Abstract
Objective
To describe the role of local anaesthetic blocks as a potential cause of paracentral acute middle maculopathy (PAMM) after uneventful ocular surgery.
Methods
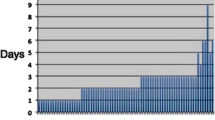
Retrospective, observational, international, multicentre case series. Nine cases of PAMM with associated visual loss following uneventful ocular surgery with local anaesthetic blocks were observed in a 9-year period (2011–2020). Demographic, ocular and systemic data, anaesthetic data and surgical details were collected. Visual acuity (VA), fundus photography, fluorescein angiography, optical coherence tomography (OCT) and optical coherence tomography angiography (OCTA) images were reviewed.
Results
All nine cases were associated with decreased VA at 24 h postoperative check (ranging from hand movement to 20/200). A hyperreflective band within the middle retinal layers was observed in the structural OCT in the acute phase, evolving to thinning and atrophy of the inner retinal layers in sequential follow-up scans performed. Fluorescein angiography showed delayed perfusion in early arterial phase with normal perfusion in late venous phases. OCTA showed decreased perfusion in the deep capillary plexus. Visual recovery was variable between cases during follow-up (ranging from count fingers to 20/20).
Conclusions
A combination of a vasoconstrictive effect of the anaesthetic agent, an intraocular pressure spike and a mechanical effect of the volume of anaesthetic injected may result in decreased retinal artery perfusion and be evidenced as PAMM in OCT scans. PAMM may present as a potential complication of local anaesthetic blocks in cases of unexpected visual loss after uneventful ocular surgery.
Similar content being viewed by others
Introduction
Paracentral acute middle maculopathy (PAMM) is an optical coherence tomography (OCT) finding defined as a band-like hyperreflective lesion mostly confined to the inner nuclear layer (INL) owing to ischaemia or infarction of the intermediate and deep retinal capillary plexus [1,2,3]. Several retinal diseases have been associated with this finding, including retinal vascular occlusive disorders such as branch or central retinal arterial occlusions (RAO), cilioretinal artery occlusion, central retinal vein occlusion (RVO), and systemic diseases such as diabetic retinopathy, hypertensive retinopathy, Purtscher retinopathy or sickle cell retinopathy [4, 5]. PAMM may be seen as an isolated finding or associated with other OCT features, including hyperreflectivity of the superficial retinal layers (retinal nerve fibre layer -RNFL-, ganglion cell layer -GCL- and Inner plexiform layer -IPL-) in RAO or diffuse thickening and macular oedema in RVO.
Local anaesthetics (sub-Tenon, peribulbar and retrobulbar) have been employed in ocular procedures for decades, and although these techniques are widely used, they are not free of complications. Well-known risks include intraorbital haemorrhage, local toxicity and, in worst case-scenarios, ocular perforation. The presence of impaired blood flow in the optic nerve head and therefore the retina has also been reported. Small case series and case reports describing retinal artery occlusions following cataract or pterygium surgery under local anaesthesia have been reported, using retrobulbar, peribulbar or sub-Tenon’s techniques [6,7,8,9,10,11,12]. Whereas in some clinical presentations these features are obvious, sometimes the fundus phenotype is more subtle and alterations can easily be overlooked in fundoscopy, and in certain cases, even in OCT images.
With this aim, we hereby describe the clinical phenotypes of a series of cases of PAMM and unexpected postoperative visual loss after uneventful ocular surgery with local anaesthetic blocks. The detailed ocular and systemic clinical characteristics of these cases are described as an attempt to share this data with the ophthalmic community, in order to identify future potential relationships between these preoperative features and PAMM which could help predict this postoperative complication.
Methods
Nine cases of PAMM following local anaesthetic blocks were observed in four medical centres, three in Spain (Hospital Clínic of Barcelona, Hospital la Arruzafa of Córdoba and Hospital Povisa of Vigo) and one in the United Kingdom (Moorfields Eye Hospital, London). Data collection was systematically performed retrospectively from clinical records produced during routine clinical care. Demographics and systemic data, including cardiovascular data and medications used were collected from all study centres. Ocular data included axial length and refraction. Details of the anaesthetic procedures included type of local anaesthesia, (sub-Tenon’s, peribulbar or retrobulbar), dose and volume of anaesthesia administered, and surgical details were collected from surgical logbooks. Visual acuity (VA), fundus photography, fluorescein angiography (FA), OCT, Spectral Domain OCT (SD-OCT) and optical coherence tomography angiography (OCTA) images, when possible, were reviewed. When appropriate, electrodiagnostic tests (EDDs) were performed at physician discretion. This study was approved by the institutional review board at Hospital Clínic (Comité Ético de Investigación Médica, CEIM) and was conducted in accordance with the Declaration of Helsinki.
Results
Baseline characteristics
Nine cases developed PAMM (seven men, two women, age range 40–83 years) with associated severe vision loss immediately after uneventful ocular surgery in a 9-year period (2011–2020). Indications for surgery were cataract (66.6%, 6/9) or pterygium surgery (33.3%, 3/9), performed under local anaesthesia of different types (peribulbar 66.6%, 6/9; retrobulbar, 22.2%, 2/9; Sub-Tenon’s, 11.1%, 1/9). No optic nerve injury or globe perforation was derived from retrobulbar or peribulbar blocks in any of these cases. Five patients presented typical findings of CRAO (55.5%, 5/9), but in the rest of cases, ischaemic damage to the retina was subtle in fundoscopy and diagnosis was made by structural OCT examination (44.4%, 4/9). In all cases, macular OCT images obtained 24-h after surgery revealed a hyperreflective band at the level of the inner retinal layers (from inner nuclear layer -INL- to outer plexiform layer -OPL-) sparing the outer retina, consistent with the diagnosis of PAMM. Optic nerve head OCT images were also obtained and showed no additional findings. Sequential SD-OCT (Cirrus HD-OCT, Carl Zeiss Meditec Inc, Dublin, CA, USA) images captured during follow-up showed progressive thinning of the inner retinal layers. In two cases, VA improved after presentation (22.2%, 2/9), whereas in 7 out of 9 cases vision alteration was permanent (77.7%, 7/9). The details of each individual case are described below. Demographics and clinical characteristics of cases included in the series are summarized in Table 1.
Case 1
A 40-year-old man underwent uneventful pterygium surgery in his right eye (OD) under sub-Tenon’s block (2% lidocaine). No significant past medical history (PMH) was described. Twenty-four h after the procedure, the patient complained of a central scotoma and VA was 20/200. Fundoscopy revealed a subtle perifoveal yellowish halo with thinning of the retinal vessels in the macular region (Fig. 1). FA showed a delayed arterial filling in the macular bundle, with normal perfusion in the late phase. SD-OCT images (Spectralis, Heidelberg Engineering, Heidelberg, Germany) revealed a hyperreflective band at the level of INL, consistent with the diagnosis of PAMM. EDDs tests showed OD marked macular dysfunction without generalized retinal dysfunction. Conservative management was indicated, and six weeks after the procedure OD VA improved to 20/32, with persistence of the hyperreflective band, thinning of the inner retinal layers and moderate macular atrophy in the SD-OCT scan.
Paracentral Acute Middle Maculopathy (PAMM) is seen in the OD of a 40-year-old man 24 h after uneventful pterygium surgery with sub-Tenon’s block of lignocaine 2%, presenting with central scotoma and decreased visual acuity (3/60). Colour fundus photographs of both eyes. In the OD, a subtle perifoveal yellowish halo with a very subtle thinning of the retinal vessels is seen in the macular region, whereas OS fundoscopy is unremarkable (a, b). Fundus fluorescein angiography revealed a delayed arterial filling in the macular bundle of the OD in the early arterial phase (c), with normal perfusion in the late phase (d). Spectral Domain Optical Coherence Tomography (SD-OCT) shows normal reflectivity of inner retinal layers in the OS (e). A hyperreflective band in the inner retinal layers is observed in the OD, consistent with the diagnosis of PAMM (f). Six weeks after the surgery, SD-OCT reveals thinning of the inner retinal layers, with persistence of the hyperreflective band and moderate macular atrophy in the SD-OCT retinal scan (g).
Case 2
An 82-year-old man with an OD preoperative VA of 20/50 underwent an uneventful phacoemulsification surgery under retrobulbar block (4 mL of a mixture of bupivacaine 0.75%, lidocaine 5% and hyaluronidase 150 IU). Significant PMH included hypertension and atrial fibrillation on anticoagulant treatment. In the 24-h postoperative check, he complained of central scotoma and VA was 20/200. Funduscopy showed a cherry red spot with whitening of the perifoveal region consistent with the diagnosis of CRAO. OCT scans revealed a hyperreflective band in the inner retinal layers. After 6 months of follow-up, VA was light perception (LP) and OCT scans confirmed a progressive retinal and optic nerve atrophy.
Case 3
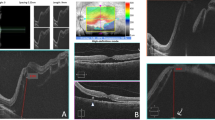
An 80-year-old woman with an OD preoperative VA of 20/50 underwent an uneventful phacoemulsification surgery under peribulbar block in her OD (6 mL of a mixture of lidocaine 1%, bupivacaine 0.5% and hyaluronidase 150 IU). Significant PMH included diabetes mellitus, HTA, hypercholesterolaemia, hypothyroidism, a history of coronary bypass and peripheral vascular disease, on treatment with antiplatelet drugs which were discontinued 3 days prior to the surgery. The day after the surgery she presented with a VA of hand movement (HM). Fundoscopy revealed a cherry red spot with whitening of the perifoveal region (Fig. 2), compatible with diagnosis of CRAO. A hyperreflective band in INL was present in the SD-OCT scan, consistent with the finding of PAMM. FA performed after 48 h confirmed delayed perfusion of the macular region. Sequential follow-up SD-OCT scans showed progressive thinning of middle retinal layers and macular atrophy. Final VA in the OD was count fingers (CF).
Paracentral Acute Middle Maculopathy (PAMM) associated to Central Retinal Artery Occlusion (CRAO) in the OD of an 80-year-old woman with pre-existing cardiovascular disease after uneventful phacoemulsification. Colour fundus photographs of the OD (a) and the OS (b) of the patient 24 h after the surgery in the OD. The presence of a cherry red spot with whitening of the perifoveal region and a perfused optic disc is seen in the OD (a). Spectral domain optical coherence tomography (SD-OCT) 24 h post-surgery (c, d). A hyperreflective band is seen in the inner retinal layers of the OD (c), in contrast with the normal reflectivity observed in the OS (d). Sequential follow up SD-OCT scans were performed in the next 2–8 weeks (e: 2 weeks, g: 4 weeks, f: 6 weeks, h: 8 weeks), which showed progressive thinning of the inner retinal layers and macular atrophy 2 months after the surgery.
Case 4
A 49-year-old man with preoperative VA of 20/20 in both eyes underwent an uneventful OD pterygium surgery under retrobulbar block (2.5 mL of a mixture of lidocaine 2% and bupivacaine 0.75%). No significant PMH was described. On day 1 he complained of decreased vision, VA was 20/200 and fundoscopy revealed whitening of the perifoveal region. SD-OCT images revealed an OD hyperreflective band in INL consistent with the diagnosis of PAMM. FA reported no ischaemia nor oedema. Carotid doppler ultrasonography and blood tests for prothrombotic factors were performed, resulting all within normal limits. Sequential follow-up SD-OCT scans showed progressive atrophy in INL and final VA was 20/200.
Case 5
An 83-year-old man with OD preoperative VA of 20/200 underwent an uneventful phacoemulsification surgery under peribulbar block (4 mL of a mixture of bupivacaine 0.75% and lidocaine 2%). Significant PMH included hypertension, myocardial infarction and hypercholesterolaemia. At the moment of the surgery, he was on antiplatelet, anticoagulant and on tamsulosin treatment. On the first postoperative review 24 h after the surgery VA was HM. Fundoscopy revealed a cherry red spot with whitening of the perifoveal region. A diagnosis of CRAO was made and SD-OCT revealed a hyperreflective band in INL consistent with PAMM. FA showed delayed arterial filling in the macular bundle in early phases with normal perfusion in late phases. Sequential follow-up SD-OCT scans showed progressive inner nuclear retinal atrophy layers and macular atrophy. Final VA was CF with residual permanent central scotoma.
Case 6
A 55-year-old male underwent an uneventful OD refractive phacoemulsification surgery under peribulbar block (4 mL of a mixture of bupivacaine 0.75% and lidocaine 2%). No significant PMH was described and preoperative VA was 20/20. On the first postoperative review 24 h after the surgery the patient complained of central scotoma and VA was 20/50. Fundoscopy was apparently normal so an SD-OCT scan was performed revealing a hyperreflective band in the INL. Sequential follow-up SD-OCT showed persistence of the hyperreflective band, thinning of middle retinal layers and moderate macular atrophy. OCTA performed 1 month after surgery showed decreased small vessel branching of the deep capillary plexus in the OD compared to the fellow eye. After six weeks of follow-up, VA was 20/20 but complained of mild decreased vision.
Case 7
An 83-year-old woman with an OD preoperative VA of 20/100 underwent an uneventful phacoemulsification surgery under peribulbar block (6 mL of a mixture of bupivacaine 0.75%, mepivacaine 2% and hyaluronidase 150 IU). Significant PMH included hypertension, acute myocardial infarction, chronic kidney failure, chronic myelocytic leukaemia, essential tremor and previous thyroidectomy and colostomy. At the moment of surgery, she was on antiplatelet treatment and bisoprolol. On the 24-h postoperative review, OD VA was 20/200 and fundoscopy revealed a subtle whitish perifoveal halo in the papillomacular bundle, with spared perfusion of the cilioretinal artery. OCT-A (SS-OCTA, Atlantis DRI, Topcon Corp, Japan) was performed revealing a markedly decreased small vessel branching of the deep capillary plexus in the OD compared to the normal left eye (OS) (Fig. 3). A hyperreflective band in the OD INL was observed in structural OCT scans. Five months after surgery, OD VA was 20/100 with a residual paracentral scotoma.
Paracentral Acute Middle Maculopathy (PAMM) in the OD of an 83-year-old woman 24 h after routine phacoemulsification under peribulbar anaesthesia. Colour fundus photographs of the OD 24 h after the surgery (a). A subtle whitish perifoveal halo is seen in the OD papillomacular bundle, with spared perfusion of the cilioretinal artery. Swept source optical coherence tomography angiography (SS-OCTA, Atlantis DRI, Topcon Corp, Japan) of the deep capillary plexus of the right eye (b) and the left eye (c) 24 h post-surgery, with the corresponding segmentation slabs inferiorly. Note a marked decrease in the small vessel branching of the PAMM-affected right eye compared to the unaffected left eye. Swept source optical coherence tomography (SS-OCT, Atlantis DRI, Topcon Corp, Japan) of the OD revealing a hyperreflective band in the inner retinal layers (d) in contrast with the normal reflectivity observed in the OS (e).
Case 8
A 53-year-old male underwent an uneventful OD pterygium surgery under peribulbar block (4 mL of a mixture of bupivacaine 0.75% + lidocaine 5% + hyaluronidase 150 IU). Preoperative OD VA was 20/20 with no remarkable PMH. The day after the surgery he complained of central scotoma and VA was reduced to 20/200. Fundoscopy revealed a cherry red spot in the OD. SD-OCT revealed a hyperreflective band in the INL consistent with the diagnosis of PAMM. Final VA was 20/200 with a residual permanent central scotoma. Sequential OCT scans showed progressive retinal atrophy over 3 months follow-up visits.
Case 9
A 68-year-old woman with an OS preoperative VA of 20/50 underwent an uneventful phacoemulsification surgery under peribulbar block (5 mL of mepivacaine 2%). Significant PMH included hypertension, diabetes mellitus, hypercholesterolaemia and arrhythmia (pacemaker carrier). At the moment of the surgery, she was on antiplatelet treatment with acetylsalicylic acid (100 mg OD PO), atorvastatin, insulin and amiodarone. On the first postoperative review 24 h after the surgery, OS VA was HM and the patient complained of no vision. Fundoscopy revealed a cherry red spot and OCT showed a hyperreflective band in the middle retinal layers. Moderate improvements in OS VA were observed during follow-up, resulting in a final VA of 20/200, a permanent central scotoma and macular atrophy on OCT scans.
Discussion
Unexpected postoperative severe visual loss after uneventful ocular surgery represents a rare but important concern for both the patient and the treating ophthalmologist. Postoperative retinal arterial occlusions after local anaesthesia may present with a broad spectrum of clinical patterns, from typical findings to very subtle alterations only apparent by structural OCT. This paper highlights the possible relationship between local anaesthetic blocks as a potential trigger for impaired foveal perfusion, resulting in a PAMM presentation pattern in structural OCT scans. A detailed description of preoperative clinical characteristics is presented to the ophthalmic community, as an attempt to identify predictive features in future studies to avoid this complication.
Different types of local anaesthesia (sub-Tenon’s, peribulbar or retrobulbar) are routinely used to carry out ocular surgeries, albeit with some potential side effects [13]. From the local complications perspective, traditional needle blocks such as retrobulbar and peribulbar provide good analgesia and akinesia but can cause serious sight threatening complications including globe or optic nerve perforation [14]. Sub-Tenon’s block appears as a safer anaesthetic technique for ocular procedures, providing good analgesia and akinesia without the risks derived from sharp needle use [15]. From the systemic complications perspective, peribulbar and retrobulbar blocks can cause major complications in cases of inadvertent injection through the optic nerve sheath such as brainstem anaesthesia, unconsciousness, severe cardiorespiratory collapse and even death [14, 16]. Cardiovascular events have also been associated to sub-Tenon’s block in some reports [15].
Retinal artery occlusions related to peribulbar and Sub-Tenon’s blocks have been described in several publications [7,8,9,10,11,12]. Since the initial description of PAMM as a manifestation of retinal capillary ischaemia [2], multiple series have associated this entity with several retinal vascular and systemic disorders [4]. The lack of adequate perfusion in the deep capillary plexus (DCP) seems to be the main cause of PAMM, as assessed by OCTA findings [3, 17, 18]. The deep capillary system is composed of an intermediate capillary plexus (ICP) and a deep capillary plexus (DCP). Anatomically, it is conceivable that the INL may receive its blood supply predominantly from the proximal ICP, whereas the OPL may receive its blood supply predominantly from the DCP [3]. The oxygen demand of the macula, especially at the level of the OPL and photoreceptor inner segments, is higher than any other region of the retina [19]. Furthermore, oxygen diffusion from the choroid to the retina is inherently limited by retinal thickness, which becomes greater parafoveally [3]. Taken together, the middle layers of the retina (INL and OPL) in the parafoveal region have a high-perfusion demand whose supply is limited by anatomical configuration, making these structures most vulnerable to ischaemia [3].
Recent reports have been directed to study the pathophysiology of retinal vascular occlusive disease [3]. Although retinal arterial occlusion can cause total inner retinal ischaemia involving all three plexuses, isolated PAMM lesions may appear as a result of preferential ICP and DCP ischaemia. In clinical practice, this means that the transient occlusion of a large retinal arteriole with rapid restoration of normal flow could induce ischaemia in the deep stratus of the middle retina, while sparing the retinal nerve fibre and ganglion cell layers presenting as isolated PAMM. We believe that this theory may help to explain the subtle clinical pictures presented by four of our patients, with minimal clinical findings of arterial hypoperfusion on direct funduscopy examinations.
After a systematic literature review on potential causative mechanisms for CRAO or transient retinal artery occlusion (TRAO) after routine intraocular procedures, we suggest three hypotheses for this PAMM phenomenon observed in this series and other preliminary reports [9, 10, 12]. First, a vasoconstrictive effect of the anaesthetic agent on the central retinal artery, second, an intraocular pressure spike resulting in decreased retinal artery perfusion and, third, a mechanical effect of the volume of anaesthetic injected in the orbit compressing the optic nerve and the central retinal artery (a sort of transient acute orbital compartment syndrome-like process). Several publications addressing the effect of local anaesthesia on ocular haemodynamic have confirmed a decreased ocular blood flow during the procedure, even without vasoconstrictors [20,21,22]. These flow reductions were still present 5 min after peribulbar anaesthesia, when intraocular pressure returned to baseline values, supporting the theory of drug-induced vasoconstriction after peribulbar anaesthesia [22]. This vasoconstriction may relate to the anaesthetic drugs themselves, as bupivacaine or lidocaine have been reported to cause temporary reduction in the blood flow of the central retinal artery [22]. In our series, 8/9 cases received at least one of these two anaesthetic drugs, with a single case receiving only mepivacaine. None of the anaesthetic block mixtures included adrenalin or similar vasoconstrictive agents, commonly used in other local procedures elsewhere in the body. With regards to the possibility of an inadvertent intraoperative IOP spike, although it cannot be excluded, all surgeries were performed at normal infusion parameters in the phacoemulsification procedures, no particular findings were reported in pterygium surgical notes by any of the surgeons and IOP was normal at the 24 h postoperative check in all nine cases. Finally, local anaesthetic blocks imply injecting a certain volume of fluid into a non-expansible compartment, and consequently, an increase of pressure in the orbit. Therefore, the injection of anaesthetics into the connective tissue surrounding the optic nerve might cause a temporary compression of the central retinal artery, resulting in a transient hypoperfusion to the retinal vasculature. In our series, the anaesthetic volume injected was similar in all cases (ranging from 2.5 to 6 mL), as was the axial length of study eyes (ranging from 23.02 to 23.76 mm). We believe that all these three situations may not have been exclusive, and a combination of them may have played a role in our patients resulting in retinal ischaemia presenting as PAMM.
We should bear in mind that PAMM is an OCT abnormality that may herald the presence of an underlying systemic condition, as it has been associated to several retinal vascular occlusive disorders [3, 4]. It is possible that patients with underlying cardiovascular pathologies could be more susceptible to transient compression or spasm on the retinal arterial circulation. Five of the patients included in our series had previously diagnosed cardiovascular diseases, but the rest had no previous relevant medical history which may indicate that these disorders might be a predisposing factor, but not a necessary condition for developing PAMM.
As in other surgical complication report studies, our series has limitations, as the relatively small number of cases and the retrospective design. Unfortunately, most of the cases were observed prior to the advent of OCTA. OCTA is the only image modality that can address the loss and extension of capillary perfusion specifically in the deep capillary plexus, the main stratus affected in this condition. Given its non-invasive nature, we would recommend performing OCTA imaging in all patients with unexplained visual loss in the early postoperative period after cataract surgery.
In conclusion, PAMM may appear secondary to local anaesthetic blocks in a broad spectrum of retinal hypoperfusion presentations, associating unexpected postoperative vision loss after uneventful ocular surgery. Increasing the awareness of this complication would lead physicians to perform OCT investigations in such cases, as no robust data are present in the literature about the incidence or prevalence of this OCT finding at the present time, and this condition may be underreported due to the absence of fundoscopic findings in the more subtle cases. Until potential risk factors for this complication are identified, an empiric alternative would be to recommend topical or intracameral anaesthesia when possible in patients with known underlying vasculopathy. Future studies with larger study populations will provide new insights to identify such predictive features and inform us for better counselling in patient-doctor discussions.
Summary
What was known before
-
Paracentral acute middle maculopathy (PAMM) is an optical coherence tomography finding associated with different retinal vascular occlusive disorders.
-
Periocular anaesthesia has been associated to vascular occlusive retinal disorders.
-
Preliminary data suggest that PAMM may be associated to periocular anaesthesia with vision loss in uneventful ocular surgery.
What this study adds
-
PAMM is presented as a common factor in a series of patients presenting with vision loss 24 h after uneventful ocular surgery performed with periocular anaesthesia.
-
Different mechanisms are proposed for the development of PAMM after anaesthetic blocks in ocular surgery.
-
This condition should be considered in patients presenting with patch-off scotoma or vision loss after uneventful ocular surgery.
References
Rahimy E, Sarraf D. Paracentral acute middle maculopathy spectral-domain optical coherence tomography feature of deep capillary ischemia. Curr Opin Ophthalmol. 2014;25:207–12.
Sarraf D, Rahimy E, Fawzi AA, Sohn E, Barbazetto I, Zacks DN, et al. Paracentral acute middle maculopathy a new variant of acute macular neuroretinopathy associated with retinal capillary ischemia. JAMA Ophthalmol. 2013;131:1275–87.
Rahimy E, Kuehlewein L, Sadda SR, Sarraf D. Paracentral acute middle maculopathy what we knew then and what we know now. Retina. 2015;35:1921–30.
Chen X, Rahimy E, Sergott RC, Nunes RP, Souza EC, Choudhry N, et al. Spectrum of retinal vascular diseases associated with paracentral acute middle maculopathy. Am J Ophthalmol. 2015;160:26–34.e1. https://doi.org/10.1016/j.ajo.2015.04.004. Available at
Pichi F, Fragiotta S, Freund KB, Au A, Lembo A, Nucci P, et al. Cilioretinal artery hypoperfusion and its association with paracentral acute middle maculopathy. Br J Ophthalmol. 2019;103:1137–45.
Feibel RM, Guyton DL. Transient central retinal artery occlusion after posterior sub-Tenon’s anesthesia. J Cataract Refract Surg. 2003;29:1821–4.
Vinerovsky A, Rath EZ, Rehany U, Rumelt S. Central retinal artery occlusion after peribulbar anesthesia. J Cataract Refract Surg. 2004;30:913–5.
Swamy BN, Merani R, Hunyor A. Central retinal artery occlusion after phacoemulsification. Retin Cases Br Rep. 2010;4:281–3.
Creese K, Ong D, Sandhu SS, Ware D, Alex Harper C, Al-Qureshi SH, et al. Paracentral acute middle maculopathy as a finding in patients with severe vision loss following phacoemulsification cataract surgery. Clin Exp Ophthalmol. 2017;45:598–605.
O’Day R, Harper CA, Wickremasinghe SS. Central retinal artery occlusion showing features of paracentral acute middle maculopathy following uncomplicated pterygium surgery. Clin Exp Ophthalmol. 2019;47:141–3. https://doi.org/10.1111/ceo.13353.
Dragnev D, Barr D, Kulshrestha M, Shanmugalingam S. A case of branch retinal artery occlusion following uneventful phacoemulsification. Case Rep. Ophthalmol 2013;4:27–31. https://www.karger.com/Article/FullText/348729 Available at
Pham C, Boo A, Chew SKH, Okada M. Paracentral acute middle maculopathy in a young patient following routine phacoemulsification surgery. Clin Exp Ophthalmol. 2019;47:1206–9. https://onlinelibrary.wiley.com/doi/abs/10.1111/ceo.13597 Available at
Sallam AAB, Donachie PHJ, Williamson TH, Sparrow JM, Johnston RL. The Royal College of Ophthalmologists’ National Ophthalmology Database Study of vitreoretinal surgery: Report 5, anaesthetic techniques. Br J Ophthalmol. 2016;100:246–52.
Hamilton RC. Retrobulbar block revisited and revised. J Cataract Refract Surg. 1996;22:1147–50. https://doi.org/10.1016/S0886-3350(96)80062-9.
Guise PA. Sub-tenon anesthesia. Anesthesiology. 2003;98:964–8.
Zhao LQ, Zhu H, Zhao PQ, Wu QR, Hu YQ. Topical anesthesia versus regional anesthesia for cataract surgery: A meta-analysis of randomized controlled trials. Ophthalmology. 2012;119:659–67.
Sridhar J, Shahlaee A, Rahimy E, Hong BK, Khan MA, Maguire JI, et al. Optical coherence tomography angiography and en face optical coherence tomography features of paracentral acute middle maculopathy. Am J Ophthalmol. 2015;160:1259–.e2. https://doi.org/10.1016/j.ajo.2015.09.016.
Pecen PE, Smith AG, Ehlers JP. Optical coherence tomography angiography of acute macular neuroretinopathy/paracentral acute middle maculopathy. JAMA Ophthalmol. 2015;133:1478–80.
Yu DY, Yu PK, Cringle SJ, Kang MH, Su EN. Functional and morphological characteristics of the retinal and choroidal vasculature. Prog Retin Eye Res. 2014;40:53–93. https://doi.org/10.1016/j.preteyeres.2014.02.001.
Watkins R, Beigi B, Yates M, Linardos E, Chang B. Intraocular pressure and pulsatile ocular blood flow after retrobulbar and peribulbar anaesthesia. Br J Ophthalmol. 2001;85:796–8.
Pianka P, Weintraub-Padova H, Lazar M, Geyer O. Effect of sub-Tenon’s and peribulbar anesthesia on intraocular pressure and ocular pulse amplitude. J Cataract Refract Surg. 2001;27:1221–6.
Findl O, Dallinger S, Menapace R, Rainer G, Georgopoulos M, Kiss B, et al. Effects of peribulbar anesthesia on ocular blood flow in patients undergoing cataract surgery. Am J Ophthalmol. 1999;127:645–9.
Funding / Support
JZ-V is a grant recipient of the Spanish Retina & Vitreous Society (Sociedad Española de Retina y Vítreo). This work was partly supported by the National Institute for Health Research Biomedical Research Centre based at Moorfields Eye Hospital National Health Service Foundation Trust and University College London Institute of Ophthalmology. The views expressed are those of the authors (PAK, DAS, AT) and not necessarily those of the National Health Service, the National Institutes for Health Research or the Department of Health.
Author information
Authors and Affiliations
Contributions
CBM, DVV, and JZV were responsible for conducting the search, writing the report, extracting and analyzing data, interpreting results, updating reference lists and creating’Summary of findings’ tables. JMCP, PAK, DAS, AA, and AT were responsible for conducting the search and provided feedback on the report.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Financial disclosures
CB-M, none; DV-V, none; JMC-P has been in advisory boards, has given lectures and has received travel grants from Alcon, Allergan, Bausch & Lomb, Bayer, DORC and Novartis and has been a lecturer for Novartis and Bausch & Lomb; PAK acts as a consultant for Novartis, Roche, Apellis, and DeepMind, he has received speaker fees from Allergan, Bayer, Topcon, and Heidelberg Engineering and has stocks in Big Picture Eye Health.; DAS no disclosures; AA has been in advisory boards for Abbvie and Novartis; AT has been in advisory boards and has given lectures for Allergan, Alimera Science, Bayer, Novartis and Roche, and has received grants from Medisoft Ltd, Notal Vision and Novartis; JZ-V has been in advisory boards, is a consultant, lecturer and has received travel grants from Alcon, Alimera Science, Allergan, Bausch & Lomb, Bayer, Brill Pharma, DORC, Novartis and Roche, is a grant holder from Allergan and Novartis, and has been a lecturer for Topcon and Zeiss
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bernal-Morales, C., Velazquez-Villoria, D., Cubero-Parra, J.M. et al. Paracentral acute middle maculopathy after uneventful ocular surgery with local anaesthetic blocks. Eye 36, 219–227 (2022). https://doi.org/10.1038/s41433-021-01481-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01481-6