caregiver studies reported few significant associations between PF or QoL and glaucoma-specific factors. The child’s age at diagnosis was not significantly associated with caregiver QoL [83, 86, 88]; however, caregivers whose child had a longer duration of glaucoma reported significantly worse QoL [86] and more time-dependent and overall burden [87] compared to caregivers of children with more recent diagnoses. Furthermore, those caregivers with children with worse best-corrected visual acuity (BCVA) reported significantly lower QoL [83] and more anxiety and depression symptoms [88] compared to that of caregivers of children with better BCVA. Caregivers were also at higher risk for moderate-to-severe anxiety and depression if their child had undergone a surgical procedure [88]. Interestingly, one study found improved caregiver QoL following their child’s surgical procedure, regardless of the surgical outcome [85]. Three studies did not find the number of surgeries to have an impact on caregiver QoL [83, 86, 87]. The strongest negative predictor of caregiver QoL in one study was the number of additional children with glaucoma [83], though a separate study [85] found no association between additional children with glaucoma and change in caregiver QoL before and after their child underwent surgery. Other glaucoma-related factors such as age at surgery [85], glaucoma medication [83, 88], laterality [83, 85], type of glaucoma [83, 88], and PCG severity [85] were not associated with caregiver QoL, mental health, or the level of caregiver burden.
Psychosocial functioning and quality of life of caregivers of individuals with childhood glaucoma: associated sociodemographic, caregiver, and family characteristics
One study found that 20% of caregivers reported anxiety symptoms, with 8.5% experiencing moderate-to-severe anxiety [88]. Depression or depressive symptoms were highly prevalent among caregivers of children with glaucoma and were negatively associated with caregiver QoL [86]. The prevalence of depressive symptoms among caregivers varied across studies (23.6% [88], 44% [86], and 69.1% [84]), which may be explained by unaccounted transient situations. For example, one study revealed that 71% of caregivers demonstrated poor to very poor pre-operative QoL with associated agitation, irritability, depression, anxiety and powerlessness, though this prevalence dropped to 20% post-operation [85].
Not surprisingly, emotional, socioeconomic and overall burdens likewise increased with the severity of depression [84]. Between 47.4 and 71% of caregivers experienced a moderate burden, and between 5% and 8.8% of caregivers felt severely burdened from caring for children with glaucoma [84, 86].
In another study, outcomes of caregiving were measured using a questionnaire that ranged from levels of positive aspects to levels of the burden of caregiving and assessed self–affirmation (e.g., increasing meaning to life) and outlook on life (e.g., positive attitude). Although a majority of caregivers showed some level of burden, most reported a moderate level of positive aspects of caregiving for children with glaucoma [87]. Only emotional burden was negatively related to the overall positive aspects of caregiving, indicating caregivers whose children behave more unpredictably were also more likely to feel unappreciated and less useful within the context of caregiving. Sociodemographic or family factors did not play an important role in the positive experience of caregiving [87].
Most studies did not find QoL to be related to caregiver sociodemographic characteristics, such as age [85, 86], gender [85, 86], marital status [83, 85], socioeconomic status, average household income [85, 86], or employment status [83, 85]. Similarly, most studies found child gender [83, 85, 86, 88] and age [83] unrelated to caregiver QoL and mental health, though caregivers of older children with PCG reported worse QoL compared to caregivers of younger children with PCG in one study [86].
These characteristics played an important role in caregiver burden in a study by Zhu et al. [87]. Overall caregiver burden was significantly higher in mothers, caregivers with higher education or household income, and employed caregivers. More specifically, parents who were older, had lower household income, or whose children were younger experienced a more time-dependent burden. The same authors also described that mothers and employed caregivers experienced more physical burden, while less-educated caregivers reported more developmental burden [87].
Study designs of included publications
The ideal study design for assessing PF or QoL in childhood glaucoma would have a large sample size, use an internationally validated instrument specific to childhood glaucoma, address each facet of PF or QoL individually, and be designed longitudinally. Currently, there are no studies that meet all the criteria outlined above.
The existing literature on PF or QoL in childhood glaucoma mainly comprises cross-sectional studies. Only two longitudinal studies were conducted, one in India studying caregivers [73] and the other in Egypt studying children [71]. Few studies reported sample size calculations, but those that did meet [86] or exceed [83] their target enrollment were determined using expected impact and prior literature.
Most studies addressed the PF or QoL of children diagnosed with childhood glaucoma, while three studies included adults [80, 81, 90] with a glaucoma diagnosis at pediatric age. One study was considered for review but excluded due to the participants’ age at diagnosis (15–40 years), which did not fit the authors’ definition of childhood glaucoma [91]. Geographically, a disproportionate number of studies was conducted in India (Fig. 2), with one study group contributing seven of the studies.
Only eight of the studies included in the review assessed elements of PF. Of those, four studied only PF [71, 84, 87, 88], and four measured both PF and QoL [80, 82, 86, 89]. Notably, Knight et al. studied PF and QoL as congruent topics encompassing emotional well-being, social well-being, inconveniences, activity limitations, and mobility in adults with a childhood glaucoma diagnosis [80] and in caregivers [89]. The remaining 14 discussed only QoL, independent of PF. No studies assessed the burden of childhood glaucoma on family members other than parents, such as siblings, or on providers who manage childhood glaucoma. Findings on PF or QoL in childhood glaucoma across the published studies remain inconsistent due in part to the cultural diversity among study populations, which limits generalizability of the findings to a global scale.
Variability of tools and results
Twenty-one instruments were used among the 22 included papers (Table 5), demonstrating a lack of consistency or standardization when researchers considered how to assess PF or QoL in childhood glaucoma. Instruments used for patient-reported outcomes measured VR-QoL, HR-QoL, general QoL, and FV, and were catered to populations with visual impairment [78] or pediatric populations in general (i.e., PedsQL or Kidscreen-27). Caregiver PF or QoL was assessed using a questionnaire specific to childhood glaucoma caregiving (CarCGQoL) as well as general caregiver instruments (i.e., PAC, CBQ, CBI). For both populations, commonly used mental health instruments included PHQ-9 or GAD-7. Most studies also incorporated supplemental questionnaires recording sociodemographic data and ocular medical history. The variability in the instruments was likely a contributing factor to the variability in results.
While a universal tool to assess PF or QoL may prove useful in drawing more generalizable conclusions, researchers developing, translating, and validating an instrument for use across various regions must consider language and culture. Culture often plays a large part in how ideas are communicated. Particularly for rural populations, variability in local colloquialism can change the meaning of a question entirely, making direct translation challenging. Culture can also dictate standards of well-being that may not be applicable worldwide [73]. For example, an instrument developed in India includes “likelihood that child will get married” [73], which, while culturally significant in India, may not universally apply.
The specificity of instruments developed can affect the accuracy of reported PF or QoL. It is important to have an instrument that is disease (glaucoma) specific in order to capture the unique challenges that the chronic condition presents, i.e., the specific impact of an uncertain visual prognosis and potentially blinding progressive disease; yet it will unsurprisingly not be applicable to populations without the disease [36]. Conversely, if an instrument is generic, it will be able to reach a broader population, but may not properly evaluate characteristics distinct to the disease(s) studied.
Furthermore, distinct concepts such as VR-QoL and FV have been inappropriately conflated in some ophthalmic literature [44]. While FV might be related to VR-QoL, they are operationalized differently. For example, FV does not include mental health, self-perception, or social functioning and is restricted to vision-related activities (i.e., the ability to watch TV), whereas VR-QoL is the patients’ perception of their own lives in relation to their eye problem (i.e., ability to make friends). The authors encourage the use of unidimensional instruments that do not conflate distinct concepts.
Another challenge to measuring PF or QoL in childhood glaucoma involves the perception and reporting of PF or QoL itself. The age at which children can reliably and accurately self-report results is inconsistent. Some studies have validated self-reporting by children as young as 5 years old [92], while other literature states children cannot reliably self-report until the age of 8 [93]. Furthermore, studies that compare children’s self-reported PF, QoL, or FV to those reported by caregivers found that caregivers consistently overestimate the burden of disease on children and underestimate their QoL [36, 79, 94], apart from one study, which showed bidirectional disagreement between patients and their caregivers (i.e., caregivers both over- and underestimated their child’s QoL) [76]. These limitations make it difficult to determine whether QoL reports by younger children or by proxy caregivers are reliable.
Discussion
Strengths
This is a novel, childhood glaucoma-specific comprehensive review of PF and QoL in children and caregivers. While there is a breadth of literature concerning QoL in patients with visual impairment and their caregivers [1,2,3,4, 6, 8, 9, 67], no extant review exists specific to childhood glaucoma.
A thorough and comprehensive search of all potentially relevant studies was conducted (details on this may be found in the section titled “Method of literature search”). Due to the paucity of research overall, literature published in any year was included. As a result, we believe that this review encompasses all literature published on PF or QoL and childhood glaucoma with either an abstract or text available in English. Still, there is a chance that relevant studies may have not been included in this review. Our results, however, indicate that investigations on this topic only recently began. Of the 22 studies included in the current review, the earliest was published in 2009, and the majority (n = 16) appeared in the literature in the last 5 years.
PROMs can help healthcare professionals to make informed decisions based on their patients’ priorities and improve the care they provide as well as evaluate the performance of their practice [15]. This review demonstrates the utility of PROMs, like the PF or QoL assessment tools, to monitor the progress of patients with childhood glaucoma, measure the impact of healthcare interventions, detect secondary problems early, and measure caregiver burden.
Lastly, this review identifies questionnaires that can be employed in clinical practice to assess childhood glaucoma’s impact on patient and caregiver health outcomes.
Limitations
There are a number of methodological issues that limit the quality of the studies reviewed. The foremost limitation of this review is that there are few definitive conclusions that can be made from the current evidence base, which is likely due to the quality of the studies present, such as small sample sizes and selective patient demographics. As discussed, the lack of standardized questionnaires specific to PF or QoL in childhood glaucoma led to researchers using several different instruments or adapting them to the population of interest, thus impacting the ability to capture glaucoma-specific concerns or impacts. Similarly, the PROMs implemented in some studies of our review do not differentiate between QoL and FV as distinct concepts, leading to imprecise results [44]. Furthermore, the literature disproportionately represents study samples from India or the Middle East, with relatively little research conducted in other parts of the world (Fig. 2), which could be an outcome of the variation in the prevalence of childhood glaucoma per global region. Cultural factors as well as variations in study methods and samples may also limit the applicability of the findings to population which differ substantially.
The authors included literature on any methodology, a potential cause for the discrepancy among the results. Two studies focused specifically on questionnaire development and validation [73, 74] and one study measured the parent–child agreement in reporting HR-QoL [76]. Two studies featured a longitudinal study design [71, 85], one of which introduced an educational intervention [71]. The remaining 17 employed a cross-sectional study design, which cannot infer causality and does not address how PF or QoL may change for patients and their caregivers over time. In addition, many studies did not utilize a control group but rather compared results to the norms of the various measures used. Another limitation was the relatively small sample sizes employed in several studies. There is also the question of possible study sample bias in many studies which did not report participation rates. Two sets of papers [37, 73, 76, 85] derived their results from the same dataset, potentially duplicating findings.
While a number of studies examined QoL in young patients with glaucoma, there were no studies of psychological and social functioning, cognitive development, or academic achievement. Among studies of QoL, few examined generic as opposed to vision-specific QoL. More studies are needed to address factors predictive of QoL (besides visual ability, bilateral condition, number of surgeries) as well as interventions to improve QoL. As the research literature in this area increases, the use of meta-analysis will be a useful tool to compare results across various studies as well as systematically evaluate the rigor of the methodologies employed. Prospective longitudinal studies with large and diverse patient samples [95] are especially needed to identify the course of psychosocial development and factors predictive of health outcomes.
Opportunities for global and public health research
Future prospective, longitudinal studies would be useful in understanding changes in PF or QoL over time as it relates to factors such as age, length of therapy, nature of the intervention, visual outcome, and complications, when applicable. As previously discussed, the development of globally accepted standard instruments for measuring PF or QoL may aid in comparing results across regions, while also appreciating how local population-specific factors might affect these. The authors also encourage a global collaboration to diversify the sample population and study size in future research.
Studying the correlations between PF or QoL and factors such as education level, health literacy, age, and marital status may improve our understanding of the effect of glaucoma on an entire family. Research to elucidate this complex area and identify interventions to support families is warranted.
The authors note that while many of the studies and interventions discussed in this review reported or addressed reports of childhood glaucoma having a negative impact on the activities of daily living of the patient and caregiver, this does not necessarily translate into lower QoL. The “disability paradox” indicates that a child’s QoL is not inherently dependent on whether or not they have functional limitations or health conditions, and therefore children with disabilities may experience QoL that is as good as, or sometimes better than, their non-disabled peers [14]. It would be of interest to investigate these issues in childhood glaucoma in diverse populations and cultures. Age and developmentally appropriate PROMs that measure QoL and FV separately are also necessary to identify the disability paradox in glaucoma populations should it exist.
Opportunities for clinic-based research
This review highlights the void as well as the potential value of using standardized outcome measures to monitor PF or QoL in patients and caregivers. Indeed, some studies on utilizing PROMs in routine clinical care display a positive impact on HR-QoL [96, 97]. Given the tendency for caregivers to under- [36, 76, 79] or overestimate [76] their child’s well-being, the authors advocate seeking self-report from subjects as the most important outcome measure rather than caregiver or proxy report when administering questionnaires related to PF or QoL in the patient. Caregivers are an integral part of the clinical relationship, and this needs to be respected when seeking such information. Raising awareness of this potential source of bias, along with specific comments on study design methodology to show how this has been addressed, will strengthen the veracity of the research findings. Furthermore, to comprehensively understand well-being in childhood glaucoma care, researchers should consider studies assessing PF or QoL in siblings and in those who provide care to individuals with childhood glaucoma. It would also be useful to explore the impact of the health provider’s or the siblings’ attitudes toward the child with glaucoma upon that child.
Opportunities for interventional research
Multiple studies included in this review identified that low FV is associated with low VR-QoL and HR-QoL [36, 38, 75, 77, 79], revealing an extra incentive to focus efforts to maximize visual health. Low-vision aids, such as manual monocular telescopic systems, can improve children’s ability to succeed developmentally, socially, and academically [98], and maybe a necessary treatment for childhood glaucoma in addition to medical and surgical therapies [83]. Research on interventions outside of the aforementioned low-vision aids is limited, leaving an opportunity for future studies.
The accelerated application of telehealth during the COVID-19 pandemic has offered options for care, but evidence of its benefits and disadvantages is mixed. Telemedicine may improve patient experience, as seen by a decreased travel burden in one review on adult glaucoma care [99]. However, “digital exclusion” of patients who lack the resources to participate in telemedicine is a growing concern and a cause of widening health inequalities [100]. There are no current studies on this topic as it pertains to childhood glaucoma and thus, studies on the outcomes of telemedicine on PF or QoL in these individuals are recommended.
There is also no literature on the role of online support groups in improving well-being in individuals with childhood glaucoma or their caregivers, and this is an area of research that the authors believe could prove clinically useful. The low cost and potential for dissemination of information through online avenues allow for a greater scope of outreach, and online interventions can help deliver benefits to patients and caregivers globally.
It is fundamental to a successful assessment program that patients noted to have low PF or QoL have access to appropriate clinical resources and support structures. In addition to specialist glaucoma care, the clinical care team ideally should include members with skills in childhood and family behavior, psychology, low vision, occupational therapy, social work, and more. Literature also emphasizes the value of health literacy regarding illness uncertainty [71, 72] and the authors encourage providing psychoeducation to patients and caregivers to improve treatment, compliance, and family adaptation.
Summary
This report addresses the peer-reviewed literature related to PF and QoL in patients with childhood glaucoma and their caregivers. The goal was to consolidate and describe the currently published evidence base, explore areas for relevant future research, and propose potential improvements in study design and methodology to deliver the highest quality evidence to improve health outcomes in this population.
Although some trends could be identified, such as significantly worse patient and caregiver PF or QoL with worse VA or younger patient age, the disparate approaches and study designs made more detailed analysis difficult. There were many inconsistencies at all stages of the study design, which while contributing to a broader picture, limit comparisons of outcomes between them, their relevance to other populations, or consolidation for meaningful collaborations and statistical analysis. Immediate important questions resulting from this work include how best to determine the most appropriate model(s) for assessment of the impact of childhood glaucoma in various healthcare settings, both for identifying patients and families who need additional support or other interventions, and how best to ensure that measures of patient and caregiver well-being are integral to these studies.
Our findings suggest healthcare teams will gain much from addressing the PF or QoL of childhood glaucoma patients and their caregivers as components of a holistic and multidisciplinary approach for families facing childhood glaucoma. The negative impact of childhood glaucoma extends into every domain of the life of the patient and beyond the patient in question to their caregivers. This impact cannot be captured through the clinical findings normally focused on by managing physicians. Whilst the literature is varied, a common theme is an advocacy for the inclusion of patient [36,37,38, 71, 75, 77, 78, 82, 90] and caregiver [73, 82,83,84,85,86,87] PF or QoL in the evaluation and treatment plan. Drawing from our review, potential avenues to address this need include discussions about health literacy [90], health educational intervention programs [71], and psychological support [75, 82, 84, 87]. There were relatively few common findings across the identified papers because of the wide variability in assessment tools, methodology, and cultures. This review highlights the need for future studies validating and employing standardized tools to measure PF or QoL of patients with childhood glaucoma and their caregivers.
References
Castañeda YS, Cheng-Patel CS, Leske DA, Wernimont SM, Hatt SR, Liebermann L, et al. Quality of life and functional vision concerns of children with cataracts and their parents. Eye (Lond). 2016;30:1251–9.
Chak M, Rahi JS, British Congenital Cataract Interest Group. The health-related quality of life of children with congenital cataract: findings of the British Congenital Cataract Study. Br J Ophthalmol. 2007;91:922–6.
Drews C, Celano M, Plager DA, Lambert SR. Parenting stress among caregivers of children with congenital cataracts. J AAPOS. 2003;7:244–50.
Tailor VK, Abou-Rayyah Y, Brookes J, Khaw PT, Papadopoulos M, Adams GGW, et al. Quality of life and functional vision in children treated for cataract—a cross-sectional study. Eye. 2017;31:856–64.
Ilhan B, Idil A, Ilhan I. Sports participation and quality of life in individuals with visual impairment. Ir J Med Sci. 2021;190:429–36.
Khan Z, Braich PS, Rahim K, Rayat JS, Xing L, Iqbal M, et al. Burden and depression among caregivers of visually impaired patients in a Canadian population. Adv Med. 2016;2016:4683427.
Pinquart M, Pfeiffer JP. Psychological adjustment in adolescents with vision impairment. Intl J Disabil Dev Educ. 2012;59:145–55.
Robertson AO, Horvat-Gitsels LA, Cortina-Borja M, Rahi JS. Distribution and associations of vision-related quality of life and functional vision of children with visual impairment. Br J Ophthalmol. 2022;106:1325–30.
Sola-Carmona JJ, López-Liria R, Padilla-Góngora D, Daza MT, Aguilar-Parra JM, Salido-Campos M. Factors associated with the anxiety, subjective psychological well-being and self-esteem of parents of blind children. PLoS One. 2016;11:e0162294.
Santos T, de Matos MG, Simões C, Leal I, do Céu Machado M. (Health-related) quality of life and psychosocial factors in adolescents with chronic disease: a systematic literature review. Int J Adolesc Med Health. 2017;31.
Pinquart M, Teubert D. Academic, physical, and social functioning of children and adolescents with chronic physical illness: a meta-analysis. J Pediatr Psychol. 2012;37:376–89.
Vinson JA. Children with asthma: initial development of the child resilience model. Pediatr Nurs. 2002;28:149–58.
Na CH, Chung J, Simpson EL. Quality of life and disease impact of atopic dermatitis and psoriasis on children and their families. Children (Basel). 2019;6:133.
Weinreb RN. Childhood glaucoma: the 9th concensus report of the World Glaucoma Association. In: Weinreb RN, Grajewski A, Papadopoulos M, Grigg J, Freedman S, editors. Consensus series; 9. Amsterdam: Kugler Publications; 2013. p. 249–54.
Dawson J, Doll H, Fitzpatrick R, Jenkinson C, Carr AJ. The routine use of patient reported outcome measures in healthcare settings. BMJ. 2010;340:c186.
Everhart RS, Greenlee JL, Winter MA, Fiese BH. Primary and secondary caregiver reports of quality of life in pediatric asthma: are they comparable? Appl Res Qual Life. 2018;13:371–83.
Kosse RC, Koster ES, Kaptein AA, de Vries TW, Bouvy ML. Asthma control and quality of life in adolescents: the role of illness perceptions, medication beliefs, and adherence. J Asthma. 2020;57:1145–54.
Rüth E-M, Landolt M, Neuhaus T, Kemper M. Health-related quality of life and psychosocial adjustment in steroid-sensitive nephrotic syndrome. J Pediatr. 2005;145:778–83.
Armstrong MI, Birnie-Lefcovitch S, Ungar MT. Pathways between social support, family well being, quality of parenting, and child resilience: what we know. J Child Fam Stud. 2005;14:269–81.
Weinreb RN. Childhood glaucoma: the 9th concensus report of the World Glaucoma Association. In: Weinreb RN, Grajewski A, Papadopoulos M, Grigg J, Freedman S, editors. Consensus series; 9. Amsterdam: Kugler Publications; 2013. p. 3–10.
Knight LSW, Ruddle JB, Taranath DA, Goldberg I, Smith JEH, Gole G, et al. Childhood and early onset glaucoma classification and genetic profile in a large Australasian Disease Registry. Ophthalmology. 2021;128:1549–60.
Papadopoulos M, Vanner EA, Grajewski AL, Mithra A, Pillai M, Upadhyaya S, et al. International study of childhood glaucoma. Ophthalmol Glaucoma. 2020;3:145–57.
Teoh LJ, Solebo AL, Rahi JS, Abbott J, Abdullah W, Adams G, et al. Visual impairment, severe visual impairment, and blindness in children in Britain (BCVIS2): a national observational study. Lancet Child Adolesc Health. 2021;5:190–200.
Lyons CJ, Lambert SR.Taylor and Hoyt’s pediatric ophthalmology and strabismus. 5th ed. Edinburgh: Elsevier; 2017.
Glaucoma for Children. Roseville, MN: American Association for Pediatric Ophthalmology and Strabismus [updated 2022]. https://aapos.org/glossary/glaucoma-for-children.
Papadopoulos M, Cable N, Rahi J, Khaw PT, BIG Eye Study Investigators. The British Infantile and Childhood Glaucoma (BIG) Eye Study. Invest Ophthalmol Vis Sci. 2007;48:4100–6.
Walton DS. Primary congenital open angle glaucoma: a study of the anterior segment abnormalities. Trans Am Ophthalmol Soc. 1979;77:329–43.
Aponte EP, Diehl N, Mohney BG. Incidence and clinical characteristics of childhood glaucoma: a population-based study. Arch Ophthalmol. 2010;128:478–82.
Weinreb RN Childhood glaucoma: the 9th concensus report of the World Glaucoma Association. In: Weinreb RN, Grajewski A, Papadopoulos M, Grigg J, Freedman S, editors. Consensus series; 9. Amsterdam: Kugler Publications; 2013. p. 15–41.
Vivar KL, Kruse L. The impact of pediatric skin disease on self-esteem. Int J Womens Dermatol. 2018;4:27–31.
Kelly KA, Balogh EA, Kaplan SG, Feldman SR. Skin disease in children: effects on quality of life, stigmatization, bullying, and suicide risk in pediatric acne, atopic dermatitis, and psoriasis patients. Children (Basel). 2021;8:1057.
Warnink-Kavelaars J, Beelen A, Goedhart T, de Koning LE, Nollet F, Alsem MW, et al. Marfan syndrome in adolescence: adolescents’ perspectives on (physical) functioning, disability, contextual factors and support needs. Eur J Pediatr. 2019;178:1883–92.
Ben-Zion I, Tomkins O, Moore DB, Helveston EM. Surgical results in the management of advanced primary congenital glaucoma in a rural pediatric population. Ophthalmology. 2011;118:231–5.e1.
Ro E, Clark LA. Psychosocial functioning in the context of diagnosis: assessment and theoretical issues. Psychol Assess. 2009;21:313–24.
World Health Organization. Programme on mental health: WHOQOL user manual. Geneva: World Health Organization; 1998. Contract No.: WHO/HIS/HSI Rev.2012.03.
Dahlmann-Noor A, Tailor V, Bunce C, Abou-Rayyah Y, Adams G, Brookes J, et al. Quality of life and functional vision in children with glaucoma. Ophthalmology. 2017;124:1048–55.
Gothwal VK, Seelam B, Mandal AK. Quality of life following surgery for congenital glaucoma: findings of the LVPEI congenital glaucoma registry. Eye (Lond). 2019;33:659–67.
Gothwal VK, Sharma S, Mandal AK. Beyond intraocular pressure: visual functioning and quality of life in primary congenital glaucoma and secondary childhood glaucoma. Am J Ophthalmol. 2020;209:62–70.
Torrance GW. Utility approach to measuring health-related quality of life. J Chronic Dis. 1987;40:593–603.
Centers for Disease Control and Prevention. Health-related quality of life (HRQOL). Washington, DC: U.S. Department of Health & Human Services [updated June 16, 2021]. https://www.cdc.gov/hrqol/index.htm.
Angeles-Han ST, Griffin KW, Harrison MJ, Lehman TJ, Leong T, Robb RR, et al. Development of a vision-related quality of life instrument for children ages 8-18 years for use in juvenile idiopathic arthritis-associated uveitis. Arthritis Care Res (Hoboken). 2011;63:1254–61.
Bennett CR, Bex PJ, Bauer CM, Merabet LB. The assessment of visual function and functional vision. Semin Pediatr Neurol. 2019;31:30–40.
Colenbrander A. Visual functions and functional vision. Int Congr Ser. 2005;1282:482–6.
Tadić V, Hogan A, Sobti N, Knowles RL, Rahi JS. Patient-reported outcome measures (PROMs) in paediatric ophthalmology: a systematic review. Br J Ophthalmol. 2013;97:1369.
Cella D, Hahn EA, Jensen SE, Butt Z, Nowinski CJ, Rothrock N, et al. Patient-reported outcomes in performance measurement. Research Triangle Park (NC): RTI Press; 2015.
Li J, Song Y. Formal and informal care. Encyclopedia of gerontology and population aging. Cham: Springer International Publishing; 2019. p. 1–8.
Liu Z, Heffernan C, Tan J. Caregiver burden: a concept analysis. Int J Nurs Sci. 2020;7:438–45.
Immelt S. Psychological adjustment in young children with chronic medical conditions. J Pediatr Nurs. 2006;21:362–77.
Pinquart M, Shen Y. Anxiety in children and adolescents with chronic physical illnesses: a meta-analysis. Acta Paediatr. 2011;100:1069–76.
Pinquart M, Shen Y. Depressive symptoms in children and adolescents with chronic physical illness: an updated meta-analysis. J Pediatr Psychol. 2011;36:375–84.
Pinquart M, Shen Y. Behavior problems in children and adolescents with chronic physical illness: a meta-analysis. J Pediatr Psychol. 2011;36:1003–16.
Manzoni AP, Weber MB, Nagatomi AR, Pereira RL, Townsend RZ, Cestari TF. Assessing depression and anxiety in the caregivers of pediatric patients with chronic skin disorders. Bras Dermatol. 2013;88:894–9.
Cohn LN, Pechlivanoglou P, Lee Y, Mahant S, Orkin J, Marson A, et al. Health outcomes of parents of children with chronic illness: a systematic review and meta-analysis. J Pediatr. 2020;218:166–77.e2.
Meltzer LJ, Mindell JA. Impact of a child’s chronic illness on maternal sleep and daytime functioning. Arch Intern Med. 2006;166:1749–55.
Rabow MW, Hauser JM, Adams J. Supporting family caregivers at the end of life: “they don’t know what they don’t know”. JAMA. 2004;291:483–91.
Cannuscio C, Jones C, Kawachi I, Colditz G, Berkman L, Rimm E. Reverberations of family illness: a longitudinal assessment of informal caregiving and mental health status in the nurses’ health study. Am J Public Health. 2002;92:1305–11.
Caicedo C. Families with special needs children: family health, functioning, and care burden. J Am Psychiatr Nurses Assoc. 2014;20:398–407.
Chen SH, Huang JL, Yeh KW, Tsai YF. The stress of caring for children with asthma: a qualitative study of primary caregivers. J Nurs Res. 2015;23:298–307.
Salvador Á, Crespo C, Martins AR, Santos S, Canavarro MC. Parents’ perceptions about their child’s illness in pediatric cancer: links with caregiving burden and quality of life. J Child Fam Stud. 2015;24:1129–40.
Puka K, Tavares TP, Anderson KK, Ferro MA, Speechley KN. A systematic review of quality of life in parents of children with epilepsy. Epilepsy Behav. 2018;82:38–45.
Tourame B, Ben Younes N, Guigou S, Denis D. [Congenital glaucoma: future of vision and pressure. Results of an 11-year study]. J Fr Ophtalmol. 2009;32:335–40.
Terry RL, Berg AJ, Phillips PE. The effect of eyeglasses on self-esteem. J Am Optom Assoc. 1983;54:947–9.
Law GC, Bülbül A, Jones CJ, Smith H. ‘The mean mummy way’ – experiences of parents instilling eye drops to their young children as described in online forums and blogs. BMC Pediatr. 2020;20:514.
Zhang X, Bullard KM, Cotch MF, Wilson MR, Rovner BW, McGwin G Jr, et al. Association between depression and functional vision loss in persons 20 years of age or older in the United States, NHANES 2005–2008. JAMA Ophthalmol. 2013;131:573–81.
Choi HG, Lee MJ, Lee SM. Visual impairment and risk of depression: a longitudinal follow-up study using a national sample cohort. Sci Rep. 2018;8:2083.
Mayro EL, Murchison AP, Hark LA, Silverstein M, Wang OY, Gilligan JP, et al. Prevalence of depressive symptoms and associated factors in an urban, ophthalmic population. Eur J Ophthalmol. 2021;31:740–7.
Akram B, Batool M. Suicidal behavior among the youth with and without sensory impairment: prevalence and comparison. Omega (Westport). 2020;81:393–403.
Waern M, Rubenowitz E, Runeson B, Skoog I, Wilhelmson K, Allebeck P. Burden of illness and suicide in elderly people: case-control study. BMJ. 2002;324:1355.
Zhang D, Fan Z, Gao X, Huang W, Yang Q, Li Z, et al. Illness uncertainty, anxiety and depression in Chinese patients with glaucoma or cataract. Sci Rep. 2018;8:11671.
Roberts CM, Sharkey CM, Bakula DM, Perez MN, Delozier AJ, Austin PF, et al. Illness uncertainty longitudinally predicts distress among caregivers of children born with DSD. J Pediatr Psychol. 2020;45:1053–62.
Mohamed EA, Bayoumi OR, Draz SF. Impact of an educational programme on knowledge, beliefs, practices and expectations about care among adolescent glaucoma patients in Cairo. East Mediterr Health J. 2011;17:960–8.
Freedman RB, Jones SK, Lin A, Robin AL, Muir KW. Influence of parental health literacy and dosing responsibility on pediatric glaucoma medication adherence. Arch Ophthalmol. 2012;130:306–11.
Gothwal VK, Bharani S, Mandal AK. Quality of life of caregivers of children with congenital glaucoma: development and validation of a novel questionnaire (CarCGQoL). Invest Ophthalmol Vis Sci. 2015;56:770–7.
Gothwal VK, Sharma S, Mandal AK. Cross-diagnostic validity of the congenital glaucoma Caregiver’s Quality of Life Questionnaire (CarCGQoL). Transl Vis Sci Technol. 2020;9:10.
Zhang XL, Du SL, Ge J, Chen WR, Fan Q, Peng SX, et al. [Quality of life in patients with primary congenital glaucoma following antiglaucoma surgical management]. Zhonghua Yan Ke Za Zhi. 2009;45:514–21.
Gothwal VK, Bharani S, Mandal AK. Parent-child agreement on health-related quality of life in congenital glaucoma. Transl Vis Sci Technol. 2018;7:15.
AlDarrab A, Al Qurashi M, Al Thiabi S, Khandekar R, Edward DP. Functional visual ability and quality of life in children with glaucoma. Am J Ophthalmol. 2019;200:95–9.
Freedman BL, Jones SK, Lin A, Stinnett SS, Muir KW. Vision-related quality of life in children with glaucoma. J AAPOS. 2014;18:95–8.
Moreno MN, Morales Fernández L, Ruiz Medrano M, Martínez de la Casa JM, Madrigal Sánchez R, Hernández García E, et al. Estudio de la calidad de vida y la función visual en niños con glaucoma en España. Arch Soc Esp Oftalmol. 2019;94:119–24.
Knight LSW, Ridge B, Staffieri SE, Craig JE, Prem Senthil M, Souzeau E. Quality of life in adults with childhood glaucoma: an interview study. Ophthalmol Glaucoma. 2022;5:325–36.
Miraftabi A, Coleman AL, Nilforushan N, Parsamanesh M, Nguyen AH, Karimi N, et al. Vision-related quality of life in patients with a history of congenital glaucoma. Eur J Ophthalmol. 2021;31:3074–9.
Silva AOD, Rolim-de-Moura C, Botelho NLP, Gracitelli CP, Ferraz NN. Psychosocial indicators of primary congenital glaucoma and filtering surgeries impacts on children and family’s quality of life. Eur J Ophthalmol. 2022;32:1997–2004.
AlQurashi M, Mocan MC, AlDarrab A, Al Thiabi S, Khandekar R, Ahmad K, et al. Quality of life of caregivers of children with glaucoma in an Arab population: a cross-sectional study. J Glaucoma. 2019;28:965–68.
Dada T, Aggarwal A, Bali SJ, Wadhwani M, Tinwala S, Sagar R. Caregiver burden assessment in primary congenital glaucoma. Eur J Ophthalmol. 2013;23:324–8.
Gothwal VK, Bharani S, Mandal AK. Impact of surgery on the quality of life of caregivers of children with congenital glaucoma. Ophthalmology. 2016;123:1161–2.
Kantipuly A, Pillai MR, Shroff S, Khatiwala R, Raman GV, Krishnadas SR, et al. Caregiver burden in primary congenital glaucoma. Am J Ophthalmol. 2019;205:106–14.
Zhu Y, Gao J, Li X, Yang Q, Lian Y, Xiao H, et al. Burden, positive aspects, and predictive variables of caregiving: a study of caregivers of patients with pediatric glaucoma. J Ophthalmol. 2019;2019:6980208.
Wy S, Choe S, Lee YJ, Bak E, Jang M, Lee SC, et al. Decision tree algorithm-based prediction of vulnerability to depressive and anxiety symptoms in caregivers of children with glaucoma. Am J Ophthalmol. 2022;239:90–7.
Knight LS, Ridge B, Staffieri SE, Craig JE, Senthil MP, Souzeau E. The caregiver experience in childhood glaucoma: an interview study. Ophthalmol Glaucoma. 2022;5:531–43.
Gothwal VK, Mandal AK. Quality of life and life satisfaction in young adults with primary congenital glaucoma. Ophthalmol Glaucoma. 2021;4:312–21.
Gupta V, Dutta P, Ov M, Kapoor KS, Sihota R, Kumar G. Effect of glaucoma on the quality of life of young patients. Invest Ophthalmol Vis Sci. 2011;52:8433–7.
Varni JW, Limbers CA, Burwinkle TM. How young can children reliably and validly self-report their health-related quality of life?: an analysis of 8,591 children across age subgroups with the PedsQL™ 4.0 Generic Core Scales. Health Qual Life Outcomes. 2007;5:1.
Tomlinson D, Tigelaar L, Hyslop S, Lazor T, Dupuis LL, Griener K, et al. Self-report of symptoms in children with cancer younger than 8 years of age: a systematic review. Support Care Cancer. 2017;25:2663–70.
Robertson AO, Tadić V, Cortina-Borja M, Rahi JS. A patient-reported outcome measure of functional vision for children and young people aged 8 to 18 years with visual impairment. Am J Ophthalmol. 2020;219:141–53.
Tadić V, Hamblion EL, Keeley S, Cumberland P, Lewando Hundt G, Rahi JS. ‘Silent voices’ in health services research: ethnicity and socioeconomic variation in participation in studies of quality of life in childhood visual disability. Invest Ophthalmol Vis Sci. 2010;51:1886–90.
Engelen V, Detmar S, Koopman H, Maurice-Stam H, Caron H, Hoogerbrugge P, et al. Reporting health-related quality of life scores to physicians during routine follow-up visits of pediatric oncology patients: is it effective? Pediatr Blood Cancer. 2012;58:766–74.
Murillo M, Bel J, Pérez J, Corripio R, Carreras G, Herrero X, et al. Impact of monitoring health-related quality of life in clinical practice in children with type 1 diabetes mellitus. Qual Life Res. 2017;26:3267–77.
Haddad MAO, Sampaio MW, Oltrogge EW, Kara-José N, Betinjane AJ. Visual impairment secondary to congenital glaucoma in children: visual responses, optical correction and use of low vision AIDS. Clinics (Sao Paulo). 2009;64:725–30.
Ertel MK, Kahook MY, Capitena, Young CE. The future is now: incorporating telemedicine into glaucoma care. Curr Ophthalmol Rep. 2021;9:88–95.
Watts G. COVID-19 and the digital divide in the UK. Lancet Digit Health. 2020;2:e395–6.
Acknowledgements
The authors thank The Samuel & Ethel Balkan International Pediatric Glaucoma Center for its philanthropic support in the production of this manuscript.
Funding
Supported by Fight for Sight PhD Studentship (AS), an unrestricted departmental grant to the Casey Eye Institute from Research to Prevent Blindness (BE), Ulverscroft Foundation (AS, JR), National Institute for Health Research Biomedical Research Centre (JR), and the National Institute of Nursing Research (Grant R01NR016838) (YK).
Author information
Authors and Affiliations
Consortia
Contributions
DEM, AS, HM, JR, ALG, and AD designed the study and were involved in the analysis. All authors contributed to the interpretation of data. DEM, AS, HM, and AJP drafted the initial manuscript. All authors helped with critical revisions of the manuscript, and reviewed the manuscript and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
McLaughlin, D.E., Semrov, A., Munshi, H. et al. The impact of childhood glaucoma on psychosocial functioning and quality of life: a review of the literature. Eye 37, 3157–3173 (2023). https://doi.org/10.1038/s41433-023-02492-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02492-1