Abstract
Objectives
To evaluate the efficacy of inner retinal fenestration as a surgical technique for the treatment of optic disc pit maculopathy (ODPM) in the paediatric population.
Methods
This is a retrospective, interventional case series of paediatric patients with ODPM treated at two tertiary hospitals in London by a single surgeon (SCW). All patients underwent pars plana vitrectomy with the creation of two inner retinal fenestrations and endogas tamponade. The partial-thickness retinotomies were made radial to the optic disc pit using a 25-gauge MVR blade. Anatomic and visual outcomes were determined by optical coherence tomography central retinal thickness and best-corrected visual acuity (BCVA), respectively.
Results
A total of six eyes were included. Average patient age was 12.0 ± 3.5 years. Preoperatively all eyes demonstrated intraretinal fluid and/or serous detachment of the central macula. Patients were followed for a mean of 22.7 ± 16.1 months after surgery. Mean preoperative BCVA was logMAR 0.71 ± 0.29 (20/100). Mean postoperative BCVA was 0.49 ± 0.30 (20/63) at 2 weeks, 0.35 ± 0.33 (20/45) at 3 months and 0.16 ± 0.29 (20/32) at 1 year. Progressive resolution of intraretinal and subretinal fluid (SRF) was observed in all eyes, with central retinal thickness significantly improved by 2 weeks postoperatively (637.83 ± 209.09 µm preoperatively and 465.40 ± 169.86 µm postoperatively, p = 0.04). Recurrence of subretinal or intraretinal fluid was not observed.
Conclusion
Dual inner retinal fenestration is an effective technique that resolves fluid and restores vision in paediatric patients with ODPM. These results support the hypothesis that enabling egress of fluid into the vitreous cavity can achieve long-lasting amelioration of ODPM.
Similar content being viewed by others
Introduction
Optic disc pits are congenital disc abnormalities secondary to a colobomatous malformation of the optic nerve head. They often appear as a solitary, oval, grey-white depression at the inferotemporal margin of the optic disc. A corresponding congenital loss retinal nerve fibre layer extending radially from the disc pit can be associated with visual field changes [1, 2]. Acquired vision loss can occur as a result of serous detachment of the macula, known as optic disc pit maculopathy (ODPM) [3].
ODPM commonly presents as a serous retinal detachment of the macula with or without intraretinal fluid accumulation or retinoschisis. While it can occur as early as 3 years of age and as late as the ninth decade of life, they are most frequently observed in early adulthood [4, 5]. There is commonly an accompanying funduscopic appearance mimicking retinoschisis [6]. Optical coherence tomography (OCT) of the macula demonstrates thickening and cystoid degeneration of the inner retina, along with SRF accumulation. These changes often occur in the nasal and central macula [7].
The source of the accumulating subretinal and intraretinal fluid continues to be debated. Lack of leakage on fluorescein angiography makes a breakdown of the blood-retina barrier or vascular source unlikely. Cerebrospinal fluid (CSF) from the peripapillary subarachnoid space is another possible origin. Some doubt this theory due to differences in hydrostatic pressure between the CSF and intraocular pressure, as well as the inability to displace the macular fluid back to the CSF [3]. Studies analysing the SRF aspirated at the time of surgery have conflicting results [8, 9]. Histopathologic analysis of a canine optic disc pit model suggests that there may be a connection between the vitreous and macular fluid [4]. This has not been demonstrated in humans. However, resolution of maculopathy following spontaneous posterior vitreous detachment (PVD) has been reported, which suggests the role of the vitreous in the pathophysiology of ODPM [10].
While this maculopathy can spontaneously resolve, the natural history of the disease process is variable. Apple et al. demonstrated visual acuity of 6/60 or worse in 80% of eyes [11]. A more recent UK national surveillance study showed that eyes with SRF were more likely to progress, had worse outcomes when observed and the best outcomes were seen with surgical intervention [5]. Multiple therapeutic approaches have been suggested to prevent permanent vision loss, including laser photocoagulation, intravitreal gas injection and pars plana vitrectomy with or without internal limiting membrane peel, endogas tamponade or endolaser [3, 12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27].
Then Spaide et al. described a novel surgical technique of a single inner retinal fenestration at the time of vitrectomy [28]. They theorised that fenestration could redirect flow and allow for an egress of fluid into the vitreous cavity, which may alleviate the accumulation of fluid. Subsequently, a case series of adult patients showed resolution in 94% of patients [29]. The purpose of this study was to determine the efficacy of inner retinal fenestrations for the treatment of ODPM in the paediatric population.
Materials and methods
This was a retrospective, interventional case series with institutional review board approval. The study adhered to the tenets of the Declaration of Helsinki. Paediatric patients treated at both Great Ormond Street Hospital and Moorfields Eye Hospital were included. All patients included underwent vitrectomy with inner retinal fenestrations. Cases were ascertained through a review of a single surgeon’s (SCW) medical records.
The diagnosis of ODPM was based on the presence of an optic disc pit in combination with intraretinal and/or SRF accumulation. All patients were evaluated with a complete ophthalmic examination including best-corrected visual acuity (BCVA). OCT was obtained for all patients at each visit before and after surgery (Spectralis SD-OCT, Heidelberg Engineering, Heidelberg, Germany).
Surgery was performed for persistent or worsening SRF associated with decreased visual acuity. All cases were performed by a single surgeon (SCW) between March 2015 and December 2018. Using 25-gauge vitrectomy, PVD and core vitrectomy were performed. Subsequently, two partial-thickness inner retinal fenestrations were created using a 25-gauge MVR blade. These fenestrations were made temporal to the optic disc pit, parallel to the papillomacular bundle. Fluid-air exchange with endogas tamponade was used in all cases. None of the eyes had internal limiting membrane peeling or peripapillary endolaser at the time of surgery.
Main outcomes included postoperative visual acuity and anatomical improvement on OCT. The Wilcoxon signed-rank test (SPSS, Version 23.0, IBM) was used to compare visual acuity and central retinal thickness (CRT) pre and post operatively. A qualitative analysis of serial OCT scans was also performed.
Results
Preoperative clinical characteristics are summarised in Table 1. A total of six eyes were included from six patients. Four patients were male. Mean patient age was 12.0 ± 3.5 years, with a range of 8–16 years. Patients were followed for a mean of 22.7 ± 16.1 months after surgery (range 6–48 months).
Preoperatively all eyes demonstrated subretinal and intraretinal fluid in the central macula on OCT, with the exception of one case where outer retinal schisis was present without SRF. All eyes had fluid accumulation or schisis of the outer retinal layers. In addition, four patients had fluid in the inner retinal layers. Macular detachment was observed in five of the six cases. None of the patients had PVD on exam or OCT.
In terms of the visual outcomes, mean preoperative BCVA was logarithm of the minimal angle of resolution (logMAR) 0.71 ± 0.29 (20/100), with a range of 0.3–1.0 (20/40–20/200). Mean postoperative BCVA was logMAR 0.49 ± 0.30 (20/70) at 2 weeks, 0.35 ± 0.33 (20/50) at 3 months, 0.26 ± 0.32 (20/40) at 6 months and 0.16 ± 0.29 (20/32) at 1 year (Fig. 1A). Visual acuity began to improve within the first postoperative month, even in the presence residual intraretinal fluid and macular detachment. Visual gains were significant at 3 months (p = 0.04), 6 months (p = 0.04) and 12 months (p = 0.04) postoperatively. The greatest visual gains were seen between 2 weeks (0.49 ± 0.30) and 3 months (0.35 ± 0.33) postoperatively (p = 0.04).
A This graph trends the mean best-corrected visual acuity with standard deviation from baseline to 12 months postoperatively. Visual acuity gains were statistically significant compared to baseline starting at 3 months postoperatively (p < 0.04). All statistically significant improvements in visual acuity are indicated with an asterisk. B This graph trends the mean OCT central retinal thickness and standard deviation from baseline to 12 months postoperatively. Statistically significant gains were seen as early as 2 weeks postoperatively (p < 0.04). All statistically significant changes in retinal thickness are indicated with an asterisk.
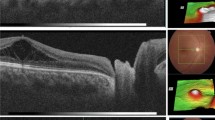
With regard to anatomical outcomes, progressive resolution of intraretinal and SRF was observed in all eyes (Fig. 1B). Mean preoperative OCT CRT was 637.83 ± 209.09 µm. Mean postoperative OCT CRT was 465.40 ± 169.86 µm at week 2, 362.75 ± 51.71 µm at month 3, 316.00 ± 33.43 µm at month 6 and 311.00 ± 40.36 µm at 1 year. The improvement in CRT was statistically significant by 2 weeks postoperatively (p = 0.04). Despite the immediate improvements in CRT, it required up to 6 months for a majority of fluid to resolve. Most patients required a minimum of 12 months for complete resolution of fluid (Fig. 2A, B). Recurrence of macular detachment or intraretinal fluid was not observed. None of the patients experienced any complications secondary to surgery, including cataract, retinal detachment or glaucoma.
A This figure includes pre- and postoperative OCT scans for all six cases with corresponding best-corrected visual acuity. These images demonstrate the progressive resolution fluid and improved visual acuity after vitrectomy with inner retinal fenestrations. B This figure utilises two example cases (Cases 2 and 6) to demonstrate the anatomic and visual improvement from baseline to the most recent postoperative visit.
Discussion
ODPM is a rare condition, and evidence for managing paediatric cases is limited to individual case reports. Previously, conservative management and observation was recommended for paediatric patients, as 25% of cases are reported to be resolved spontaneously [30]. However, long-standing SRF has recently been shown to have a poorer prognosis. It is suspected that the presence of SRF may lead to outer retinal atrophy, often resulting in poor visual outcomes [5]. Even when fluid spontaneously resolves, vision function (measured by BCVA, microperimetry, and electrodiagnostic testing) is not commonly restored [31,32,33].
This is the first paediatric-only case series to address the surgical management of ODPM. We chose to modify the original technique described by Spaide et al. and study the use of dual (rather than single) inner retinal fenestrations. With dual fenestrations we hoped to compensate for the more severe and typically more chronic clinical presentation seen in our paediatric patients, as well as greater healing response in children and thus potential closure of the fenestration. The results of our study demonstrate that this technique allows for fluid resolution and visual recovery.
OCT revealed a reduction in inner and SRF postoperatively. The greatest resolution of fluid occurred between 3 and 6 months postoperatively. Residual fluid present at 6 months often required at least 12 months before completely resolving. We found that serous macular detachment improved before the inner retinal fluid or retinoschisis. As the SRF approached complete resolution, the inner retinal fluid then began to resolve. As the inner retinal fluid is loculated in a series of pockets, there is likely greater resistance to fluid out of the layer.
In addition to anatomical improvement on OCT, our patients also achieved excellent visual gains. Interestingly, visual acuity began to improve immediately after surgery, even when patients had not demonstrated a significant reduction of fluid on OCT. This was a similar finding in the adult case series [29]. While there was some visual improvement in the immediate postoperative period, visual gains were greatest after the macular detachment resolved. Final visual outcomes were better in our paediatric series compared to adults [17, 19, 23, 25, 26, 29, 34]. This suggests that paediatric patients may have a better reserve for improvement, even in the presence of SRF, than the adult population.
None of our patients experienced any complications from surgery. To date, none have developed cataract or required further surgery. In addition, none of our patients required repeat intervention. Other surgical techniques such as vitrectomy with PVD induction and gas tamponade (with or without laser or inner limiting membrane (ILM) peel) have been described in the adult and young-adult population, but with a higher reoperation rates compared to inner retinal fenestration [15, 17,18,19, 23,24,25,26, 29, 34, 35].
Paediatric vitrectomy is often difficult to perform, as the vitreous is strongly adherent to the retina in young patients, increasing the risk of retinal tears or retinal detachment during PVD induction. In fact, case reports of surgical intervention for paediatric ODPM demonstrated difficulty completing a complete PVD or limiting the detachment to the posterior pole [20, 24]. Paediatric case reports (and children included in an adult case series) demonstrate that vitrectomy, PVD induction and gas with or without ILM peel or laser photocoagulation show variable to good anatomic results. However, repeat surgical intervention was often required and final visual acuity often was limited [16, 20, 21, 23, 24]. This suggests that our technique may be more efficacious.
This study has several limitations. The retrospective nature of this study does not allow for a control group to establish if vitrectomy, PVD and endogas without fenestrations, or even vitrectomy alone, can provide similar results. In addition, our small sample size may not represent the full range of paediatric ODPM presentations and outcomes. Despite these limitations, our results suggest that vitrectomy with two inner retinal fenestrations can safely provide anatomic and functional improvement without requiring additional treatment. This is the first case series, to our knowledge, in the management of paediatric ODPM. It is also the first case series to establish the use of inner retinal fenestrations at the time of vitrectomy for the treatment of paediatric ODPM. It supports the theory that fenestrations can redirect flow and encourage an egress of fluid into the vitreous cavity. This allows for restoration of anatomy and reversal of the pathologic processes induced in ODPM, offering visual recovery to our paediatric patients.
Summary
What was known before
-
Outcomes of surgery for paediatric optic disc pit maculopathy are variable. Single inner retinal fenestration is an effective technique in adults.
What this study adds
-
Good anatomic and visual outcomes demonstrated in a series of paediatric optic disc pit maculopathies, with significant improvement in vision despite chronicity. Dual inner retinal fenestration appears to be effective.
References
Christoforidis JB, Terrell W, Davidorf FH. Histopathology of optic nerve pit-associated maculopathy. Clin Ophthalmol. 2012;6:1169–74. https://doi.org/10.2147/OPTH.S34706
Meyer CH, Rodrigues EB, Schmidt JC. Congenital optic nerve head pit associated with reduced retinal nerve fibre thickness at the papillomacular bundle. Br J Ophthalmol. 2003;87:1300–1.
Gass JD. Serous detachment of the macula. secondary to congenital pit of the optic nervehead. Am J Ophthalmol. 1969;67:821–41. 0002-9394(69)90075-0
Brown GC, Shields JA, Patty BE, Goldberg RE. Congenital pits of the optic nerve head. I. Experimental studies in collie dogs. Arch Ophthalmol. 1979;97:1341–4.
Steel DHW, Suleman J, Murphy DC, Song A, Dodds S, Rees J. Optic disc pit maculopathy: a two-year nationwide prospective population-based study. Ophthalmology. 2018;125:1757–64. S0161-6420(18)30774-7
Lincoff H, Lopez R, Kreissig I, Yannuzzi L, Cox M, Burton T. Retinoschisis associated with optic nerve pits. Arch Ophthalmol. 1988;106:61–7.
Lincoff H, Schiff W, Krivoy D, Ritch R. Optic coherence tomography of optic disk pit maculopathy. Am J Ophthalmol. 1996;122:264–6. S0002-9394(14)72021-5
Turkcuoglu P, Taskapan C. The origin of subretinal fluid in optic disc pit maculopathy. Ophthalmic Surg Lasers Imaging Retin. 2016;47:294–8. https://doi.org/10.3928/23258160-20160229-15
Makdoumi K, Nilsson TK, Crafoord S. Levels of beta-trace protein in optic disc pit with macular detachment. Acta Ophthalmol. 2017;95:815–9. https://doi.org/10.1111/aos.13527
Gupta RR, Choudhry N. Spontaneous resolution of optic disc pit maculopathy after posterior vitreous detachment. Can J Ophthalmol. 2016;51:e24–7. https://doi.org/10.1016/j.jcjo.2015.09.020
Apple DJ, Rabb MF, Walsh PM. Congenital anomalies of the optic disc. Surv Ophthalmol. 1982;27:3–41. 0039-6257(82)90111-4
Mustonen E, Varonen T. Congenital pit of the optic nerve head associated with serous detachment of the macula. Acta Ophthalmol (Copenh). 1972;50:689–98.
Cox MS, Witherspoon CD, Morris RE, Flynn HW. Evolving techniques in the treatment of macular detachment caused by optic nerve pits. Ophthalmology. 1988;95:889–96. S0161-6420(88)33078-2
Theodossiadis GP. Treatment of maculopathy associated with optic disk pit by sponge explant. Am J Ophthalmol. 1996;121:630–7. S0002-9394(14)70628-2
Lincoff H, Yannuzzi L, Singerman L, Kreissig I, Fisher Y. Improvement in visual function after displacement of the retinal elevations emanating from optic pits. Arch Ophthalmol. 1993;111:1071–9.
Snead MP, James N, Jacobs PM. Vitrectomy, argon laser, and gas tamponade for serous retinal detachment associated with an optic disc pit: a case report. Br J Ophthalmol. 1991;75:381–2.
Dai S, Polkinghorne P. Peeling the internal limiting membrane in serous macular detachment associated with congenital optic disc pit. Clin Exp Ophthalmol. 2003;31:272–5. 652
Poulson AV, Snead DR, Jacobs PM, Ahmad N, Snead MP. Intraocular surgery for optic nerve disorders. Eye (Lond). 2004;18:1056–65. 6701572
Hirakata A, Okada AA, Hida T. Long-term results of vitrectomy without laser treatment for macular detachment associated with an optic disc pit. Ophthalmology. 2005;112:1430–5. S0161-6420(05)00310-6
Hirakata A, Hida T, Wakabayashi T, Fukuda M. Unusual posterior hyaloid strand in a young child with optic disc pit maculopathy: intraoperative and histopathological findings. Jpn J Ophthalmol. 2005;49:264–6. https://doi.org/10.1007/s10384-004-0185-5
Ishikawa K, Terasaki H, Mori M, Sugita K, Miyake Y. Optical coherence tomography before and after vitrectomy with internal limiting membrane removal in a child with optic disc pit maculopathy. Jpn J Ophthalmol. 2005;49:411–3. https://doi.org/10.1007/s10384-004-0225-1
Schaal KB, Wrede J, Dithmar S. Internal drainage in optic pit maculopathy. Br J Ophthalmol. 2007;91:1093. 91/8/1093 [pii]
Ghosh YK, Banerjee S, Konstantinidis A, Athanasiadis I, Kirkby GR, Tyagi AK. Surgical management of optic disc pit associated maculopathy. Eur J Ophthalmol. 2008;18:142–6.
Georgalas I, Petrou P, Koutsandrea C, Papaconstadinou D, Ladas I, Gotzaridis E. Optic disc pit maculopathy treated with vitrectomy, internal limiting membrane peeling, and gas tamponade: a report of two cases. Eur J Ophthalmol. 2009;19:324–6.
Hirakata A, Inoue M, Hiraoka T, McCuen BW II. Vitrectomy without laser treatment or gas tamponade for macular detachment associated with an optic disc pit. Ophthalmology. 2012;119:810–8. https://doi.org/10.1016/j.ophtha.2011.09.026
Theodossiadis GP, Grigoropoulos VG, Liarakos VS, Rouvas A, Emfietzoglou I, Theodossiadis PG. Restoration of the photoreceptor layer and improvement of visual acuity in successfully treated optic disc pit maculopathy: a long follow-up study by optical coherence tomography. Graefes Arch Clin Exp Ophthalmol. 2012;250:971–9. https://doi.org/10.1007/s00417-011-1918-z
Postel EA, Pulido JS, McNamara JA, Johnson MW. The etiology and treatment of macular detachment associated with optic nerve pits and related anomalies. Trans Am Ophthalmol Soc. 1998;96:73–88. discussion 88-93
Spaide RF, Fisher Y, Ober M, Stoller G. Surgical hypothesis: inner retinal fenestration as a treatment for optic disc pit maculopathy. Retina. 2006;26:89–91. 00006982-200601000-00014
Ooto S, Mittra RA, Ridley ME, Spaide RF. Vitrectomy with inner retinal fenestration for optic disc pit maculopathy. Ophthalmology. 2014;121:1727–33. https://doi.org/10.1016/j.ophtha.2014.04.006
Georgalas I, Ladas I, Georgopoulos G, Petrou P. Optic disc pit: a review. Graefes Arch Clin Exp Ophthalmol. 2011;249:1113–22. https://doi.org/10.1007/s00417-011-1698-5
Benatti E, Garoli E, Viola F. Spontaneous resolution of optic disk pit maculopathy in a child after a six-year follow-up. Retin Cases Brief Rep. 2021;15:453–6. https://doi.org/10.1097/ICB.0000000000000815.
Polunina AA, Todorova MG, Palmowski-Wolfe AM. Function and morphology in macular retinoschisis associated with optic disc pit in a child before and after its spontaneous resolution. Doc Ophthalmol. 2012;124:149–55. https://doi.org/10.1007/s10633-012-9314-5
Akca Bayar S, Sarigul Sezenoz A, Yaman Pinarci E, Yilmaz G. Spontaneous regression of optic disc pit maculopathy in a six-year-old child. Turk J Ophthalmol. 2017;47:56–58. https://doi.org/10.4274/tjo.57614
Bottoni F, Cereda M, Secondi R, Bochicchio S, Staurenghi G. Vitrectomy for optic disc pit maculopathy: a long-term follow-up study. Graefes Arch Clin Exp Ophthalmol. 2018;256:675–82. https://doi.org/10.1007/s00417-018-3925-9
Lincoff H, Kreissig I. Optical coherence tomography of pneumatic displacement of optic disc pit maculopathy. Br J Ophthalmol. 1998;82:367–72.
Author information
Authors and Affiliations
Contributions
SCW was responsible for identifying the patients, performing the procedure, interpreting results and revising the manuscript, figures and tables. NKS was responsible for analysing data, interpreting the results, writing the manuscript and creating the reference list, figures and tables.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wong, S.C., Scripsema, N.K. Inner retinal fenestration for paediatric optic disc pit maculopathy: a case series. Eye 36, 2111–2115 (2022). https://doi.org/10.1038/s41433-021-01813-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01813-6