Abstract
Background
Ophthalmic examinations are mostly documented using sketches and written descriptions. Improvements in app security and IT infrastructure mean that high-quality anterior segment photographs can be routinely collected with smartphones alone. The lid oncology team relied on pre-operative formal slit-lamp imaging in the one-stop biopsy clinic, a lengthy process with capacity limitations, that risked delays to care.
Methods
A Bring Your Own Device (BYOD) photography service was developed through a series of iterations and collaborations. Healthcare Assistants took photographs on iPhone SE with Quikvue lens attachments in Pando app. Lesions requiring a slit lamp were photographed by the doctor. Images were uploaded to the patient record twice weekly. The service was evaluated using time–motion studies, imaging quality and utility grading, and patient feedback.
Results
BYOD photography saved lid oncology patients 41 min (one-third of total appointment time) and reduced delays to treatment to zero. A patient survey reflected the acceptability of the service, with 100% feeling photography was important at every visit. In terms of utility, 97.5% of smartphone images were suitable for monitoring lesions and making management decisions. The management plan based on the smartphone photographs was consistent with the management plan formulated face-to-face in clinic in 92.5% images.
Conclusion
BYOD photography has replaced formal slit-lamp imaging in the lid oncology service. This sustainable, cost-effective BYOD solution requires little training and can be adapted, reproduced, and scaled globally. BYOD photography can offer detailed records to monitor progress, contribute to remote care models, improve patient experience, and reducing medical error.
Similar content being viewed by others
Background
Bring Your Own Device (BYOD) refers to employees using personal devices for work purposes. Studies exploring BYOD in healthcare suggest that use of personal devices can improve productivity, efficiency, and communication, and reduce device procurement costs [1].
However, BYOD implementation in the NHS has been limited by concerns over data security. The sensitive and confidential nature of clinical data make potential security breaches an unacceptable risk [2] and lack of standardisation between BYOD policies make it difficult to fully utilise [3]. Recently, frameworks in data security have been developed for healthcare technology companies, and improvements in cybersecurity have made BYOD solutions more plausible [4]. Information Governance teams understand that if BYOD policies are not developed, employees could utilise unofficial BYOD channels, which pose greater risk [5]. New secure applications have been developed in line with NHS cybersecurity guidelines, which allow images to be captured and stored securely within the application, compartmentalised from the device itself [6]. In addition, hardware improvements mean that personal devices can be used in ways not previously possible. Modern smartphone cameras now produce high-resolution photographs thanks to increased megapixels, optical image stabilisation and image signal processors.
The main tool for ophthalmic examination, the slit-lamp biomicroscope, allows individual cells to be seen within the eye. Modern smartphone cameras have the capability to capture this level of detail. However, documentation uses written descriptions and freehand sketches, losing vast amounts of clinical detail. Our emergency eye-care structure often involves offering remote advice out-of-hours. This advice is often based on verbal descriptions from referring clinicians, who often have little training in eyes. Decisions are made without the support of visual clues, creating a high-risk environment for medical error.
The advantages of photographs to document and monitor disease process are well described, and clinical photography is established in many medical specialities [7,8,9]. In ophthalmology, medical photography, alongside other specialised imaging modalities, form a fundamental part of clinical decision-making. Until recently, ocular photography was limited to slit-lamp cameras, priced around £25,000 per unit. The cost is prohibitive, and as a result many ophthalmology departments do not have photography access. Studies have shown that image quality from digital cameras mounted to the slit-lamp eye piece are comparable to formal slit-lamp cameras [10] and recent developments of slide-on magnification lenses with LED lights, have meant that high-resolution anterior segment photographs can be taken with smartphones without a slit-lamp. With 99% of doctors and 95% of nurses in the UK owning a smartphone [11], this is technology that can be harnessed over a wide range of clinical scenarios and has the potential to significantly aid ophthalmic care.
The benefits of BYOD camera technology have been yet more evident in the remote consultation services that have been adopted through the Covid-19 pandemic [12]. The change in delivery of clinical services through the pandemic has unveiled an evident need to streamline the pathways used to capture clinical photographs. There is a move in healthcare to improve services using user-centred design principles. User-centred service design is the term applied to a multidisciplinary approach, which combines methods from several disciplines using design tools to co-ordinate the delivery of high-quality, efficient services, with greater impact. In the context of healthcare, these services aim to meet targets, whilst providing more-personalised care, and reduce the burden on frontline staff [13].
The lid oncology service in the adnexal department at Moorfields Eye Hospital offers a one-stop biopsy clinic for patients with potentially malignant eyelid and conjunctival lesions. Patients are required to undergo photography prior to the biopsy, as per gold standard procedure set out by the British Association of Plastic, Reconstructive and Cosmetic Surgeons code of practice [14].
These photographs were previously captured using a Haag Streit BX 900 LED (Light Emitting Diode) slit-lamp camera by trained medical photographers, in the imaging suite. This process placed time pressure on patients to return to adnexal clinic in time to undergo biopsy. Due to capacity limitations, on average 1-2 patients per could not have photographs, resulting in reliance on pre-operative photographs provided by the patient, or rebooked biopsy slots, risking delays to treatment. During the first wave of Covid-19 in March 2020, this movement through the hospital was also identified as a transmission risk due to the increased time spent in a public building, and additional contact points.
The aim of this paper is to describe and evaluate a new BYOD clinical photography service in the lid oncology clinic, to improve patient experience and reduce pressure on staff, whilst ensuring every patient underwent pre-operative high-resolution photography.
Materials and Methods
Photography applications and hardware
The Department of Digital Medicine evaluated several applications for secure photography. Applications included Consultant Connect Ltd (Oxford, UK), Hospify (Lancashire, UK), Signal Messenger LLC (Signal Technology Foundation, California, USA), Wire (Wire Swiss GmBH, Zug, Switzerland), Slack (Slack Technologies, Vancouver, Canada), Microsoft Teams (Microsoft, New Mexico USA), Pando (Forward, London, UK), Accurx (London, UK), Celo (Auckland, NZ) and Cinapsis (London, UK). Each application was given red, amber or green score on the following parameters: Application security, photograph capabilities, image compression, cost to user, export security, group functions, personal privacy and overall ease of use. Pando was considered the most appropriate application for this project at the time, due to the security benefits, location of servers within the UK and ability to maintain photograph resolution. The team noted that applications are updated regularly and that frequent reviews would be required.
Hardware comparisons were made between slit-lamp smartphone mounts. Celestron NexYZ (Celestron 81055, California, USA), Orion Steadypix (Orion Optics, Staffordshire, UK) and MicroREC (Custom Surgical GmBH, Munchen Germany) 3D-printed mounts were compared based on price, ease of use and compatibility with various smartphones and slit lamps. Celestron was considered the most versatile and cost-effective. Magnification lenses were also compared, including Quikvue (Visuscience Meditech Co Ltd, Shanghai, China), Selvim phone camera lens kit (Shenzhen Laika Technology Co., Shenzen, China), Luxsure Professional iPhone Lens (Luxsure Group, Paris, France) and Apexel Universal Phone Camera Lens Kit (Apexellens, Shenzen, China). The Quikvue was the only lens that was CE marked and offered LED lights to illuminate the subject.
Project design
The lid oncology team in the Oculoplastic department at Moorfields Eye Hospital worked collaboratively with the medical imaging department and the Department of Digital Medicine, a dedicated clinical informatics team, who use data and digital technology to support efficient and safe delivery of patient care.
Time and motion studies were performed on patients attending the medical photography suite from the lid oncology service between October and December 2020. These determined the additional time required to undergo photography, and the number of additional contact points.
Time–motion studies were also performed for these same patients to subsequently undergo BYOD photography within the lid oncology clinic space. Photography was performed using NHS Digital approved Pando application (Pando, Forward Clinical Ltd, London, UK), a secure photography and instant messaging application, whose compartmentalised data is stored only in the NHS-approved secure cloud. Pando app was approved for the acquisition and sharing of identifiable clinical data on personal devices in line General Medical Council guidance by the Trust’s information Governance team in March 2020, following a successful Data Protection Impact Assessment. The images were taken within Pando application using the registrar’s iPhone 7.
Image quality was assessed by MD and HT, and management plans were provisionally formulated based on the smartphone images versus formal slit-lamp images to determine clinical correlation. Assessment of images was carried out by two independent oculoplastic consultants (HT and CD) based on the following parameters related to the clinical usefulness of the image: image suitability for monitoring lesions, ability to make management decisions based on the image, management decision (biopsy, monitor or discharge) and whether the management decision based on the smartphone image concurs with that of the formal slit-lamp camera. Assessment of images was also made on the following parameters related to the quality of the image. Photographs were graded as good, poor or unusable for focus, lighting, colour, magnification and movement artefact.
A new service was created following user-centred service design principles, balancing desirability, feasibility, and viability of different options. The process followed the Design Council’s Double Diamond principle to Discover, Define, Develop and Deliver through a series of iterations and collaborations [15]. A minimum viable service was created in November 2020, whereby clinicians in the lid oncology clinics used Pando application on their own smartphones (1 × iPhone 7, 1 × iPhone 11 and 1 × Huawei P20), attached to the slit lamp using the NexYZ adaptor (Celestron 81055, California, USA). Images were captured at ×10 magnification and illumination mirrors were flipped to reduce glare. After the consultation, images were sent from Pando to the linked nhs.net address, from where, the clinicians uploaded photographs to the hospital’s image database, Eyesuite (Haag Streit Group, Köniz, Switzerland) located on the secure Clinical Services server.
A formalised, second iteration of the service design was formulated through feedback from the clinical team, further time–motion studies and monthly virtual multidisciplinary collaboration. This iteration involved purchasing two Trust owned second-generation iPhone SEs (Apple Inc, California, USA). Pando app was installed on these phones and registered to generic clinic nhs.net email address. Two Quikvue lenses (Visuscience Meditech Co. Ltd, Shanghai, China) were also purchased. Quikvue is a ×15 magnification slide-on smartphone lens attachment with white and blue LED light sources. Two healthcare assistants were trained to take photographs in Pando app using iPhone SE-plus-Quikvue. Any images requiring a slit lamp were taken by the doctors in clinic on the iPhone SEs attached to the slit lamp with the NexYZ adaptor. The full photography process is summarised in Fig. 1.
Fifty-five images, collected over one month (September–October 2021), were graded by the same clinicians on the quality and clinical usefulness parameters described above. Of these, 36/55 were taken with the iPhone SE-plus-Quikvue by the healthcare assistants, and 19/55 were taken with the iPhone SE-NexYZ adaptor-plus slit lamp by doctors in clinic. It was no longer possible to compare management decisions based on smartphone photographs compared to formal slit-lamp photographs because patients no longer attended the medical imaging suite. The images were instead combined with basic history and the management decision was compared to those made face-to-face in clinic.
Patient experience is key to user-centred design principles. Patient-related outcome measures were collected via survey for patients who underwent BYOD photography during a week in June 2021. The survey included six questions using a five-point Likert scale based on their experience of and attitudes towards BYOD photography.
All patients whose lesions are biopsied are discussed at a weekly lid oncology multidisciplinary team (MDT) meeting. Data were collected on photographs missing from consecutive MDTs for one month in November 2021, and reasons for missing images were identified through mapping the image journey.
The DODM held a cross-Trust collaboration session in January 2021. Collaborators included clinicians, operations, IT, management and photography departments, The results of this session were used to inform the next iteration of the service, due to be launched following deployment of the new hospital EPR (OpenEyes v.5, Toukanlabs, London, UK) in April 2022.
Results
Time and motions studies
Sixteen patients underwent time–motion studies of the baseline service. The entire clinic process took on average 2 h 10 min and consisted of 16 contact points (Fig. 2). A third of this total time was spent undergoing photography. It took an average of 43 min for each patient to leave the oculoplastic clinic on the ground floor, travel to the medical imaging suite on the lower ground floor, register, wait, undergo photography and return to clinic.
The process involved two additional contact points over two floors. In the pilot cohort, 12.5% (2/16) returned from the photography suite without having had photographs taken and 6.3% (1/16) had their biopsy in a later clinical session.
In comparison, photographs taken in Pando with the smartphone-plus-slit-lamp took an average of 1 min and 21 s. The patient did not leave the clinic. They encountered on average 0–1 extra member of staff and had to wait on average 4 min for a trained member of staff to take the photograph.
Photographs taken in Pando using the Trust-owned smartphone-plus-Quikvue took 23 s on average. The photograph was taken when the patient had their visual acuity and intraocular pressure measurements with the healthcare assistant, which meant that no extra members of staff were encountered, and no further delays incurred. This iteration allowed ophthalmologists to review the images on the phone for quality approval prior to biopsy. There have been no reported delays to care for patients due to BYOD photography, in fact the service model was so successful, patients were no longer sent to the medical imaging suite after the first service iteration.
Timing studies were also performed for the steps taken to download the image from the NHS.net inbox to uploading it to the patient record in Eyesuite by the medical photography team. This process took on average 3 min 40 s per photograph. Delays were encountered due to photographs having not been labelled with the patient ID.
Image quality and clinical usability assessments
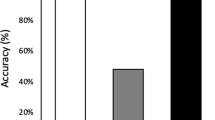
The image quality was assessed in the first service iteration, sixteen images were taken with smartphones-plus slit lamps 81.3% (13/16) of images were graded good for overall quality. In the second iteration, Nineteen smartphone-NexYZ mount-plus-slit-lamp images were collected by doctors in the clinic. Of these 89.5% (17/19) were graded good quality overall. Thirty-six smartphone-plus-Quikvue images taken by the healthcare assistants were analysed. Of these, 97.2% (35/36) graded good for overall quality. The grades for the individual quality parameters are shown in Fig. 3.
In the first iteration, 87.5% (28/32, 16 images each) of the smartphone images were deemed suitable for monitoring lesions. Of those images deemed suitable for lesion monitoring, clinicians felt able to make a management decision in 90.7% (29/32). Management plans were the same for the smartphone images and formal slit-lamp camera images in 90.7% (29/32) of patients.
In the second iteration, 2/55 of the images could not be reconciled with a patient record, 13/55 were of post-operative patients, so management assessments were formulated based on the remaining 40 images—26/36 of the smartphone-plus-Quikvue images taken by the healthcare assistants and 14/19 of the smartphone-NexYZ mount-plus-slit-lamp images were included. The reviewing consultants deemed 97.5% (78/80, 40 images each) of smartphone images suitable for both monitoring lesions and making management decisions. The two unsuitable images were slit-lamp mounted smartphone images. The management plan based on the smartphone photographs plus history was consistent with the management plan formulated face-to-face in clinic in 92.5% images (74/80). These results are summarised in Fig. 4.
Patient-reported outcome measures
Data were collected from 25 patients attending two subsequent clinics and undergoing BYOD photography. 92.0% (23/25) felt comfortable having their photograph taken in clinic and 0.0% felt uncomfortable. 100% of patients felt that their clinical team should take photographs to document their eye condition at every clinic visit and that their clinical team should be able to review previous photographs of their eye to monitor changes over time. 76.0% (19/25) preferred BYOD photography. When considering virtual diagnostic clinics, only 24% (6/24) reported that they would not be happy being seen in virtual clinics if their clinical team had access to photographs of their eye. This reflected the change in attitude to remote care since the start of the pandemic., The survey results are summarised in Fig. 5.
Images missing from the patient record
Twenty-two cases were discussed in the weekly lid oncology MDT meetings in November 2021. Of these, 18.2% (4/22) did not have images available to review on Eyesuite. All patients had photographs taken in clinic within Pando app, but the image had not been exported or properly labelled. This was supported in the findings with the collection of the 55 consecutive images, that were used for the quality grading. 18.1% (10/55) of these were not labelled. For safety, each photograph of a patient’s eye was sandwiched between photographs of their identification label. Two patient photographs (2/55) could not be reconciled with their notes.
Discussion
The Covid-19 pandemic highlighted a need to streamline clinical services to curtail viral transmission. Using a system engineering approach, any service designed to minimise patient movement, with fewer contact points, runs more efficiently, and reduces delays to care [16]. The last point being particularly important when managing potentially malignant ocular lesions. By following user-centred service design principles, and with the support of the DODM, the lid oncology team was quick to mobilise available technology and staff to improve the quality of care for patients. This BYOD photography solution has become routine service; zero patients were required to attend the medical imaging suite after June 2021 from this clinic, due to the success of the BYOD photography service design.
Prior to March 2020, approximately 15 patients per lid oncology clinic were sent for formal photography; an average of 40 patients per week. BAPRAS recommends pre-operative photographs for all surgery with cosmetic impact [14]. This guidance encompasses all oculoplastic conditions, not just potentially malignant lesions. An estimated 7800 clinical photographs would need to be captured from the oculoplastic department annually to meet this standard. BYOD photography methods have accommodated this, where previously there was not capacity.
The success of the BYOD photography service at the City Road site has led to plans to expand to satellite units, where there are no formal photography capabilities—an identified clinical safety risk. The service blueprint is reproducible for any outpatient environment requiring anterior segment imaging, due to the low cost, low complexity and digitally secure methods of image capture described in this paper. Other ophthalmic sub-specialities at Moorfields Eye Hospital are also piloting BYOD photography solutions, including ocular oncology, glaucoma, eye casualty and uveitis teams.
The high-quality images produced by Quikvue lenses and smartphones have initiated a new era of anterior segment photography that does not require a slit-lamp. This increases the scope of BYOD ocular photography as it is quick and easy to train staff to use these devices, and little or no prior ophthalmic knowledge is required to capture lesions of interest. It is worth noting that the Quikvue is not compatible with certain models of Android smartphones where the camera is placed in the centre of the phone.
The ability to make management decisions based on smartphone photographs, and the consistency of these decisions with face-to-face management plans, could unlock the potential for BYOD photography in virtual models of care. The adnexal team and DODM are exploring options for monitoring patients with stable lid lesions using BYOD photography in diagnostic clinics, as well as offering photography services to those who are referred from external units with inadequate photographs to aid triage and referral refinement. It also helps to address ‘digital exclusion’ in patients, who are increasingly asked to digitally engage in their medical care, through supporting easy to use home-monitoring and unlocking community-based photography by non-ophthalmic clinicians. The ubiquity and familiarity of smartphone photography means that very little training is required to produce high-quality photographs, and slide-on magnification lenses eliminate dependency on a slit lamp or specialist equipment for anterior segment imaging.
Pando app is free to use, the Quikvue, £115, The NexYZ, £50, and if a smartphone is purchased, the £399 iPhone SE within most departmental budgets. This hardware costs a fraction compared to formal slit-lamp cameras and allows units to expand photography solutions where previously not considered. Importantly, it unlocks the potential for photography to improve documentation and monitoring of ophthalmic conditions and support remote decision-making in less economically developed areas of the world. This cost-effective solution to capacity limitations in formal imaging departments means that trained medical photographers can be utilised elsewhere, particularly important with the rise in complexity of posterior segment imaging modalities.
Limitations of this paper include the fact that the original comparisons were made between smartphone images taken by untrained clinical staff to formal slit-lamp photographs taken by trained professionals. Subsequently, the differences in perceived quality may represent the staffs’ photographic capabilities rather than the hardware. In the second iteration, the team was unable to compare the quality of the Quikvue images to formal slit-lamp photography, because of the change in service pathway. Instead, images were compared with face-to-face clinic outcomes, risking confounding interpersonal differences in management of certain cases. To reduce this bias, two consultants graded the usability of the images. For consistency, these were the same two consultants who graded the initial smartphone and formal slit-lamp photographs. There was a risk of recall bias because it was possible the consultants may have had previous consultations with the patients.
When implementing a new service, it is important to identify and mitigate risk. The current BYOD photography service contains elements that have been identified as barriers to scaling the solution and could introduce clinical risk. These risks were identified through mapping the image journey and noting incomplete steps. Firstly, the use of external applications such as Pando to take clinical photographs can create “orphan medical records,” where key clinical data is not integrated into the patient’s record and therefore inaccessible to key clinical care providers. Pando app was not developed primarily to link to other IT systems. As a result, several manual processes are required to ensure images and data are transferred. These processes include renaming the image with patient’s hospital number, exporting, and checking for error messages. Another staff member uploads images to patient records from the inbox. This relies on the image having been correctly labelled and exported, and it depends on staffing capacity to monitor the inbox.
A Trust-wide collaborative session was held in January 2022 to address these issues. The next iteration of the service will allow secure smartphone photography to be taken within the patient record on Trust-owned or personal devices, securely via a VPN (Virtual Private Network) link in the new version of OpenEyes—Go Live date expected April 2022. This update eliminates the manual processes involved in renaming, exporting, and uploading images, reducing burden on the medical photography team, and allowing this service, along with other BYOD photography solutions, to be rapidly scaled internally.
Conclusion
The last 18 months have seen a change in attitude towards the traditional outpatient clinic model. The lid oncology department has demonstrated a sustainable, cost-effective, and reproducible BYOD photography service that can be adapted, reproduced, and scaled globally. Smartphone camera technology is only set to improve and advances in Trust IT infrastructure can ensure smooth automated processes for BYOD photography. This will allow detailed records to compare progress, base clinical decisions on and contribute to remote care models, improving patient experience, and reducing medical error.
Summary
What was known before
-
The benefits of smartphone photography for retinal imaging have been explored in low resource settings Improvements in anterior segment smartphone photographs have led to pilot studies proving worth in cataract assessment, corneal pathology monitoring and glaucoma bleb grading.
-
Smartphones and BYOD devices are increasingly being used for video-consultations in ophthalmology.
What this study adds
-
Smartphone photography can be incorporated into routine clinical practice to improve efficiency and patient flow.
-
BYOD photography using smartphones can be used to document anterior segment examination findings and monitor clinical progress.
-
Management decisions based on smartphone photographs correlate with face-to-face management decisions, meaning BYOD smartphone photography can support remote and virtual models of care
Data availability
The data that support the findings of this study are available on request from the corresponding author, CK. The data are not made publicly available due to the inclusion of photographs that could compromise the privacy of the participants.
References
Nerminathan A, Harrison A, Phelps M, Alexander S, Scott KM. Doctors’ use of mobile devices in the clinical setting: a mixed methods study. Intern Med J. 2017;47:291–8.
Wani TA, Mendoza A, Gray K. Hospital bring-your-own-device security challenges and solutions: systematic review of Gray literature. JMIR Mhealth Uhealth 2020;8:18175.
Moyer JE. Managing mobile devices in hospitals: a literature review of BYOD policies and usage. J Hosp Librarian. 2013;13:197–208.
NHSx. Bring your own device guidance. 2021. https://www.nhsx.nhs.uk/informationgovernance/guidance/bring-your-own-devices-byod-ig-guidance/#healthcare_worker.
Mars M, Scott RE. WhatsApp in clinical practice: a literature review. Stud Health Technol Inf. 2016;231:82–90.
NHSx. Digital tool assessment criteria version 1. 2019. https://www.nhsx.nhs.uk/keytools-and-info/digital-technology-assessment-criteria-dtac/.
Aveta A, Filoni A, Persichetti P. Digital photography in plastic surgery: the importance of standardization in the era of medicolegal issues. Plast Reconstr Surg. 2012;130:490–1.
Kunde L, McMeniman E, Parker M. Clinical photography in dermatology: ethical and medico-legal considerations in the age of digital and smartphone technology. Australas J Dermatol 2013;54:192–7.
Morse GA, Haque MS, Sharland MR, Burke FJ. The use of clinical photography by UK general dental practitioners. Br Dent J. 2010;208:14–15.
Oliphant H, Kennedy A, Comyn O, Spalton DJ, Nanavaty MA. Commercial slit lamp anterior segment photography versus digital compact camera mounted on a standard slit lamp with an adapter. Curr Eye Res. 2018;43:1290–4.
Mobasheri MH, King D, Johnston M, Gautama S, Purkayastha S, Darzi A. The ownership and clinical use of smartphones by doctors and nurses in the UK: a multicentre survey study. BMJ Innov. 2015;1:174–81.
Kilduff CL, Thomas AA, Dugdill J, Casswell EJ, Marcin Dabrowski M, Lovegrove C, et al. Creating the Moorfields’ virtual eye casualty: video consultations to provide emergency teleophthalmology care during and beyond the COVID-19 pandemic. BMJ Health Care Inform. 2020;27:100179.
Shaw J, Agarwal P, Desveaux L, Cornejo Palma D, Stamenova V, Jamieson T, et al. Beyond “implementation”: digital health innovation and service design. NPJ Digit Med. 2018;1:48.
British Association of Plastic Reconstructive and Aesthetic Surgeons Code of Practice (BAPRAS). 2019. http://www.bapras.org.uk/docs/default-source/default-documentlibrary/code-of-practice-2019_final.pdf?sfvrsn=2.
Altman M, Huang TTK, Breland JY. Design thinking in health care. Prev Chronic Dis. 2018;15:E117.
Chong YJ, Henry M, Logeswaran A, Sivaraj R. Planning ophthalmology workflow in response to the Covid-19 pandemic: a systems engineering approach. J Improvement Sci. 2020;69:1–10.
Acknowledgements
The authors would like to acknowledge Safwana Abdulrasid and the wider team at the Department of Digital Medicine at Moorfields Eye Hospital for collaborating and brainstorming ideas to improve the service. They would also like to acknowledge Richard Poynter and Hemali Ranawaka in the medical photography department for running the image upload service. They would like to acknowledge Carl Nicholls for his technical expertise and contributions. Finally, they would like to acknowledge Halima Musse and Victor, the healthcare assistants in the lid oncology service, for expanding their roles to run the in-clinic BYOD photography service.
Author information
Authors and Affiliations
Contributions
CK is the corresponding author and contributed to designing the work that led to the submission, acquired data, and played an important role in interpreting the results. She revised the manuscript. She approved the final version. She agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. MD contributed to designing the work that led to the submission, acquired data, and played an important role in interpreting the results. She drafted the manuscript. She approved the final version. She agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. GG played an important role in interpreting the results. She approved the final version of the manuscript. JN contributed to designing the work that led to the submission. She approved the final version of the manuscript. CD contributed to designing the work that led to the submission, acquired data, and played an important role in interpreting the results. She approved the final version of the manuscript. She agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. PT contributed to designing the work that led to the submission. He approved the final version of the manuscript. CL contributed to designing the work that led to the submission. DS contributed to designing the work that led to the submission. HT contributed to designing the work that led to the submission, acquired data, and played an important role in interpreting the results. She revised the manuscript. She approved the final version. She agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kilduff, C.L.S., Deshmukh, M., Guevara, G. et al. Creating a secure clinical ‘Bring Your Own Device’ BYOD photography service to document and monitor suspicious lesions in the lid oncology clinic. Eye 37, 744–750 (2023). https://doi.org/10.1038/s41433-022-02049-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02049-8
This article is cited by
-
Korneale Endothelzellfotografie: Vergleich von Smartphones
Die Ophthalmologie (2023)