Abstract
Purpose
Altered glucose metabolism, along with low-grade inflammation, has been proposed to be involved in retinal detachment (RD)-induced cone loss. Here, we assessed intravitreal glucose and cytological profile in patients with macula-off RD.
Methods
Glucose concentration was analysed in vitreous samples from 137 non-diabetic patients undergoing vitrectomy for either primary macula-off RD (n = 73) or epiretinal membrane (ERM; n = 64). Cellularity was assessed in vitreous cytospin preparations by a semi-quantitative immunostaining approach.
Results
Intravitreal glucose concentration was higher in the RD group (2.28 mmol.L-1 n =73 vs 1.6 mmol.L-1 n = 64; p < 0.0001). Overall cellularity and density of macrophages were significantly higher in the vitreous of RD patients (respectively p = 0.003 and p < 0.0001). Among the RD patients, intravitreal glucose concentration correlated with macrophages density (p = 0.002): its levels remained significantly higher in eyes in which macrophages were innumerable compared to lower macrophages densities RD eyes (p = 0.0095).
Conclusions
We observed a strong relationship between intravitreal glucose concentration and vitreous macrophage density. Additional indicators for vitreous glycation and low-grade inflammation should be further studied.
Similar content being viewed by others
Introduction
As a consequence of age, the vitreous liquefies, detaches from the retina. This can lead to peripheral vitreo-retinal traction, retinal tear formation and rhegmatogenous retinal detachment (RD) or to vitreo-macular traction and epiretinal membrane (ERM) formation [1, 2]. In spite of the frequent anatomical success of RD surgery, photoreceptor cell death may limit postoperative visual recovery [3]. Modulation of these cell death signalling pathways is an interesting therapeutic strategy to prevent blindness [4]. The precise mechanisms leading to photoreceptor cell death remain poorly understood, although many studies have shown the critical role of macrophage accumulation in the subretinal space, associated with changes in chemokine and cytokine levels in RD-associated vitreous [5, 6].
Interestingly, increased levels of intravitreal glucose and advanced glycation endproducts (AGE) have been observed in the vitreous of both non-diabetic and diabetic RD patients, with significantly higher concentrations in the latter [7,8,9,10]. AGEs are associated with mononuclear chemotaxis, and activation of macrophages through specific receptors (R-AGE) could be responsible for low-grade inflammation [11]. Over the last decade it has been shown that in several types of human retinal diseases, cone function and viability as well as inflammatory cells such as intravitreal macrophages are highly dependent on glucose metabolism [12,13,14]. Recently, Conart et al. [15] described a new mechanism by which inflammation induces retinal detachment-cone death through cone starvation, a mechanism that could be reversed by insulin.
The purpose of this study was to investigate a possible link between intravitreal glucose metabolism, low-grade inflammation and photoreceptor loss in an existing cohort of non-diabetic macula-off RD patients compared to control non-diabetic ERM patients.
Patients and methods
The vitreous of patients undergoing vitrectomy is routinely collected at Reims University Hospital. Patients with macula-off RD or ERM requiring vitrectomy between March 2015 and November 2017 were consecutively enrolled. Patients with diabetes, vitreous haemorrhages, previous history of vitreo-retinal surgery or uveitis, were excluded, as were patients who did not complete the follow-up period of 3 months. Written informed consent was obtained from all the patients. The study adhered to the tenets of the Declaration of Helsinki.
At the beginning of the 25-gauge pars plana vitrectomy, a 0.2 mL sample of undiluted vitreous fluid was collected by aspiration with a syringe before opening the infusion line. After the opening of the infusion line, a 5 mL-diluted vitreous sample was collected. All surgeries were performed by the same physician (CA).
Undiluted samples were analysed within 45 min in the laboratory of biochemistry at Reims University Hospital, using GOD-PAP colorimetric procedures. Perioperative capillary glycaemia and intravitreal glucose concentration were monitored as a standard procedure in all patients, regardless of diabetes status, with validated routine enzymatic assays with automated spectrophotometric detection (hexokinase method, Cobas 8000, ROCHE, Switzerland). Cytological examination was performed at the Department of Pathology at Reims University Hospital on the diluted samples (5 mL volume). Samples were first centrifuged using cytospin and six slides were prepared for microscopy as follows. Two slides were used for Papanicolaou and May–Grünwald–Giemsa stainings. The four remaining slides were treated with Merckofix® fixative spray (Millipore, MERCK, Germany), then stained by immunochemistry with the BenchMark XT automated slide stainer (Ventana Medical System, Tucson, USA), using with the following antibodies: AE1/AE3 (1:50) for epithelial cells identification, CD68-KP1 (1:100) for macrophages identification, GFAP (1:400) for glial cells identification and CD45 (1:50) for hyalocytes identification (all antibodies from DAKO, USA). All slides were microscopically evaluated by an experienced pathologist (CB) blinded to ophthalmological information. Macrophages, hyalocytes, lymphocytes, neutrophils, glial cells, red cells and epithelial cells were scored using a semi-quantitative scale: 0 = acellular vitreous sample, 1 = less than 10 cells on the whole slide, 2 = more than 10 cells on the slides but less than 10 on the most cellular field at high magnification (x40 magnification), 3 = innumerable cells.
Patient’s age, gender, preoperative best corrected visual acuity (BCVA) were obtained from their medical files. In case of RD, median number of retinal tears, Proliferative Vitreoretinopathy (PVR) stage (none, A, B or C) and RD extent (clock hours) were collected. Postoperative follow-up was performed at three weeks and three months and included BCVA, slit-lamp biomicroscopy, fundus view and OCT (Spectralis, Heidelberg engineering, Heidelberg, Germany), to measure the Mean Foveal Thickness (MFT). The main outcome measure was intravitreal glucose concentration. Cellularity, postoperative BCVA and MFT at three months were secondary outcome measures. For descriptive analysis, variables were expressed as mean values with standard deviation. Mann–Whitney tests were performed to compare quantitative variables. The correlation between intravitreal glucose concentration and different clinical or paraclinical parameters was evaluated with Pearson’s correlation tests after testing both variables for normality. Fisher exact tests and Chi2 tests were used to compare qualitative variables of cytologic findings. The relation between cytological findings and intravitreal glucose concentration was evaluated with ANOVA and Kruskal–Wallis tests with pairwise Bonferroni correction for multiple comparisons. Any p value below 0.05 was considered statistically significant.
Results
General findings
A total of 137 patients who underwent pars plana vitrectomy between March 2015 and November 2017 were included in the study: seventy-three eyes with primary macula-off RD and 64 with ERM. Details are given in Table 1. RD patients had a lower mean age than ERM patients (61 vs. 71 years; p = 0.002). Both far and near preoperative visual acuity were worse in the RD group, whereas post-operative visual acuity was not significantly different between the two groups. The RD extended between 1 to 12 clock hours (mean 8.2 ± 3.1). The postoperative mean MFT was significantly lower in the RD group.
Intravitreal glucose
Although RD patients were significantly younger than ERM patients, no correlation was found between patient’s age and intravitreal glucose level in neither RD (r = 0.04; p = 0.75) nor ERM (r = 0.12; p = 0.34) group. Intravitreal glucose concentration was on average 40% higher in the RD group compared to the ERM group (mean 2.28 vs 1.60 mmol.L−1; p < 0.0001). A significant correlation between blood glucose levels and intravitreal glucose concentration was found only in the ERM group (r = 0.7; p = 0,0071; Table 2). In the RD group, intravitreal glucose concentration was inversely correlated with post-operative MFT (r = −0.51; p = 0.0001). We also observed a significant (r = 0.38; p = 0.013) correlation between intravitreal glucose concentration and RD extent, while a tendency with no statistically significant correlation was noticed between the intravitreal glucose concentration and the number of retinal breaks (r = 0,25; p = 0.07; Table 2).
Vitreous cellularity
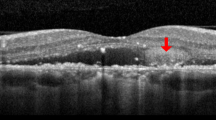
Macrophages, hyalocytes, lymphocytes, neutrophils, glial cells, red cells and epithelial cells were scored using a semi-quantitative immunostaining approach (Fig. 1, Table 3). The overall cellularity and the number of macrophages were significantly higher in the RD group compared to the corresponding values in the ERM group (Table 3). Macrophage density increased with RD extent (p < 0.0001, ANOVA test), while no such correlation was found for epithelial cells (p = 0.21, ANOVA test). No relationship between the density of macrophages and PVR was found (p = 0.98 CHi2 test). However, the density of epithelial cells was consistently higher in cases with PVR stage C compared with cases with no PVR (p = 0.002 CHi2 test).
Relationship between intravitreal glucose and cellularity
Among the RD patients, there was a direct link between glucose concentration and the density of vitreal macrophages (p = 0.0001, ANOVA test). The intravitreal glucose concentration was 50% higher in eyes in which macrophages were innumerable compared to RD eyes with no macrophages (2.98 ± 0.13 mmol.L−1 vs 2.03 ± 0.14 mmol.L−1, p < 0.0001; Table 4a), though no correlation was noticed with any other cell type (Table 4b and data not shown).
Discussion
In this study, both intravitreal glucose concentration and cytology were analysed in non-diabetic patients who underwent surgery for macula-off RD or ERM treatment. In RD patients, intravitreal glucose concentration and cytological findings were correlated to RD extent. Intravitreal glucose concentration was found to be strongly correlated with the density of vitreal macrophages. This is, to our knowledge, the first study describing and comparing intravitreal glucose concentration and cytology in human non-diabetic patients with RD and ERM.
Intravitreal glucose concentration was 40% higher in RD patients compared to ERM patients, in spite of the fact that none of the patients was diabetic. These values were lower than those previously reported in non-diabetic patients (3.5 ± 1.8 mmol.L−1) by Lundquist and Österlin [8]. It has been demonstrated that intravitreal glucose reflects glycaemia, owing to the influx of glucose through the blood retina barrier through GLUT-1 transporters [7,8,9]. Glucose concentration in the vitreous is about half its plasma concentration. We observed a correlation between intravitreal glucose and glycaemia in ERM patients, but not in RD patients. This indicates that glycaemia solely cannot explain this difference of intravitreal glucose levels between RD and ERM patients and suggests that intravitreal glucose concentration can depend on the underlying retinal disease, i.e. RD or ERM in our study, and not only on the diabetic status. This is also the first study to show no correlation between age and intravitreal glucose level.
In parallel, we observed significantly higher levels of overall cellularity, as well as higher macrophage density in the vitreous of RD patients compared to ERM patients. In contrast, the density of epithelial cells was similar in the two groups. In the RD eyes, increased epithelial cell density was significantly associated with a higher PVR stage. This is in accordance both with previous data and with the hypothesis that PVR could be associated with the migration of pigment epithelial cells out of the subretinal space [16, 17]. Macrophages are known to be either vitreous resident microglial cells or blood-borne cells that enter the vitreous following activation by multiple stimuli e.g., injury [18]. For this reason, patients with macroscopic vitreous haemorrhage were not included in this study. Since the number of red cells detected in RD eyes was not significantly higher than in ERM eyes, the augmentation that we observed in both the number of macrophages and the intravitreal glucose in the vitreous of RD patients could result from a non-haemorrhagic breakdown of the blood-ocular barrier, as already reported by Hiscott et al. [19]. This hypothesis is further supported by the correlation between the RD extent and both the higher density of macrophages and the increased intravitreal glucose. Cantrill and Pederson previously described such a breakdown of the blood-retinal barrier in rhegmatogenous RD [20]. It is likely that these permeability changes induced by some local effect are partly mechanical in nature, possibly involving fluid displacement through the retinal break, and physical disruption of tissues caused by the separation of the neurosensory retina and retinal pigment epithelium. In addition, permeability changes may also be brought about by locally increased vascular permeability [21], such as an increased influx of glucose into the vitreous via GLUT-1 transporters through the subretinal space [22]. However, our data do not support that hypothesis, since we observed no correlation between intravitreal glucose and glycemia in the RD group compared with the ERM group.
Another explanation for our findings could be a pre-existing higher intravitreal glucose level in eyes eventually developing RD. Stitt and al. suggested that the exposure to high glucose concentrations in diabetic patients could result in increased levels of advanced glycation end products (AGE) in the vitreous [23]. Indeed, AGE are formed through the non-enzymatic glycation of proteins by aldehyde or keto groups of reducing sugars in a process known as the Maillard reaction [24]. Further, AGE-induced cross-links in the vitreous collagen of extracellular matrix are known to cause tissue rigidity [9, 24,25,26]. Such irreversible cross-links persist on long-lived proteins and have been shown to accumulate with aging and at an accelerated rate in diabetes[27, 28]. This could also be the case in rhegmatogenous RD and proliferative diabetic retinopathy, as recently demonstrated by Fokkens et al. [10] and Coral et al. [29, 30].
To summarize, the increased intravitreal glucose concentration in the RD group could be associated with the loss of collagen elasticity through glycation and therefore an increase in vitreoretinal traction. As mentioned above, RD extent was significantly associated with both intravitreal glucose and macrophage density. However, no relationship was found between the number of retinal breaks and either intravitreal glucose or the score of macrophages, in spite of the fact that the number of tears could be an indicator of vitreoretinal traction and loss of elasticity.
Although we could not assess cone functionality using electrophysiology, this deserves further explorations. Indeed, previous electrophysiological studies of RD human eyes have reported reduced amplitudes and increased latencies compared to normal values, in full filed electroretinograms (ERGs) [31], focal ERGs [32] or multifocal ERGs [33], with evidence for retinal dysfunction due to outer retinal alterations in primary macula-off RD.
Our study did not investigate low-grade inflammation associated with the release of cytokines and chemokines. Such a mechanism could also contribute to macrophage proliferation [5, 15]. Several studies in mammalian model systems have demonstrated that, in response to retinal damage, bone-marrow-derived cells are homed to the eye where they proliferate, accumulate in the retina and in the subretinal space, contributing to retinal pathology following RD [6, 18, 34]. It has also been shown that monocyte chemoattractant protein 1 mediates RD-induced photoreceptor apoptosis by triggering macrophage accumulation and promoting oxidative stress [35]. Finally, apoptotic photoreceptors in a rat RD-induced model were found to be selectively eliminated from the original nuclear layer of the retina and directed into the subretinal space where they were phagocytosed by infiltrating monocyte-derived macrophages [36]. In parallel with the extent of the retinal detachment, low-grade inflammation is likely to be increased [37]. Additional indicators for vitreous glycation and low-grade inflammation, such as inflammatory cytokines, which could not be assessed in the setting of our study, should be further studied. Conart et al. [15] recently evaluated these inflammatory cytokines levels in RD eyes, and their data strongly suggested a link between insulin signalling and cone malfunction or death.
Summary
What was known before:
-
Inflammation induces retinal detachment-cone death through cone starvation, a mechanism that could be reversed by insulin.
What this study adds:
-
This study shows increased intravitreal glucose levels and macrophage cells density in non-diabetic patients with rhegmatogenous retinal detachment compared to patients with epiretinal membrane. First report showing that intravitreal glucose concentration can depend on the underlying retinal disease and not only on the diabetic status.
References
Sebag J. Anomalous posterior vitreous detachment: a unifying concept in vitreo-retinal disease. Graefe’s Arch Clin Exp Ophthalmol. 2004;242:690–8.
Sebag J. Vitreoschisis. Graefe’s Arch Clin Exp Ophthalmol. 2008;246:329–32.
Murakami Y, Notomi S, Hisatomi T, Nakazawa T, Ishibashi T, Miller JW, et al. Photoreceptor cell death and rescue in retinal detachment and degenerations. Prog Retin Eye Res. 2013;37:114–40.
Bird A. How to keep photoreceptors alive. Proc Natl Acad Sci USA. 2007;104:2033–4.
Kataoka K, Matsumoto H, Kaneko H, Notomi S, Takeuchi K, Sweigard JH, et al. Macrophage- and RIP3-dependent inflammasome activation exacerbates retinal detachment-induced photoreceptor cell death. Cell Death Dis. 2015;6:e1731–10.
Sene A, Apte RS. Inflammation-induced photoreceptor cell death. Adv Exp Med Biol. 2018;1074:203–8.
Sebag J, Buckingham B, Charles MA, Reiser K. Biochemical abnormalities in vitreous of humans with proliferative diabetic retinopathy. Arch Ophthalmol. 1992;110:1472–6.
Lundquist O, Österlin S. Glucose concentration in the vitreous of nondiabetic and diabetic human eyes. Graefe’s Arch Clin Exp Ophthalmol. 1994;232:71–4.
Sebag J. Diabetic vitreopathy. Ophthalmology 1996;103:205–6.
Fokkens BT, Mulder DJ, Schalkwijk CG, Scheijen JL, Smit AJ, Los LI. Vitreous advanced glycation endproducts and α-dicarbonyls in retinal detachment patients with type 2 diabetes mellitus and non-diabetic controls. PLoS One. 2017;12:1–11.
Singh R, Barden A, Mori T, Beilin L. Advanced glycation end-products: A review. Diabetologia 2001;44:129–46.
Chertov AO, Holzhausen L, Kuok IT, Couron D, Parker E, Linton JD, et al. Roles of glucose in photoreceptor survival. J Biol Chem. 2011;286:34700–11.
Aït-Ali N, Fridlich R, Millet-Puel G, Clérin E, Delalande F, Jaillard C, et al. Rod-derived cone viability factor promotes cone survival by stimulating aerobic glycolysis. Cell 2015;161:817–32.
Rajala A, Dighe R, Agbaga MP, Anderson RE, Rajala RVS. Insulin receptor signaling in cones. J Biol Chem. 2013;288:19503–15.
Conart JB, Blot G, Augustin S, Millet-Puel G, Roubeix C, Beguier F, et al. Insulin inhibits inflammation-induced cone death in retinal detachment. J Neuroinflammation. 2020;17:1–15.
Machemer R, Van Horn D, Aaberg TM. Pigment epithelial proliferation in human retinal detachment with massive periretinal proliferation. Am J Ophthalmol. 1978;85:181–91.
Mudhar HS. A brief review of the histopathology of proliferative vitreoretinopathy (PVR). Eye 2020;34:246–50.
Kataoka K, Nishiguchi KM, Kaneko H, van Rooijen N, Kachi S, Terasaki H. The roles of vitreal macrophages and circulating leukocytes in retinal neovascularization. Investig Ophthalmol Vis Sci. 2011;52:1431–8.
Hiscott PS, Grierson I, Mcleod D. Natural history of fibrocellular epiretinal membranes: a quantitative, autoradiographic, and immunohistochemical study. Br J Ophthalmol. 1985;69:810–23.
Cantrill HL, Pederson JE. Experimental retinal detachment. III. Vitreous fluorophotometry. Arch Ophthalmol. 1982;100:1810–3.
Little BC, Ambrose VMG. Blood—Aqueous barrier breakdown associated with rhegmatogenous retinal detachment. Eye 1991;5:56–62.
Takata K, Kasahara T, Kasahara M, Ezaki O, Hirano H. Ultracytochemical localization of the erythrocyte/HepG2-type glucose transporter (GLUT1) in cells of the blood-retinal barrier in the rat. Investig Ophthalmol Vis Sci. 1992;33:377–83.
Stitt AW, Moore JE, Sharkey JA, Murphy G, Simpson DAC, Bucala R, et al. Advanced glycation end products in vitreous: Structural and functional implications for diabetic vitreopathy. Investig Ophthalmol Vis Sci Ophthalmol Vis Sci. 1998;39:2517–23.
Bucala R, Vlassara H, Cerami A Advanced glycosylation endproducts. In: Harding JJ, Crabbe MJC, editors. Post Translational Modifications of Proteins Vol 2. CRS Press Inc., Boca Raton, FL; 1992. p. 53–9.
Fu MX, Wells-Knecht KJ, Blackledge JA, Lyons TJ, Thorpe SR, Baynes JW. Glycation, glycoxidation, and cross-linking of collagen by glucose: Kinetics, mechanisms, and inhibition of late stages of the Maillard reaction. Diabetes 1994;43:676–83.
Charonis AS, Tsilibary EC. Structural and functional changes of laminin and type IV collagen after nonenzymatic glycation. Diabetes. 1992;41:49–51.
Kohn RR, Cerami A, Monnier VM. Collagen aging in vitro by nonenzymatic glycosylation and browning. Diabetes 1984;33:57–9.
Stitt AW, Li YM, Gardiner TA, Bucala R, Archer DB, Vlassara H. Advanced glycation end products (AGEs) co-localize with AGE receptors in the retinal vasculature of diabetic and of AGE-infused rats. Am J Pathol. 1997;150:523–31.
Coral K, Angayarkanni N, Madhavan J, Bharathselvi M, Ramakrishnan S, Nandi K, et al. Lysyl oxidase activity in the ocular tissues and the role of LOX in proliferative diabetic retinopathy and rhegmatogenous retinal detachment. Investig Ophthalmol Vis Sci. 2008;49:4746–52.
Coral K, Madhavan J, Pukhraj R, Angayarkanni N. High glucose induced differential expression of lysyl oxidase and its isoform in ARPE-19 cells. Curr Eye Res. 2013;38:194–203.
Lin JB, Sein J, Van Stavern GP, Apte RS. Preoperative electrophysiological characterization of patients with primary macula-involving rhegmatogenous retinal detachment. J Ophthalmic Vis Res. 2018;13:241–8.
Montrone L, Ziccardi L, Stifano G, Piccardi M, Molle F, Focosi F, et al. Regional assessment of cone system function following uncomplicated retinal detachment surgery. Doc Ophthalmol. 2005;110:103–10.
Sasoh M, Yoshida S, Kuze M, Uji Y. The multifocal electroretinogram in retinal detachment. Doc Ophthalmol. 1997;94:239–52.
Kaneko H, Nishiguchi KM, Nakamura M, Kachi S, Terasaki H. Characteristics of bone marrow-derived microglia in the normal and injured retina. Investig Ophthalmol Vis Sci. 2008;49:4162–8.
Nakazawa T, Hisatomi T, Nakazawa C, Noda K, Maruyama K, She H, et al. Monocyte chemoattractant protein 1 mediates retinal detachment-induced photoreceptor apoptosis. Proc Natl Acad Sci USA. 2007;104:2425–30.
Hisatomi T, Sakamoto T, Goto Y, Yamanaka I, Oshima Y, Hata Y, et al. Critical role of photoreceptor apoptosis in functional damage after retinal detachment. Curr Eye Res. 2002;24:161–72.
Pollreisz A, Sacu S, Eibenberger K, Funk M, Kivaranovic D, Zlabinger GJ, et al. Extent of detached retina and lens status influence intravitreal protein expression in rhegmatogenous retinal detachment. Investig Ophthalmol Vis Sci. 2015;56:5493–502.
Acknowledgements
Authors would like to thank D. Marc and C. Bradley for their constructive comments and diligent proofreading of this manuscript.
Funding
This work was partly funded by a grant from the « Appel d’Offre Local » AOL 2010 of the Robert Debre Universitary Hospital, Reims, France.
Author information
Authors and Affiliations
Contributions
CA, BH, FH, MA, were responsible for designing the protocol, performing surgeries, collecting samples and data, interpreting results, and writing. CB performed statistical analyses and provided feedback on the report. PG and LR were responsible for designing the protocol, performed biochemical analyses, and contributed to writing the report. AH was responsible for extracting and analysing data, interpreting results, updating reference lists, and contributed writing the report. CBR was responsible for designing the protocol, conducted immunohistochemistry on samples, and contributed to interpreting results and writing the report.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Arndt, C., Hubault, B., Hayate, F. et al. Increased intravitreal glucose in rhegmatogenous retinal detachment. Eye 37, 638–643 (2023). https://doi.org/10.1038/s41433-022-01968-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-01968-w
This article is cited by
-
Developing and validating a clinlabomics-based machine-learning model for early detection of retinal detachment in patients with high myopia
Journal of Translational Medicine (2024)