Abstract
Purpose
The purpose of this study is to investigate potential factors predicting complete recovery of visual acuity following surgery for macula off retinal detachment (RD).
Patients and methods
Retrospective review of patients operated for macula-off RD at Jules-Gonin Eye Hospital between January 2015 and December 2016. The study included patients with visual acuity recovery of 0 LogMAR. A control group of 83 patients with comparable baseline characteristics but partial recovery of visual acuity after vitrectomy for macula-off RD was used for statistical comparison analysis.
Results
Seventy-four patients, 46 males (62%) and 28 females (38%), were included. Mean age was 65 years (standard deviation: 12). Median follow-up was 6 months (interquartile range: 3). Fifty patients (68%) were pseudophakic. Median pre-op best-corrected visual acuity (BCVA) was 2 LogMAR (interquartile range: 1.22). Forty-three of the patients (58%) had preoperative BCVA equivalent of count fingers or less. The majority of the patients (91%) had up to 3-day duration of macular detachment (MD) before surgery. In comparison only 18% of the group of patients with partial recovery of visual acuity after vitrectomy for macula-off RD had been operated within 3 days of MD (p < 0.0001). In 63% of the 40 cases in whom an optical coherence tomography (OCT) of the fovea could be interpreted, OCT image showed a retained foveal depression of the detached retina, whereas only 35% of the 46 control eyes with adequate OCT imaging showed a retained foveal depression (p = 0.01).
Conclusions
In our study, patients had significantly better chances of complete visual acuity recovery when operated within 3 days of MD in comparison to more delayed surgery. Additionally, preservation of the foveal depression of the detached retina appeared to be a common characteristic among patients demonstrating complete visual recovery.
Similar content being viewed by others
Background
Surgical management of macula-off rhegmatogenous retinal detachment (RRD) has been associated with a high rate of anatomical success in recent years [1]. Nevertheless, functional outcomes after surgery are variable and unpredictable for these cases and patients present more often with incomplete recovery of their visual acuity [2]. Many preoperative factors have been reported to be affecting the recovery of vision following reattachment of a macula-off RRD including age of the patient, height of the macular detachment (MD), duration of the MD and the best-corrected visual acuity (BCVA) [1,2,3,4,5,6,7,8]. It has been suggested that a macula-off RD should be operated within the 1st week after its development and that a more urgent surgical repair does not affect visual outcome and is therefore not necessary [9]. Many vitreoretinal departments apply that timeframe for surgery of macula-off RDs.
However, in recent years, emerging data from experimental research studies, but also from few clinical studies, are suggesting that a more timely intervention may be required in macula-off RRD than previously believed in order to achieve the healing of cellular damage coupled with full functional recovery [1, 4, 10,11,12].
Furthermore, in recent years, optical coherence tomography (OCT) has allowed objective and quantitative measurements of RRD height and a more precise evaluation of the architectural changes of the detached retina. These data have allowed new insights into understanding visual recovery after successful macula-off RD surgery and the potential predictive factors associated with functional recovery [2, 13,14,15,16,17,18].
In the present study, we have evaluated the characteristics of patients presenting complete short-term recovery of visual acuity (0 LogMAR units) after vitrectomy for macula-off RD.
Patients and methods
This is a retrospective review of patients operated on by two of the authors (LK and TJW) at the Jules-Gonin Eye Hospital between January 2015 and December 2016.
Inclusion criteria were:
-
(1)
Cases of RD with confirmed macular involvement for which postoperative follow-up data were available.
-
(2)
Recovery of at least 0 LogMAR visual acuity in at least 2 follow-up visits postoperatively.
Exclusion criteria were:
-
(1)
Uncertain preoperative macular involvement, e.g., bullous superior RD without demonstrable proof of macular involvement.
-
(2)
Dense ocular media pre-operatively, e.g., significant cataract and vitreous haemorrhage.
-
(3)
Patients with incomplete MD and/or good preoperative vision (LogMAR 0.0 or better).
-
(4)
Patients for which postoperative follow-up data were not available.
A control group of 83 patients was used for statistical comparison analysis. Patients of the control group were operated on by two of the authors (LK and TJW) at the Jules-Gonin Eye Hospital between January 2015 and May 2018.
Inclusion criteria of the control group were:
-
(1)
Cases of RD with confirmed macular involvement for which postoperative follow-up data were available.
-
(2)
Patients that had documented visual acuity of 0 LogMAR prior to the development of RD.
-
(3)
Patients with a final VA > 0.2 LogMAR after vitrectomy for macula-off RD.
Exclusion criteria of the control group were the same as for the study group.
All patients had a comprehensive ophthalmic examination including measurements of BCVA, intraocular pressure, slit lamp, fundus and OCT examinations. All cases in all their consultations had their visual acuity examined by highly experienced certified optometrists using standardised refraction techniques.
Additionally, we recorded the gender, age, lens status and the duration of MD. A Heidelberg Spectralis SD-OCT instrument was used to obtain all SD-OCT images (Heidelberg Engineering, Heidelberg, Germany). The height of the RD was measured when possible using the computer-based calliper measurement tool of the SD-OCT. All patients underwent standard three-port pars plana vitrectomy using 23-gauge instruments with either the Constellation (ALCON, Fort Worth, USA) or the Eva Machine (DORC, Zuidland, The Netherlands). Descriptive analyses concerning mean/median values and standard deviations (SD) were performed were performed using SPSS software (SPSS v.25 for mac; SPSS Inc., Chicago, IL).
The BCVAs were converted to logarithm of the minimum angle of resolution for statistical analysis. BCVAs of counting fingers and hand movements at two feet were valued 2 and 3 LogMAR units, respectively [19].
Statistical analysis of differences between proportions of prevalence of the two groups was conducted using MedCalc (MedCalc Software, Ostend, Belgium). Comparisons of proportions were evaluated by the “N-1” chi-squared test as recommended by Campbell and Richardson [20]. Associations were considered statistically significant when p values were <0.05.
Results
Seventy-four patients—46 males (62%) and 28 females (38%)—were included in the study after having been operated on for a macula-off RD by one of two authors (LK and TJW). During the study period, all patients demonstrated complete visual recovery. Median follow-up was 6 months (interquartile range: 3) (minimum 4 to maximum 9 months). Mean age was 65 years (SD: 12). Fifty patients (68%) were pseudophakic. Median pre-op BCVA was: 2 LogMAR (interquartile range: 1.22). Forty-three of the patients (58%) had BCVA equivalent of counting fingers or less. Gas tamponade (SF6–21% and C3F8–12%) was used in the majority—70 cases (95%). Silicone oil was used in three cases because two patients were living at high altitude and one needed to fly the next days after the surgery. In all three cases, silicone oil was removed at about 7 weeks after the first surgery.
The control group consisted of 83 patients, 54 males (65%) and 29 women (35%), 58 (70%) pseudophakic. Median pre-op VA was 2 LogMAR (interquartile range: 1.22). Median follow-up was 6 months (interquartile range: 3) (minimum 4 to maximum 10 months). There were no statistical differences between the two groups regarding gender, age, lens status, preoperative BCVA and follow-up duration.
None of the patients of both groups demonstrated any signs of proliferative vitreoretinopathy at presentation.
In the study group, the mean interval between the beginning of central visual disturbance and surgical intervention was 2.4 (SD: 1.4) days (range: 1–9 days) (Fig. 1). The majority of patients—67 patients (91%)—had up to 3-day duration of central visual disturbances before undergoing surgery. The number of patients who demonstrated full visual acuity recovery was more or less proportionately distributed among days 1, 2 and 3 with 26% of the cases having surgery up to 1 day after MD, 34% up to 2 days after MD and 31% of the cases up to 3 days after MD.
In comparison to the study group, only 18% (15 of 83 patients) of the control group of patients with partial recovery of visual acuity after vitrectomy for macula-off RD had been operated on within 3 days of MD. (The difference of proportions was statistically significant between the two groups p < 0.0001). (Fig. 2).
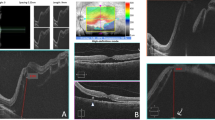
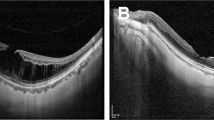
In the study group, OCT images were obtainable in 51 patients but only in 40 could the foveal area be interpreted. In 63% (25 patients) of these 40 cases the OCT image shown a retained foveal depression of the detached retina (Fig. 3). In 37% (15 patients) of these 40 cases the OCT image showed oedema in the external plexiform layer of the detached retina. Measurement of the MD height was possible in 36 patients and its mean value was 942 μm (SD: 267). In the remaining 38 patients, the height of the MD was higher than the OCT could measure. In four cases, OCTs of the foveal area were obtainable and interpretable, but the height of MD was not measurable.
In comparison to the study group, OCT imaging in the control group showed a retained foveal depression of the detached retina only in 16 (35%) of 46 cases in whom an OCT of the fovea could be interpreted. The difference of proportions was statistically significant between the two groups (p = 0.010)
In 37% (17 patients) of the 46 cases of the control group, the OCT image showed oedema in the external plexiform layer of the detached retina. OCT measurement of the MD height was possible in 42 patients, and its mean value was 902 μm (SD: 204 μm). The difference of proportions was not statistically significant between the two groups regarding oedema in the external plexiform layer of the detached retina and MD height.
In all but one patient in the study group and in two cases in the control group, the retinas were re-attached with a single procedure. The visual acuities in these three cases were not altered after the second surgery.
Discussion
The conundrum of macular recovery after RRD has occupied the ophthalmic research community for over a century [3]. Many preoperative factors have been reported to be affecting the recovery of vision following reattachment of a macula-off RRD including the age of the patient, height of the MD, duration of the MD and the preoperative BCVA [1,2,3,4,5,6,7,8] along with several OCT characteristics [2, 6, 14, 18].
Several studies have suggested that the most important predictor for visual recovery after macula-off RRD surgery is preoperative vision [21,22,23]. However, in a recent study by Kobayashi et al. [18] preoperative vision did not appear to significantly correlate with the final vision [18]. In our present study, 58% of our patients had preoperative vision equivalent to counting fingers or less and nevertheless showed complete VA recovery after surgery indicating that additional factors such as short duration of the RRD may play a significant role.
The accurate impact of duration of the MD on functional recovery and the optimal timing of surgery is not yet unanimously established [1, 3, 4, 9, 24, 25].
Ross et al. [9] advocated in a landmark study that the duration of MD within the 1st week does not influence the visual recovery after the RRD surgery. Many vitreoretinal centres worldwide apply this timeframe for surgery of macula-off RDs.
Recent studies have, however, suggested that an earlier intervention could probably be even more advantageous. Cell death in the retina after detachment peaks at the 3-day time point after which it continues at lower levels as long as the retina is detached [26]. Lewis et al. [10] showed in experimental RDs that retinal reattachment within 1 day of detachment is remarkably effective in halting many of the cellular changes at the photoreceptor level that may pose a threat to the return of normal vision. From a clinical stand point, Van Bussel et al. recently conducted a systematic review and meta-analysis of nine studies on the impact of the duration of macula-off RD on visual outcome. Their analysis suggested that scleral buckling for MD must preferably be performed within 3 days to optimise visual outcome. However, they found only limited amount of data regarding pars plana vitrectomy, which precluded a meta-analysis with substantial results [1]. Frings et al. [12] investigated the influence of lag time between the onset of central visual acuity loss and surgical intervention of macula-off RD and concluded that patients who are treated up to 3 days after the onset of central vision loss have a better final visual acuity than patients with longer lag times. However, they did not find statistically significant differences regarding surgery within the first 3 days [12]. On the other hand, Greven et al. [4] reported that the duration of MD affected the final BCVA even in patients whose MD was <3 days, with significant differences in the final BCVA between detachments of 1- vs 3-day duration.
In our study, patients had significantly better chances of complete visual acuity recovery when operated on within 3 days of MD compared to more delayed surgery. Our study could not ascertain if earlier surgery, i.e., day 1 rather day 2 or 3 could potentially be even more advantageous. The number of patients who demonstrated full visual recovery was more or less proportionately distributed among days 1, 2 and 3 of the duration of MD.
On another note, several recent OCT studies assessed various characteristics of detached retinal architecture revealing some insights that may help understand some novel elements of visual recovery after successful surgery [2, 13,14,15,16,17,18, 27, 28].
In our study, the preservation of the foveal depression in the detached retina appeared to be more often correlated with patients achieving complete visual recovery after surgery. As only about half of our patients the study and the control group had interpretable OCT images, consequently these results should be interpreted with caution. Furthermore, it is possible that increased MD duration may lead to more degenerative retinal changes and to the loss of the foveal depression, in which case some OCT changes could merely reflect duration.
Obvious limitations of our study consist of it being retrospective in character. Furthermore, the duration of MD may be biased by patient perception and therefore may not be particularly accurate. The effects of such bias may be overstated as in almost all cases the patient’s description often matched the information provided by the referring ophthalmologist. Lastly, we evaluated only relatively short-term visual acuity recovery, even though it is known that patients’ postoperative BCVA may continue to improve up to several years after surgery for macula-off RD [29].
Another issue to be considered is that complete visual acuity recovery does not necessarily reflect complete functional recovery or having attained the status quo ante. Some of our patients reported quality of vision issues such as a slight attenuation of colour perception despite excellent BCVA. We did not perform auxiliary tests due to the limitations of the retrospective design and additional tests like microperimetry [30] may provide a more precise assessment of functional recovery.
One interesting point that is emerging from our study is that there were cases that—against all odds—and despite presenting many unfavourable signs such as long documented duration of MD and high MD have still achieved full BCVA recovery. It is unknown which other potential protective parameters or even possible genetic characteristics allow some patients to achieve such a favourable evolution and not to others.
In conclusion, in our study patients had significantly better chances of complete visual acuity recovery when operated on within 3 days of MD in comparison to more delayed surgery. Additionally, preservation of the foveal depression of the detached retina appeared to be a common characteristic among patients demonstrating complete visual acuity recovery suggesting a potential association with functional recovery. Ultimately, the only predictive factor that is modifiable by the surgical management is the duration of MD, and our results suggest, therefore, that a macula-off RD should preferably be repaired within 3 days of the macula detaching.
Summary
What was known before
-
There are emerging data albeit limited suggesting that more timely intervention may be required in macula-off RRD than previously believed.
What this study adds
-
We describe characteristics of patients presenting complete visual acuity recovery after vitrectomy for macula-off retinal detachment.
-
In our study patients had significantly better chances of complete visual acuity recovery when operated within 3 days of macular detachment in comparison to more delayed surgery.
-
Additionally, preservation of foveal depression of the detached retina appeared to be a relatively common characteristic among patients demonstrating complete visual acuity recovery suggesting a potential association with functional recovery though that change could be merely a reflection of duration.
-
Ultimately, the only factor that is modifiable is the duration of MD and probably a well-timed intervention is advantageous.
References
van Bussel EM, van der Valk R, Bijlsma WR, La, Heij EC. Impact of duration of macula-off retinal detachment on visual outcome: a systematic review and meta-analysis of literature. Retina. 2014;34:1917–25.
Hirata N, Iwase T, Kobayashi M, Yamamoto K, Ra E, Terasaki H. Correlation between preoperative factors and final visual acuity after successful rhegmatogenous retinal reattachment. Sci Rep. 2019;9:3217.
Abouzeid H, Wolfensberger TJ. Macular recovery after retinal detachment. Acta Ophthalmol Scand. 2006;84:597–605.
Greven MA, Leng T, Silva RA, Leung LB, Karth PA, Moshfeghi DM, et al. Reductions in final visual acuity occur even within the first 3 days after a macula-off retinal detachment. Br J Ophthalmol. 2019;103:1503–6.
Hassan TS, Sarrafizadeh R, Ruby AJ, Garretson BR, Kuczynski B, Williams GA. The effect of duration of macular detachment on results after the scleral buckle repair of primary, macula-off retinal detachments. Ophthalmology. 2002;109:146–52.
Karacorlu M, Sayman Muslubas I, Hocaoglu M, Arf S, Ersoz MG. Correlation between morphological changes and functional outcomes of recent-onset macula-off rhegmatogenous retinal detachment: prognostic factors in rhegmatogenous retinal detachment. Int Ophthalmol. 2018;38:1275–83.
Khanzada MA, Wahab S, Hargun LD. Impact of duration of macula off rhegmatogenous retinal detachment on visual outcome. Pak J Med Sci. 2014;30:525–9.
Park DH, Choi KS, Sun HJ, Lee SJ. Factors associated with visual outcome after macula-off rhegmatogenous retinal detachment surgery. Retina. 2018;38:137–47.
Ross WH, Kozy DW. Visual recovery in macula-off rhegmatogenous retinal detachments. Ophthalmology. 1998;105:2149–53.
Lewis GP, Charteris DG, Sethi CS, Leitner WP, Linberg KA, Fisher SK. The ability of rapid retinal reattachment to stop or reverse the cellular and molecular events initiated by detachment. Invest Ophthalmol Vis Sci. 2002;43:2412–20.
Lewis GP, Charteris DG, Sethi CS, Fisher SK. Animal models of retinal detachment and reattachment: identifying cellular events that may affect visual recovery. Eye. 2002;16:375–87.
Frings A, Markau N, Katz T, Stemplewitz B, Skevas C, Druchkiv V, et al. Visual recovery after retinal detachment with macula-off: is surgery within the first 72 h better than after? Br J Ophthalmol. 2016;100:1466–9.
Wolfensberger TJ, Gonvers M. Optical coherence tomography in the evaluation of incomplete visual acuity recovery after macula-off retinal detachments. Graefes Arch Clin Exp Ophthalmol. 2002;240:85–9.
Hagimura N, Suto K, Iida T, Kishi S. Optical coherence tomography of the neurosensory retina in rhegmatogenous retinal detachment. Am J Ophthalmol. 2000;129:186–90.
Maruko I, Iida T, Sekiryu T, Saito M. Morphologic changes in the outer layer of the detached retina in rhegmatogenous retinal detachment and central serous chorioretinopathy. Am J Ophthalmol. 2009;147:489–94.e1.
Lecleire-Collet A, Muraine M, Menard JF, Brasseur G. Evaluation of macular changes before and after successful retinal detachment surgery using stratus-optical coherence tomography. Am J Ophthalmol. 2006;142:176–9.
Schocket LS, Witkin AJ, Fujimoto JG, Ko TH, Schuman JS, Rogers AH, et al. Ultrahigh-resolution optical coherence tomography in patients with decreased visual acuity after retinal detachment repair. Ophthalmology. 2006;113:666–72.
Kobayashi M, Iwase T, Yamamoto K, Ra E, Murotani K, Terasaki H. Perioperative factors that are significantly correlated with final visual acuity in eyes after successful rhegmatogenous retinal detachment surgery. PLoS ONE. 2017;12:e0184783.
Holladay JT. Proper method for calculating average visual acuity. J Refract Surg. 1997;13:388–91.
Campbell I. Chi-squared and Fisher-Irwin tests of two-by-two tables with small sample recommendations. Stat Med. 2007;26:3661–75.
Tani P, Robertson DM, Langworthy A. Prognosis for central vision and anatomic reattachment in rhegmatogenous retinal detachment with macula detached. Am J Ophthalmol. 1981;92:611–20.
Ross WH. Visual recovery after macula-off retinal detachment. Eye (London, England). 2002;16:440–6.
Wilkinson CP. Mysteries regarding the surgically reattached retina. Trans Am Ophthalmol Soc. 2009;107:55–7.
Burton TC. Recovery of visual acuity after retinal detachment involving the macula. Trans Am Ophthalmol Soc. 1982;80:475–97.
Diederen RM, La Heij EC, Kessels AG, Goezinne F, Liem AT, Hendrikse F. Scleral buckling surgery after macula-off retinal detachment: worse visual outcome after more than 6 days. Ophthalmology. 2007;114:705–9.
Cook B, Lewis GP, Fisher SK, Adler R. Apoptotic photoreceptor degeneration in experimental retinal detachment. Invest Ophthalmol Vis Sci. 1995;36:990–6.
Lee SY, Joe SG, Kim JG, Chung H, Yoon YH. Optical coherence tomography evaluation of detached macula from rhegmatogenous retinal detachment and central serous chorioretinopathy. Am J Ophthalmol. 2008;145:1071–6.
Nakanishi H, Hangai M, Unoki N, Sakamoto A, Tsujikawa A, Kita M, et al. Spectral-domain optical coherence tomography imaging of the detached macula in rhegmatogenous retinal detachment. Retina. 2009;29:232–42.
Kusaka S, Toshino A, Ohashi Y, Sakaue E. Long-term visual recovery after scleral buckling for macula-off retinal detachments. Jpn J Ophthalmol. 1998;42:218–22.
Rossetti A, Doro D, Manfre A, Midena E. Long-term follow-up with optical coherence tomography and microperimetry in eyes with metamorphopsia after macula-off retinal detachment repair. Eye. 2010;24:1808–13.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Konstantinidis, L., Stappler, T., Potic, J. et al. Characteristics of patients with complete visual acuity recovery after vitrectomy for macula-off retinal detachment. Eye 35, 2834–2839 (2021). https://doi.org/10.1038/s41433-020-01322-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01322-y