Abstract
Background
Susac’s syndrome, a rare autoimmune vasculo-occlusive disease, may pose a diagnostic challenge and result in a devastating ocular and systemic outcome. Our study identifies a new retinal finding and evaluates disease outcome. We aimed to assess clinical and imaging findings, systemic manifestations and disease outcome in patients with ocular Susac’s syndrome under immunosuppressive/immunomodulation therapies.
Methods
Retrospective tertiary center study including patients with a diagnosis of Susac’s syndrome with >12 months follow up. Medical record review including ocular, neurological and auditory clinical and imaging findings, and treatment modalities. Main outcome measures were clinical manifestations and disease outcome.
Results
Seven patients (14 eyes) with a mean age of 34.1 years were included. Mean follow-up was 31.9 months (12.4–72.4). All had bilateral ocular disease. Retinal microaneurysms, a new ocular finding, were demonstrated in 5 patients and persisted at the final visit. In 5 eyes, they further extended during follow-up. All were treated with immunosuppressive drugs and 5/7 additional immunomodulation therapy. At last examination, best corrected visual acuity was >20/40 in all eyes, 1/10 eyes had visual field deterioration, no eye had active ocular disease, all patients achieved neurological stability, and 1 patient had auditory deterioration.
Conclusion
Retinal microaneurysms, a new ocular finding in Susac’s syndrome, were present in most of our patients, indicating ischemic retinal damage. Immunosuppressive and immunomodulation therapies seem to be highly effective in the control of disease activity.
Similar content being viewed by others
Introduction
Susac’s syndrome consists of the clinical triad of encephalopathy, branch retinal artery (BRAO) occlusion and sensorineural hearing loss. The syndrome has a female predominance and affects young patients [1, 2]. It is considered to be an autoimmune vasculo-occlusive disease, in which the vascular endothelium is injured by circulating antibodies, and results in arterial micro infarcts affecting the central nervous system (CNS), retina, and inner ear [3,4,5,6].
A study of experts of the European Susac Consortium (EuSaC) team [7], describes established criteria for diagnosis of either definite or probable Susac syndrome. In definite Susac, patients present an unequivocal clinical and/or paraclinical involvement of all three main organs (fulfilling the typical clinical triad), including (1) brain involvement with new cognitive impairment and/or behavioral changes and/or new focal neurological symptoms and/or new headache, and typical cranial MRI findings; (2) retinal involvement, i.e., BRAOs or arteriolar wall hyperfluorescence (AWH) in fluorescein angiography (FA) or signs of branch retinal ischemia; (3) vestibulocochlear involvement with new tinnitus and/or sensorineural hearing loss and/or peripheral vertigo, supported by objective testing. Probable Susac defined patients with an unequivocal clinical and/or paraclinical involvement of two of the three main organs. In patients with some of the typical features of Susac, who do not fulfill even two of the main organs, the diagnosis should be considered as possible and these patients need careful and frequent follow-up since the diagnosis could evolve in the future.
In another Susac diagnostic criteria published by Egan [2], the author concludes that in the absence of the clinical triad, the presence of AWH remote from retinal vascular injury and central callosal lesions are confirmatory of the diagnosis because they have never been described in any other condition.
Susac’s syndrome clinical manifestations may vary between patients and may resemble other neurological, ophthalmic and auditory diseases. Hence, it is crucial to be familiar with disease clinical and imaging manifestations in order to allow a proper and fast systemic immunosuppressive treatment which may alter disease final outcome [8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26].
An English literature search revealed only few case-reports and small case-series, consisting mainly of small number of patients [8, 9, 11, 12, 14, 20,21,22, 24], describing clinical and imaging findings of ocular Susac’s syndrome.
Recently, we had an outbreak of Susac’s patients in our medical center; 10 patients were diagnosed between July 2017 and November 2019 which represent about a fivefold increase in incidence as compared to previous years and to the expected incidence according to population size.
In the current study we assessed patients’ ocular characteristics using multimodal imaging, the correlation with neurological and auditory findings and disease outcome under immunosuppressive treatment and in most cases a combination of immunosuppressive and immunomodulation drugs in a cohort of patients with Susac’s syndrome.
Methods
This retrospective study was approved by the Institutional Review Board of Tel Aviv Medical Center (0435-19-TLV). Consecutive Patients with a follow-up time of >12 months, diagnosed with Susac’s syndrome, between May 2013 and November 2019, were included in the study. Definite or probable Susac’s syndrome was defined according to the EuSaC criteria [7].
Demographic and clinical data were obtained from medical files. Color fundus photography was performed using a conventional fundus photography camera (FF450; Carl Zeiss Meditec Inc, Jena, Germany). After pupil dilation, patients underwent spectral-domain optical coherence tomography (OCT) and OCT Angiography (OCTA, Spectralis; Heidelberg Engineering, Heidelberg, Germany). Macular OCT scans were evaluated for (1) areas of hyperreflective thickening of retinal nerve fiber layer to the outer plexiform layer which is indicative for tissue swelling due to acute BRAO, and (2) areas of thinning of these layers indicative for previous ischemic damage. FA montage composite pictures were evaluated (HRA; Heidelberg Engineering, Heidelberg, Germany or FF450; Carl Zeiss Meditec Inc, Jena, Germany). Visual field (Humphrey SITA Fast 30‐2 program) test results were reviewed and evaluated for (1) defects within the central 10 degrees, (2) mid peripheral defects within 10 to 30 degrees, and (3) concentric defects, i.e., involvement of at least 3 quadrants with peripheral defects.
Patients were diagnosed with ocular Susac’s syndrome if they have met the ‘retinal involvement criterion’, as was published by the EuSaC team, i.e., BRAOs or AWH in FA or characteristic signs of branch retinal ischemia in funduscopy or OCT [7].
VA was measured on Snellen chart. The equivalent logarithm of the minimum angle of resolution acuity (logMAR) was calculated and used for analysis. The mean logMAR at presentation and at final visit were compared. In addition, VA was stratified by three groups: <0.3 logMAR (better than 20/40 Snellen equivalent), 0.3–1.0 logMAR (20/40–20/200) and >1.0 logMAR (worse than 20/200), corresponding to good VA, moderate vision loss and severe vision loss, respectively.
CNS involvement was characterized by both clinical and radiological evidence [7]. Grading of severity of CNS involvement was according to Rennebohm and colleagues publication, differentiating between mild, moderate, severe, and very severe disease according to clinical features, MRI and CSF findings [27]. Clinical follow up and repeat MRIs were scheduled every 3 months or whenever a relapse was suspected.
MRI improvement was defined as a decrease in lesion load or resolution of enhancement/restricted diffusion.
Vestibulocochlear involvement was defined as new tinnitus and/or sensorineural hearing loss, and/or peripheral vertigo. An audiometry was performed every 6 months in order to support the auditory complaints.
Medical treatments were recorded at the first examination, during follow-up and at the last visit. Treatments strategies were updated in accordance with newly published guidelines [27] and included IV methyprednisolone (IVMP), intravenous immune globulin (IVIG) and mycophenolate mofetil for mild cases, an addition of cyclophosphamide (CPM) in moderate cases and rituximab for severe CNS involvement.
In cases of active ocular disease in the absence of acute neurological or auditory findings, treatment was modified either by adding Rituximab to the regimen or IVIG.
Results
Baseline demographics and ocular characteristics
During the study period, 12 patients were diagnosed with Susac’s syndrome. Seven patients (14 eyes) with a follow-up time of more than 12 months were included in the study. Of them, 4 (57.1%) were women. The mean age at presentation was 34.1 years (range 20–44). The mean follow-up time was 35.1 months (range 12.4–72.4). Five patients presented with definite Susac’s syndrome and 2 patients presented with probable Susac’s syndrome. All had a bilateral ocular disease. One patient presented with extremely severe CNS disease, 3 patients presented with severe CNS disease and the rest had mild-moderated CNS involvement. All patients had MRI lesions at the corpus callosum. In addition, 6 out of 7 patients had MRI lesions involving other sites of the brain. Five patients had sensorineural hearing loss and in 4/5 patients the disease was bilateral. Table 1 presents baseline characteristics.
Ocular manifestations at baseline are described in Table 2. Mean BCVA at presentation was 0.07 ± 0.13 logMAR, (0–0.4;20/20–20/50). All patients (14/14 eyes, 100%) had extra-macular BRAO, 4 eyes of 3 patients (4/14, 28.6%) had also macular BRAO (patients no. 3, 4, 7). Gass plaques were found in 4 eyes of 3 patients (4/14, 28.6%; patients no. 2, 5, 7).
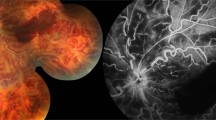
FA findings included extra-macular BRAO in all eyes, macular BRAO in 3 eyes of 3 patients (3/14, 21.4%; no. 3, 4, 7), AWH in 6 eyes of 4 patients (6/14, 42.9%; no. 2, 4, 6, 7), capillary non perfusion (CNP) in 3 eyes of 2 patients (3/14, 21.4%; no. 4, 7) and retinal microaneurysms in one eye of one patient (1/14, 7.1; no.7). Figures 1 and 2 present characteristic FA findings.
A Left eye fundus fluorescein angiography (patient no. 6) showing areas of peripheral capillary nonperfusion and retinal microaneurysms without leakage in 4 quadrants (arrows). B Magnified picture on retinal microaneuryms in the inferior periphery demonstrating various sizes. C Left eye (patient no. 2 | ) showing microaneurysms without leakage in the superior periphery. Note AWH and peripheral capillary nonperfusion.
Two patients performed OCT at first presentation (patients no. 3 and 7). Patient no. 3 (both eyes) and Patient no.7 (left eye) had signs of acute retinal hypoxia indicating on an acute macular BRAO. In addition, both patients showed bilateral signs of retinal thinning, compatible with previous events of macular ischemia.
Ocular findings during follow-up
At presentation, 13 out of 14 eyes had good VA (>20/40 Snellen equivalent) (78.6%, 11/14 eyes had BCVA of 20/20) and one eye had moderate VA. At final visit all eyes had good VA (20/20 in 6 eyes). Mean BCVA at final visit was stable (0.08 ± 0.07 logMAR, 0-0.2;20/20-20/30).
During follow-up, we observed new ocular findings: new extra-macular BRAO in 11 eyes of all 7 patients (11/14, 78.6%), new macular BRAO in 2 eyes of 2 patients (2/14, 14.3%; no.1 and 7), new Gass plaques in 5 eyes of 3 patients (5/14, 35.7%; no. 1, 4, 7), new AWH in 10 eyes of 5 patients (10/14, 71.4%; no. 1, 2, 3, 4, 5), new CNP areas in 11 eyes of 6 patients (11/14, 78.6%; all patients except no.3) and new NVES in 2 eyes of 2 patients (2/14, 14.3%; no. 6, 7).
New retinal microaneurysms were found in 8 eyes of 5 patients (8/14, 57.1%; no. 2, 4, 5, 6, 7) and in 5 eyes (5/14, 35.7%; no. 2, 5, 6) the number of involved retinal quadrants increased (Fig. 2) during the follow up. The retinal microaneurysms presented at ischemic and non-ischemic areas, involving the posterior pole or the periphery. Notably, the microaneurysms were of different sizes and did not leak. Retinal microaneurysms did not resolve at final visit.
Six patients (no. 1,2,3,4,6,7) were followed up with serial OCT imaging over the study period. Patient no. 1 showed signs of acute macular BRAO on OCT which was performed 11 months after initial presentation, patient no.2 had no abnormal findings, patient no.3 who had acute macular BRAO at presentation developed bilateral sectorial macular retinal thinning, patient no.4 showed bilateral sectorial macular retinal thinning on OCT 2 month post initial presentation, patient no.6 had no abnormal findings, and patient no. 7 who presented with acute BRAO superior to the fovea in her left eye, developed acute signs of an additional macular BRAO in the superior macula of the same eye 6 months after initial presentation and subsequent macular retinal thinning (Fig. 3).
Color fundus picture (A) showing retinal whitening in the area of a superior macular branch artery occlusion. In addition, note 2 cotton wool spots. Red free image (B) shows the ischemic area brighter than the surrounding tissue. (C) 30–2 degree visual field testing displays a corresponding inferior scotoma. Superficial (D) and deep (E) vessel plexus show reduced vessel density in the area of the BRAO.
OCT-A was performed in 2 patients (no. 4 and 6). Patient no.4 showed decreased vascular perfusion of both superficial and deep plexuses in the area of the occluded macular arteriole (Fig. 4). OCT-A imaging was normal in patient no.6.
Five patients performed visual field testing during the follow-up period (no. 2,3,4,7 within the first year, patient no. 6 after 6 years). Patients no. 1 and 5 were unable to perform the test due to their neurological condition. Patient no.6 had normal visual fields in both eyes. Four eyes of 3 patients (4/14, 28.6%; no. 3,4,7) showed a scotoma within the 10 central degrees (Fig. 4). Three patients (no. 3,4,7) had bilateral peripheral visual field defects and patient no. 2 had unilateral peripheral visual field defects. Concentric defects were noted bilaterally in patients no.3 and no.7, and unilaterally in patient no. 4.
Immunosuppressive treatment
Initial treatments included intravenous methylprednisolone followed by prednisone 1 mg/kg in all patients. Six out of 7 patients had additional treatments: Cyclophosphamide (n = 4), mycophenolate mofetil (n = 2), intravenous immunoglobulins (n = 3), azathioprine (n = 1). At final visit: 1 patient (no.6) was able to stop all treatments, 2 patients were on a single treatment (no.3 - mycophenolate mofetil, no.7 – rituximab), 4 patients were on combination therapy (no.1- prednisone above 7.5 mg-day, IVIG, rituximab; no.2- IVIG, rituximab; no.4 - prednisone above 7.5 mg-day, IVIG, CPM; no.5 - prednisone above 7.5 mg-day, IVIG, mycophenolate mofetil).
Additional ocular treatments included scatter panretinal laser photocoagulation (PRP) due to retinal neovascularizations (NVEs) (in 2 eyes/2 patients –no.5,7).
Ocular and systemic outcome
All eyes maintained good VA at final visit (≥20/30), and one eye improved from moderate VA to good VA. FA demonstrated AWH in the far retinal periphery in 5 eyes of 3 patients (no. 2, 4, 5). These AWH areas thought to be secondary to a past capillary damage as they were demonstrated clearly in comparison of serial FA exams. Notably, none of these eyes had signs of new BRAOs. The retinal NVEs (2 eyes/2 patients no.5,7) regressed. Gass plaques were not found in any eye.
VF at final visit was available in 10 eyes of 5 patients (no. 2, 3, 4, 6, 7). Patient no. 7 experienced deterioration in her left eye: Mean deviation deteriorated from −9.2 to −13.6, and peripheral defects were present in 4 compared to 3 quadrants on first available VF. Patient no. 3 experienced slight improvement in his left eye: Mean deviation improved from −13.0 to −10.0, and peripheral defects were less severe. The other 8 eyes remained stable.
Macular OCT at final visit was performed in all but one patient (no.5) and showed bilateral thinning of retinal layers in 4 patients (no. 1, 3, 4, 7). OCT was normal in both eyes of patients no. 2 and no.6.
All patients achieved neurological stability, both clinically and radiologically: Four patients improved clinically and 3 were stable. On MRI, 5 patients showed decrease of lesion load (patients no. 1, 2, 3, 4, 7), and 2 were stable. All but one patient (no.4) had a stable or improved hearing thresholds on audiometry.
Discussion
Our study presents a comprehensive case-series on ocular and systemic Susac’s syndrome under immunosuppressive and immunomodulation treatments. We demonstrate a new ocular finding, which was not previously reported, the presence of retinal microaneurysms in most of the eyes. We believe that this noveal ocular manifestation may shed a light on disease pathogenesis. In addition, the current study shows beneficial effect of systemic treatment on ocular and systemic outcomes.
Most of our patients (71%) presented with definite Susac’s syndrome. In other published case-series, definite Susac’s syndrome was found in 13–100% of the patients (Dörr et al. 2013; Jarius et al. 2014; Mateen et al. 2012; Vishnevskia-Dai et al. 2016). There is a high importance of physicians’ awareness of the disease and of a good multidisciplinary collaboration as part of the disease workup.
Retinal microaneurysms were found in the majority of eyes and the number of involved retinal quadrants increased during follow-up. The formation of retinal microaneurysms is the result of focal damage to the capillary wall and may be due to loss of pericytes. In addition, we hypothesize that damage to endothelial cells, may be by anti-endothelial cell antibodies which was shown to exist in a subset of patients with definite Susac’s syndrome [5], may cause secondary damage to the pericytes that wrap around the endothelial cells. Moreover, retinal ischemia induces expression of vascular endothelial growth factor, which has been shown to play a role in the formation of microaneurysms in other retinal vascular diseases [28]. Retinal microaneurysms did not resolve during follow-up and were demonstrated in our patients as a permanent finding.
All our patients presented with bilateral extra-macular BRAOs and experienced additional extramacular BRAOs during the study period. The diagnosis of extra-macular BRAO may be missed as the patients may be asymptomatic and ocular findings may be subtle on clinical examination. Hence, a high clinical suspicion for Susac is warranted in order to refer the patients for ocular examination including FA in all cases. It is recommended to use a FA montage image or wide-field FA in order to allow a thorough assessment of the peripheral retina. In addition, some patients presented or developed macular BRAO. However, VA remained stable in these eyes due to partial foveal sparing.
The presence of AWH is the second angiographic sign for ocular disease activity [7] and was found in all our patients during the study period. AWH may be either proximal or distant to arteriolar occlusion and is a pathognomonic finding in ocular Susac’s syndrome. If distant from a BRAO, it may indicate a more widespread disorder (Egan 2019; Egan, Hills & Susac 2010). Three of our patients presented AWH in the absence of BRAOs at last visit, which were assumed to be secondary to incompletely healed capillary damage from past vasculopahy and did not indicate on an active disease. This highlights the importance of an aggressive systemic therapy which allowed to prevent further ischemic events.
Other FA findings include the presence of CNP areas and retinal neovascularization. While only a minority of the eyes (3/14) had CNP at presentation, new CNP areas were demonstrated during follow-up, in all but one patient, indicating on an ongoing ischemia. However, NVE’s were a rare finding in our cohort and fully regressed post scatter PRP, which indicates on a good control of the disease.
Ocular outcome was favorable with good visual acuity in all eyes at last follow-up. Although visual fields at final visit were impaired in 5 out of 10 eyes, these defects were stable in all but 1 eye. FA allowed to monitor ocular disease activity based on the presence of new BRAOs and AWH. At last follow-up, no eye had an active ocular disease, 4 patients were able to stop systemic corticosteroids and the remaining patients were on prednisone above 7.5 mg/day, but in a tapering- down regimen.
Overall, neurological and auditory results were good; all patients achieved neurological improvement or stability and all but one patient had stable or improved thresholds on audiometry.
Our study has some limitations similar to previous case series; its retrospective design and the absence of VF test in some of the eyes. Other publications on Susac’s syndrome showed similar limitations as no prospective study was conducted to date.
In conclusion, the data provided in the current study highlights a new FA finding, the presence of retinal microaneurysms. We believe that ophthalmologists should be aware to this finding when considering the diagnosis of Susac’s syndrome. In addition, our study reinforces the importance of a good multidisciplinary collaboration as part of the disease workup and treatment, as Susac’s syndrome may lead to severe visual, cognitive and auditory impairment while prompt immunosuppressive/ immunomodulation therapy targeted according to the clinical findings may be associated with a favorable outcome and achievement of disease stability.
Summary
What was known before
-
Susac’s syndrome is a rare autoimmune vasculo-occlusive disease.
-
It may pose a diagnostic challenge and result in a devastating ocular and systemic outcome.
What this study adds
-
We presents a new ocular finding in Susac’s syndrome: retinal microaneurysms were found in most of our patients.
-
We suggest that this may shed a light on disease pathogenesis.
-
Modern systemic treatment is highly effective in the control of disease activity.
References
Susac JO. Susac’s syndrome: the triad of microangiopathy of the brain and retina with hearing loss in young women. Neurology. 1994;44:591–3. https://www.ncbi.nlm.nih.gov/pubmed/8164809
Egan RA. Diagnostic criteria and treatment algorithm for Susac syndrome. J Neuroophthalmol. 2019;39:60–67. https://www.ncbi.nlm.nih.gov/pubmed/29933288
Gross CC, Meyer C, Bhatia U, Yshii L, Kleffner I, Bauer J, et al. CD8+ T cell-mediated endotheliopathy is a targetable mechanism of neuro-inflammation in Susac syndrome. Nat Commun. 2019;10:5779. https://doi.org/10.1038/s41467-019-13593-5
Jarius S, Kleffner I, Dörr JM, Sastre-Garriga J, Illes Z, Eggenberger E, et al. Clinical, paraclinical and serological findings in Susac syndrome: an international multicenter study. J Neuroinflammation. 2014;11:46. https://www.ncbi.nlm.nih.gov/pubmed/24606999
Jarius S, Neumayer B, Wandinger KP, Hartmann M, Wildemann B. Anti-endothelial serum antibodies in a patient with Susac’s syndrome. J Neurol Sci. 2009;285:259–61. https://www.ncbi.nlm.nih.gov/pubmed/19643446
Magro CM, Poe JC, Lubow M, Susac JO. Susac syndrome: an organ-specific autoimmune endotheliopathy syndrome associated with anti-endothelial cell antibodies. Am J Clin Pathol. 2011;136:903–12. https://www.ncbi.nlm.nih.gov/pubmed/22095376
Kleffner I, Dörr J, Ringelstein M, Gross CC, Böckenfeld Y, Schwindt W, et al. Diagnostic criteria for Susac syndrome. J Neurol Neurosurg Psychiatry. 2016;87:1287–95. https://www.ncbi.nlm.nih.gov/pubmed/28103199
Bernard JT, Romero R, Agrawal K, Jager R, Rezania K. Optical coherence tomography in Susac’s syndrome. Mult Scler Relat Disord. 2014;3:110–6. https://www.ncbi.nlm.nih.gov/pubmed/25877981
Brandt AU, Oberwahrenbrock T, Costello F, Fielden M, Gertz K, Kleffner I, et al. Retinal lesion evolution in SUSAC syndrome. Retina. 2016;36:366–74. https://www.ncbi.nlm.nih.gov/pubmed/26200513
Rennebohm RM, Egan RA, Susac JO. Treatment of Susac’s syndrome. Curr Treat Options Neurol 2008;10:67–74. https://www.ncbi.nlm.nih.gov/pubmed/18325301
Ringelstein M, Albrecht P, Kleffner I, Bühn B, Harmel J, Müller A-K, et al. Retinal pathology in Susac syndrome detected by spectral-domain optical coherence tomography. Neurology. 2015;85:610–8. https://www.ncbi.nlm.nih.gov/pubmed/26203089
Salvanos P, Moe MC, Utheim TP, Bragadóttir R, Kerty E. Ultra-wide-field fundus imaging in the diagnosis and follow-up of Susac syndrome. Retin Cases Brief Rep. 2018;12:234–9. https://www.ncbi.nlm.nih.gov/pubmed/27828899
Saw VP, Canty PA, Green CM, Briggs RJ, Cremer PD, Harrisberg B, et al. Susac syndrome: microangiopathy of the retina, cochlea and brain. Clin Exp Ophthalmol. 2000;28:373–81. https://www.ncbi.nlm.nih.gov/pubmed/11097286
Spiess K, Martínez JRG. OCT angiography: assessment of retinal ischemia in Susac’s syndrome. Ophthalmic Surg Lasers Imaging Retina. 2017;48:505–8. https://www.ncbi.nlm.nih.gov/pubmed/28613358
Vishnevskia-Dai V, Chapman J, Sheinfeld R, Sharon T, Huna-Baron R, Manor RS, et al. Susac syndrome: clinical characteristics, clinical classification, and long-term prognosis. Medicine. 2016;95:e5223–e5223. https://www.ncbi.nlm.nih.gov/pubmed/27787385
Yepez JB, Murati FA, Pettito M, Arevalo JF. Intravitreal triamcinolone in susac syndrome. Retin Cases Brief Rep. 2017;11:236–9. https://www.ncbi.nlm.nih.gov/pubmed/27276498
Dörr J, Radbruch H, Bock M, Wuerfel J, Brüggemann A, Wandinger KP, et al. Encephalopathy, visual disturbance and hearing loss-recognizing the symptoms of Susac syndrome. Nat Rev Neurol. 2009;5:683–8. https://www.ncbi.nlm.nih.gov/pubmed/19953118
Dörr J, Krautwald S, Wildemann B, Jarius S, Ringelstein M, Duning T, et al. Characteristics of Susac syndrome: a review of all reported cases. Nat Rev Neurol. 2013;9:307–16. https://www.ncbi.nlm.nih.gov/pubmed/23628737
Buelens T, Ossewaarde-van Norel J, de Boer JH, Nubourgh I, Glibert G, Kamgang Semeu P, et al. Evaluation of tumor necrosis factor inhibitor therapy in susac syndrome. Retina. 2019: https://doi.org/10.1097/IAE.0000000000002466. Available at:https://www.ncbi.nlm.nih.gov/pubmed/30707148
Egan RA, Ha Nguyen T, Gass JDM, Rizzo JF 3rd, Tivnan J, Susac JO. Retinal arterial wall plaques in Susac syndrome. Am J Ophthalmol. 2003;135:483–6. https://www.ncbi.nlm.nih.gov/pubmed/12654364
Egan RA, Hills WL, Susac JO. Gass plaques and fluorescein leakage in Susac Syndrome. J Neurol Sci. 2010;299:97–100. https://www.ncbi.nlm.nih.gov/pubmed/20880549
Egan RA, Jirawuthiworavong G, Lincoff NS, Chen JJ, Francis CE, Leavitt JA. Retinal arterio-arterial collaterals in Susac syndrome. J Neuroophthalmol. 2018;38:459–61. https://www.ncbi.nlm.nih.gov/pubmed/29341996
Heng LZ, Bailey C, Lee R, Dick A, Ross A. A review and update on the ophthalmic implications of Susac syndrome. Surv Ophthalmol. 2019;64:477–85. https://www.ncbi.nlm.nih.gov/pubmed/30703404
Martinet N, Fardeau C, Adam R, Bodaghi B, Papo T, Piette J-C, et al. Fluorescein and indocyanine green angiographies in Susac syndrome. Retina 2007;27:1238–42. https://www.ncbi.nlm.nih.gov/pubmed/18046231
Mastropasqua R, Toto L, Senatore A, D’Uffizi A, Neri P, Mariotti C, et al. Optical coherence tomography angiography findings in Susac’s syndrome: a case report. Int Ophthalmol. 2018;38:1803–8. https://www.ncbi.nlm.nih.gov/pubmed/28730399
Mateen FJ, Zubkov AY, Muralidharan R, Fugate JE, Rodriguez FJ, Winters JL, et al. Susac syndrome: clinical characteristics and treatment in 29 new cases. Eur J Neurol. 2012;19:800–11. https://www.ncbi.nlm.nih.gov/pubmed/22221557
Rennebohm RM, Asdaghi N, Srivastava S, Gertner E Guidelines for treatment of Susac syndrome - An update. Int. J. Stroke. 2018: 1747493017751737–1747493017751737. Available at:https://www.ncbi.nlm.nih.gov/pubmed/29319463.
Tomiyasu T, Hirano Y, Suzuki N, Esaki Y, Yasuda Y, Uemura A, et al. Structural and functional analyses of retinal ischemia in eyes with retinal vein occlusion: relationship with macular edema or microaneurysm formation. Ophthalmic Res. 2019;61:218–25. https://www.karger.com/DOI/10.1159/000493489
Acknowledgements
We would like to thank our photographers Mrs. Galit Yair-Pur and Mrs. Oshrat Barzilai.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dinah Zur, Michaella Goldstein, Barequet, D. et al. Susac’s syndrome – A new ocular finding and disease outcome. Eye 36, 781–788 (2022). https://doi.org/10.1038/s41433-021-01464-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01464-7