Abstract
Background
To assess patients with indirect carotid-cavernous fistulas (CCF) for evidence of hypercoagulable state (HS) by combination of comprehensive medical questionnaire and laboratory testing.
Methods
Patients with confirmed diagnosis of CCF treated between 2003 and 2019 were included and administered a questionnaire screening for HS risk factors and undergone laboratory investigations which included complete blood count (CBC), prothrombin time (PT), partial thromboplastin time (PTT), fibrinogen, antiphospholipid antibodies (lupus anticoagulant and anticardiolipin antibody titres), Factor V Leiden, prothrombin, protein C, protein S, antithrombin III, homocysteine, prothrombin G20210, CALR and JAK2 mutation screening. Participants with abnormal laboratory testing and/or past history of ischemic stroke, atrial fibrillation, cancer or hypercoagulability-associated hereditary disorders were deemed to have HS.
Results
Twenty-two patients were enrolled. Seventeen were women and the mean age at diagnosis was 60. Fourteen (64%) had evidence of HS: six on medical history, three with laboratory evidence and five with both. Eight (36%) had current abnormal hypercoagulability markers. One had a diagnosis of Klippel–Trenaunay Syndrome, but no others had evidence of hereditary thrombophilia. Nine were on anti-coagulation initiated after diagnosis of stroke or atrial fibrillation discovered on average 5.5 years after the diagnosis of CCF.
Conclusion
A total of 64% percent of patients with previous indirect CCF had evidence of underlying HS indicating that hypercoagulability might play a role in the pathogenesis of CCF. The results support need for comprehensive testing for underlying HS in patients with indirect CCFs to better identify, manage, and prevent further thromboembolic events.
Similar content being viewed by others
Introduction
Carotid cavernous fistulas (CCFs) are among the most frequently encountered cranial arteriovenous shunts by ophthalmologists. Direct CCFs are high-flow shunts between the internal carotid artery (ICA) and the cavernous sinus (CS) and are almost always due to trauma. Indirect CCFs are low-flow shunts between the dural branches of the ICA or external carotid artery (ECA) or both and CS and their aetiology is not entirely clear. CCFs commonly cause a well-recognized constellation of symptoms of orbital venous stasis due to backflow of venous blood from the cavernous sinus to the orbit: proptosis, chemosis, conjunctival arterialization, diplopia, increased intraocular pressure and decreased visual acuity [1,2,3]. If untreated, they can lead to compressive optic neuropathy, venous stasis retinopathy, choroidal detachment, and rarely venous strokes due to rupture of cortical veins filled with arterialized blood.
Indirect CCFs are a subtype of brain dural arteriovenous fistulas (DAVFs) and are thought to form due to a combination of venous thrombosis, venous hypertension, angiogenesis, and arterial wall defects [4,5,6]. The sequence of the causative events is debatable, with one hypothesis being that venous thrombosis leads to venous hypertension and ischemia thus triggering angiogenesis [5,6,7,8]. While animal studies support this notion [4], there are no clinical studies evaluating whether dural sinus thrombosis (DST) precedes DAVF formation, is a consequence of it, or co-occurs with DAVF formation secondary to a yet undiscovered mechanism [5]. An association of hypercoagulable state (HS) with DAVFs has been suggested in prior studies, with one hypothesis being that HS may predispose patients to DST and subsequent DAVF formation [7].
Hypercoagulability risk factors for venous thromboembolic events (VTE) can be divided into three categories: situational, inherited and acquired [9, 10]. Situational risk factors are well-defined, transient clinical circumstances that are associated with greater VTE risk while they are present and for a short period after their resolution. These include surgery, prolonged immobilization, oral contraceptive pill (OCP) use, hormone replacement therapy (HRT), pregnancy, cancer chemotherapy and heparin-induced thrombocytopenia (HIT) [9]. Inherited risk factors include conditions causing disruption of coagulation homeostasis, resulting in greater thrombin generation and increased risk of clinical VTE. They include genetic mutations and polymorphisms that result in natural anticoagulant deficiencies (e.g., protein C, protein S or antithrombin), inherent abnormalities of procoagulant factor accumulation (e.g. prothrombin G20210A), coagulation factor resistance to inactivation by a natural anticoagulant (e.g., Factor V Leiden), and JAK2 mutations associated with polycythaemia vera, essential thrombocythemia, and other myeloproliferative disorders. Acquired risk factors include medical conditions or non-hereditary hematologic abnormalities that interfere with haemostasis. These include inflammatory bowel disease, nephrotic syndrome, vasculitis, presence of antiphospholipid antibodies, paroxysmal nocturnal haemoglobinuria, hyperviscosity syndromes, myeloproliferative disorders, and cancer. Hyperhomocysteinemia and elevated levels of factor VIII are examples of risk factors that can be either acquired or have a genetic predisposition [9].
A recent study by Polster et al. demonstrated that 15 out of 17 patients with DAVFs had a co-existing HS [11]. However, patients with CCFs were poorly and inconsistently represented among previously published cohorts. Given the hypothesized association of HS with future risk of thromboembolic events [11, 12], we assessed the largest cohort of patients with indirect CCFs to date for evidence of HS by a combination of comprehensive medical history assessment and laboratory testing.
Methods
Study design
A descriptive, investigational study based on a retrospective cohort.
The study was approved by the University of Toronto Health Sciences Research Ethics Board.
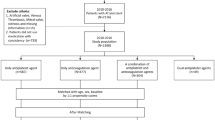
Patient selection
Between 2003 and 2019, 70 patients were diagnosed and treated for CCF at the University Health Network, a University of Toronto associated hospital. Of these, 55 had indirect CCFs and were considered for enrollment into the study.
Inclusion criteria was restricted to individuals over 18 years of age with previously confirmed diagnosis of indirect CCF on neuro-imaging (CT or MR angiography, Digital Subtraction Angiography (DSA) or cerebral angiogram) who were available for follow-up to complete a detailed hypercoagulable questionnaire and undergo laboratory work-up.
Data acquisition
All enrolled patients completed a clinical questionnaire inquiring about their smoking history, medication history (specifically inquiring about oral contraceptive therapy (OCT), hormone replacement therapy (HRT), and anticoagulants use), and past medical history (specifically inquiring about previous history of cancer, stroke, VTE, previous history of surgery or immobilization). All participants had a panel of laboratory investigations which included CBC, PT, PTT, D-dimer, Fibrinogen, antiphospholipid antibodies (lupus anticoagulant and anticardiolipin antibody titres), Factor V Leiden, prothrombin, protein C, protein S, antithrombin III, homocysteine, and prothrombin G20210 and JAK2 mutation screening.
Risk of hypercoagulability included hereditary risk factors known to predispose or cause VTE, situational risk factors such as surgery with immobilization greater than 2 weeks, pregnancy within 2 years preceding CCF diagnosis, use of HRT or OCT for 5 consecutive years or longer within 2 years preceding CCF diagnosis, and cancer-related treatment within 2 years preceding CCF diagnosis. Acquired risk factors included any medical condition known to be associated with thrombo-embolic disease.
A patient was defined as being a hypercoagulable state based on laboratory results if they had an abnormal results in any one of the following: antiphospholipid antibodies (lupus anticoagulant and anticardiolipin antibody titres), Factor V Leiden, prothrombin, protein C, protein S, antithrombin III, homocysteine, and prothrombin G20210 and JAK2 mutation screening. A patient was defined as being in a HS based on history if they had a positive history of any one of: stroke, atrial fibrillation, cancer, hormone replacement therapy (HRT). One patient was categorized as being in HS based on history of a Klippel Trenaunay Syndrome, a congenital vascular malformation syndrome with a high rate of VTE. Last, a patient was defined as being in HS state if they met either laboratory or history criteria above.
Data analysis
Data was captured onto a standardized excel data collection spreadsheet and descriptive statistics, such as measures of centrality (mean, median, mode) for continuous variables as well as ratios or percentages, were employed. Mann–Whitney testing was used to compare the time interval from diagnosis of CCF to hypercoagulability assessment between patients with a medical history of HS and those without. Where applicable, Fisher’s exact testing was used to compare proportions. A p value of 0.05 or less was considered to be of statistical significance.
Results
Patient sample
Twenty-two patients out of a total of fifty-five patients with indirect CCFs treated at the same institution between 2003 and 2019 fulfilled inclusion criteria and underwent hypercoagulability assessment. Mean age at CCF diagnosis was 59.4 years and 17 (77%) of patients were female.
Clinical questionnaire risk factors for hypercoagulability
Eleven patients (50%) had a history compatible with HS (Tables 1, 2): 1 with underlying hereditary risk factor, 9 with acquired risk factors and 1 with a situational risk factor. 5 patients were current or past smokers. Of the 17 female patients, 14 had a history of previous pregnancy but none occurred within 4 years of CCF diagnosis. 3 had a history of previous miscarriage, with 2 out of 3 reporting recurrent pregnancy loss. Four patients had a history of cancer but no history of metastasis. 2 were diagnosed and treated before CCF diagnosis. Of these 2 patients, 1 was diagnosed with left pheochromocytoma and underwent left adrenalectomy while the other was diagnosed with cancer of the vocal cords diagnosed ~6 years prior to CCF diagnosis and underwent radiation therapy only. Of the remaining 2 patients, 1 had a diagnosis of endometrial cancer diagnosed ~5 years after CCF diagnosis and underwent hysterectomy with bilateral oophorectomy while the other patient was diagnosed with right breast cancer diagnosed approximately 8 years after CCF diagnosis and underwent lumpectomy and lymph node removal followed by radiation therapy and chemotherapy.
Fourteen patients underwent some form of non-cancer related surgery but all reported an immobilization period of <1 week post-operatively. One patient had a history of Klippel-Trenaunay Syndrome (KTS) (a hereditary vascular malformation-related syndrome) but none others had a history of hereditary thrombophilic disease. Atrial fibrillation (AF) was present in 4 patients and history of previous stroke was reported in 3. Nine patients were currently on or had a history of being on anticoagulation therapy. There were no patients with a history of pulmonary embolism (PE) or deep vein thrombosis (DVT). Although 1 of 22 patients confirmed a history of previous heparin therapy in the past, none were ever diagnosed with heparin-induced thrombocytopenia.
Presence of hypercoagulable state on laboratory blood investigation
Eight (36%) patients had abnormal hypercoagulability markers with moderately elevated homocysteine (HC) levels (between 15 and 30 mcmol/L) in 4, and positive anti-cardiolipin antibody (ACLA) titers in 4. Of the 4 patients with elevated ACLA titres, 3 were female and 1 reported a history of miscarriage. There was no patient with elevated levels of Protein S or C. Zero patients (of 17 tested) had HIT platelet factor 4 antibodies and none tested positive for hereditary thrombophilias (Table 3).
Prevalence of hypercoagulable state based on both clinical history and laboratory investigation
Altogether, 14 (64%) patients had evidence of current and past HS based on clinical and/or laboratory criteria. Of the 8 patients with positive laboratory findings, 6 also had a positive history for hypercoagulability risk factors.
CCF diagnosis precedes discovery of hypercoagulable state
Nine patients in the cohort were on anti-coagulant medication. For 8 of these the indication to start anti-coagulation was discovered after CCF diagnosis. This delay was substantial, averaging 5.5 years and ranging from 0.6 to 13.3 years. The 2 patients with the longest delays had strokes. The rest were anti-coagulated because of a new diagnosis of atrial fibrillation or a hereditary condition. Concordant with this data, 11 patients with a medical history compatible with HS were diagnosed with CCF more remotely than those who did not (8.7 years vs. 3.5 years, Mann–Whitney test, P = 0.001) (Fig. 1). Taken together, this data strongly suggests that a diagnosis of CCF implies an underlying hypercoagulable state.
Age comparison in those with and without evidence of hypercoagulable state
Patients with evidence of underlying HS were not significantly older than those with no evidence of underlying hypercoagulability (95% CI [−10.7, 18.7], p = 0.549), suggesting age did not have a detectable effect on developing HS in this cohort. Similarly, patients with evidence of underlying HS did not differ from those without any evidence of underlying HS by age at which CCF was diagnosed (95% CI [−14.3, 15.2], p = 0.95).
Discussion
Indirect CCFs represent a subgroup of DAVFs which are low flow fistulas with more gradual onset [2]. The pathogenesis of DAVFs and CCFs is multifactorial and postulated to involve hypercoagulable predisposition [5,6,7]. We hypothesized that patients with indirect CCFs have an underlying or associated HS, as previous studies reported this relationship in patients with DAVF [5,6,7]. By systematically evaluating the largest cohort of patients with indirect CCFs to date, we found that an overwhelming proportion of patients (72.7%) had evidence of HS.
Laboratory evidence of hypercoagulability has been detected at highly variable rates among previously published patient cohorts with DAVF. The variable proportions and limited subgroup analysis of patients with indirect CCFs in those cohorts makes it difficult to compare them to our study population. However, in a case-control study of 18 patients with DAVFs, 12 of whom had CCF, Izumi et al. detected elevated D-dimer levels in 88.9% preoperatively [13]. Notably, D-dimer levels tended to increase immediately post-treatment, and then decreased to control levels after 1 year with subsequent decline over long-term follow-up, suggesting that hypercoagulability in DAVF may be a transient state. In our study, D-Dimer levels were elevated in a smaller proportion (n = 6, 27%) of patients, consistent with a more remote history of CCF treatment than that in Izumi et al. However, our results also suggest that D-dimer levels may remain elevated for a protracted period of time after indirect CCF treatment, as the mean time from CCF treatment to laboratory testing was 6.1 years (range: 0.4–15.1 years).
Antiphospholipid syndrome is an acquired thrombophilia known to be associated with VTE and stroke [14]. Risk of thrombosis is dependent on the type and number of antiphospholipid antibodies present. Lupus anticoagulant holds 6–11 fold increased risk while presence of anticardiolipin antibodies (ACLA) holds a 1.6–3.2 fold increased risk of VTE [9, 14]. Furthermore, antiphospholipid antibodies are present in about 9% of patients with a history of miscarriage, in 14% with history of stroke and in 11% with myocardial infarction [14]. We identified the presence of raised titres of ACLA in 4 (18%) patients in our study. Of these, 1 patient had a history of previous miscarriage and AF while another had a history of cancer and AF.
Hyperhomocysteinemia is associated with a 2–4 fold increased risk for VTE [9]. In patients with associated methylenetrahydrofolate (MTHFR) polymorphisms in the C677T gene, the risk is higher. Elevated homocysteine levels were found in 4 (18%) of our patients, similar to prior reports evaluating patients with DAVF [11, 15].
Prior studies estimate the incidence of hereditary thrombophilias in patients DAVF to be between 10% and 40% [11, 12, 15,16,17,18]. Although early studies rarely assessed >20 patients, two recent cohorts totaling 281 patients with DAVF, 47 of whom had CCF, detected the prothrombin G20210A mutation in 6–18% cases, Factor V Leiden in 3–8%, and MTHFR in 15% [12, 18]. However, these studies did not distinguish between direct or indirect CCFs, nor was a comprehensive assessment of hypercoagulability performed. Nevertheless, such estimates are in keeping with 5- and 10-fold increase in frequency of DAVF in patients with Factor V Leiden and prothrombin G20210A mutations [17]. In our study sample of 22 patients with indirect CCF, none of the patients had evidence of hereditary thrombophilia despite testing for Factor V Leiden and prothrombin G20210A mutations in addition to more recently described mutations (JAK2 and CALR) associated with hypercoagulable state. While this could be secondary to the relatively small sample size, it might suggest that hereditary thrombophilias are less common in patients with indirect CCFs [17].
After completion of an extensive questionnaire, we identified 50% of patients in our study who had risk factors for HS, such as atrial fibrillation, stroke, cancer, and a hereditary vascular disorder. History of current or previous smoking was reported in 5 patients, 4 of whom also had independent risk factors for a HS. However, due to the small study population and lack of supportive literature, we did not consider smoking a risk factor for HS.
Presence of cancer is an established risk factor for a HS and VTE [9, 11] while prevalence of underlying HS in patients with DAVFs has been established to be higher when compared with the general population [5,6,7]. Thus, screening for cancer in patients with evidence of a HS (such as in cases with DAVF) is considered reasonable clinical practice. Although Polster et al. found that cancer was very common in their series of patients with DAVFs [11], cancer history was reported in only 18.2% (n = 4) of patients in our cohort. It is possible that this discrepancy stems from small sample sizes in both studies or suggests patients with indirect CCFs are distinct from those with DAVFs. In any case, prevalence of cancer increases independently with age [9, 11]. Therefore, results from both Polster et al. and this cohort should be interpreted with caution, as both study populations were predominantly older with mean age of 62 and 60, respectively.
PE and DVT are common presentations of VTE in patients with underlying HS which constitute the third most common cardiovascular disease [9]. None of the patients in our study had a confirmed history of previous PE or DVT.
There were a large number of patients within this cohort with known vascular risk factors such as dyslipidemia, hypertension and diabetes mellitus (Table 1) which may contribute to the risk factor profile for patients with CCF.
The most significant limitation of this study was its small sample size given the nature of the prevalence of indirect CCFs. In addition, it suffers from selection and survival biases as only a subset of patients who were available and consented to participate in the study were included and it was not control-based. Due to the retrospective cohort of patients having already been diagnosed and treated for CCF, data related to laboratory investigations for HS at time of initial presentation is lacking and, thus, trend analysis is deficient.
However, when combining results from the clinical history and laboratory testing, we detected evidence of HS in an overwhelming majority of patients (64%) who were treated for indirect CCF (n = 14) in the past. These results support the hypothesis that underlying HS is common in patients with indirect CCFs and validate the recommendation that all patients with indirect CCF should undergo laboratory testing for underlying HS. Our study adds to the growing evidence base that DAVFs are associated with HS. Critically, nine patients were on anti-coagulation therapy, with 8 of those starting medication for an indication discovered on average 5.5 years after CCF diagnosis. Such a delay may risk irreversible consequences of HS, such as stroke or MI. Identifying HS early and treating it is important in preventing further cardiovascular events and mitigating risk for patients with indirect CCFs.
Conclusion
We describe the presence of risk factors for HS in the largest cohort of patients with indirect CCFs to date. Our results indicate that patients with indirect CCFs have a very high prevalence of HS and contributes to increasing evidence that DAVFs are associated with HS. This study supports the need for all patients with newly diagnosed indirect CCFs to undergo a comprehensive hypercoagulability screen in order identify and mitigate the risk of future thrombo-embolic events.
SUMMARY
What was known before
-
Carotid-cavernous fistulas are the most common arterio-venous shunts encountered by ophthalmologists who are often the one diagnosing this condition. Most ophthalmologists in any sub-specialty will encounter a patient with CCF in their practices. While the aetiology of indirect CCF formation is poorly understood, recent work has suggested that hypercoagulability plays an important role in pathogenesis. Prevalence of hypercoagulable state (HS) has been evaluated in patients with brain dural arterio-venous fistulas recently, however, no study has specifically looked at this relationship in a subset of patients with CCF.
What this study adds
-
We describe the presence of risk factors for HS in the largest cohort of patients with indirect CCFs to date. Our results indicate that patients with indirect CCFs have a very high prevalence of HS and contributes to increasing evidence that DAVFs are associated with HS. This study supports the need for patients with newly diagnosed indirect CCFs to undergo a comprehensive hypercoagulability screen in order to identify and mitigate the risk of future thrombo-embolic events.
References
Chung SJ, Kim JS, Kim JC, Lee SK, Kwon SU, Lee MC, et al. Intracranial dural arteriovenous fistulas: analysis of 60 patients. Cerebrovasc Dis. 2002;13:79–88.
Gemmete JJ, Chaudhary N, Pandey A, Ansari S. Treatment of carotid cavernous fistulas. Curr Treat Options Neurol. 2010;12:43–53.
Gandhi D, Chen J, Pearl M, Huang J, Gemmete JJ, Kathuria S. Intracranial dural arteriovenous fistulas: classification, imaging findings, and treatment. Am J Neuroradiol. 2012;33:1007–13.
Herman JM, Spetzler RF, Bederson JB, Kurbat JM, Zabramski JM. Genesis of a dural arteriovenous malformation in a rat model. J Neurosurg. 1995;83:539–45.
Williams ZR. Carotid-cavernous fistulae: a review of clinical presentation, therapeutic options, and visual prognosis. Int Ophthalmol Clin. 2018;58:271–94.
Uranishi R, Nakase H, Sakaki TS. Expression of angiogenic growth factors in dural arteriovenous fistula. J Neurosurg. 1999;91:781–6.
Mironov A. Classification of spontaneous dural arteriovenous fistulas with regard to their pathogenesis. Acta Radiol. 1995;36:582–92.
Bhogal P, Yeo LL, Henkes H, Krings T, Söderman M. The role of angiogenesis in dural arteriovenous fistulae: the story so far. Inter Neuroradiol. 2018;24:450–4.
Deitcher SR, Gomes MPV. Hypercoagulable state testing and malignancy screening following venous thromboembolic events. Vasc Med. 2003;8:33–46.
Beckman MG, Hooper WC, Critchley SE, Ortel TL. Venous thromboembolism: a public health concern. Am J Prev Med. 2010;38:S495–501.
Polster SP, Zeineddine HA, Baron J, Lee SK, Awad IA. Patients with cranial dural arteriovenous fistulas may benefit from expanded hypercoagulability and cancer screening. J Neurosurg. 2018;129:954–60.
LaHue SC, Kim H, Pawlikowska L, Nelson J, Cooke DL, Hetts SW, et al. Frequency and characteristics associated with inherited thrombophilia in patients with intracranial dural arteriovenous fistula. J Neurosurg. 2018:1–5.
Izumi T, Miyachi S, Hattori K, Iizuka H, Nakane Y, Yoshida J. Thrombophilic abnormalities among patients with cranial dural arteriovenous fistulas. Neurosurgery. 2007;61:262–8.
Carroll BJ, Piazza G. Hypercoagulable states in arterial and venous thrombosis: When, how, and who to test?. Vasc Med. 2018;23:388–99.
Gerlach R, Boehm-Weigert M, Berkefeld J, Duis J, Raabe A, Seifert V. et al. Thrombophilic risk factors in patients with cranial and spinal dural arteriovenous fistulae. Neurosurgery. 2008;63:693–98.
Gerlach R, Yahya H, Rohde S, Böhm M, Berkefeld J, Scharrer I. et al. Increased incidence of thrombophilic abnormalities in patients with cranial dural arteriovenous fistulae. Neurol Res. 2003;25:745–8.
van Dijk JM, TerBrugge KG, Van der Meer FJ, Wallace MC, Rosendaal FR. Thrombophilic factors and the formation of dural arteriovenous fistulas. J Neurosurg. 2007;107:56–9.
Aiello G, Rinaldo L, Marshall AL, Vine RL, Lanzino G. Incidence of hereditary thrombophilia in patients with cranial dural arteriovenous fistulae. J Clin Neurosci. 2020;73:136–9.
Author information
Authors and Affiliations
Contributions
EM, TJP, KZ and PN contributed to the planning, assisted in conducting the study as well as reporting of the work described in the article. All four authors equally accept responsibility as guarantor for the overall content.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Patel, T.J., Zaslavsky, K., Nicholson, P. et al. Hypercoagulability in patients with indirect carotid cavernous fistulas. Eye 36, 1982–1987 (2022). https://doi.org/10.1038/s41433-021-01801-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01801-w