Abstract
Background
Acanthamoeba keratitis (AK) is an important cause of ocular morbidity in both contact lens wearers and non wearers. Medical management comprises prolonged empiric treatment with multiple drugs, leading to adverse effects and suboptimal cure. The present study evaluated the efficiency and safety of common antimicrobial agents used in treatment of AK.
Methods
Six Acanthamoeba isolates (four AK, two water samples) were axenized and subjected to in vitro susceptibility testing against chlorhexidine, pentamidine isethionate, polymyxin B, miltefosine, and fluconazole to check for trophocidal and cysticidal activity. The safety profile was analysed by observing the cytotoxicity of the highest cidal concentration toward human corneal epithelial cell (HCEC) line.
Results
Chlorhexidine had the lowest cidal concentration against both cysts and trophozoites (range 4.16–25 μg/ml) followed by pentamidine isethionate (range 25–166.7 μg/ml). Both agents were nontoxic to HCEC. Polymyxin B (range 25–200 μg/ml) and fluconazole (range 64–512 μg/ml) had relatively higher minimum inhibitory concentrations (MIC); fluconazole was nontoxic even at 1024 μg/ml, but cytotoxicity was observed at 400 μg/ml with polymyxin B. Miltefosine was not effective against cysts at tested concentrations. A. castellanii were more susceptible to all agents (except pentamidine isethionate) than A. lenticulata. Clinical isolates were less susceptible to polymyxin B and fluconazole than environmental isolates, reverse was true for miltefosine.
Conclusion
Chlorhexidine and pentamidine isethionate were the most effective and safe agents against both trophozoites and cysts forms of our Acanthamoeba isolates. Fluconazole had higher MIC but was nontoxic. Polymyxin B was effective at high MIC but therapeutic dose was found toxic. Miltefosine, at tested concentrations, could not inhibit cysts of Acanthamoeba. Clinical isolates had higher MICs for polymyxin B and fluconazole.
Similar content being viewed by others
Introduction
Acanthamoeba keratitis (AK), the corneal infection caused by pathogenic free-living amoeba belonging to genus Acanthamoeba, is a severe and potentially sight-threatening condition [1]. Though AK was first reported in early 1970s, a steep increase in incidence of AK was observed in 1980s parallel to the usage of soft contact lenses (CL) [2] so much so that Centers for Disease Control and Prevention (CDC) issued an advisory in 1985 to alert the ophthalmologists regarding the association of AK with use of CL [3]. The factors contributing to this association include a combination of corneal microtrauma, suboptimal CL hygiene, exposing CL to contaminated water environments and improper storage [2]. Another more traditional route of infection, the predominating risk factor for AK in Asian countries [4] and rural settings [5], is the exposure of an injured corneal epithelium to water or soil contaminated with Acanthamoeba. Thus, environmental contamination, especially that via water containing Acanthamoeba [6], is an important risk factor for AK for both CL- and non-CL wearers. AK has also been reported following invasive corneal surgery [7] and there is one reported case where no risk factor could be identified [8].
The global incidence of AK is difficult to ascertain as not only the incidence varies with geographical area and risk factor involved, but the clinical presentation of AK also mimics those of other infectious keratitis, especially herpetic and fungal [9]. Though a tentative diagnosis of AK can be made by visualizing the typical parasite using either in vivo confocal microscopy [10] or examining the corneal scraping under microscope, culture remains the gold standard for microbiological diagnosis [11]. Culture being cumbersome and time-consuming, PCR-based identification is being widely used as a rapid and sensitive approach for AK diagnosis [12].
The management of AK encompasses timely diagnosis and achieving medical cure with restoration of corneal transparency. Penetrating keratoplasty is done in elective conditions for optical indications [2, 9]. To achieve a medical cure, a variety of drugs are usually started empirically and given for long durations of time extending for months together [13]. However, since Acanthamoeba can biologically shift between trophozoite and cyst forms, not all drugs can effectively clear the infection as either the cyst form is resilient to the usual dosage of drug or the dosage required for clearance is too toxic for corneal epithelium [14]. Thus, in vitro susceptibility testing (IVST) of potential therapeutic agents against both morphological forms of Acanthamoeba may contribute to customized therapy for the patient of AK, thereby leading to favorable clinical outcomes. Though several studies have evaluated the in vitro susceptibility of varied drugs on AK isolates [15,16,17,18], these studies are geographically limited and have employed varied parameters for end-result evaluation. To the best of our knowledge, other than a study by Narsimhan et al. [19] that evaluated minimum cysticidal concentration (MCC) for two antiparasitic agents in year 2002, there is no Indian study evaluating IVST for AK isolates. The present study was therefore designed to systematically carry out IVST of Acanthamoeba isolates from AK and environmental sources to determine the therapeutic options for Indian isolates. Miltefosine, the repurposed drug being increasingly used for AK, granulomatous amoebic encephalitis and fungal keratitis, was also evaluated along with other conventional drugs. Further, host cytotoxicity assays were conducted to evaluate safety of use for the resultant effective drug concentrations. To the best of our knowledge, such cytotoxicity assays on human corneal epithelial cell (HCEC) lines have not been performed for anti-acanthamoebic drugs.
Materials and methods
Acanthamoeba strains
Out of 300 clinically-suspected cases of AK presenting to our tertiary care center over a period of 4 years (2014–2018), 11 cases were confirmed as AK by 18S rDNA sequencing, as described previously for granulomatous amoebic encephalitis isolates [20]. Further, from 100 water samples (tap water or swabs from inner side of tap mouth) collected from various intensive care units of our institute in the year 2014, four were molecularly confirmed to be containing Acanthamoeba spp [21]. Although nine out of 11 AK isolates and all four water isolates could be cultured on NNA medium, only four AK and two water isolates could be axenized and maintained for carrying out all IVST experiments. Among the four AK isolates, two were A. castellanii (T4), 1 A. lenticulata (T5), and 1 A. hatchetti (T3). Between the two water isolates, one was A. castellanii and other was A. lenticulata. The study was approved by the Institute Ethics Committee (INT/IEC/2017/674).
Maintenance of Acanthamoeba isolates
All the six Acanthamoeba isolates were slowly adapted to axenic culture without bacteria in improvised PYG media supplemented with RNAase and NCTC109 vitamin mixture till Acanthamoeba trophozoite monolayer was obtained [22]. For encystment, Acanthamoeba trophozoites in axenic culture were inoculated onto non-nutrient agar plates without Escherichia coli. The NNA plates were incubated at 30 °C for 7 days. After encystment the actively multiplying trophozoites were converted to cysts and were then collected in 1 ml of PBS and stored at 4 °C for drug susceptibility testing.
In vitro drug susceptibility testing
Procedure
The Acanthamoeba isolates were tested for their susceptibility to the following drugs: chlorhexidine, pentamidine isethionate, polymyxin B sulfate, miltefosine, and fluconazole (all purchased from Sigma Aldrich, India). The drug susceptibility testing were designed to determine minimal motility inhibition concentration (MMIC), minimal inhibitory concentration (MIC), and MCC of the drugs. Briefly, the stock solutions of all the therapeutic drugs were prepared in peptone yeast dextrose medium and subsequently twofold serial dilutions were made. The numbers of cysts or trophozoites were counted in a hemocytometer and suspension was adjusted to a final concentration of 104 cysts or trophozoites/mL. Four hundred microliter of each drug concentration was placed in 24 well tissue culture plate (Greiner Bio-one, Germany). One hundred microliter suspensions containing 104 trophozoites/ml were added to each well and were incubated at 30 °C for 6, 24, and 48 h, as described previously [23]. The positive control was trophozoite/cysts mixed with PBS and negative control contains only drug without the addition of the trophozoite/cysts. The plates were incubated for a total of 48 h and read at 6 h for MMIC determination, and at 24 h and 48 h for MIC50 and MIC90 determination. The in vitro drug susceptibility testing was carried out in triplicate in three different sets of experiments and subjective assessment was performed by a trained microscopist. Means were calculated for the 6 h—MMIC, 24 h and 48 h MIC50 and MIC90, and MCC against each strain for every drug.
Interpretation
MMIC-6 h
The MMICs at 6 h were visually observed by microscopic examination and compared with controls. The MMIC was defined as the minimum concentration of drug that inhibits pseudopodial activity as compared to controls and is characterized by rounding up, diminution in size, and increase in granulation [23].
MIC50-24, MIC50-48, MIC90-24, and MIC90-48 h
The MIC50 and MIC90 was defined as the minimum concentration of drug at which growth was <50% and 90%, respectively, as compared to control, as observed by microscopic examination [23].
MCC
MCC was defined as the minimum concentration of drug needed to prevent trophozoite formation after 14 days of incubation. The twofold drug dilutions were made for each drug, 100 µl of cysts at a concentration of 104 cysts/ml was added and the tubes were incubated at 30 °C for 48 h. After 48 h of incubation, the tubes were centrifuged at 5000 × g for 5 min. The supernatant of drug solution were removed and deposited cysts were washed twice with PBS to remove the drug. The NNA plates with E.coli were labeled and final washed cysts were inoculated on respective plate including controls and incubated at 30 °C. Plates were first examined after 2 days and then daily till 14 days for the presences of trophozoites. Results were compared to positive control without drug which show presence of trophozoites after 48 h of incubation [19].
Host cytotoxicity assay
Cell culture
The HCEC were grown in 25 cm2 culture flasks (Greiner Bio-one, Frickenhausen, Germany). The cells were cultured in Dulbecco’s Modified Eagle’s Medium DMEM/F-12 1:1 (Sigma) supplemented with 10% fetal bovine serum and 1% penicillin/streptomycin/amphotericin B (sigma) in humidified environment at 37 °C with 5% CO2. The cell lines were allowed to grow for 48–72 h. The growth medium was replaced with fresh growth medium every second day. After formation of confluent monolayers (examined under inverted phase contrast microscope), the cells were sub cultured by splitting with trypsin EDTA.
Cytotoxicity assay
The MTT assay was performed to determine the cell cytotoxicity of all the therapeutic drugs for Human corneal cell line (HCEC). The evaluation is based on the reduction of MTT (3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyl tetrazolium bromide) by the mitochondrial dehydrogenase of viable cells, to give a blue formazan product that is measured spectrophotometrically. The MTT was dissolved in the growth medium as 5 mg/ml stock solution.
The HCEC cells (1 × 105/ml) were seeded in 96 well microplates and incubated at 37 °C overnight with 5% CO2 for attachment. After 24 h, when 90% confluence was achieved, freshly prepared dilutions of all the therapeutic drugs in growth medium were added to the each well and the cultures were further incubated. After 6, 12, 24, and 48 h, the cells were washed with 1× sterile PBS and 20 µl freshly prepared working solution of MTT was added for a further incubation period of 3 h. After 3 h, the MTT solution was removed and 100 µl of DMSO was added in both treated and non-treated wells to dissolve the formazan and incubated for 15 min at 37 °C with shaking. Optical density was measured spectrophotometrically at 596 nm with 620 nm as reference wavelength. Cell line without drug was taken as positive control and cells without MTT as negative control. Percentage of cell cytotoxicity was calculated as:
The acceptable limit of cytotoxicity was taken as the viability cutoff of 60%, as described previously [24], thus a cytotoxicity of >40% was considered unacceptable.
Results
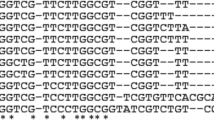
In vitro activity of anti-Acanthamoebic drugs (Figs. 1, 2, 3)
Chlorhexidine
Among all the tested drugs, chlorhexidine was effective at the lowest concentrations for all parameters. It showed both trophocidal and cysticidal activity. The environmental A. castellanii (4.16 μg/ml; N = 1) had lower MMIC-6 h than clinical A. castellanii (10.42 μg/ml; N = 2). The MIC90 was lower for A. castellanii as compared to A. lenticulata for the environmental isolates [(MIC90-24 h) (6.25 μg/ml vs. 12.5 μg/ml, N = 1 for each] and clinical isolates [(MIC90-48 h) mean 10.42 μg/ml, N = 2; vs. 16.67 μg/ml; N = 1) strains]. The MCC among AK isolates was lower for A. castellanii (mean 12.5 μg/ml; N = 2) and A. hatchetti (12.5 μg/ml; N = 1) as compared to A. lenticulata (25 μg/ml; N = 1), while no such difference was observed between water samples.
The isolates consisted of A. castellaniii (n = 2), A. lenticulata (n = 1) and A. hatchetti (n = 1). The susceptibility was evaluated against miltefosine, chlorhexidine, fluconazole, pentamidine isethionate and polymyxin B. The x-axis represents the six parameters used to test susceptibility and the y-axis represents the mean drug concentration.
Pentamidine isethionate
The trophocidal activity of pentamidine isethionate was nearly uniform for all isolates, irrespective of their origin (clinical or environmental) and genotype. With regard to cysticidal activity, the MCC of pentamidine isethionate was higher for clinical strain of A. lenticulata (166.7 μg/ml; N = 1) as compared to both A. castellanii (mean 100 μg/ml; N = 2) and A. hatchetti (100 μg/ml; N = 1). No such difference was observed between environmental isolates.
Polymyxin B sulfate
With regard to trophocidal activity, similar response was observed among clinical isolates, irrespective of genotype. The trophocidal activity among environmental isolates varied with the genotype; A. castellanii was more susceptible than A. lenticulata for all parameters tested except MMIC-6 h. Among A. castellanii isolates, clinical strains were less susceptible than environmental strains for all the parameters tested except MIC90-24 h. With regard to cysticidal activity, A. lenticulata (200 μg/ml; N = 1) was least susceptible to polymyxin B, irrespective of source.
Miltefosine
With regard to trophocidal activity, miltefosine showed better activity against clinical isolates for both the genotypes than their corresponding environmental isolates; i.e., clinical A. castellanii was more susceptible than environmental A. castellanii, and clinical A. lenticulata was more susceptible then environmental A. lenticulata against the parameters MMIC-6 h and MIC50. For MIC90, this difference was observed only for A. castellanii. Even among the clinical strains, the MIC at 24 h (both MIC50-24 h and MIC90-24 h) was lower for A. castellanii that other two genotypes. The cysticidal activity of miltefosine was poor with all strains having MCC of 256 μg/ml, irrespective of source and genotype.
Fluconazole
The trophocidal activity of fluconazole varied with the source as well as genotype. While clinical isolates of A. castellanii were more susceptible to fluconazole than A. lenticulata or A. hatchetti for all parameters tested, no such difference was observed among environmental strains for any of the parameters. Further, with respect to genotype A. lenticulata per se, clinical isolates were less susceptible than environmental isolates for all parameters. The cysticidal activity for fluconazole was observed at relatively higher concentrations that all other drugs tested. Among clinical isolates, MCC was lower for A. castellanii (mean 341.3 μg/ml; N = 2) as compared to other two genotypes (512 μg/ml; N = 1 for each); no difference among environmental isolates was observed. With regard to genotype, cysts of A. lenticulata from clinical samples (MCC 512 μg/ml; N = 1) were more resilient to fluconazole that those recovered from water samples (MCC 256 μg/ml; N = 1).
The MIC of each isolate against each parameter and drug, when done in triplicate, was within ±1 twofold dilution, thus vouching for repeatability of assay.
Host cytotoxicity analysis
The cytotoxic effect of different drugs, as tested on HCEC using MTT assay, is depicted in Table 1. At observed effective drug concentrations, chlorhexidine and polymyxin B were least toxic to HCEC cells with 24.67% and 24.89% cytotoxicity, respectively, at 24 h and 25.8% and 27% cytotoxicity, respectively, at 48 h. The cytotoxicity of pentamidine isethionate at observed cidal concentrations was 26.78% at 24 h and 28.9% at 48 h. Fluconazole exhibited toxicity of 31.61% for observed cidal concentration at 24 hr and 29.18% at 48 h. For miltefosine, the cytotoxicity could not be evaluated as the observed cidal concentration was 256 μg/ml and the range of drug concentration tested was 2–128 μg/ml.
On evaluating the cytotoxicity of these drugs at the highest concentration tested, chlorhexidine had the least toxicity of 29.45% at 24 h and 32.34% at 48 h. Pentamidine isethionate, at highest concentration of 400 μg/ml, had acceptable toxicity of 39.29% at 24 h which increased to unacceptable toxicity of 44.67% at 48 h. The toxicity of polymyxin B, at highest tested concentration of 400 μg/ml, was >40% at both times with highest toxicity of 46.67% at 48 h. The cytotoxicity of fluconazole at highest tested concentration of 1024 μg/ml was marginally above 40% at both the times and that for miltefosine at highest tested concentration of 128 μg/ml was ~37% at both the times.
Discussion
AK is a therapeutic challenge with potential for treatment failure. With no specific drug being approved for AK by Food Drug and Administration [9], various antimicrobials are given in different combinations for different durations to increase the likelihood of successful treatment. The treatment is to be continued for prolonged periods of time even after clinical resolution of active infection as the drugs are less active against the cystic forms and untimely stoppage of medication can result in relapse [9]. Further, since Acanthamoeba are eukaryotes and share several functional homologies with mammalian cells, many of the drugs cannot be prescribed at their effective concentrations due to untoward side effects. Therefore, as rightly suggested by Siddiqui et al. [25] in their elaborate review, a “targeted therapeutic approach” should be developed based on the mechanism of action of the drugs so as to harness their maximum antiparasitic effect without concomitant host damage. Broadly, anti-AK drugs can be grouped as membrane-acting agents [like biguanides (chlorhexidine), antibacterial agents (polymyxin B), and antifungal agents (fluconazole)], nucleic acid acting agents (pentamidine isethionate), and intracellular targeting agents (miltefosine) [25]. For the present study on in vitro evaluation of susceptibility of Acanthamoeba, we intentionally selected agents representing each of these mechanisms of action. The commonly used drug polyhexamide (PHMB) was intentionally not evaluated as the phase III ODAK (Orphan drugs for AK) clinical trial (European Clinical Trial 2016-001823-30) addressing its efficacy and safety profile is underway since 2017.
In the current study, the drug with highest anti-acanthamoebic activity was chlorhexidine. With an MIC ranging from 4.16 to 16.67 μg/ml and MCC ranging from 12.5 to 25 μg/ml, it showed potent trophocidal and cysticidal activity. A. castellanii strains were more susceptible than A. lenticulata, and environmental strains were more susceptible than AK strains. Single study by Padzik et al. [26] reported environmental A. castellanii Neff strain to be more resilient to chlorhexidine than clinical A. polyphaga from AK patient. Since no other study on anti-acanthamoebic drugs has compared in vitro activity of AK strains with environmental strains or inter-genotypic evaluation, a direct comparison with available literature is not possible. With regard to trophocidal activity of chlorhexidine, the MIC of our isolates lie well within the range reported in previous studies. Elder et al. [16] in their pioneering work on 23 AK isolates from London in 1994, reported mean MIC of 0.7 μg/ml for chlorhexidine and Lim et al. [15] reported mean MIC of 32 μg/ml (ranging from 16 to 64 μg/ml) for their 19 Australian AK isolates. However, while Elder et al. [16] have not reported genotypic characterization of isolates, Lim et al. [15] included one A. castellanii and two A. hatchetti strains but have not reported any inter-genotypic comparison. Ortega et al. [17] reported MIC of 4.68 μg/ml for chlorhexidine against one clinical A. castellanii strain from AK patient. With regard to cysticidal activity of chlorhexidine, our isolates (n = 6) had MCC similar to that reported by Llyod (27 μg/ml) [27] and lower than 40 μg/ml reported from Australia in the year 2000 (n = 19) [15] and 32.81 μg/ml reported from South India in 2001 (n = 19) [19]. This difference could arise due to geographical and genotypic variations among the isolates, and differences in in vitro assays. Interestingly, the mean MCC for chlorhexidine reported by Elder et al. [16] from London in 1994 was 2.77 μg/ml and that by Perez et al. [28] from the same hospital in London, in 2003 was 10.8 μg/ml. This suggests that, may be slowly, but MCC to even the most active agent has increased over a decade and hence it becomes important that local susceptibility data is generated as a continuous process.
Chlorhexidine, in the present study, was found to be safe for use at observed cidal concentration (25 μg/ml) and highest tested concentration (50 μg/ml) with cytotoxicity ranging from 24 to 32%. For the treatment of AK, chlorhexidine is used as a 0.02% topical agent, i.e., concentration of 200 μg/ml. Although the available world literature has reported highest MIC or MCC of 64 μg/ml for chlorhexidine among AK isolates, the recommended dosage contains a 2–3 higher fold concentration as firstly, it would compensate for the dilution of drug happening by continuous lacrimal fluid flow, and secondly, even at higher concentration than 200 μg/ml, chlorhexidine has been found safe [29]. However, the concentration of chlorhexidine (0.003%; 30 μg/ml) present in multiple purpose contact lens solution may not be able to kill all Acanthamoeba species which may be one of the reasons for predominance of AK in contact lens wearers.
The anti-acanthamoebic activity of pentamidine isethionate, in the current study, varied from MIC of 25 to 100 μg/ml and MCC of 100 to 166.7 μg/ml. The MICs of our isolates were higher than those reported earlier, ranging from 0.56 μg/ml in London [16] to 60 μg/ml in Australia [15]. The cysticidal activity of pentamidine isethionate, however, was in concordance with prior studies reporting MCC ranging from 64 to >128 μg/ml [15, 16, 18]. Pentamidine isethionate is clinically used at a cidal concentration of 0.01–0.02% [100–200 μg/ml [25] On toxicity assay analysis of our study, the highest cidal concentration of 166.7 μg/ml was found to be safe for use, however, the highest concentration tested (400 μg/ml) was safe at 24 h but produced >40% toxicity on prolonged exposure of 48 hr. This is in accordance with a study by Alizadeh et al. [30] wherein short term contact of pentamidine isethionate with cell cultures was found safe for use while prolonged exposure caused some damage to superficial epithelium.
Polymyxin B was observed to have MIC ranging from 25 to 100 μg/ml and MCC from 50 to 200 μg/ml. A single study [16] evaluating the in vitro susceptibility of polymyxin B as monotherapy, reported a trophozoite minimum amoebicidal concentration of 19.2 μg/ml and a much higher MCC of >500 μg/ml. These vast differences could possibly arise from differences in genotypes and the methodology employed for MCC. On cytotoxicity evaluation, while 200 μg/ml was found safe for HCEC cells, the highest tested concentration of 400 μg/ml produced unacceptable toxicity even at 24 h which increased by 48 h. The therapeutic dose for AK is 10,000–25,000 U/ml which corresponds to 1–2.5 mg/ml, and hence 1000–2500 μg/ml [31]. With no studies evaluating its corneal toxicity, extrapolating our results of polymyxin B toxicity make this therapeutic dose appear too toxic for use. Further studies are suggested to define the limits of toxicity for this antibacterial agent.
The MIC for miltefosine ranged from 64 to 256 μg/ml and MCC was 256 μg/ml for all in the present study. This is similar to the observations of Garajova et al. [32] who in their evaluation of four alkylphophocholines (miltefosine and its analogs) on two AK (A. castellanii) isolates observed the MIC to range from 26 to 256 μg/ml and MCC was >256 μg/ml. Similarly, Chao et al. [33] in their evaluation of in vitro cysticidal activity of miltefosine against three environmental Acanthamoeba isolates, documented MCC of 4.84 mM at day 7 of incubation [corresponding to 2 g/ml]. The ocular drops of miltefosine contain 65.12 μg/ml. While this concentration was found nontoxic [34] and our experiments have shown that a concentration of 128 μg/ml is also safe, the concentration of miltefosine in therapeutic solution may not kill all trophozoites of Acanthamoeba and any cyst at all. Mrva et al. [35] have also cautioned against the clinical efficacy of miltefosine owing to its insusceptibility against cyst forms. It is possible that the greater content of cellulose present in the cyst wall hampers activity of miltefosine [27].
Fluconazole, the last drug included in the present analysis, had MIC range from 64 to 256 μg/ml and MCC range from 256 to 512 μg/ml. This was in accordance with the results of prior two studies wherein MIC of fluconazole was reported to be >320 μg/ml [16] and >1024 μg/ml [36], while MCC was reported as >500 μg/ml [16] and >128 μg/ml [18]. While Hernández-Martínez et al. [37] reported higher in vitro susceptibility to voriconazole in their two A. castellaniii isolates from Mexican patients, Talbot et al. [38] did not find it cysticidal in any of their ten AK isolates (mean MCC > 10,000 μg/ml). Thus, therapeutic success of AK with fluconazole is questionable. All azoles, other than fluconazole, are lipophilic and hence are poorly absorbed in aqueous medium [39]. Azoles are used as 1% topical agent for fungal ocular infections and the same dosage is extended as anti-acanthamoebic treatment. This concentration is used to cover even those fungal agents that have high MIC for fluconazole. Previous studies, as reviewed by Lakhani et al. [39] have shown fluconazole to be minimally toxic to corneal epithelium even at high concentrations and fluconazole-loaded implants are also used for sustained and prolonged release of the drug. In our study also, minimal cytotoxicity was observed at the highest tested concentration of fluconazole.
Another observation made in the current study was that clinical strains had a general trend of higher MICs to all drugs except miltefosine than their environmental counterparts; especially for polymyxin B and fluconazole (even for MCC). It could be possible that the rampant use of these two drugs in clinical practice for their basic antibacterial and antifungal role, respectively made the clinical isolates less susceptible to them. Interestingly, in miltefosine MIC, reverse phenomenon was noticed i.e., environmental isolates had higher MICs for all the parameters tested than the clinical isolates. This could possible arise due to the conferring of cross-resistance by various phosphocholines and their ammonium derivatives that are used as cleaning agents and disinfectants, thus making the environmental isolates more resilient. The observation that A. lenticulata stains had higher MICs than A. castellanii irrespective of the source, can be explained by the fact that A. lenticulata belong to group III morphotype which have thicker wall [40] conferring protection against physical and chemical treatment.
The study has following limitations: only six isolates of Acanthamoeba could be evaluated for in vitro susceptibility. Though nine AK and four water isolates could be successfully cultured, only six out of these 13 could be properly axenized and revived for each experiment. Though our results can help ophthalmologists choose a suitable drug with least toxicity for AK treatment, such small sample size precludes any generalizations and warrants further evaluation in larger prospective studies. While studies on Acanthamoeba susceptibility have documented evaluation of a single drug [17] to as many as 31 drugs [18], we used only five that were more clinically relevant and represented all mechanisms of action. Lastly, longer incubation could have been carried out beyond 48 h to evaluate Acanthamoeba activity after the drug treatment.
To summarize, chlorhexidine was the most effective agent against our isolates having potent trophocidal and cysticidal activity with no toxic effects. The second best anti-Acanthamoebic agent was pentamidine isethionate with good activity and safety profile. To ensure optimal medical cure, a combination of the two could be used. Polymyxin B and fluconazole could be used a alternatives especially if concomitant coinfection with bacterial and fungal agents is suspected. However, dosage of polymyxin B appeared too toxic and may be replaced with some other antibacterial agent while fluconazole was well tolerated and could be used as sustained-release depots. Miltefosine had relatively higher MIC and MCC and the therapeutic dose was found insufficient to clear all the trophozoites and any of the cysts. Clinical isolates, in comparison to environmental isolates, had higher MICs for polymyxin B and fluconazole, and lower MICs for miltefosine. Among the clinical isolates, A. lenticulata had the highest MICs.
Summary
What was known before
-
Acanthamoeba keratitis, the corneal infection caused by Acanthamoeba, is a severe and potentially sight-threatening condition.
-
The treatment is largely empirical and there is an unmet need for evaluating drug susceptibility testing for local strains.
-
In vitro susceptibility testing of potential therapeutic agents against both trophozoite and cysts contribute to customized therapy for the patient of AK, thereby leading to favorable clinical outcomes.
What this study adds
-
Clinical as well as environmental isolates representing different genotypes of Acanthamoeba were evaluated for in vitro drug susceptibility testing using six different parameters (6 hr – MMIC, 24-hr & 48-hr MIC50 and MIC90, and MCC) against five drugs along with cytotoxicity assay on human corneal epithelial cells. Chlorhexidine and pentamidine isethionate were the most effective and safe agents against both trophozoites and cysts forms of our Acanthamoeba isolates.
-
Fluconazole had higher MIC but was non-toxic.
-
Polymyxin B was effective at high MIC but therapeutic dose was found toxic.
-
Miltefosine, at tested concentrations, could not inhibit cysts of Acanthamoeba.
References
Szentmary N, Daas L, Shi L, Laurik KL, Lepper S, Milioti G, et al. Acanthamoeba keratitis—clinical signs, differential diagnosis and treatment. J Curr Ophthalmol. 2018;31:16–23. https://doi.org/10.1016/j.joco.2018.09.008.
Hammersmith KM. Diagnosis and management of Acanthamoeba keratitis. Curr Opin Ophthal. 2006;17:327–31.
US Department of Health and Human Services. Acanthamoeba keratitis associated with contact lenses-United States. MMWR Morb Mortal Wkly Rep. 1986;35:405–8. https://doi.org/10.1097/00004397-199400000-00009.
Buerano CC, Trinidad AD, Fajardo LSN, Cua IY, Baclig MO, Natividad FF. Isolation of Acanthamoeba genotype T4 from a non-contact lens wearer from the Philippines. Trop Med Health. 2014;42:145–7. https://doi.org/10.2149/tmh.2014-15.
Garg P, Kalra P, Joseph J. Non-contact lens related Acanthamoeba keratitis. Indian J Ophthalmol. 2017;65:1079–86. https://doi.org/10.4103/ijo.IJO.
Tawfeek GM, Bishara SA, Sarhan RM, ElShabrawi T, ElSaady K. Genotypic, physiological, and biochemical characterization of potentially pathogenic Acanthamoeba isolated from the environment in Cairo, Egypt. Parasitol Res. 2016;115:1871–81. https://doi.org/10.1007/s00436-016-4927-3.
Sharma DP, Sharma S, Wilkins MR. Microbial keratitis after corneal laser refractive surgery. Future Microbiol. 2011;6:819–31. https://doi.org/10.2217/fmb.11.61.
Cristina S, Cristina V, Mihaela P. Acanthamoeba keratitis challenges a case report. Rom J Ophthalmol. 2016;60:40–2.
Juárez MM, Tártara LI, Cid AG, Real JP, Bermúdez JM, Rajal VB. Acanthamoeba in the eye, can the parasite hide even more? Latest developments on the disease. Contact Lens Anterior Eye. 2018;41:245–51. https://doi.org/10.1016/j.clae.2017.12.017.
Villani E, Baudouin C, Efron N, Hamrah P, Kojima T, Patel SV, et al. In vivo confocal microscopy of the ocular surface: from bench to bedside. Curr Eye Res. 2014;39:213–31. https://doi.org/10.3109/02713683.2013.842592.
Lorenzo-morales J, Khan NA, Walochnik J. An update on Acanthamoeba keratitis: diagnosis, pathogenesis and treatment. Parasite. 2015;22:1–20. https://doi.org/10.1051/parasite/2015010.
Schroeder JM, Booton GC, Hay J, Niszl IA, Seal DV, Markus MB, et al. Use of subgenic 18S ribosomal DNA PCR and sequencing for genus and genotype identification of Acanthamoebae from humans with keratitis and from sewage sludge. J Clin Microbiol. 2001;39:1903–11. https://doi.org/10.1128/JCM.39.5.1903.
Carrijo-carvalho LC, Peracini V, Foronda AS, De Freitas D, Ramos F, Carvalho DS. Therapeutic agents and biocides for ocular infections by free-living amoebae of Acanthamoeba genus. Surv Ophthalmol. 2016;62:203–18. https://doi.org/10.1016/j.survophthal.2016.10.009.
Baltaza W, Padzik M, Szaflik JP, Perkowski K, Dybicz M, Chomicz L. Evaluation of in vitro effects of selected physical and chemical agents on detected in Poland Acanthamoeba strains—factors of increasing threats for public health. Anal Parasitol. 2019;65:19–25. https://doi.org/10.17420/ap6501.179.
Lim L, Coster DJ, Badenoch PR. Antimicrobial susceptibility of 19 Australian corneal isolates of Acanthamoeba. Clin Exp Ophthalmol. 2000;28:119–24.
Elder MJ, Kilvingtonj MJES, Dart KG. A clinicopathologic study of in vitro sensitivity testing and Acanthamoeba keratitis. Investig Ophthalmol Vis Sci. 1994;35:1059–64.
Ortega-rivas A, Padrón JM, Valladares B, Elsheikha HM. Acanthamoeba castellaniii: a new high-throughput method for drug screening in vitro. Acta Trop. 2016;164:95–9. https://doi.org/10.1016/j.actatropica.2016.09.006.
Osato MS, Robinson NM, Wilhelmus KR, Jones DB. In vitro evaluation of antimicrobial compounds for cysticidal activity against Acanthamoeba. Rev Infect Dis. 1991;13 Suppl 5:S431–5.
Narasimhan S, Madhavan HN, Therese KL. Development and application of an in vitro susceptibility test for Acanthamoeba species isolated from keratitis to polyhexamethylene biguanide and chlorhexidine. Cornea. 2002;21:203–5.
Megha K, Sehgal R, Khurana S. Genotyping of Acanthamoeba spp. isolated from patients with granulomatous amoebic encephalitis. Indian J Med Res. 2018;148:456–9. https://doi.org/10.4103/ijmr.IJMR.
Khurana S, Biswal M, Kaur H, Malhotra P, Arora P, Megha K, et al. Free living amoebae in water sources of critical units in a tertiary care hospital in India. Indian J Med Microbiol. 2015;33:343–8. https://doi.org/10.4103/0255-0857.158543.
Megha K, Gupta A, Sehgal R, Khurana S. An improvised medium for axenic cultivation of Acanthamoeba spp. Indian J Med Microbiol. 2017;35:597–9. https://doi.org/10.4103/ijmm.IJMM.
Duma RJ, Finley R. In vitro susceptibility of pathogenic Naegleria and Acanthamoeba species to a variety of therapeutic agents. Antimicrob Agents Chemother. 1976;10:370–6. https://doi.org/10.1128/AAC.10.2.370.
van Goethem F, Adriaens E, Alepee N, Straube F, De Wever B, Cappadoro M, et al. Prevalidation of a new in vitro reconstituted human cornea model to assess the eye irritating potential of chemicals. Toxicol In Vitro. 2006;20:1–17. https://doi.org/10.1016/j.tiv.2005.05.002.
Siddiqui R, Aqeel Y, Khan A. The development of drugs against Acanthamoeba infections. Antimicrob Agents Chemother. 2016;60:6441–50. https://doi.org/10.1128/AAC.00686-16.Address.
Padzik M, Baltaza W, Conn DB, Szaflik JP, Chomicz L. Effect of povidone iodine, chlorhexidine digluconate and toyocamycin on amphizoic amoebic strains, infectious agents of Acanthamoeba keratitis—a growing threat to human health worldwide. Ann Agric Environ Med. 2018;25:725–31. https://doi.org/10.26444/aaem/99683.
Lloyd D. Encystment in Acanthamoeba castellaniii: a review. Exp Parasitol. 2014;145:S20–7. https://doi.org/10.1016/j.exppara.2014.03.026.
Perez-Santonja JJ, Kilvington S, Hughes R, Tufail A, Matheson M, Dart JKG. Persistently culture positive Acanthamoeba keratitis—in vivo resistance and in vitro sensitivity. Ophthalmology. 2003;110:1593–600. https://doi.org/10.1016/S0161-6420(03)00481-0.
Fernández-Ferreiro A, Santiago-Varela M, Gil-Martínez M, González-Barcia M, Luaces-Rodríguez A, Díaz-Tome V, et al. In vitro evaluation of the ophthalmic toxicity profile of chlorhexidine and propamidine isethionate eye drops. J Ocul Pharmacol Ther. 2017;33:202–9. https://doi.org/10.1089/jop.2016.0053.
Alizadeh H, Silvany R, Meyer D, Dougherty J, McCulley J. In vitro amoebicidal activity of propamidine and pentamidine isethionate against Acanthamoeba species and toxicity to corneal tissues. Cornea. 1997;16:94–100.
Humphrey JH, Lightbown JW, Mussett MV. The International Standard for polymyxin B. Bull Wld Hlth Org. 1959;20:1229–32.
Garajova M, Mrva M, Timko L, Lukac M, Ondriska F. Cytomorphological changes and susceptibility of clinical isolates of Acanthamoeba spp. to heterocyclic alkylphosphocholines. Exp Parasitol. 2014;145 Suppl:S102–10. https://doi.org/10.1016/j.exppara.2014.05.015.
Chao M, Thongseesuksai T, Boonmars T, Laummaunwai P. Investigation of the in vitro cysticidal activity of miltefosine against Acanthamoeba spp. J Parasit Dis. 2020;44:491–5. https://doi.org/10.1007/s12639-020-01204-w.
Polat ZA, Walochnik J, Obwaller A, Vural A. Miltefosine and polyhexamethylene biguanide: a new drug combination for the treatment of Acanthamoeba keratitis. Clin Exp Ophthalmol. 2014;42:151–8. https://doi.org/10.1111/ceo.12120.
Mrva AM, Garajová M, Luká M, Ondriska F, Ondriska FÀ, Sciences N. Weak cytotoxic activity of miltefosine against clinical isolates of Acanthamoeba spp weak cytotoxic activity of miltefosine against clinical isolates of Acanthamoeba spp. J Parasitol. 2011;97:538–40. https://doi.org/10.1645/GE-2669.1.
Nakaminami H, Tanuma K, Yoshimura Y, Onuki T, Nihonyanagi S, Hamada Y, et al. Evaluation of in vitro antiamoebic activity of antimicrobial agents against clinical Acanthamoeba isolates. J Ocul Pharmacol Ther. 2017;33:629–34. https://doi.org/10.1089/jop.2017.0033.
Hernández-Martínez D, Reyes-Batlle M, Castelan-Ramírez I, Hernández-Olmos P, Vanzzini-Zago V, Ramírez-Flores E, et al. Evaluation of the sensitivity to chlorhexidine, voriconazole and itraconazole of T4 genotype Acanthamoeba isolated from Mexico. Exp Parasitol. 2019;197:29–35. https://doi.org/10.1016/j.exppara.2019.01.006.
Talbott M, Cevallos V, Chen MC, Chin SA, Lalitha P, Seitzman GD, et al. Synergy testing of antiamoebic agents for Acanthamoeba: antagonistic effect of voriconazole. Cornea. 2019;38:1309–13. https://doi.org/10.1097/ICO.0000000000002055.
Lakhani P, Patil A, Majumdar S. Challenges in the polyene- and azole-based pharmacotherapy of ocular fungal infections. J Ocul Pharmacol Ther. 2019;35:6–22. https://doi.org/10.1089/jop.2018.0089.
Pussard M, Pons R. Morphologie de la paroi kystique et taxonomie du genre Acanthamoeba (Protozoa, Amoebida). Protistologica. 1977;13:557–98.
Funding
This work was financially supported by Indian council of Medical Research grant number vide no. 5/3/3/33/2013-ECD-I.
Author information
Authors and Affiliations
Contributions
Conceptualization: SK, AG, data curation: KM, AG, and CS, experiments: KM, CS, analysis: MS, KM, and SK, draft preparation: MS, KM, revision and editing: KM, MS, and SK, and study supervision: SK, RS.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Megha, K., Sharma, M., Sharma, C. et al. Evaluation of in vitro activity of five antimicrobial agents on Acanthamoeba isolates and their toxicity on human corneal epithelium. Eye 36, 1911–1917 (2022). https://doi.org/10.1038/s41433-021-01768-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01768-8