Abstract
This study aimed to compare efficacy and treatment burden of treat-and-extend (T&E) anti-VEGF against fixed and pro re nata (PRN) regimens for neovascular age-related macular degeneration (nAMD). MEDLINE, CENTRAL, and EMBASE were searched. Randomized-controlled trials and observational studies comparing T&E to PRN or fixed dosing for treatment-naïve AMD patients were included. Mean difference (MD) for visual acuity (VA) and number of injections are presented. Risk of bias was assessed according to Cochrane guidelines. Methodology was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). VA improvement was similar with T&E and fixed dosing at one (MD −0.08 letters, p = 0.95) and two years (MD 0.58 letters, p = 0.62). In contrast, VA improvements were significantly greater for T&E when compared against a PRN regimen at one (MD 3.95 letters, p < 0.0001) and two years (MD 4.08 letters, p < 0.001). Significantly fewer ranibizumab injections were administered in the T&E arm at one (MD –2.42 injections, p < 0.0001) and two years (MD –6.06 injections, p < 0.00001) relative to fixed dosing. Fewer aflibercept injections were likewise administered to patients on a T&E regimen versus fixed dosing at one year (MD –0.78 injections, p < 0.0001). Low-certainty evidence from the present synthesis implies that T&E preserves VA similar to fixed schedules with significantly fewer injections at one and two years. Also, patients with T&E dosing achieved better VA outcomes than those on PRN regimen but T&E dosing was associated with more injections.
摘要
本研究旨在比较治疗-延长(T&E)方案的抗VEGF给药与固定剂量和按需(PRN)方案的给药对新生血管性年龄相关黄斑变性的疗效和治疗负担。我们搜索了MEDLINE, CENTRAL和 EMBASE数据库, 纳入了比较T&E与PRN或固定剂量给药初治AMD患者的随机对照试验和观察性研究。这些研究中均包含了视力(VA)的平均差异(MD)和注射次数的信息。我们根据Cochrane指南评估偏倚风险, 参照系统综述和荟萃分析的首选报告条目(PRISMA)进行了方法学分析。T&E和固定剂量给药对于视力改善的程度在1年(MD −0.08 个字母, p = 0.95)和2年 (MD 0.58 个字母, p = 0.62)内是相似的。然而, 与PRN方案相比, T&E方案在1年(MD 3.95个字母, p < 0.0001)和2年(MD 4.08个字母, p < 0.001)里对视力有显著改善。与固定剂量给药相比, T&E给药在1年(MD–2.42次注射, p < 0.0001)和2年(MD–6.06次注射, p < 0.00001)里的雷珠单抗注射次数显著减少。同时, 相较于固定剂量给药, 在1年里采用T&E给药的患者接受阿柏西普注射的次数更少(MD −0.78次注射, p < 0.0001)。目前低等级的证据显示, T&E对视力的改善与固定剂量给药相似, 但在1年和2年里的注射药物次数却显著减少。此外, T&E给药对患者的视力改善优于PRN方案, 但T&E方案的药物注射次数却较多。
Similar content being viewed by others
Introduction
The development of anti-vascular endothelial growth factor (anti-VEGF) agents represented a dramatic breakthrough in the treatment of neovascular age-related macular degeneration (nAMD). Fixed monthly treatment was the first approved dosing regimen for anti-VEGF treatment based on the results of numerous pivotal phase III clinical trials [1,2,3]. Repeated monthly injections, however, can place a substantial financial, emotional, and psychological burden on the patient, family and doctor [4].
To address this challenge, subsequent investigations have focused on the development of individualized regimens to minimize injection frequency while still achieving favorable visual outcomes. The pro re nata (PRN) approach, for instance, involves treatment with three monthly loading phase injections, followed by maintenance therapy triggered by functional and/or anatomical signs of disease activity [5]. The real-life outcome and longer-term performance of PRN dosing, however, has been disappointing. Multiple phase III trials have demonstrated good visual outcomes with PRN dosing when patients are monitored monthly but consistently showed loss of visual acuity (VA) gains in patients receiving PRN medication for prolonged periods in excess of 12 months, when monitoring was less frequent [6,7,8].
The treat-and-extend (T&E) paradigm was developed to address the shortcomings associated with fixed and PRN regimens, whereby patients receive fixed monthly injections until clinical remission, followed by a stepwise increase or decrease in treatment intervals based on the presence or absence of continued remission [4, 9,10,11]. Unlike other treatment protocols, T&E eliminates the need for monthly assessment. Moreover, T&E regimens attempt to treat patients just prior to the development of disease activity or fluid accumulation by determining the patient-specific interval of recurrence, in contrast to the PRN regimen, wherein treatment is applied only in response to clinical worsening [4, 5].
In recent years, T&E has undergone widespread adoption, with a survey of retinal surgeons in the United States indicating that this dosing regimen was their preferred strategy for treatment of nAMD [12]. Limited evidence, however, exists to support the long-term use of T&E over other anti-VEGF treatment regimens. To date, the findings of pairwise meta-analyses comparing T&E to fixed dosing have largely been powered by two large RCTs with opposing trends with regard to visual acuity improvement [10, 11, 13,14,15,16]. Moreover, various network meta-analyses comparing T&E and PRN regimens have led to conflicting conclusions, and none to date have investigated long-term outcomes beyond one year [17, 18]. There likewise remains a dearth of syntheses investigating the relative efficacy of T&E to PRN therapy. While a recent Cochrane review published by Li et al. provides a broad overview of randomized trial data on various injection regimens, the authors pooled PRN and T&E arms together in an effort to compare “flexible” regimens to “fixed” dosing schedules, and did not account for the proliferation of observational studies comparing T&E to alternative treatment regimens through 12 months and beyond [19]. Moreover, the recent release of comprehensive data from two large multicentre clinical trials further necessitate a holistic reappraisal of the literature in support of T&E therapy [20, 21]. For these reasons, we performed a systematic review and meta-analysis of RCTs and observational studies to compare the efficacy and safety of T&E anti-VEGF therapy against PRN and fixed dosing for treatment of nAMD at 1 and 2 years.
Methods
The authors conducted this systematic review and meta-analysis in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (http://www.prisma-statement.org; accessed December 29th, 2020) (Supplementary Fig. S1). The authors prospectively registered the study protocol PROSPERO (CRD42020205249) and received no funding for the present synthesis.
Literature search
On July 15th, 2020, the authors conducted a systematic search to capture references on MEDLINE, EMBASE, and CENTRAL published from 2004 onward. This date was chosen as it reflects the year in which anti-VEGF agents were first approved for the treatment of nAMD [22]. The sensitive search strategy was devised in collaboration with an academic research librarian and involved MeSH headings and text terms to identify studies assessing for the efficacy of anti-VEGF dosing strategies for treatment of AMD, as illustrated in Supplementary Table S1. To aid in analysis, we applied a filter to restrict the systematic search to studies performed on human subjects. Citations from previous systematic reviews were likewise referenced to ensure the identification of all eligible studies. Captured citations were deduplicated using Mendeley software and subsequently exported to Covidence for further screening.
Selection process
Two independent reviewers (DD, or FD, or JG, or AS) performed a comprehensive title and abstract screen, selecting for comparative studies involving treat-and-extend anti-VEGF therapy for treatment of AMD. The full text was consulted for all potentially eligible citations identified through the title and abstract screen, to select for studies which directly compared treat-and-extend anti-VEGF monotherapy to either PRN or fixed regimens. To control for the differential effect of various anti-VEGF agents, only comparisons using the same drug were included. As prior AMD treatment may modulate response to further therapy, only studies enrolling treatment-naïve patients were considered. Comparisons involving “off-label” use of anti-VEGF agents (e.g., bimonthly ranibizumab, bevacizumab) were excluded from further assessment to provide a comparison between T&E schedules and anti-VEGF dosing regimens approved for use on nAMD patients. Thus, our synthesis focused on comparisons involving 0.5 mg ranibizumab administered on a T&E, PRN, or fixed monthly regimen, and 2 mg aflibercept administered on a T&E, PRN, or fixed bimonthly dosing regimen. To assess for long-term safety and efficacy of anti-VEGF treatment in accordance with the previous meta-analysis published by Okada et al, eligible studies had to follow patients for a minimum period of 48 weeks, with reporting of baseline and change in visual acuity as an outcome measure [13]. To aid in study interpretation and risk of bias assessment, only reports published in English were included in the present review. Brief correspondences and conference abstracts were considered alongside outcomes reported in full-length, peer-reviewed publications. Information from the study protocol was likewise consulted, when available, from trial registries including ClinicalTrials.gov.
Outcomes and extraction
Two independent reviewers (DD, JG, or AS) transferred all relevant data from each study to a predefined, pilot-tested extraction sheet, designed in Microsoft Excel. A third arbitrator (DR) resolved discordance between authors. Pertinent details included study methodology, country of origin, subject eligibility criteria, sample size, intervention time, and length of clinical follow-up. Funding sources were likewise recorded.
The primary outcome of the present synthesis was change in best-corrected visual acuity at 12 months. Additional outcomes included change in BCVA at 24 months, change in retinal thickness at 12 and 24 months, number of intravitreal injections received at 12 and 24 months, frequency of serious ocular adverse events at 12 and 24 months, as well as the results of any patient-reported outcome. For quantitative synthesis, serious adverse events were included when referred to specifically as “serious ocular adverse events” by the study author. In the absence of specific phraseology, we considered the presence of endophthalmitis, vitreous opacity or hemorrhage, vision-threatening recurrence, retinal/epithelial tear, significant rise in intraocular pressure (IOP), and uveitis as serious ocular adverse events of interest. The proportion of patients achieving at least a 15 ETDRS letter improvement at 12- and 24-months follow-up was also collected.
Missing data
In the event of missing or unclear reporting of data, we contacted the corresponding author to obtain clarification. In the absence of important summary data, we performed our analysis based on the data as reported. It was assumed that all patient data were completely missing at random. Precision estimates were imputed according to Cochrane Collaboration recommendations when necessary [23].
Risk of bias
Two assessors (DR, DD) performed risk of bias assessment in accordance with the revised Cochrane Risk of Bias tool and The Risk of Bias in Non-Randomized Studies – of Interventions (ROBINS-I) framework for outcomes derived from RCTs and observational studies, respectively. The effect of assignment to interventions at baseline were assessed for all outcomes.
Synthesis and analysis
Risk ratios and 95% confidence intervals (CI) described summary measures for dichotomous variables, which included frequency of adverse events, and gain of 15 or more ETDRS letters. Mean differences and 95% CI described summary measures for continuous variables, which included mean BCVA improvement, treatment frequency, and change in retinal thickness. Pooled mean estimates were calculating by random-effects meta-analysis for all outcomes. All analyses were performed using RevMan 5.3 software.
Statistical heterogeneity was assessed to determine suitability of each meta-analysis. Chi-square analyses resulting in a p-value below 0.10 were considered an indicator of statistically significant heterogeneity. The I2 statistic was used to interpret the magnitude of heterogeneity. In accordance with Cochrane Collaboration guidelines, I2 values of 75–100% represented considerable heterogeneity. In the presence of considerable unexplained heterogeneity, we deferred meta-analysis in favor of narrative synthesis. One-study-removed sensitivity analyses were performed for all outcomes, wherein effect size is recalculated after removal of one study at a time, for every study included in a given synthesis.
Results
Selection of studies
We identified 9540 references in our systematic search. Following removal of duplicates, 6401 unique references were assessed. 85 records were identified as having involved a T&E protocol for treatment of AMD during the title and abstract screen, but only 33 reports met full eligibility criteria for inclusion (Supplementary Fig. S2). We removed 27 reports as they did not directly compare a clearly defined fixed or PRN regimen to a treat-and-extend regimen that involved an initial loading phase and subsequent maintenance phase. An additional 8 reports were excluded due to prior treatment of AMD in enrolled patients, four studies were excluded due to insufficient follow-up or change in group assignment prior to 48 weeks, and 3 used “off label” anti-VEGF treatment or compared the efficacy of T&E with one drug to fixed or PRN dosing with a different anti-VEGF agent. Finally, an additional 10 references were removed as they presented no outcomes relevant for extraction in the present synthesis.
The 33 relevant reports included 11 conference abstracts, 19 full-length publications, and 3 clinical trial registrations corresponding to 6 unique RCTs and 5 retrospective comparative studies. An additional 3 registrations were manually retrieved from ClinicalTrials.gov, the EU Clinical Trials Register, and the UMIN Clinical Trials Registry. Of these, 10 conference abstracts and one full-length publication listed interim study data or sub-analyses that were redundant to the primary publication. In total, 15 full-length manuscripts, one conference abstract, and six trial registries were consulted for extraction.
Characteristics of included studies
Of the six included trials, three compared 0.5 mg ranibizumab administered on T&E and monthly dosing regimens (Table 1). The TREX-AMD trial was conducted at two American centers, wherein 60 patients were randomized 1:2 to monthly or T&E therapy, and subsequently followed for 2 years. Patients assigned to monthly treatment, as well as patients achieving a 12-week T&E extension interval, were subsequently transitioned to a PRN regimen and followed for one additional year. Similarly, the CANTREAT study involved 1:1 randomization of 526 patients to 0.5 mg ranibizumab on monthly or T&E schedules, with follow-up extending to 24 months. The TREND trial likewise involved recruitment of 650 patients randomly assigned to two monthly or T&E dosing of 0.5 mg ranibizumab, with 12 months of follow-up.
Two trials involved administration of 2 mg aflibercept. ARIES was a multicentre trial comparing a traditional T&E protocol against a “late-start T&E” arm wherein a 3-month loading phase was followed by bimonthly aflibercept up to week 48, followed by T&E aflibercept through to study completion at 24 months. The present synthesis involved extraction of 1-year ARIES data available on clinical trial registries, as this represents a direct comparison between T&E and bimonthly aflibercept. By year 2, both arms in the ARIES trial followed a T&E regimen. As such, 2-year data for ARIES was not considered.
A recent study by Haga et al. likewise randomized 41 patients to bimonthly and T&E aflibercept in a Japanese population. Crucially, their patient population comprised a variety of diagnoses, including polypoidal choroidal vasculopathy and retinal angiomatous proliferation in addition to more typical presentations of AMD. We elected to retain this study for quantitative assessment as it did not significantly increase heterogeneity or adversely influence size, direction, or significance of measured effect for any outcome in sensitivity analysis.
Finally, one trial randomly assigned 104, 99, and 102 eyes to receive T&E, PRN, and bimonthly ranibizumab respectively. We did not extract data for bimonthly ranibizumab as this regimen represents a significant deviation from standard practice.
The five observational studies included in the present synthesis investigated T&E versus PRN ranibizumab, with a combined total of 426 and 644 eyes reporting visual acuity outcomes with at least 12 months of follow-up, respectively. The observational study by Augsburger et al. also included a T&E aflibercept arm, but this data was not extracted due to absence of a PRN or fixed aflibercept comparator.
Visual acuity
T&E vs fixed
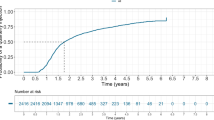
TREND, TREX-AMD, and CANTREAT each reported visual acuity outcomes following 12 months of T&E and monthly ranibizumab. The ARIES trial, as well as the recently published RCT by Haga et al, likewise compared T&E versus fixed bimonthly dosing of aflibercept at one year (Fig. 1, Analysis 1.1). Taking together all comparisons of T&E versus fixed anti-VEGF regimens, the present analysis did not identify any significant difference between arms with regard to visual acuity improvement at 12 months (5 studies, 743 eyes T&E, 725 eyes fixed; MD −0.08 letters, 95% CI −2.52–2.36, p = 0.95, I2 = 69%). Notably, sensitivity analysis with removal of the CANTREAT trial revealed a significant effect of 1.64 letters in favor of fixed dosing (Supplementary Fig. S3, Analysis 1.1).
Forest plots are presented for all meta-analyses, including visual, anatomical, treatment burden, and adverse events compared between T&E and alternative dosing regimens. Funnel plots or other tests of publication bias were deferred due to the low number of included studies. T&E treat-and-extend, VEGF vascular endothelial growth-factor agent, PRN pro-re-nata.
Subgroup analyses stratified by anti-VEGF agent yielded similar results, as demonstrated in Figure Analyses 1.1.1 and 1.1.2. Among trials comparing T&E to fixed aflibercept (Haga et al, ARIES), visual acuity gain at one year did not differ significantly between arms (2 studies, 127 eyes T&E, 124 eyes fixed; MD −1.39 letters, 95% CI −5.52–2.73, p = 0.51, I2 = 26%). While similar trends were observed among studies comparing T&E to fixed ranibizumab (CANTREAT, TREND, TREX-AMD), significant heterogeneity precludes the presentation of quantitative synthesis.
The TREX-AMD and CANTREAT trials likewise reported BCVA results out to 24 months, as outlined in Fig. 1, Analysis 1.2. No significant differences were observed (2 studies, 260 eyes T&E, 249 eyes fixed; MD 0.58 letters, 95% CI −1.74–2.90, p = 0.62, I2 = 0%).
Differences in retreatment criteria and length of the loading phase may have contributed, in part, to the heterogeneity and fragility of this outcome. For instance, CANTREAT and TREX-AMD involved administration of 3 loading doses prior to the extension phase, whereas investigators in the TREND study only injected patients twice prior to initiation of their T&E protocol. Accordingly, both TREX-AMD and CANTREAT revealed a non-significant difference in BCVA change favouring treat-and-extend, whereas the TREND study demonstrated the reverse – after 12 months, the T&E arm gained 6.2 (SD 12.5) letters, whereas the monthly arm gained 8.1 (SD 12.6) letters.
The proportion of patients gaining 15 or more ETDRS letters was also similar between groups (Fig. 1, Analyses 1.3 and 1.4) without any significant difference between T&E and fixed anti-VEGF treatment at one (5 studies, 726 eyes T&E, 706 eyes fixed; OR 1.06, 95% CI 0.76–1.48, p = 0.74, I2 = 32%) and two years (2 studies, 277 eyes T&E, 249 eyes fixed; OR 1.18, 95% CI 0.79–1.76, p = 0.79, I2 = 0%). Specifically, 183 of 726 (25.2%) T&E eyes and 170 of 706 (24.1%) fixed monthly eyes included in the present analysis achieved a BCVA gain of at least 15 letters at one year. By year two, 72 of 277 (26.0%) and 57 of 249 (22.9%) T&E and fixed monthly eyes had gained at least 15 letters, respectively. In contrast to assessment of VA improvement as a continuous variable, these findings were robust to sensitivity analysis (Supplementary Fig. S3, Analyses 1.3 and 1.4).
T&E vs PRN
In contrast to comparisons with fixed dosing, meta-analysis revealed a significant effect in favor of T&E with regard to BCVA improvement at 12 months, as demonstrated in Fig. 1, Analysis 2.1 (6 studies, 525 eyes T&E, 748 eyes PRN; MD 3.95 letters, 95% CI 2.13–5.77, p < 0.0001, I2 = 40%). This finding was consistent across numerous studies, with the exception of an RCT conducted by Lopez-Galves et al. and an observational study by Garweg et al. in which no significant difference between treatment arms was identified. One-study-removed sensitivity analysis yielded no meaningful changes with regard to effect size, direction, or significance of the present synthesis (Supplementary Fig. S3, Analysis 2).
Two observational studies reported BCVA results at 24 months (Fig. 1, Analysis 2.2). The BCVA gains observed at year 1 were preserved at year 2, with a modest effect in favor of T&E ranibizumab over PRN dosing (2 studies, 85 eyes T&E, 187 eyes PRN; MD 4.08 letters, 95% CI 1.67–6.49, p < 0.001, I2 = 0%).
The RCT conducted Lopez-Galves et al. was the only study to report the proportion of patients achieving an additional 15 or more ETDRS letters at month 12 and demonstrated such gains in 23.9% and 31.6% of T&E and PRN patients, respectively. However, no significant difference between arms was identified (p = 0.473).
Retinal thickness
T&E vs monthly
Change in retinal thickness after fixed and T&E ranibizumab was reported in TREND and TREX-AMD, whereas retinal thickness with aflibercept was reported in ARIES and in the study conducted by Haga et al. (Fig. 1, Analysis 3.1). Meta-analysis revealed no significant difference between arms with respect to retinal thickness change at 12 months (4 studies, 446 eyes T&E, 430 eyes PRN: MD 5.10 um, 95% CI −1.79–24.00, p = 0.60, I2 = 0%). TREX-AMD was the only study to provide 2-year results, which likewise suggested no or trivial difference between T&E and fixed ranibizumab with respect to anatomical outcomes (p = 0.99). All findings were robust to sensitivity analysis (Supplementary Fig. S3, Analysis 3).
T&E vs PRN
Two observational studies and one RCT reported change in retinal thickness after 12 months of PRN versus T&E ranibizumab therapy. Garweg et al. and Lopez-Galves et al. both observed significant declines in retinal thickness among T&E and PRN patients during the loading phase, which were subsequently maintained through to month 12. Hatz et al. likewise observed a rapid decrease in retinal thickness following 3 months of ranibizumab therapy. The results reported by Hatz et al., however, were not maintained in the PRN arm, such that by month 12, a statistically significant mean difference of 58 um was observed in favor of T&E. Meta-analysis failed to identify a significant difference between treatment regimens (3 studies, 180 eyes T&E, 211 eyes PRN; MD −12.03 um, 95% CI −62.69–38.62, p = 0.64, I2 = 70%), albeit with considerable heterogeneity (Fig. 1, Analysis 4.1). Only Garweg et al. provided 2-year data for retinal thickness, demonstrating no significant difference between arms (p = 0.73). These findings were unchanged with one-study-removed sensitivity analysis (Supplementary Fig. S3, Analysis 4).
Number of injections
T&E vs monthly
A total of 3 RCTs comparing T&E and monthly ranibizumab, and 2 RCTs comparing T&E and bimonthly aflibercept, provided relevant data. Notably, reports on CANTREAT and TREX-AMD failed to present relevant precision estimates. We thus imputed precision estimates from the TREND trial and applied them to the findings from CANTREAT and TREX-AMD to enable quantitative synthesis in accordance with Cochrane recommendations.
As expected, significant heterogeneity was observed upon synthesis of studies comparing monthly to T&E ranibizumab, and trials assessing bimonthly to T&E aflibercept (I2 = 96%). Stratification of results by use of aflibercept (2 studies, 127 eyes T&E, 124 eyes PRN; MD –0.78 injections, 95% CI −1.14 to −0.42, p < 0.0001, I2 = 53%) or ranibizumab (3 studies, 628 eyes T&E, 604 eyes PRN; MD –2.42 injections, 95% CI −2.71 to −2.14, p < 0.0001, I2 = 0%) resolved this heterogeneity, and thereby demonstrated a significant reduction in number of injections following a T&E regimen versus fixed dosing regardless of anti-VEGF agent used (Fig. 1, Analysis 5.1).
Only CANTREAT and TREX-AMD presented the number of injections received at 24 months. As was done for our 12-month synthesis, we imputed SDs from another study presenting 2-year injection outcomes to permit quantitative synthesis (Fig. 1, Analysis 5.2). At two years, meta-analysis demonstrated a mean difference of (2 studies, 267 eyes T&E, 249 eyes PRN; MD –6.06 injections, 95% CI −6.79 to −5.34, p < 0.00001, I2 = 17%) injections in favor of T&E. All findings in the present synthesis were robust to sensitivity analysis (Supplementary Fig. S3, Analysis 5).
T&E vs PRN
One RCT and four observational studies reported the outcome of interest. All included studies consistently demonstrated a significantly greater number of injections with T&E relative to PRN, as outlined in Table 2. Significant heterogeneity was observed for this outcome, precluding meta-analysis. Only one study compared number of injections at two years, demonstrating significantly fewer injections for patients receiving therapy on a PRN basis versus T&E, in keeping with data presented at twelve months. (p = 0.002).
Serious ocular adverse events
T&E vs monthly
In the TREND trial, 1.2% of patients in both monthly and T&E arms developed a serious ocular adverse event through to month 12. Notably, one case of endophthalmitis was observed in the monthly treatment group, whereas retinal detachment developed in a single patient randomized to T&E dosing.
In the TREX-AMD trial, two patients experienced serious ocular adverse events in the T&E arm, including progression of macular atrophy and pigment epithelial tear. In contrast, no adverse events were observed in the fixed ranibizumab arm at 12 months. After 24-months of the TREX-AMD trial, a total 5 serious ocular events (13%) had developed among T&E eyes, with none recorded for the monthly cohort. At 36 months, those figures rose to 2 (10%) and 6 (15%) for monthly and T&E arms respectively.
The CANTREAT trial presented the frequency of study withdrawal secondary to any adverse event, not stratified by severity or relevance to the eye. Overall, 7 (1.7%) monthly and 2 (0.7%) T&E patients withdrew due to an adverse event at 12 months. At 24 months, 8 (2.7%) and 4 (1.4%) patients had withdrawn from monthly and T&E treatment arms respectively. A sub-study assessing for significant IOP elevation likewise found that a similarly low proportion of patients experienced an IOP rise greater or equal to 15 mmHg in the T&E (1%) and monthly cohorts (1.1%).
The ARIES trial found the proportion of patients developing serious ocular adverse events at 1 year to be 0% among those in the T&E, and 2.2% among those on a fixed 2q8 aflibercept regimen. Unfortunately, no safety data was reported for the RCT conducted by Haga et al.
Quantitative synthesis of studies reporting serious ocular adverse events suggests no or trivial difference between fixed and T&E paradigms with respect to development of adverse events at one year (3 studies, 498 eyes T&E, 482 eyes PRN; OR 0.85, 95% CI 0.26 to 2.80, p = 0.79, I2 = 1%), as outlined in Fig. 1, Analysis 6.1. No changes in effect were observed through sensitivity analysis (Supplementary Fig. S3, Analysis 6).
T&E vs PRN
One RCT and two observational studies reported on the relative frequency of serious ocular adverse events experienced by patients assigned to T&E and PRN regimens. In the retrospective assessment conducted by Hatz et al, vision-threatening recurrence or hemorrhage was observed in 23 of 70 patients (32.9%) assigned to PRN treatment, with no ocular events noted in the T&E cohort. Oubraham et al. likewise reported the development of severe hemorrhage in two patients assigned to PRN treatment, with no serious ocular events recorded among those assigned to T&E ranibizumab. While Lopez-Galves et al. presented data on adverse events after one year of anti-VEGF therapy, the relative frequency of serious ocular adverse events was not formally defined or presented. As such, we tallied the frequency with which the study authors recorded the development of endophthalmitis, retinal hemorrhage, retinal tear, pigment epithelial tear, uveitis, vitreous hemorrhage, and increased IOP among patients assigned to T&E and PRN paradigms. In total, 8 of the aforementioned serious ocular adverse events were recorded among 98 patients randomized to the T&E arm, and 9 were recorded from 104 patients receiving PRN treatment – it remains unclear, however, whether a smaller number of patients experienced multiple concurrent adverse events, or if each event developed in a unique patient. Given the considerable differences in reporting of adverse events and significant heterogeneity in results among the included studies, meta-analysis was deferred.
Quality of Life: The TREND trial assessed patient quality of life with the VFQ-25 questionnaire and found a mean increase of 2.3 points (SD 13.93) and 4 points (SD 13.72) on a 100-point scale after 12 months of T&E and fixed monthly ranibizumab, respectively. Lopez-Galvez assessed for change in quality of life from baseline through the “VFL-25” survey and found modest improvements from 76.1 (SD16.2) to 77.5 (SD 17.9) after 12 months of T&E ranibizumab, and from 73.9 (SD 18.4) to 76.6 (SD 18.9) for those on a PRN regimen, measured on a similar 100-point scale. These findings were not statistically significant. Meta-analysis was deferred as no two studies used the same patient-reported outcome.
Risk of bias
RCTs
Details with regard to risk of bias assessment are illustrated in Supplementary Fig. S4. At least one domain was found to be at a “high” risk of bias for all included trials, primarily related to the nature of administering anti-VEGF injections regimens which precludes masking of participants and personnel. Risk of bias related to random sequence generation was likewise rated as unclear for three trials. Insufficient information with regard to allocation concealment was noted for two RCTs, and all trials failed to adequately disclose methodology for masking of outcome assessment. Significant attrition bias was noted among three trials, and one study was rated at high risk of bias for failure to report adverse events, despite its role as a core outcome measure in clinical trials.
Observational studies
In addition to the biases inherent with included observational studies, such as their retrospective nature and relatively small sample sizes, a number of additional sources of significant bias were identified (Supplementary Fig. S4). Of five included observational studies, four assessed PRN and T&E patients from different time periods. Advancements in imaging technology and understanding of disease over time thus place these studies at significant risk of confounding bias. Various included studies were likewise at moderate to severe risk of selection bias, attrition bias, and deviation from the intended protocol, as large variations in follow-up visits in the PRN arm indicated that numerous assessment visits were missed.
Discussion
The present synthesis assesses the efficacy, safety, and treatment burden of T&E aflibercept and ranibizumab compared against alternative dosing regimens. While previous meta-analyses have sought to address this topic, none to date have included data from the ARIES trial, and none since the initial pairwise meta-analysis by Okada et al. have sought to include the results from both RCTs and real-world observational studies [10, 11, 13,14,15,16,17,18]. Four new RCTs, and three additional observational studies have since been published, representing a meaningful expansion of literature involving direct head-to-head anti-VEGF dosing strategy comparisons [21, 24,25,26,27,28,29].
Taken together, the current findings affirm the noninferiority of T&E compared to fixed anti-VEGF treatment based on the largest pairwise sample of nAMD patients to date. The pooled difference in BCVA ranged from 0.08 to 0.58 letters at one and two years respectively, reflecting a clinically insignificant difference between arms which remained consistent irrespective of anti-VEGF agent used. Notably, T&E treatment was able to achieve efficacy comparable to fixed dosing while exerting significantly lower treatment burden – pooled analysis revealed that T&E dosing led to a reduction of 0.78 and 2.42 injections over a one-year period when compared against fixed aflibercept and ranibizumab respectively. At two years, 6.06 fewer injections of ranibizumab were required in the T&E arm to achieve efficacy comparable to monthly treatment. These results align closely with an Australian database study, wherein patients treated on a T&E regimen were matched to patients enrolled in the Phase III Minimally Classic/Occult Trial of the Anti-VEGF Antibody Ranibizumab study [30]. In that analysis, fewer injections were administered in patients receiving T&E treatment while visual acuity gains comparable to those assigned to fixed ranibizumab were maintained. Our synthesis also expands on the work of Fallico et al., who recently completed a meta-analysis of four trials, and likewise concluded that T&E regimens can successfully preserve vision in nAMD patients while exerting significantly lower treatment burden than fixed dosing schedules [14]. With the inclusion of recently published ARIES results, our study presents, for the first time, a pairwise synthesis of multiple trials comparing T&E to fixed bimonthly aflibercept [21]. In doing so, we add to the growing consensus in support of T&E anti-VEGF regimens for the treatment of nAMD.
Patients with T&E dosing achieved better visual acuity outcomes relative to PRN regimen. At one year, patients receiving T&E gained an additional 3.95 letters over their PRN counterparts. This difference grew to 4.08 letters at two years, suggesting a persistent visual acuity advantage in favor of T&E. While our findings corroborate those of previous meta-analyses published by Okada et al, and more recently by Ye et al., they contradict a recent network meta-analysis of RCTs published by Garmo et al., which found no meaningful difference in visual outcomes for patients receiving ranibizumab PRN relative to any other anti-VEGF injection regimen [13, 17, 18].
Notably, the efficacy of PRN as observed in numerous RCTs has failed to translate to real-world assessments. For instance, in the PrONTO trial, study investigators recorded 99.1% patient attendance at their scheduled monthly visits, and likewise noted impressive visual acuity gains of 9.3 letters after one year, and 11.1 letters after 2 years [5]. In contrast, BCVA improvement among the observational studies included in the present synthesis ranged from 0.7 to 5.0 letters at one year, and from −3.7 to 4.5 letters after two years of PRN treatment. Oubraham et al. likewise found that patients in the PRN arm were only examined 8.8 times per year instead of 12 times as would be expected on a PRN regimen, again highlighting the lack of monthly assessments [26]. Differences in patient compliance between RCTs and real-world assessments might explain, in part, the discordance between our findings and those of Garmo et al., whose meta-analysis was powered exclusively by data extracted from landmark RCTs. CATT and other trials have needed monthly assessments for PRN arm which is not feasible in real life. Further, it has previously been reasoned that clinic attendance for retinal monitoring, rather than for a guaranteed injection, may be less rewarding for patients [13].
A number of studies suggest a physiological basis for the superiority of T&E and monthly regimens relative to PRN. Post-hoc analyses of the CATT, HARBOR, and IVAN trials demonstrate a trend toward poorer visual outcomes in eyes subject to greater fluctuations in retinal thickness following anti-VEGF therapy [31, 32]. As PRN regimens only involve retreatment upon the presence of disease activity, it is possible that such reactive regimens may predisposing patients to greater fluctuations in retinal thickness relative to alternative, proactive dosing schedules such as T&E.
Recent investigations have also sought to further refine the T&E paradigm by comparing 2- versus 4-week extension intervals, and retreatment criteria that permit residual subretinal fluid in the absence of intraretinal fluid or other signs of disease activity [33, 34]. Such innovations might serve to further reduce the treatment burden of the T&E paradigm relative to alternative regimens.
Despite a growing number of head-to-head comparisons, the low number of studies collecting long-term safety and efficacy outcomes beyond one year remain a crucial weakness of the field. In the present review, only two eligible RCTs and two observational studies compared visual acuity results at 24 months. Further limitations include heterogeneity among the included studies precluding the synthesis of numerous outcomes. In particular, we observed marked variability in the reporting quality of adverse events across numerous RCTs and observational studies, necessitating a standardized method for the communication of safety outcomes in trials assessing anti-VEGF agents. Finally, our search strategy was limited only to publications in English to enable accurate data extraction and comprehensive risk of bias assessment. It is therefore possible that a small number of non-English studies were missed in the present review.
Conclusion
The present review suggests that at 12 and 24 months, T&E therapy preserves visual acuity similar to fixed schedules while exerting significantly lower treatment burden, regardless of anti-VEGF agent used. Additionally, T&E was found to deliver superior visual acuity outcomes relative to PRN at one or two years.
Summary
What is known about this topic
-
Various treatment paradigms for management of neovascular age-related macular degeneration (nAMD) with anti-VEGF agents are routinely used in clinical practice including PRN treatment, fixed dosing and treat-and-extend.
-
Individual clinical trials have provided increasingly robust evidence for the efficacy, safety and treatment burden for a pro-active T&E paradigm for nAMD management with anti-VEGF agents.
What this study adds
-
This study provides the largest evidence synthesis to date in terms of efficacy and treatment burden of T&E versus fixed dosing and PRN paradigm in management of nAMD.
-
The effect size estimates demonstrate that T&E is non-inferior to gold standard fixed dosing regimens while reducing treatment burden at month 12 and 24.
-
In addition, T&E resulted in statistically superior visual outcomes relative to PRN paradigm at month 12 and 24.
References
Rosenfeld PJ, Brown DM, Heier JS, Boyer DS, Kaiser PK, Chung CY, et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med. 2006;355:1419–31.
Brown DM, Kaiser PK, Michels M, Soubrane G, Heier JS, Kim RY, et al. Ranibizumab versus verteporfin for neovascular age-related macular degeneration. N. Engl J Med. 2006;355:1432–44.
Heier JS, Brown DM, Chong V, Korobelnik JF, Kaiser PK, Nguyen QD, et al. Intravitreal aflibercept (VEGF trap-eye) in wet age-related macular degeneration. Ophthalmology. 2012;119:2537–48.
Spaide R. Ranibizumab according to need: a treatment for age-related macular degeneration. Am J Ophthalmol. 2007;143:679–80.
Lalwani GA, Rosenfeld PJ, Fung AE, Dubovy SR, Michels S, Feuer W, et al. A variable-dosing regimen with intravitreal ranibizumab for neovascular age-related macular degeneration: year 2 of the PrONTO Study. Am J Ophthalmol. 2009;148:43–58.
Writing Committee for the UK Age-Related Macular Degeneration EMR Users Group. The neovascular age-related macular degeneration database: multicenter study of 92 976 ranibizumab injections: report 1: visual acuity. Ophthalmology. 2014;121:1092–101.
Ho AC, Busbee BG, Regillo CD, Wieland MR, Van Everen SA, Li Z, et al. Twenty-four-month efficacy and safety of 0.5 mg or 2.0 mg ranibizumab in patients with subfoveal neovascular age-related macular degeneration. Ophthalmology. 2014;121:2181–92.
Chakravarthy U, Harding SP, Rogers CA, Downes SM, Lotery AJ, Culliford LA, et al. Alternative treatments to inhibit VEGF in age-related choroidal neovascularisation: 2-year findings of the IVAN randomised controlled trial. Lancet. 2013;382:1258–67.
Engelbert M, Zweifel SA, Freund KB. ‘Treat and extend’’ dosing of intravitreal antivascular endothelial growth factor therapy for type 3 neovascularization/retinal angiomatous proliferation. Retina. 2009;29:1424–31.
Chin-Yee D, Eck T, Fowler S, Hardi A, Apte RS. A systematic review of as needed versus treat and extend ranibizumab or bevacizumab treatment regimens for neovascular age-related macular degeneration. Br J Ophthalmol. 2016;100:914–917.
Rufai SR, Almuhtaseb H, Paul RM, Stuart BL, Kendrick T, Lee H, et al. A systematic review to assess the ‘treat-and-extend’ dosing regimen for neovascular age-related macular degeneration using ranibizumab. Eye. 2017;31:1337–44.
American Society of Retina Specialists. Annual preferences and trends survey, 2014. http://www.asrs.org.
Okada M, Kandasamy R, Chong EW, McGuiness M, Guymer RH. The treat-and-extend injection regimen versus alternate dosing strategies in age-related macular degeneration: a systematic review and meta-analysis. Am J Ophthalmol. 2018;192:184–97.
Fallico M, Lotery AJ, Longo A, Avitabile T, Bonfiglio V, Russo A, et al. Treat and extend versus fixed regimen in neovascular age related macular degeneration: a systematic review and meta-analysis. Eur J Ophthalmol. 2020. https://doi.org/10.1177/1120672120964699.
Silva R, Berta A, Larsen M, Macfadden W, Feller C, Monés J, TREND Study Group. Treat-and-extend versus monthly regimen in neovascular age-related macular degeneration: results with ranibizumab from the TREND study. Ophthalmology. 2018;125:57–65.
Kertes PJ, Galic IJ, Greve M, Williams RG, Rampakakis E, Scarino A, et al. Canadian treat-and-extend analysis trial with ranibizumab in patients with neovascular age-related macular disease: one-year results of the randomized Canadian treat-and-extend analysis trial with ranibizumab study. Ophthalmology. 2019;126:841–848.
Ye L, Jiaqi Z, Jianchao W, Zhaohui F, Liang Y, Xiaohui Z. Comparative efficacy and safety of anti-vascular endothelial growth factor regimens for neovascular age-related macular degeneration: systematic review and Bayesian network meta-analysis. Ther Adv Chronic Dis. 2020. https://doi.org/10.1177/2040622320953349.
Garmo V, Stoilov I, Solon C, Ali FS, Uyei J, Bilir P, et al. Do Comparative efficacy of anti-vascular endothelial growth factor (anti-VEGF) treatment regimens for neovascular age-related macular degeneration (nAMD): a network meta-analysis [ARVO abstract]. Invest Ophthalmol Vis Sci. 2020;61:4228.
Li E, Donati S, Lindsley KB, Krzystolik MG, Virgili G Treatment regimens for administration of anti-vascular endothelial growth factor agents for neovascular age-related macular degeneration. Cochrane Database Syst Rev. 2020;5. https://doi.org/10.1002/14651858.CD012208.pub2.
López Gálvez MI, Barquet LA, Figueroa MS, García-Layana A, Ruiz Moreno JM, In-Eye Study Group. Bimonthly, treat-and-extend and as-needed ranibizumab in naïve neovascular age-related macular degeneration patients: 12-month outcomes of a randomized study. Acta Ophthalmol. 2020;98:820–829.
Mitchell P, Holz FG, Hykin P, Midena E, Souied E, Allmeier H, et al. Efficacy and safety of intravitreal aflibercept using a treat-and-extend regimen for neovascular age-related macular degeneration: the aries study: a randomized clinical trial. Retina. 2020;41:1911–1920.
Vinores SA. Pegatanib in the treatment of wet, age-related macular degeneration. Int J Nanomed. 2006;1:263–268.
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.1 (updated September 2020). Cochrane, 2020. www.training.cochrane.org/handbook.
Kertes PJ, Galic IJ, Greve M, Williams G, Baker J, Lahaie M, et al. Efficacy of a treat-and-extend regimen with ranibizumab in patients with neovascular age-related macular disease: a randomized clinical trial. JAMA Ophthalmol. 2020;138:244–250.
Haga A, Kawaji T, Ideta R, Inomata Y, Tanihara H. Treat-and-extend versus every-other-month regimens with aflibercept in age-related macular degeneration. Acta Ophthalmol. 2018;96:393–398. https://doi.org/10.1111/aos.13607.
López Gálvez MI, Barquet LA, Figueroa MS, García-Layana A, Ruiz Moreno JM, In-Eye Study Group. Bimonthly, treat-and-extend and as-needed ranibizumab in naïve neovascular age-related macular degeneration patients: 12-month outcomes of a randomized study. Acta Ophthalmol. 2020;98:820–829. https://doi.org/10.1111/aos.14399.
Garweg JG, Niderprim SA, Russ HM, Pfister IB. Comparison of strategies of treatment with ranibizumab in newly-diagnosed cases of neovascular age-related macular degeneration. J Ocul Pharm Ther. 2017;33:773–778. https://doi.org/10.1089/jop.2017.0006.
Aurell S, Sjövall K, Paul A, Morén Å, Granstam E. Better visual outcome at 1 year with antivascular endothelial growth factor treatment according to treat-and-extend compared with pro re nata in eyes with neovascular age-related macular degeneration. Acta Ophthalmol. 2019;97:519–524. https://doi.org/10.1111/aos.13989.
Augsburger M, Sarra GM, Imesch P Treat and extend versus pro re nata regimens of ranibizumab and aflibercept in neovascular age-related macular degeneration: a comparative study. Graefes Arch Clin Exp Ophthalmol. 2019;257:1889–95. https://doi.org/10.1007/s00417-019-04404-0.
Gillies MC, Walton RJ, Arnold JJ, McAllister IL, Simpson JM, Hunyor AP, et al. Comparison of outcomes from a phase 3 study of age-related macular degeneration with a matched, observational cohort. Ophthalmology. 2014;121:676–81. https://doi.org/10.1016/j.ophtha.2013.09.050.
Seth V, Blotner S, Malhotra M, D’Rozaio M, Shamik G. Fluctuations in central foveal thickness and vision outcomes with Anti-VEGF therapy for neovascular age-related macular degeneration [ARVO abstract]. Invest Ophthalmol Vis Sci. 2020;61:4224.
Evans RN, Reeves BC, Maguire MG, Martin DF, Muldrew A, Peto T, et al. Associations of variation in retinal thickness with visual acuity and anatomic outcomes in eyes with neovascular age-related macular degeneration lesions treated with anti–vascular endothelial growth factor agents. JAMA Ophthalmol. 2020;138:1043–1051.
Guymer RH, Markey CM, McAllister IL, Gillies MC, Hunyor AP, Arnold JJ, FLUID Investigators. Tolerating subretinal fluid in neovascular age-related macular degeneration treated with ranibizumab using a treat-and-extend regimen: FLUID study 24-month results. Ophthalmology. 2019;126:723–734.
Ohji M, Takahashi K, Okada AA, Kobayashi M, Matsuda Y, Terano Y, et al. Efficacy and safety of intravitreal degeneration: 52- and 96-week findings from ALTAIR. Adv Ther. 2020;37:1173–1187.
Wykoff CC, Croft DE, Brown DM, Wang R, Payne JF, Clark L, et al. Prospective trial of treat-and-extend versus monthly dosing for neovascular age-related macular degeneration: TREX-AMD 1-year results. Ophthalmology. 2015;122:2514–2522.
Wykoff CC, Ou WC, Brown DM, Croft DE, Wang R, Payne JF, TREX-AMD Study Group, et al. Randomized trial of treat-and-extend versus monthly dosing for neovascular age-related macular degeneration: 2-year results of the TREX-AMD study. Ophthalmol Retin. 2017;1:314–321.
Wykoff CC, Ou WC, Croft DE, Payne JF, Brown DM, Clark WL, et al. Neovascular age-related macular degeneration management in the third year: final results from the TREX-AMD randomised trial. Br J Ophthalmol. 2018;102:460–464.
Abdelfattah NS, Al-Sheikh M, Pitetta S, Mousa A, Sadda SR, Wykoff CC, Treat-and-Extend Age-Related Macular Degeneration Study Group. Macular atrophy in neovascular age-related macular degeneration with monthly versus treat-and-extend ranibizumab: findings from the TREX-AMD trial. Ophthalmology. 2017;124:215–223.
Oubraham H, Cohen SY, Samimi S, Marotte D, Bouzaher I, Bonicel P, et al. Inject and extend dosing versus dosing as needed: a comparative retrospective study of ranibizumab in exudative age-related macular degeneration. Retina. 2011;31:26–30.
Hatz K, Prunte C. Treat and Extend Versus Pro Re Nata regimens of ranibizumab in neovascular age-related macular degeneration: a comparative 12 month study. Acta Ophthalmol. 2017;95:67–72. https://doi.org/10.1111/aos.13031.
Author information
Authors and Affiliations
Contributions
VC, SJB, DS, CMGC, CCW and SS were responsible for conceptualization of the study. VC, DR, DMD, JG, AS, MRP and GSS were responsible for study implementation and analysis of the data. VC, SJB, CMGC, CCW, SS, DR, MRP were responsible for the interpretation of the data. All authors were responsible for critically appraising and revising the manuscript. All the authors provided major contributions to the writing and have critically appraised and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
SS reports receiving research grants from Novartis, Bayer, Allergan, Roche, Boehringer, Ingelheim and Optos Plc, Travel grants from Novartis, Bayer, speaker fees from Novartis, Bayer and Optos Plc, and attending advisory board meetings for Novartis, Bayer, Allergan, Roche, Boehringer, Ingelheim, Optos Plz, Oxurion, Ophthea, Apellis, Oculis and Heidelberg Engineering. CMGC reports grants and speaker fees from Roche, Novartis, Bayer, Allergan, and Topcon outside the submitted work. DS has acted as consultant for Amgen, Bayer, Genentech, Novartis, and Optovue, and reports grants from Amgen, Genentech, Heidelberg, Optovue, Regeneron and Topcon, outside the submitted work. SJB has acted as a consultant for Adverum, Alimera, Apellis, Allergan, Eyepoint, Kala, Genentech, Novartis, Oxurion, Roche, and Zeiss, outside the submitted work. CCW reported consulting for Acuela, Adverum Biotechnologies, Inc, Aerpio, Alimera Sciences, Allegro Ophthalmics, LLC, Allergan, Apellis Pharmaceuticals, Bayer AG, Chengdu Kanghong Pharmaceuticals Group Co, Ltd, Clearside Biomedical, DORC (Dutch Ophthalmic Research Center), EyePoint Pharmaceuticals, Gentech/Roche, GyroscopeTx, IVERIC bio, Kodiak Sciences Inc, Novartis AG, ONL Therapeutics, Oxurion NV, PolyPhotonix, Recens Medical, Regeron Pharmaceuticals, Inc, REGENXBIO Inc, Santen Pharmaceutical Co, Ltd, and Takeda Pharmaceutical Company Limited and receiving research funding from Adverum Biotechnologies, Inc, Aerie Pharmaceuticals, Inc, Aerpio, Alimera Sciences, Allergan, Apellis Pharmaceuticals, Chengdu Kanghong Pharmaceutical Group Co, Ltd, Clearside Biomedical, Gemini Therapeutics, Genentech/Roche, Graybug Vision, Inc, GyroscopeTx, Ionis Pharmaceuticals, IVERIC bio, Kodiak Sciences Inc, Neurotech LLC, Novartis AG, Opthea, Outlook Therapeutics, Inc, Recens Medical, Regeneron Pharmaceuticals, Inc, REGENXBIO Inc, Samsung Pharm Co, Ltd, Santen Pharmaceutical Co, Ltd, and Xbrane Biopharma AB. VC reports acting as an advisory board member, grants and other from Novartis, acting as an advisory board member, grants and other from Bayer, grants from Allergan, and acting as an advisory board member for Roche, outside the submitted work. The remaining authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rosenberg, D., Deonarain, D.M., Gould, J. et al. Efficacy, safety, and treatment burden of treat-and-extend versus alternative anti-VEGF regimens for nAMD: a systematic review and meta-analysis. Eye 37, 6–16 (2023). https://doi.org/10.1038/s41433-022-02020-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02020-7
This article is cited by
-
Home Optical Coherence Tomography Monitoring for Neovascular Age-Related Macular Degeneration: Transformative Technology or Cool Toy?
Ophthalmology and Therapy (2024)
-
Six-month outcomes of switching from aflibercept to faricimab in refractory cases of neovascular age-related macular degeneration
Graefe's Archive for Clinical and Experimental Ophthalmology (2024)
-
Treat & extend in neovascular age-related macular degeneration: how we got here and where do we go next?
Eye (2023)
-
Systematic Review of Neovascular Age-Related Macular Degeneration Disease Activity Criteria Use to Shorten, Maintain or Extend Treatment Intervals with Anti-VEGF in Clinical Trials: Implications for Clinical Practice
Ophthalmology and Therapy (2023)
-
Difference in characteristics and lesion reactivation between type 3 macular neovascularization with and without subretinal fluid at baseline
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)