Abstract
Background/objectives
This study aims to benchmark the training programs of European ophthalmology residents.
Subjects/Methods
An online survey, aimed at European ophthalmology residents in training and those within two years of completion, was sent through the national representatives of the European Society of Ophthalmology, Young Ophthalmologists section (SOE-YO). The study involved 214 subjects representing 36 of the 44 European countries offering ophthalmology training programs.
Results
Among the surveyed, 74.8% of participants had an official national curriculum; 55.8% had a national specialty examination to accredit their training as ophthalmologists. 45.8% were satisfied or very satisfied with the clinical skills acquired, while 42.1% were completely dissatisfied with the surgical skills achieved. Considering the 4th year residents (mean duration of the residency), many of them did not perform phacoemulsification surgery (34%), pterygium excision (46.9%), or repair of eyelid laceration (31.3%).
Conclusions
There is great heterogeneity in the competencies achieved by residents in training according to their country of origin, especially in terms of surgical competences.
Similar content being viewed by others
Introduction
Residency programs have been established as the pillar of the medical specialization training. As modern Ophthalmology undergo further subspecialisation, the importance of training could not be understated. However, despite its importance, there is currently no consensus on the medical and surgical competences that a trainee should acquire during residency in order to obtain certification to practice as an ophthalmologist in the different countries in Europe. This causes enormous variations of training experience among trainees in different countries in the continent. Additionally, the lack of standardization in terms of ophthalmic training does not facilitate globalization, labor/skills interchange, clinical and scientific collaboration, and people movement that was enshrined by the European Union acquis communautaire since 1995 [1]. Thus, the training of professionals should include minimum standards regardless of the country in which they have been trained in order to guarantee optimum patient care.
In this context, the Union of the European Medical Specialists (UEMS) attempts to harmonize the training of specialists to the highest possible level. For Ophthalmology, the UEMS has offered guidelines [2] to be followed by European countries, including the possibility to evaluate the level of training individually acquired with the European Board of Ophthalmology (EBO), founded by the UEMS in 1992 [3]. However, each European country ultimately decides the extent of adopting these guidelines and whether the EBO is a necessary step for trainees to be certified as ophthalmologists.
There is currently a paucity of information regarding the training content and conditions in the different European countries. Thus, the aim of this study is to benchmark ophthalmology residency training in European countries, to assess the differences and possible deficiencies, and to gauge among the trainees their degree of satisfaction with residency training, in order to harmonize and enhance training in Ophthalmology across Europe.
Materials and Methods
A survey was conducted using the online platform GoogleForm(R) between November 2018 and January 2020. We targeted all the European young ophthalmologists (YOs) who were undertaking residency training and those within 2-years of completing residency training. We asked YOs in training to respond based on their training experience up to the time of the survey. If the respondents have completed residency training, we asked them to respond according to the overall experience of their residency.
The survey was developed and refined by the fellowship subcommittee of the European Society of Ophthalmologists, Young Ophthalmologists section (SOE-YO). The subcommittee included both members-in-training and YOs in clinical practice, in addition to a senior faculty who is experienced in quality studies and survey design. The survey is consisted of 5 different sections: personal data, content of the training curriculum, characteristics of the training program, medical and surgical competencies, and degree of satisfaction and agreement. The survey questions can be found in the supplementary information section (available at Eye´s website). Regarding the medical competencies, respondents were asked to self-assess their level of confidence in performing different procedures using a Likert scale. The values were distributed as follows: 1 = not at all confident, 2 = slightly confident, 3 = somewhat confident, 4 = confident and 5 = very confident. We ensured that the wording and interpretation were understandable for YOs in all European regions and that all answer possibilities were covered. The survey was designed to take no longer than 25 min to complete. The validity of the questionnaire was verified after a detailed review of each question by the SOE-YO committee. All personal data and privacy were protected according to the General Data Protection Regulation (GDPR) of the European Union [4] and only anonymized data was used in the analysis.
To facilitate the distribution of the survey, we identified all the YO members on the SOE email distribution list and sent them a URL of the survey via email. Additionally, national representatives of the SOE-YO section assisted in approaching potential participants in their corresponding country. Finally, the survey was also advertised on the SOE social media platform and in the newsletter of the SOE-YO.
Statistical analysis was performed using IBM SPSS V. 25 software (SPSS, Chicago, IL, USA) and GraphPad Prism Software (GraphPad Software, CA, USA). Median, standard error of the mean [SEM], and 95% confidence interval (CI) were calculated. Non-parametric Kruskal–Wallis test was used for data comparisons. Correlation analysis was performed using the Pearson correlation coefficient for bivariate variables. A p < 0.05 is considered statistically significant. A linear regression analysis was performed, determining the R2 value and considering significant also those results with p-value < 0.05.
Results
Participants demographics
After excluding those who submitted incomplete responses (n = 25), 214 participants were included in data analysis. These participants represent 36 European countries, all of which offer ophthalmology residency training. The median number of participants per country was 7 [SEM, 0.02]. The country with the highest number of participants was Portugal (n = 19), followed by France and Turkey (n = 18 each) (Fig. S1). Austria, Iceland, Kazakhstan, Latvia, and Montenegro offer ophthalmic residency training programs but were not represented by any participants.
Among the respondents, 83% (178/214) indicated that they undertake residency training in a public medical system, 13% (28/214) in a mixed public-private model, and 4% (8/214) exclusively in a private medical center. At the time of the survey, 63% of the participants (134/214) were residents, 9% (20/214) fellows (post-residency trainee), and 28% (60/214) ophthalmologists/consultants (post-training position). Among the participating residents, 21% were in their first year of training (28/134), 18% in the second year (24/134), 23% in the third year (31/134), 23% in the fourth year (31/134), 13% in the fifth year (17/134) and 2% in the seventh year (3/134). Fig. S2.
General organization of the residency programs
The median for the duration in years of ophthalmology training of the survey participants was 4 [0.07] (Fig. 1). The countries with the longest training were Ireland and the United Kingdom with 7 years. By contrast, Ukraine and Russia (2 years) and Belarus (one and a half years), were the countries with the shortest training.
Among all the respondents, 74.8% stated that they had a national residency curriculum common to all training centers; 20.6% did not have one; and 4.7% did not know if they have one. Additionally, 22.9% indicated that they had regional or local programs different from the national curriculum, while 69.6% did not and 7.5% were unsure. 69.2% of participants responded that they had an assigned mentor during their training period (Fig. S3). The time to spend in each subspecialty was not defined by the program in 49% of respondents. In those cases where it was defined, this period was between 2 to 6 months depending on the subspecialty. Strabismus, Retina, Glaucoma, and Cornea-Anterior Segment present a length of 4-6 months. Cataract, Oculoplastics, Oncology-Pathology, Neuro-Ophthalmology, Refractive surgery, Trainees´ area of interest, and Observership program last 2–3 months (Fig. S4).
Regarding accreditation, 55.8% reported the presence of a mandatory certification process, either in the form of a specific national examination or a national board for Ophthalmology, while 20.6% are not required to sit any mandatory examination prior to practicing as an independent ophthalmologist. The remainder is required to sit regional examinations, the EBO or the ICO (International Council of Ophthalmology) examinations (Table S1).
Only 17.3% of the respondents had a program that defined the number of on-call days to be performed each month. 78% performed on-call days in the initial phase of their residency, increasing this percentage to 91.6% for the middle and final phases of the residency period (Fig. S5).
Medical competences
Most of participants reported a good level of confidence in the clinical competencies achieved during their training period. The respondents reported the highest confidence in the examination of the visual field by confrontation, the measurement of intraocular pressure, and the examination of the fundus of the eye. Conversely, procedures in which respondents felt least confident in were the forced duction test, interpretation of electrophysiology studies, indirect ophthalmoscopy with scleral indentation, and prism cover test (Table 1).
Surgical competencies
Table 2 shows the surgical exposure among participants in relation to their stages of training at the time of the survey.
Respondents that reported to have a curriculum were asked about the minimum surgical cases mandated by their residency training program, and the results are shown in Table S2.
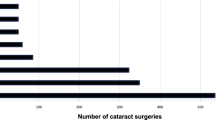
Regarding cataract surgery, based on those who have a minimum surgical number mandated by their training program, the median number of phacoemulsification surgery required for each trainee was 25 [14.3]. The number of surgeries performed per resident in each European country is shown in Fig. 2. The countries in which residents perform the highest number of phacoemulsification surgeries were Portugal (250 surgeries), United Kingdom (235), and Greece (119). When the median minimum number estimated from our survey was used as a threshold, 59.7% of all surveyed participants performed less than 25 cases, while within the remaining 40.3% there were some participants who were able to perform more than 200 surgeries. Focused on those respondents in their 4th to 7th year of residency or those who already finished, the median of phacoemulsification surgeries performed were 50 [14] during the residency period, and 46.8% of them performed less than 25 cases.
Most of the respondents (72%) indicated that they should perform an average minimum of 100 cataract surgeries in order to feel surgically independent. The values for other cataract surgery subtypes depending on the country can be found in Table S3. The median values per country for other surgeries (repair of palpebral lacerations or enucleation, among others) can be consulted in Fig. 2 (specific data for each type of surgery and country can be consulted in Table S4). By surgeries, we mean procedures performed in the operating room. Therefore, procedures such as laser photocoagulation or intravitreal injections, which can be performed in the office or in a clean room set up for this purpose, were excluded.
Degree of satisfaction/agreement
The majority of participants (69%) were in favor of an official program common to all European countries (Fig. 3A). Most participants agreed (40.6%) or completely agreed (23.8%) with the need to complete an exam (e.g., EBO or ICO) in order to be eligible to practice as an ophthalmology specialist (Fig. 3A). The majority of respondents indicated that they were moderately satisfied (36.9%), very satisfied (39.7%), or completely satisfied (6.1%) with the clinical competencies achieved during their residency. However, regarding surgical competences, 42.1% of respondents indicated that they were not at all satisfied with their acquired surgical skills (Fig. 3B).
There was a significant positive correlation between the degree of satisfaction of the participants with the acquired surgical skills during their training period and the total number of surgeries performed for all the surgical techniques analyzed (p < 0.05), except for ECCE, ICCE and enucleation-evisceration surgeries. The highest correlations found based on the Pearson´s coefficient were total phacoemulsification surgeries (0.40), followed by total glaucoma filtration surgeries (0.25) and total eyelid lacerations repair surgeries (0.20). The highest value of the coefficient of determination (R2) was obtained for the total phacoemulsification surgeries performed (0.16), showing a very low capability of the linear regression predictions to fit the data (Table S5).
We found no significant correlation between the length of residency and the average confidence level in the clinical competencies acquired by respondents (p > 0.05). Similarly, we found no statistically significant correlation between the degree of satisfaction of the participants with the duration of the residency and the total duration (in years) of the training program (p > 0.05).
Discussion
In this work, we highlight the differences in various aspects of ophthalmology residency training in different European countries. This heterogeneity covers multiple fields from duration of residency to medical and surgical competences achieved.
Globally, various organizations have defined medical and surgical standards, including minimum surgical competencies to be achieved by ophthalmology residents before completing their training. Among those, the Accreditation Council for Graduate Medical Education (ACGME) in the USA [5], the International Council of Ophthalmology (ICO) [6] and the Pan American Council of University Professors of Ophthalmology (PACUPO) [7], are some of the more well-known examples [8].
Despite of the disparities in terms of the duration of the residency, ranging from 1.5 to 7 years, most of the countries establish training programs of ≥4 years. Eight countries have residency programs that last for 3 years or less: Armenia, Azerbaijan, Belarus, Estonia, Lithuania, Moldova, Russia and Ukraine. UEMS have claimed 3 years as a minimum residency time, which may explain the observation that mainly non-EU countries with less than 3 years.
The standard competences to be achieved by the resident precise a minimum residency length in order to build confidence. However, there is no consensus among the countries to establish that minimum duration of the training program. Thus, experienced supranational committees should work on finding this consensus internationally, including a minimum curriculum to be obtained during those training years. In this sense, most of the respondents (69%) agree to have an official program common to all European countries.
This consensus should value the national programs already on going and find an equilibrium. Most of the respondents (74.8%) described that they have a national residency curriculum to be followed. The rest of the respondents (20.6%) do not have one. Surprisingly, some of the respondents (4.7%) do not know if they have a curriculum. The importance of following a residency program to acquire the necessary competences should be transmitted to the residents, not only for knowing and expecting what they will do in the residency, but also for them to demand a proper training.
The heterogenicity among countries also affects the need of a mandatory examination prior to practicing as an independent ophthalmologist. Competency assessment has been always established as a critical step in the residency training program in order to guarantee optimum training and patient safety. Different tools and strategies have been described and validated to help the assessment of ophthalmic competences [9,10,11,12,13]. including on-call performance [14]. To our surprise, some European countries (i.e., Belarus, Denmark, Finland, France, Italy, Norway, Spain, Sweden and Turkey) has no mandatory requirement for their residents to undergo any accreditation process to work as an ophthalmologist, even though training centers and trainers would recommend their trainees to undertake international exams such as the EBO or ICO diploma examination. Among those with mandatory requirement, most require their residents to sit national examinations of which the content is vastly different. According to our data, only Belgium, France and Switzerland require to pass the EBO or ICO exams, instead of national examination. Most of the respondents (64.4%) agree to have an unifying evaluation system such as EBO or ICO that endorses their residency training.
It is evident from our data that there is a deficient surgical training since a considerable proportion of the respondents are far from achieving the minimum standards set by some of the European countries included in this survey. The deficient surgical training is also reflected in the degree of satisfaction of the participants. While most were either completely satisfied (6%) or very satisfied (40%) with their medical competences, only 16.3% were completely or very satisfied with the acquired surgical competences, and 42% indicated that they were completely unsatisfied with their surgical competencies. Surgical competencies are more challenging to teach and assess compared to medical ones, as it has been previously described in ophthalmic education [15] and may explain the vastly different experience that the respondents are receiving.
If we consider the 4th year residents as a reference, as it corresponds to the median duration of residency in our study and therefore should reflect the representative final surgical volume for a given resident in Europe, more than 34% would have graduated without performing a single phacoemulsification surgery, 47% without ever excising a pterygium, and 31% never repaired any eyelid lacerations. These values are staggering especially since these are common procedures considered essential for any ophthalmologist [5]. In specific cases, medians obtained were lower than the minimum number defined by the official curriculum (e.g., 350 for phacoemulsification surgeries in the United Kingdom), which may be conditioned by fewer participants belonging to the last years of residency (only two for the 7th year), with a lower accumulated surgical experience. The lack of supervised surgical experience would logically result in insecurity in early career ophthalmologists when faced with their first independent surgeries, and likely increase their complication rate [16]. Indeed, previous studies that have shown that the complication rate among residents who have performed between 50 and 250 cataract surgeries is around 0.8%; and lower rate of complications could be reached once 250 to 350 cases have been performed [17,18,19,20]. A potential solution would be the establishment of a minimum surgical curriculum agreeable by all the European countries. This curriculum should outline the basic surgical competences to be performed and acquired by the trainee during the residency training period. Several authors have demonstrated a significant reduction in the rate of intraoperative complications by establishing a comprehensive surgical curriculum [16, 21], and the development of such a curriculum in Europe will enhance the standard of Ophthalmology training and subsequently patient safety in Europe regardless of the country of origin.
The deficient surgical training leads some of the new specialists to look for ways to prolong or complete their training, such as fellowship programs, in order to feel surgically independent [22, 23]. In this sense, very few countries have established fellowship programs as a requirement in order to become an ophthalmic consultant totally independent to perform surgery (e.g., United Kingdom). Conversely, other countries in Europe, such as Switzerland and Ireland, have subdivided training into medical and surgical streams. However, most of European countries still support that residency should enable ophthalmologists to be able to comprehensively manage common ophthalmic presentations, including those that require surgery. Thus, fellowships should not be taken as a solution to compensate deficient residency training, and should be established as a complementary subspecialisation if necessary after completing a well-defined residency programs with minimum standards.
In conclusion, this study reflects the great heterogeneity in the different residency training programs and competencies achieved by ophthalmologists in training according to their country of residency, especially in terms of surgical skills. Residency in ophthalmology has vital importance in the abilities to be acquired by the staff during the training period in order to act as an independent ophthalmologist. Thus, it would be essential for national governments as well as governing bodies (e.g., UEMS and EBO) to establish a European training curriculum common to all national teaching committees.
Summary
What was known before
-
The training of ophthalmology residents across Europe takes place in centers with very different characteristics. The competent supranational organizations are trying to standardize the training that ophthalmology residents in Europe should acquire.
What this study adds
-
There is a wide disparity in the training of residents in Europe depending on the country in which they undertake their training program. There is a high degree of satisfaction with the medical competencies acquired during residency. In contrast, a significant proportion of residents are dissatisfied with the surgical competencies acquired during their training program.
Data availability
The data that support the findings of this study are available upon request from the corresponding author, [MGA]. The data are not publicly available because they contain information that could compromise the privacy of the participants.
References
European Union. Council Directive 93/16/EEC of 5 April 1993 to facilitate the free movement of doctors and the mutual recognition of their diplomas, certificates and other evidence of formal qualifications. Off J Eur Commun. 1993; L 165/1:1–24.
Me EDES, Spe D. European Union Of Medical Specialists Chapter 6, Charter on training of medical specialists in the EU. Oncology 2004;70:115–6. https://uems.eu/__data/assets/pdf_file/0011/1415/906.pdf.
Mathysen DGP, Ringens PJ, Midena E, Klett A, Sunaric-Mégevand G, Martinez-Costa R, et al. Procedural aspects of the organization of the comprehensive European Board of Ophthalmology Diploma examination. J Educ Eval Health Prof. 2016;13:27.
Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data, and repealing Directive 95/46/EC. Off J Eur Union. 2016;59: 1–88.
ACGME. ACGME. Required minimum number of procedures for graduating residents in ophthalmology. Published online 2018. https://www.acgme.org/Portals/0/PFAssets/ProgramResources/OPH_CaseLogInfo.pdf.
International Council of Ophthalmologists. International Council of Ophthalmology Residency Curriculum. 2016; 1:1-219. http://www.icoph.org/dynamic/attachments/curriculum_documents/pdf_doc/updated-ico-residency-curriculum.pdf.
Pan-American council of university professors of ophthalmology minimum requirements for the ophthalmology residency. http://icoph.org/downloads/PACUPOOphthalmologyResidency.pdf.
Chan WH, Saedon H, Falcon MG. Postgraduate ophthalmic training: how do we compare? Eye. 2011;25:965–7. https://doi.org/10.1038/eye.2011.120.
Golnik KC, Law JC, Ramasamy K, Mahmoud TH, Okonkwo ON, Singh J, et al. The ophthalmology surgical competency assessment rubric for vitrectomy. Retina. 2017;37:1797–804. https://doi.org/10.1097/IAE.0000000000001455.
Motley WW, Golnik KC, Anteby I, Atilla H, Gole GA, Murillo C, et al. Validity of ophthalmology surgical competency assessment rubric for strabismus surgery in resident training. J AAPOS Publ Am Assoc Pediatr Ophthalmol Strabismus. 2016;20:184–5. https://doi.org/10.1016/j.jaapos.2015.12.007.
Green CM, Salim S, Edward DP, Mudumbai RC, Golnik K. The ophthalmology surgical competency assessment rubric for trabeculectomy. J Glaucoma. 2017;26:805–9. https://doi.org/10.1097/IJG.0000000000000723.
Law JC, Golnik KC, Cherney EF, Arevalo JF, Li X, Ramasamy K. The ophthalmology surgical competency assessment rubric for panretinal photocoagulation. Ophthalmol Retin. 2018;2:162–7. https://doi.org/10.1016/j.oret.2017.06.002.
Casswell EJ, Salam T, Sullivan PM, Ezra DG. Ophthalmology trainees’ self-assessment of cataract surgery. Br J Ophthalmol 2016;100:766–71. https://doi.org/10.1136/bjophthalmol-2015-307307.
Golnik KC, Lee AG, Carter K. Assessment of ophthalmology resident on-call performance. Ophthalmology 2005;112:1242–6. https://doi.org/10.1016/j.ophtha.2005.01.032.
Wentzell DD, Chung H, Hanson C, Gooi P. Competency-based medical education in ophthalmology residency training: a review. Can J Ophthalmol. 2020;55:12–19. https://doi.org/10.1016/j.jcjo.2019.07.004.
Oetting TA. Surgical competency in residents. Curr Opin Ophthalmol. 2009;20:56–60. https://doi.org/10.1097/icu.0b013e328319914f.
Randleman JB, Wolfe JD, Woodward M, Lynn MJ, Cherwek DH, Srivastava SK. The resident surgeon phacoemulsification learning curve. Arch Ophthalmol (Chic, Ill 1960). 2007;125:1215–9. https://doi.org/10.1001/archopht.125.9.1215.
Rutar T, Porco TC, Naseri A. Risk factors for intraoperative complications in resident-performed phacoemulsification surgery. Ophthalmology. 2009;116:431–6. https://doi.org/10.1016/j.ophtha.2008.10.028.
Puri S, Kiely AE, Wang J, Woodfield AS, Ramanathan S, Sikder S. Comparing resident cataract surgery outcomes under novice versus experienced attending supervision. Clin Ophthalmol. 2015;9:1675–81. https://doi.org/10.2147/OPTH.S85769.
Gupta S, Haripriya A, Vardhan SA, Ravilla T, Ravindran RD. Residents’ learning curve for manual small-incision cataract surgery at Aravind Eye Hospital, India. Ophthalmology. 2018;125:1692–9. https://doi.org/10.1016/j.ophtha.2018.04.033.
Borboli-Gerogiannis S, Jeng-Miller KW, Koulisis N, Moustafa GA, Chang KK, Chen SH, et al. A comprehensive surgical curriculum reduced intra-operative complication rates of resident-performed cataract surgeries. J Surg Educ. 76:150–7. https://doi.org/10.1016/j.jsurg.2018.07.009.
Gedde SJ, Volpe NJ, Feuer WJ, Binenbaum G. Ophthalmology resident surgical competence: a survey of program directors. Ophthalmology. Published online February 20, 2020. https://doi.org/10.1016/j.ophtha.2020.02.017.
Dean WH, Grant S, McHugh J, Bowes O, Spencer F. Ophthalmology specialist trainee survey in the United Kingdom. Eye. 2019;33:917–24. https://doi.org/10.1038/s41433-019-0344-z.
Acknowledgements
We acknowledge the SOE and its YO committee, and their National Representatives, for their help and support to validate and distribute the survey. We thank all the young ophthalmologists who responded and helped us to perform this study.
Funding
RAA and MGA acknowledge the support of the OFTARED RETICS network (RD16-0008), aimed at the prevention, early detection, treatment and rehabilitation of eye diseases—Ministry of Economy and Competitiveness/Health Institute Carlos III co-financed by FEDER funds.
Author information
Authors and Affiliations
Contributions
Conceptualization: RAA, MGA. Methodology: RAA, MGA, MLR, JP, SF. Analysis and visualization: RAA, MGA. Supervision: MGA. Writing—original draft: RAA. Writing—review & editing: MGA, SF, MLR, JP.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Anaya-Alaminos, R., Rassmussen, M.L., Fung, S.S.M. et al. Comparative analysis of European residency programs: benchmarking and harmonizing ophthalmology training in Europe. Eye 37, 725–731 (2023). https://doi.org/10.1038/s41433-022-02040-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02040-3