Abstract
Objective
To assess the diagnostic information provided by digital subtraction dacryocystography (DCG) and dacryoendoscopy in patients with epiphora.
Methods
Sixty-eight lacrimal systems of 34 patients with epiphora were prospectively studied. Patients were initially examined with syringing, followed by digital subtraction DCG and dacryoendoscopy to confirm the diagnosis. Obstructions in lacrimal pathways were evaluated by degree, location, and cause. The weighted kappa coefficient was used to compare the agreement between the tests.
Results
Of the 68 lacrimal pathways, partial or complete obstructions were identified in 56 cases (82.3%) with syringing, in 38 cases (55.9%) with DCG, and in 60 cases (88.2%) with dacryoendoscopy. DCG and dacryoendoscopy showed the same result in 42 of the 68 (61.8%) lacrimal pathways. The weighted kappa value for DCG and dacryoendoscopy was 0.60 (95% CI: 0.40–0.81). The most common sites of obstruction were the common canaliculus (36.7%) and the nasolacrimal duct (28.3%) in dacryoendoscopy. Thirty-three lacrimal pathways (48.5%) were identified to have obstructions on the same level between DCG and dacryoendoscopy. Among the 30 lacrimal pathways (44.1%) that were normal by DCG, obstruction was revealed in 22 cases by dacryoendoscopy, with 11 cases in the common canaliculus. Additional useful information on the cause of obstruction and identification of multiple obstructed sites was provided by dacryoendoscopy.
Conclusions
DCG and dacryoendoscopy showed moderate agreement in detecting lacrimal pathway obstruction. Dacryoendoscopy allowed for comprehensive investigations of the lacrimal pathway and can help explain unidentified factors associated with lacrimal pathway obstruction in patients with epiphora.
Similar content being viewed by others
Introduction
Epiphora is a common symptom encountered in ophthalmic practice and is usually caused by a structural or functional disturbance in the lacrimal pathway. The lacrimal pathway is a continuous anatomical structure consisting of the punctum, canaliculus, lacrimal sac, and nasolacrimal duct (NLD). Partial or complete obstruction of the lacrimal pathway causing epiphora is primarily diagnosed by symptoms and lacrimal syringing. Syringing can be easily performed in the clinic; however, the results are limited by the fact that they are affected by the clinician’s experience and subject’s response.
Various objective investigations including dacryocystography (DCG), lacrimal scintigraphy, and computed tomography (CT) have been proposed to determine the cause of epiphora [1,2,3,4]. Among them, DCG has been most widely used for intuitive visualisation of the lacrimal drainage process and for the identification of lacrimal pathway obstructions. Digital subtraction DCG, a modification of DCG using fluoroscopy, delineates high-quality anatomical detail by producing bone-free images [5, 6]. However, DCG is limited in use due to the need for contrast agents and the inability to visualise anatomical structures beyond the initial obstruction site in the lacrimal pathway.
Recently, dacryoendoscopy has been developed to identify morphological abnormalities of the entire nasolacrimal pathway, including the lacrimal sac and canaliculus. Dacryoendoscopy can directly visualise the degree, level, and nature of an obstruction, and simultaneously treat the obstruction if necessary [7]. The purpose of this study was to evaluate the clinical efficacy of dacryoendoscopy in diagnosing patients with epiphora by comparing its results of the degree, level, and cause of obstruction in lacrimal pathways with those of DCG.
Materials and methods
The protocol and consent forms for the study were approved by the Institutional Review Board of Chung-Ang University Hospital and Yeouido St. Mary’s Hospital of Catholic University (Seoul, Korea), respectively. This was a prospective study in which all procedures were performed under the tenets of the Helsinki Declaration, and informed consent was obtained from all patients before enrolment.
Between June 2017 and November 2018, 68 eyes of 34 patients who visited Chung-Ang University Hospital or Yeouido St. Mary’s hospital of Catholic University with epiphora and who were scheduled to undergo DCG and dacryoendoscopy for diagnosis were recruited for this study. Exclusion criteria included a history of facial trauma, allergy to contrast agents, pregnancy, concurrent lid or ocular disorder including punctal abnormalities, and patients under 19 or over 80 years old. All patients underwent full ophthalmic examinations prior to entry including lid position, tear meniscus height, and dye disappearance test. Lacrimal syringing was performed using a 27-gauge blunt-tipped cannula and was recorded as patent to the nose or as a subjective percentage of reflux through the other punctum. Partial obstruction was defined as a partial reflux through the other punctum with partial flow in the nose. Complete obstruction was defined as total reflux with no flow in the nose or pharynx [8].
DCG was performed by a radiologist on a different day after the clinical evaluation. With the patient supine, local anaesthesia of the conjunctiva was performed. Catheterisation of the inferior punctum of the affected eye was done with a blunt metal cannula. A slow injection of 1–2 mL of a water-soluble contrast medium (iohexol; Bonorex®, Central Medical Service, Seoul, Korea) was carried out while acquiring a series of radiographs. The patient was placed under fluoroscopic control, and bone images were digitally subtracted from the sequence. Partial lacrimal obstruction was defined as either delayed transit time or an area of stenosis anywhere along the lacrimal pathway. Complete obstruction was defined as failure of the contrast agent to reach the inferior meatus of the nasal cavity [8]. The images were assessed by both a radiologist and an ophthalmologist who were blinded to patient information. Obstruction in the lacrimal pathway was evaluated by degree, level, and cause until a consensus was reached by the two examiners.
Dacryoendoscopy was done on a separate day, following the DCG. After instillation of paracaine and infratrochlear anaesthesia, the upper and lower lacrimal puncta were dilated. A dacryoendoscope (FT-201, Fibertech, Tokyo, Japan) was inserted through the upper and lower canaliculus. Saline was injected through the water channel for clear viewing of the lumen. The dacryoendoscope proceeded slowly to the sac and was then held upright and advanced into the NLD under the visual guidance of a monitor screen. In the process, the location and nature of lacrimal obstructions were identified. The obstructed area was opened if possible, followed by silicone tube intubation.
All statistical analyses were performed using R software (version 3.4.0). Data were expressed as mean (SD) for continuous variables, and sample number and percentages for categorical variables. A weighted kappa coefficient with a 95% confidence interval (CI) was used to compare the agreement between the tests. When interpreting kappa values, strength of agreement was described based on Landies and Koch’s classification [9], which includes slight (≤0.20), fair (0.21–0.40), moderate (0.41–0.60), substantial (0.61–0.80), and almost perfect (0.81–1.00) agreement. A value of p < 0.05 was considered statistically significant.
Results
This study included 68 lacrimal pathways of 34 subjects (11 males and 23 females). The mean age was 65.59 (11.08) years, with a range of 33–80 years. The average duration of tearing symptoms was 31.30 (32.52) months (range: 1.0–120.0 months). Out of the 68 lacrimal pathways, partial or complete obstructions were identified in 56 (82.3%) lacrimal pathways with syringing. The remaining 12 lacrimal pathways were normal in syringing but were enrolled in the study due to unknown cause for epiphora or suspected functional NLD obstruction.
Of all the 68 lacrimal pathways, partial or complete obstruction was identified in 38 (55.9%) cases by DCG and in 60 (88.2%) cases by dacryoendoscopy. Of the 56 lacrimal pathways diagnosed with partial or complete obstruction on syringing, 52 had lacrimal pathway abnormalities on the dacryoendoscopic examination, whereas only 38 lacrimal pathways had stenosis or obstruction by DCG (Table 1). Of the 20 lacrimal pathways with complete obstruction in syringing, 13 were diagnosed as complete obstruction in both DCG and dacryoendoscopy, and 4 were partially obstructed in DCG and dacryoendoscopy. In contrast, only 14 of the 36 lacrimal pathways with partial obstruction in syringing were diagnosed with partial lacrimal obstruction by both DCG and dacryoendoscopy. The other 14 lacrimal pathways diagnosed with partial obstruction in syringing were identified as partial obstruction on dacryoendoscopy, but 13 of them were normal in DCG. Twelve lacrimal pathways with normal patency in syringing were also normal by DCG, but eight were identified as partial obstruction on dacryoendoscopy. All of them showed stenosis at the Rosenmüller valve.
The degree of agreement between the tests was then evaluated. Of the 68 lacrimal pathways, 42 exhibited identical results by DCG and dacryoendoscopy, with 61.8% agreement. The weighted kappa value for DCG and dacryoendoscopy was 0.60 (CI: 0.40–0.81). Including syringing, 31 lacrimal pathways showed the identical results by the three diagnostic methods and the agreement was lowered to 45.6%. The weighted kappa value for syringing and DCG was 0.41 (CI: 0.17–0.66), and 0.55 (CI: 0.37–0.73) for syringing and dacryoendoscopy. Thus, the three tests showed moderate agreement, but the lowest agreement was between syringing and DCG.
The common canaliculus was the most common site of obstruction (36.7%) in the lacrimal pathway, followed by the NLD (28.3%) and Krause valve (18.3%) on dacryoendoscopy (Table 2). In contrast, obstructions in the Krause valve (34.2%) and NLD (31.6%) were more common than in the common canaliculus by DCG. Concerning the agreement of examinations in the level of obstruction, 33 lacrimal pathways (48.5%) were identified to have an obstruction at the same level between DCG and dacryoendoscopy. In five lacrimal pathways (7.4%), the localization of the lacrimal obstruction was different. Among the remaining 30 lacrimal pathways (44.1%) that were normal in DCG, the levels of obstruction were revealed in 22 cases by dacryoendoscopy, with 11 cases in the common canaliculus and 6 cases in the NLD.
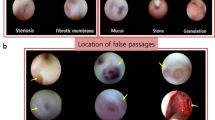
Dacryoendoscopy provided additional information of multiple obstructions in 15 of the lacrimal pathways (Table 3). NLD obstructions were further observed in 7 lacrimal pathways where obstructions were identified in canaliculi or sacs. Multiple obstructions involving the Hasner valve were also found in 5 lacrimal pathways. The causes of obstruction in the lacrimal pathway were also directly identified in dacryoendoscopy. Among 60 eyes with lacrimal insufficiency in Dacryoendoscopy, the most common cause was stenosis in 48 (70.6%) cases, followed by mucus in 5 (7.4%) cases, stones in 4 (5.9%) cases, and granulation in 3 (4.4%) cases. Of the 48 cases with stenosis, 4 were accompanied by mucus.
Discussion
This study tried to verify the diagnostic value of DCG and dacryoendoscopy in patients with epiphora. Our result revealed moderate agreement between DCG and dacryoendoscopy, but dacryoendoscopy and syringing were more consistent than DCG and syringing. Dacryoendoscopy was also preferable in detecting anatomical obstructions compared with DCG. Partial or complete obstruction in lacrimal pathways was identified in 60 of 68 (88.2%) cases with dacryoendoscopy but only in 38 of 68 (55.9%) cases with DCG. Eight of 12 lacrimal pathways with normal patency in syringing were also identified as partial obstruction on dacryoendoscopy. This means the dacryoendoscopy may be more helpful in demonstrating lacrimal pathway abnormalities that may not be evident by other diagnostic modalities. Considering the merits of directly visualising a lesion, the high sensitivity of dacryoendoscopy was quite natural. In addition, the identification of additional obstructed lesions can be done with dacryoendoscopy. Although dacryoendoscopy has several disadvantages, including a high cost and a less durable probe, it can be expected to help identify pathogenic mechanisms of cases of epiphora whose exact cause is unknown by traditional examination, such as functional NLD obstruction [10].
Previous studies have reported sufficient sensitivity and accuracy of DCG in identifying anatomical obstructions of the lacrimal pathway [11,12,13]. Moreover, digital subtraction DCG performed with fluoroscopic control has been reported to provide better reliability than conventional DCG in pinpointing the location of an obstruction [14]. Considering these reports, our results showed a relatively lower sensitivity of DCG than expected. DCG was normal in 18 of 56 lacrimal pathways diagnosed as partial or complete obstruction in syringing. In particular, 16 of 36 lacrimal pathways with partial obstruction in syringing were normal in DCG. All 12 lacrimal pathways that were patent in syringing also showed normal findings in DCG. However, 22 of these 30 lacrimal pathways, which were normal in DCG, were eventually confirmed to have partial obstruction in dacryoendoscopy. Therefore, our study suggested that digital subtraction DCG had little value in diagnosing partial or functional obstruction in the lacrimal pathway [15]. Using dacryoendoscopic findings as standard reference, DCG showed 63.3% sensitivity and 100% specificity. The reason for the low sensitivity of DCG in detecting partial or functional lacrimal obstruction was unclear. One possible explanation may be that the expansion of the lacrimal pathway according to the force of the dye injection may mask clinically significant stenosis or functional disturbance. Although delayed radiography with DCG or three-dimensional helical computed tomographic DCG is recommended as an alternative to identify partial or functional lacrimal obstruction, the accuracy of these methods needs to be verified by dacryoendoscopy [8, 16].
In this study, the most common level of obstruction by DCG was the Krause valve (34.2%), followed by the NLD (31.6%). These findings are consistent with previous reports that the junction of the lacrimal sac and NLD was the most common site of obstruction in DCG [17, 18]. In contrast, obstruction in the common canaliculus was more common than in the NLD or Krause valve in dacryoendoscopy. Dacryoendoscopy also revealed obstructions of the common canaliculus in 11 of the 30 lacrimal pathways which were patent in DCG, suggesting that DCG may be more likely to miss lesions in the common canaliculus. It is presumed that the anatomy of the lacrimal pathway, with the small diameter of the canaliculus and the Rosenműller valve, might be a possible explanation for the relatively lower detection of common canalicular lesions by DCG. A previous study also indicates that the delineation of the common canaliculus is less clear compared with the sac and NLD by DCG [19].
The importance of diagnostic syringing is well-known in evaluating epiphora. Nevertheless, syringing is often considered less valuable as an isolated modality than in combination with other examinations in diagnosing lacrimal pathway obstruction [6, 20]. Although this study was not intended to explore the diagnostic value of syringing, the clinical utility of syringing could be assessed based on the results of dacryoendoscopy. In this study, 52 of 56 eyes that showed lacrimal insufficiency in syringing were confirmed as having lacrimal stenosis or an obstruction on dacryoendoscopy. This result corresponds to 86.7% sensitivity and 92.9% positive predictive value, suggesting that syringing is a reliable screening test to detect lacrimal pathway obstruction in patients with epiphora. However, it is difficult to differentiate between complete and partial lacrimal obstruction with syringing, since only 44 of 56 eyes diagnosed with lacrimal pathway obstruction by syringing exhibited the same complete or partial lacrimal obstruction through dacryoendoscopy. Thus, if partial or functional obstruction was suspected by syringing, it would be better to identify the cause of tearing through dacryoendoscopy rather than performing an additional DCG to confirm any blockages in the lacrimal pathway.
Stenosis was the most common cause of lacrimal pathway obstruction, followed by mucus and stones in our study. Stenosis, which refers to abnormal narrowing or contraction of the lacrimal pathway, is presumed to be the result of chronic inflammation and fibrosis with remodelling of connective tissue fibre [21]. During dacryoendoscopy, stenotic lumens were widened using a probe. Mucus or stones in the lacrimal pathway could also be removed directly using mechanical force with the probe under direct visualisation with the dacryoendoscope. Another advantage of dacryoendoscopy is that it can be used to simultaneously diagnose and treat the cause of lacrimal pathway obstruction.
The limitation of this study was that much of the data provided by this study was qualitative in nature and based on subjective interpretations of images. To overcome these limitations, DCG was interpreted by both a radiologist and an ophthalmologist in blinded state. However, the dacryoendoscopic video images could not be interpreted by a blinded examiner due to their relatively low resolution and poor magnification. The resolution of the dacryoendoscopy used was still not good enough to fully visualise the entire lumen of the lacrimal pathway. Technical improvements such as an external monitor and scope fibre with increased resolution will help overcome this limitation.
In conclusion, the present study comprehensively evaluated and simultaneously compared DCG and dacryoendoscopic findings to evaluate their impact on the diagnosis of epiphora. DCG is less sensitive in diagnosing partial or functional obstruction in the lacrimal pathway and needs to be employed only in limited situations, not in routine examinations. Dacryoendoscopy allowed for comprehensive investigation of the lacrimal pathway and can help explain unidentified factors associated with the lacrimal pathway in patients with epiphora.
Summary
What was known before
-
Dacryocystography has been the most widely used imaging technique to identify the cause of epiphora.
-
Dacryoendoscopy can directly visualise the degree, level, and nature of an obstruction, and simultaneously treat the obstruction if necessary.
What this study adds
-
Dacryocystography had little value in diagnosing partial or functional obstruction in the lacrimal pathway and might be more likely to miss a lesion in the common canaliculus.
-
Dacryoendoscopy was preferable in detecting anatomical obstructions compared with dacryocystography and provided additional information on the cause of obstruction and identification of multiple obstructed sites.
References
Montanara A, Catalino P, Gualdi M. Improved radiological technique for evaluating the lacrimal pathways with special emphasis on functional disorders. Acta Ophthalmol (Copenh). 1979;57:547–63.
Detorakis ET, Zissimopoulos A, Ioannakis K, Kozobolis VP. Lacrimal outflow mechanisms and the role of scintigraphy: current trends. World J Nucl Med. 2014;13:16–21.
Ashenhurst M, Jaffer N, Hurwitz JJ, Corin SM. Combined computed tomography and dacryocystography for complex lacrimal problems. Can J Ophthalmol. 1991;26:27–31.
Papathanassiou S, Koch T, Suhling MC, Lenarz T, Durisin M, Stolle SRO, et al. Computed tomography versus dacryocystography for the evaluation of the nasolacrimal duct-a study With 72 patients. Laryngoscope Investig Otolaryngol. 2019;4:393–8.
Galloway JE, Kavic TA, Raflo GT. Digital subtraction macrodacryocystography. A new method of lacrimal system imaging. Ophthalmology. 1984;91:956–62.
Saleh GM, Gauba V, Tsangaris P, Tharmaseelan K. Digital subtraction dacryocystography and syringing in the management of epiphora. Orbit. 2007;26:249–53.
Sasaki T, Nagata Y, Sugiyama K. Nasolacrimal duct obstruction classified by dacryoendoscopy and treated with inferior meatal dacryorhinotomy. Part I: Positional diagnosis of primary nasolacrimal duct obstruction with dacryoendoscope. Am J Ophthalmol. 2005;140:1065–9.
Freitag SK, Woog JJ, Kousoubris PD, Curtin HD. Helical computed tomographic dacryocystography with three-dimensional reconstruction: a new view of the lacrimal drainage system. Ophthalmic Plast Reconstr Surg. 2002;18:121–32.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159–74.
Takahashi Y, Nakamura Y, Kakizaki H. Dacryoendoscopic findings in the lacrimal passage in failed dacryocystorhinostomy. Ophthalmic Plast Reconstr Surg. 2013;29:373–5.
Irfan S, Cassels-Brown A, Nelson M. Comparison between nasolacrimal syringing/probing, macrodacryocystography and surgical findings in the management of epiphora. Eye (Lond). 1998;12(Pt 2):197–202.
Cibis GW, Spurney RO, Waeltermann J. Radiographic visualization of congenital lacrimal sac mucoceles. Ann Ophthalmol. 1986;18:68–9.
Manfre L, de Maria M, Todaro E, Mangiameli A, Ponte F, Lagalla R. MR dacryocystography: comparison with dacryocystography and CT dacryocystography. AJNR Am J Neuroradiol. 2000;21:1145–50.
Sousa PC, Pinto P, Leite E, Cunha-Vaz JG. Morphological and/or functional imagiology diagnosis of epiphora. Doc Ophthalmol. 1993;83:337–48.
Guzek JP, Ching AS, Hoang TA, Dure-Smith P, Llaurado JG, Yau DC, et al. Clinical and radiologic lacrimal testing in patients with epiphora. Ophthalmology. 1997;104:1875–81.
Wearne MJ, Pitts J, Frank J, Rose GE. Comparison of dacryocystography and lacrimal scintigraphy in the diagnosis of functional nasolacrimal duct obstruction. Br J Ophthalmol. 1999;83:1032–5.
Nahata MC. Dacryocystography in diseases of the lacrimal SAC. Am J Ophthalmol. 1964;58:490–3.
Francisco FC, Carvalho AC, Francisco VF, Francisco MC, Neto GT. Evaluation of 1000 lacrimal ducts by dacryocystography. Br J Ophthalmol. 2007;91:43–6.
Nixon J, Birchall IW, Virjee J. The role of dacryocystography in the management of patients with epiphora. Br J Radio. 1990;63:337–9.
Conway ST. Evaluation and management of “functional” nasolacrimal blockage: results of a survey of the American Society of Ophthalmic Plastic and Reconstructive surgery. Ophthalmic Plast Reconstr Surg. 1994;10:185–7.
Ali MJ, Paulsen F. Human lacrimal drainage system reconstruction, recanalization, and regeneration. Curr Eye Res. 2020;45:241–52.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This study was funded by Sung Wha medical Inc. (Seoul, Korea) – the seller of dacryoendoscope. The sponsor had no role in the design of the study, collection and analysis of data and decision to publish. The authors have no other conflicts of interest to disclose.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bae, S.H., Park, J. & Lee, J.K. Comparison of digital subtraction dacryocystography and dacryoendoscopy in patients with epiphora. Eye 35, 877–882 (2021). https://doi.org/10.1038/s41433-020-0990-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-0990-1
This article is cited by
-
Soft stop on syringing and probing may have a high false-positive rate in diagnosing pre-sac obstruction
International Ophthalmology (2022)
-
Syringing has limited reliability in differentiating nasolacrimal duct stenosis from functional delay
Graefe's Archive for Clinical and Experimental Ophthalmology (2022)