Abstract
Objectives
This study reports the surgical outcomes of evisceration with primary orbital implant placement in patients with endophthalmitis and analyses the association with implant exposure and extrusion.
Methods
A retrospective, multicentre, Chinese cohort study. Review of medical records and orbital images of patients who underwent evisceration with primary orbital implant placement between January 2005 and January 2021.
Results
Out of 79 patients who underwent orbital evisceration with primary orbital implant placement, 26 (26 eyes) of them (male = 13) suffered from endophthalmitis. The duration from endophthalmitis diagnosis (19 = exogenous, 7 = endogenous) to evisceration was 9 standard deviation ± 5 (range: 1–15) days. The follow-up was 70 ± 46 (24–180) months after operation. The orbital implant size was 17 ± 3 (14–20) mm, and silicone was the most used material (69%, 18/26 of patients). The most frequent post-operative complication was orbital implant exposure (42%, 11/26), followed by orbital implant extrusion (12% 3/26) and ptosis (8%, 2/26). Implant exposure or extrusion was more commonly associated with endophthalmitis in comparison to non-endophthalmitis patients that required evisceration and primary orbital implant placement (54% versus 17%, P < 0.05). Univariate analysis showed single scleral closure technique (100% versus 58%, P < 0.05) and endogenous endophthalmitis (50% versus 0%, P < 0.05) were associated with implant exposure or extrusion, and only endogenous endophthalmitis was significant with multivariate analysis (P < 0.05).
Conclusions
Primary implant placement during evisceration should be avoided in eyes with endophthalmitis especially in those with an endogenous source, and double scleral closure technique may be a better alternative for primary orbital implant placement in infected eyes.
Similar content being viewed by others
Introduction
Orbital evisceration is the complete removal of intraocular contents with the preservation of both the scleral shell and the extraocular muscle attachments [1]. Evisceration was introduced as a way to prevent intracranial spread of infection from endophthalmitis eyes [2], and almost a quarter of eyes with endophthalmitis required anophthalmic surgery despite antibiotic treatment [3]. Evisceration is traumatic in both physical and psychological ways to patients. Orbital implants are often placed to correct the orbital volume loss and maximize the motility of prosthesis to improve cosmetic outcomes [4].
The option of primary orbital implant placement in eyes with endophthalmitis during evisceration remains controversial. Up to 50% of surgeons preferred delayed orbital implant placements in endophthalmitis eyes from a United Kingdom study [5]. Delayed implant placement was recommended to reduce risk of implant exposure and extrusion [6, 7]. On the other hand, second stage orbital implant placement may be less cost effective due to the further hospitalization and prolonged wound care [8]. Recent studies suggested that primary orbital implant placement in patients with infected eyes was an acceptable treatment option with a low risk of orbital implant extrusion [9, 10].
The risk factors of orbital implant exposure or extrusion, and their significance, after evisceration remains underexplored. Orbital cellulitis was reportedly a risk factor for implant extrusion in eyes with endophthalmitis [11]. Eyes infected with pseudomonas aeruginosa may be predisposing to implant exposure [12]. Over the past 15 years, we have been performing orbital eviscerations with primary orbital implant placement in patients with endophthalmitis. We would like to report the long term surgical outcomes and analyse the associations of implant exposure or extrusion after primary orbital implant placement in eyes with endophthalmitis.
Methods
This retrospective cohort study was approved by the Institutional Review Board of the Hong Kong East Cluster (HKECREC-2019016). The study was conducted in accordance with the Declaration of Helsinki. Medical records of patients who underwent evisceration at Tung Wah Eastern Hospital and Pamela Youde Nethersole Eastern Hospital between 1st January 2005 and 1st January 2021 were reviewed. All operations were supervised by the same consultant oculoplastic surgeon.
We only included patients who had at least 24 months follow up to monitor for postoperative complications. Patients under the age of 18, without primary orbital implant placement, and incomplete clinical documents were excluded. The diagnosis of endophthalmitis was made based on clinical, microbiological and ultrasonographic information [13]. Patients’ information including age, sex, past medical history, types of endophthalmitis, surgical technique, orbital implant material and size, intraoperative and postoperative complications were reviewed by 2 ophthalmologist trainees independently.
Informed consent for evisceration surgery was obtained in all patients before the surgery. Single scleral closure techniques were performed as described in literature [14]. We also performed double scleral closure technique similar to the technique as described by Jordan et al. [15], with orbital implant placed posterior to the posterior sclera.
Statistical analyses were performed using the SPSS statistical software package (Window version 24.0; IBM corp. in Armonk, NY; US). Risk factors of implant exposure or extrusion were compared using the fisher’s exact test and unpaired T-test. Multivariate logistic regression was also used to evaluate the associations in eyes with implant exposure or extrusion. The test of significance was performed with P < 0.05 and a confidence interval (CI) of 95%.
Results
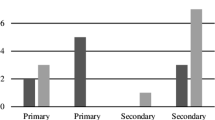
A total of 79 patients who underwent orbital evisceration with primary orbital implant placement were reviewed. 33% (26/79) of patients were diagnosed with endophthalmitis and the average age was 75 standard deviation (±) 12 (range: 56–88) years old. The average postoperative follow up was 74 ± 46 (24–180) months. The most frequent size of implant used was 20 mm (43%, 11/26 of patients), and the average size was 17 ± 3(14–20) mm. Silicone (69%, 18/26) was the most commonly used orbital implant material, followed by acrylic (5/26), porous polyethylene (2/26) and glass (1/26). 81% (21/26) of patients underwent single scleral closure, and 19% (5/26) of patients had double scleral closure with orbital implant placed posterior to the posterior sclera. 27% (7/26) of patients had an endogenous source of infection (6 = Klebsiella pneumoniae related liver abscess and 1 = Haemophilus influenzae related nephropathy complicated with urinary tract infection). Up to 53% (14/26) of patients suffered orbital implant exposure or extrusion at 7 months after surgeries. Orbital implant exposure or extrusion was significantly associated with eyes with endophthalmitis when compared to other surgical indications in our study (54% vs 17%, P < 0.05). The post-operative complications are summarized in Table 1.
We compared the endophthalmitis patients who suffered from orbital implant exposure or extrusion to those without, and found significant associations with single sclera closure technique (100% vs 58%, P < 0.05) and endogenous endophthalmitis (50% vs 0%, P < 0.05) with univariate analysis (Table 2). Multivariate analysis showed that only endogenous endophthalmitis was associated with implant exposure or extrusion (P < 0.05) (Table 3).
Discussion
Over the years, it is debatable whether one should perform primary orbital implant placement in eyes with endophthalmitis. Some suggested that orbital implant placement should be delayed and therefore reduces the risk of implant exposure or extrusion [6, 7]. Meanwhile, primary implant placement is more cost effective and avoids a second stage operation in patients [8]. In the past 17 years, 26 eyes with endophthalmitis underwent evisceration with primary implant placement in our centres, and they had a significantly higher rate of implant exposure or extrusion when compared to non-endophthalmitis eyes. Endogenous source of infection is considered as a risk factor of implant exposure or extrusion with multivariate analysis. Single scleral closure was associated with implant exposure or extrusion when compared to double scleral closure with orbital implant placement posterior to the posterior sclera [15] with univariate analysis.
The most common complication of orbital Implant is exposure, which can result in orbital infection and implant extrusion if there is further break down of the scleral and conjunctival layers [16]. The rate of implant exposure or extrusion varies, depending on different factors such as implant material, size, surgical technique and pegging of implant [17, 18]. The rate of implant exposure or extrusion in eyes with endophthalmitis was significantly higher when compared to the non-infected eyes in our study, and we suggest that primary orbital implant placement should be avoided in eyes with endophthalmitis. Chiu et al. recently reported that the disinsertion of the optic nerve was able to achieve an acceptable rate of implant exposure following primary implant placement in acute infected or inflamed eyes [10]. This is in keeping with our study, the 5 patients who underwent double scleral closure with optic nerve disinsertion did not experience any implant related complications. Therefore, we suggest careful preoperative planning of surgical technique and timing of implant placement for eyes with endophthalmitis to minimise the risk of implant exposure or extrusion.
Endophthalmitis is an ophthalmic emergency that can be classified according to the infection sources, and most cases had an exogenous source after ocular surgery or penetrating ocular trauma [19]. Endogenous endophthalmitis is usually a result from a distant spread of an organism which crosses the blood ocular barrier, penetrating the retina, choroid, vitreous cavity and anterior chamber of the eyes [20, 21]. Klebsiella pneumoniae is a common pathogen in endogenous endophthalmitis, and accounts for up to half of the endogenous endophthalmitis cases [22, 23]. Although intravitreal antibiotics and vitrectomy may improve the visual prognosis, over 40% of infected eyes with klebsiella pneumonia required evisceration [24]. Six of the 7 eyes with endogenous endophthalmitis showed klebsiella pneumoniae growth in our study, and they were associated with orbital implant exposure and extrusion. Bee et al. [25] reported that an elevated white blood cell count was associated with a higher risk of implant exposure, and we postulate that a severe inflamed scleral shell, tenon capsule and conjunctiva tissue may increase the risk of implant exposure or extrusion due to poor wound healing. However, whether an endogenous endophthalmitis is associated with a more severe ocular inflammation than exogenous endophthalmitis remains unclear.
Both orbital implant exposure and extrusion rates were significantly lowered when we placed the orbital implant posterior to the posterior sclera with univariate analysis. A single centre from Taiwan reported a different rates of implant extrusion in eyes with endophthalmitis undergoing different surgical techniques [14]. Jordan et al. [15] reported in 2015 a surgical technique to place the orbital implant posterior to the posterior sclera which showed a low rate of orbital implant extrusion. Our technique was similar to this reported technique [15], and we also ensured that the two relaxing posterior sclerotomy incisions were perpendicular to the two relaxing anterior sclerotomy incisions in order to decrease the tension on the wound. The double scleral closure technique with orbital implant placement posterior to the posterior sclera could be a reasonable choice of surgical technique for primary orbital implant placement in infected eyes.
Orbital implants are usually placed during orbital evisceration to correct the orbital volume loss and maximize the motility of the prosthesis to improve cosmetic outcome [26]. Adequate size of orbital implants can replace the volume and prevent anophthalmic socket deficiencies. However, an oversized implant may predispose to wound breakdown and result in wound infection [27]. The most common complication in our study was orbital implant exposure or extrusion, followed by abnormal lid position. One patient who was receiving warfarin therapy suffered from hematoma on day 1 post-surgery which self-resolved after 2 weeks. None of the patients developed sympathetic ophthalmia in an average of 70 months follow up.
There are several limitations in our study. Firstly, this is a retrospective study with inherent differences in documentation from the 2 collaborating centres. Secondly, the number of patients with endophthalmitis who underwent primary implant placement was relatively small, which is expected as it is uncommon to perform primary implant placement in infected eyes. Future studies with larger sample sizes are warranted. Thirdly, our cohort study consists only of Chinese patients. Finally, prosthetic motility measurements were not reported in this study.
Conclusion
Orbital implant exposure or extrusion was significantly higher in eyes with endophthalmitis when compared to the non-infected eyes, and they were associated with endogenous sources of infection. Double scleral closure technique with primary orbital implant placement posterior to the posterior sclera may be a reasonable option to reduce the risk of implant exposure and extrusion in eyes with endophthalmitis. We suggest avoiding primary orbital implant placement in eyes with endophthalmitis, and careful planning of surgical technique is important to minimise the risk of implant exposure or extrusion.
Summary
What was known before
-
The option of primary orbital implant placement in eyes with endophthalmitis during evisceration remains controversial. The risk factors of orbital implant exposure or extrusion, and their significance, after evisceration, remains underexplored.
What this study adds
-
Primary implant placement during evisceration should be avoided in eyes with endophthalmitis especially in those with an endogenous source, and double scleral closure technique may be a better alternative for primary orbital implant placement in infected eyes.
Data availability
All relevant raw data will be freely available to any researcher wishing to use them for non-commercial purposes, without breaching participant confidentiality.
References
Soares IP, França VP. Evisceration and enucleation. Semin Ophthalmol. 2010;25:94–7.
Dada T, Ray M, Tandon R, Vajpayee RB. A study of the indications and changing trends of evisceration in north India. Clin Exp Ophthalmol. 2002;30:120–3.
Tsai YY, Tseng SH. Risk factors in endophthalmitis leading to evisceration or enucleation. Ophthalmic Surg Lasers. 2001;32:208–12.
Yousuf SJ, Jones LS, Kidwell ED Jr. Enucleation and evisceration: 20 years of experience. Orbit 2012;31:211–5.
Viswanathan P, Sagoo MS, Olver JM. UK national survey of enucleation, evisceration and orbital implant trends. Br J Ophthalmol. 2007;91:616–9.
Shore JW, Dieckert JP, Levine MR. Delayed primary wound closure. Use to prevent implant extrusion following evisceration for endophthalmitis. Arch Ophthalmol. 1988;106:1303–8. 10
Walter WL. Update on enucleation and evisceration surgery. Ophthalmic Plast Reconstr Surg. 1985;1:243–52.
Holds JB, Anderson RL. Primary vs Delayed Implant in Evisceration. Arch Ophthalmol. 1989;107:952.
Tawfik HA, Budin H. Evisceration with primary implant placement in patients with endophthalmitis. Ophthalmology 2007;114:1100–3.
Chiu SJ, Tan JHY, Currie ZI. To implant or not to implant: emergency orbital eviscerations with primary orbital implants. Eye. 2021;35:3077–86.
Kim JM, Sung JY, Lim HB, Choi EJ, Lee SB. Risk Factors for Orbital Implant Extrusion after Evisceration. J Clin Med 2021;10:3329. Published 2021 Jul 28
Dresner SC, Karesh JW. Primary implant placement with evisceration in patients with endophthalmitis. Ophthalmology. 2000;107:1661–4; discussion 1664–5.
Relhan N, Forster RK, Flynn HW Jr. Endophthalmitis: Then and Now. Am J Ophthalmol. 2018;187:xx–xxvii.
Liu D. A comparison of implant extrusion rates and postoperative pain after evisceration with immediate or delayed implants and after enucleation with implants. Trans Am Ophthalmol Soc. 2005;103:568–91.
Jordan DR, Stoica B. Evisceration with implant placement posterior to posterior sclera. Ophthalmic Plast Reconstr Surg. 2016;32:178–82.
Curragh DS, Kamalarajah S, Lacey B, White ST, McNab AA, Kalantzis G, et al. Primary replacement for the management of exposed orbital implant. Orbit 2019;38:461–7.
McElnea EM, Ryan A, Fulcher T. Porous orbital implant exposure: The influence of surgical technique. Orbit. 2014;33:104–8.
Nunery WR, Heinz GW, Bonnin JM, Martin RT, Cepela MA. Exposure rate of hydroxyapatite spheres in the anophthalmic socket: Histopathologic correlation and comparison with silicone sphere implants. Ophthalmic Plast Reconstr Surg. 1993;9:96–104.
Durand ML. Endophthalmitis. Clin Microbiol Infect. 2013;19:227–34.
Sadiq MA, Hassan M, Agarwal A, Sarwar S, Toufeeq S, Soliman MK, et al. Endogenous endophthalmitis: Diagnosis, management, and prognosis. J Ophthalmic Inflamm Infect. 2015;5:32.
Chee SP, Jap A. Endogenous endophthalmitis. Curr Opin Ophthalmol. 2001;12:464–70.
Wong JS, Chan TK, Lee HM, Chee SP. Endogenous bacterial endophthalmitis: An east Asian experience and reappraisal of severe ocular affliction. Ophthalmology 2000;107:1483–91.
Chen YJ, Kuo HK, Wu PC, Kuo ML, Tsai HH, Liu CC, et al. A 10-year comparison of endogenous endophthalmitis outcomes: an east Asian experience with Klebsiella pneumoniae infection. Retina 2004;24:383–90.
Yang CS, Tsai HY, Sung CS, Lin KH, Lee FL, Hsu WM. Endogenous Klebsiella endophthalmitis associated with pyogenic liver abscess. Ophthalmology 2007;114:876–80.
Bee YS, Lin MC, Sheu SJ, Ng JD. Elevated white blood cell count may predict risk of orbital implant exposure. Can J Ophthalmol. 2014;49:45–9.
Su GW, Yen MT. Current trends in managing the anophthalmic socket after primary enucleation and evisceration. Ophthal Plast Reconstr Surg. 2004;20:274–80.
Jordan DR. Problems after evisceration surgery with porous orbital implants: Experience with 86 patients. Ophthalmic Plast Reconstr Surg. 2004;20:374–80.
Author information
Authors and Affiliations
Contributions
All authors were responsible for the design of this study, extracting and analyzing data, drafting the manuscript, revising the manuscript critically, creating 'Summary of findings’ tables, provided feedback on the study and updated reference lists.
Corresponding author
Ethics declarations
COMPETING INTERESTS
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Lai, K.K.H., Au, A.K.H., Kuk, A.K.T. et al. Surgical outcomes of orbital evisceration with primary orbital implant placement in patients with endophthalmitis. Eye 37, 1361–1364 (2023). https://doi.org/10.1038/s41433-022-02135-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02135-x