Abstract
Objective
To compare the surgical outcomes of 1-disc diameter (DD) and 2-DD conventional internal limiting membrane peeling (C-ILMP) in large full-thickness macular holes (FTMHs).
Materials and methods
A prospective randomized controlled trial. One hundred patients with large idiopathic full-thickness macular hole (FTMH) were randomized into C-ILMP and extended C-ILMP (EC-ILMP) groups. The primary outcome was closure rate at 6 months after surgery. Secondary outcomes were visual acuity (VA), closure type, consequence of ILMP and complications.
Results
The mean symptom duration was 12.19 ± 9.64 months. Mean preoperative VA was 1.25 ± 0.37 logMAR. The average minimum linear diameter was 633.05 ± 129.82 µm and basal linear dimension was 1158.49 ± 249.07 µm. The two groups did not differ in term of demographic data. Closure rate was significantly higher in the EC-ILMP group (76.47% vs. 51.02%, 95% CI 7.24–43.66; p = 0.008). There were also no significant differences in closure type, central foveal thickness, dissociated optic nerve fibre layer detection, or change in fovea-to-disc distance. There were also no significant differences in postoperative VA (p = 0.069) or visual improvement (mean 0.39 ± 0.43 logMAR; p = 0.286). According to subgroup analysis, EC-ILMP resulted in a higher closure rate in patients with chronic FTMH for >6 months, (p = 0.008). Furthermore, EC-ILMP resulted in better anatomical closure and visual result in patients with FTMH with macular hole closure index ≤0.5, p = 0.003 and p = 0.010, respectively.
Conclusion
Extended C-ILMP yielded a significantly higher closure rate in large FTMHs, but visual outcome did not differ significantly. According to subgroup analysis, extended C-ILMP was more effective in chronic large FTMH with MHCI ≤ 0.5.
Similar content being viewed by others
Introduction
The standard treatment for large full-thickness macular holes (FTMHs) is pars plana vitrectomy (PPV) combined with internal limiting membrane peeling (ILMP) and intravitreal gas tamponade [1]. Although there is no general consensus regarding the optimal extent of the internal limiting membrane (ILM) to be peeled, many surgeons peel an area with a radius of 1-disc diameter (DD) [2, 3]. Both sulfur hexafluoride (SF6) and perfluoropropane (C3F8) appear to have achieved similar outcomes and risk of adverse events [4]. In cases of FTMH is >400 µm, postoperative facedown positioning had significant benefit on successful hole closure [5]. Despite advances in surgical techniques and technology, large chronic FTMH remains a challenge for retinal surgeons. Several surgical techniques have been introduced to improve outcomes in these cases such as extended ILMP, inverted flap ILMP and temporal macular arcade retinotomy [6]. Al Sabti et al. reported the first successful use of extended ILMP (up to arcade) to treat the large macular holes in 2009 [7]. Although there have been many randomized controlled trials (RCT) involving extended ILMP, all of these have included FTMHs at all stages [8,9,10].
The purpose of this prospective RCT was thus to determine whether conventional ILMP (C-ILMP) area affects the outcomes of macular hole surgery in patients with large idiopathic macular holes.
Materials and methods
This prospective randomized controlled trial was performed at the Khon Kaen University Eye Center, at Srinagarind Hospital, in Thailand. The study protocol was approved by the institutional review board and Khon Kaen University Ethics Committees in Human Research (IRB no. 00001189). The study adhered to the Consolidated Standards of Reporting Trials (CONSORT) statement and was registered in the Thai Clinical Trials Registry (identifier: TCTR20180719001). The procedures conformed to the tenets of the Declaration of Helsinki. The Invitation Research Fund had no role in this study.
Patient eligibility
Patients with large idiopathic FTMH who underwent surgery were recruited between July 2018 and July 2019. For patients with bilateral FTMH, only one eye was enrolled. Written informed consent was obtained from all subjects before enrolment.
Inclusion criteria included (1) age >50 years, (2) FTMH with a minimum linear diameter (MLD) >400 µm confirmed by spectral-domain optical coherent tomography (SD-OCT) (Spectralis, Heidelberg Engineering, Heidelberg, Germany), and (3) 6 months of follow-up. Exclusion criteria included (1) refractive error ≥3 dioptres, (2) Secondary FTMH such as traumatic macular hole, (3) glaucoma, (4) macular scarring, (5) media opacities resulting in poor OCT image quality, (6) macular hole-induced retinal detachment, (7) history of traumatic eye or head injury, (8) previous vitreoretinal disorder,(9) previous vitreoretinal surgery and (10) need general anaesthesia.
Randomization and masking procedures
Participants were randomly allocated to the C-ILMP group (1 DD radius of C-ILMP) and the extended C-ILMP (EC-ILMP) group (2 DD radii of C-ILMP) at a 1:1 ratio using a varying blocked randomization generator. The registration centre assigned the intervention and provided the fundus photography with outlined ILMP area in circle to the surgeon. All patients, technicians and examining ophthalmologists were masked to treatment allocation throughout the study. Only the surgeon was unmasked, but she did not participate in the postoperative evaluations.
Surgical procedures
All patients underwent standard 23-guage three-port PPV performed by one surgeon (SS). After trypan blue and brilliant blue staining (Membrane Blue-Dual, DORC, Zuidland, Netherlands) for 1 min, C-ILMP was performed with an approximate radius of either 1 or 2 DD surrounding the FTMH based on preoperative contoured fundus pictures. Intravitreal gas tamponade was performed with 20% sulphur hexafluoride (SF6). Patients were instructed to remain in a facedown position for 1–2 weeks depending on the surgical outcomes at 1 week postoperatively. If the FTMH was not closed, the patient was asked to maintain the posture for another week. Phacovitrectomy was conducted in patients with cataract. If the macular hole remained unclosed after the primary procedure, the patients were advised to undergo reoperation consisting of more extensive C-ILMP as soon as possible.
Patient evaluation
Participants were assessed at baseline and then at 1, 3 and 6 months after surgery. Demographic data were recorded including sex, age, duration of symptoms (from the onset of symptoms reported by patients until date of surgery) and lens status. Complete ophthalmic examinations were performed at baseline, including best-corrected visual acuity (BCVA), slit-lamp biomicroscopy, intraocular pressure measurement, indirect ophthalmoscopy and optical coherent tomography (OCT). The minimum linear diameter was defined as FTMH size when the horizontal SD-OCT scan passed through the centre of the macular hole. We also measured basal linear diameter (BLD) and calculated the macular hole closure index (MHCI). The MHCI was calculated as the sum length of the detached photoreceptor arms divided by BLD (Fig. 1). The detached photoreceptor arm was defined as a straight line from the broken end point of the external limiting membrane to the junction of the detached photoreceptors with retinal pigment epithelium. The disc-to-fovea distance (DFD) was measured from the centre of fovea to a landmark at the temporal disc margin. The foveal centre of FTMH was guided by OCT. The end of the half-length of the BLD was the centre of fovea. All lengths were measured using Spectralis software’s built-in callipers. Vitreomacular interface (VMI) abnormalities such as epimacular membrane and vitreomacular traction were also evaluated using OCT imaging. At each follow-up visit, BCVA and SD-OCT were performed. Any adverse events were evaluated and recorded.
Outcome measures
The primary outcome was the anatomical closure at 6 months after surgery. The secondary outcomes were postoperative BCVA, closure type, central foveal thickness (CFT), change of DFD distance, detection of dissociated optic nerve fibre layer (DONFL) and related adverse events. Based on a previous study, we classified the macular hole closure at 6 months after treatment into four types (1) regular foveal contour (U-type), (2) steep foveal contour (V-type), (3) irregular foveal contour (Irregular or W-type), and (4) unclosed macular hole or open type (Fig. 2) [11]. The masked ophthalmologists evaluated the type of closure, CFT, DFD and DONFL. In cases of anatomical closure, the thinnest fovea on the OCT scan was measured. If there was disagreement, a final closure type classification was made by two of the three evaluators.
Statistical analysis
A sample size calculation for detecting 20% difference was applied to compare OCT-based anatomical closures at 6 months with a power of 80%. The resulting estimated required sample size was 45 eyes per group. With an expected 15% protocol non-compliance rate, the final estimate for enrolment consisted of 52 patients per group. Analyses were performed on an intention-to-treat basis by an independent statistician using Stata version 10.1 (StataCorp LP College Station, Texas, USA). Fisher’s exact and chi-square tests were used to analyse categorical variables. A Wilcoxon rank sum test and t-test were used to analyse continuous variables. P values < 0.05 indicated statistical significance.
Results
Baseline characteristics and patient disposition
A total of 122 consecutive patients with idiopathic FTMH were assessed, but 18 did not meet inclusion criteria. The causes for exclusion were media opacity (5 eyes), high myopia (4 eyes), traumatic FTMH (4 eyes), perifoveal scarring (2 eyes), macular hole-induced retinal detachment (2 eyes) and the need for general anaesthesia (1 eye). Six of the 104 participants had bilateral FTMHs. The mean duration of symptoms was 12.19 ± 9.64 months, with a range of 2–72 months. The majority of patients (80.77%) experienced symptoms for over 6 months and six had had symptoms for more than 24 months. In 12 out of the 20 patients with symptoms for ≤6 months, FTMH was detected after an uneventful phacoemulsification before referral. As four patients were lost to follow-up, the final analysis included 49 eyes in the C-ILMP group and 51 eyes in the EC-ILMP group (Fig. 3). Patients’ demographic and clinical characteristics are presented in Table 1. No significant differences between the two groups in any baseline variables were observed and detected complications were comparable. The most common complication was secondary cataract; however, there was only one patient with significant cataract that caused a reduction in OCT quality image. The patient was in the C-ILMP group and underwent phacoemulsification at 5 months.
Anatomical outcome
Complete closure of FTMH was achieved in 64 eyes. In most cases, the hole was closed within the first month. There were only two patients whose FTMH closed at 3 months. The closure rate was significantly higher in the EC-ILMP group (76.47% vs. 51.02%, 95% CI 7.24–43.66; p = 0.008). After the stratification of chronicity, we found that EC-ILMP resulted higher closure rate in chronic FTMH (>6 months; 95% CI 8.64–50.40, p = 0.008). According to subgroup analysis, EC-ILMP resulted in significantly better visual outcome in FTMH with preoperative MHCI ≤ 0.5 (95% CI 9.09–54.24, p = 0.004), but not in FTMH with preoperative MHCI > 0.5 (p = 0.778). The closure types in patients with anatomical success were V-type 48.44%, U-type 35.94% and W-type 15.62%. Closure type did not significantly differ between the two groups (Table 2). Only two patients with unclosed hole in the C-ILMP group decided to undergo second operation within 2–3 months after acknowledgement of the risks and benefits, and the hole closure was achieved after extended ILMP to arcade in both cases. No reopening occurred during the follow-up period.
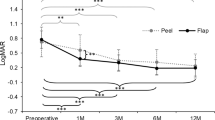
Visual outcome
BCVA improved from a mean ± SD value of 1.25 ± 0.37 before vitrectomy to 0.85 ± 0.32 at 6 months postoperatively; average visual improvement was 0.39 ± 0.43 logMAR. The average visual improvement in patients with anatomical success was 0.51 ± 0.44 logMAR. There was no statistically significant difference in postoperative VA and visual improvement at 6 months after vitrectomy between the C-ILMP and EC-ILMP groups; p = 0.096, p = 0.292 and p = 0.898 respectively. After adjustment with phacovitrectomy; p values were 0.069, 0.286 and 0.581, respectively. According to subgroup analysis, EC-ILMP resulted in significantly better visual outcome in FTMH with preoperative MHCI ≤ 0.5 (95% CI −0.35 to −0.07, p = 0.003; Table 2). The causes of visual deterioration were unclosed hole, secondary cataract and wide photoreceptor loss.
Discussion
ILMP has been proven to improve the closure rate of FTMHs when combined with vitrectomy and gas tamponade [12]. The closure rate is as high as 90–100%, but the outcomes in certain types of macular holes remain unsatisfactory [13]. Large hole size, chronic macular hole (>6 months duration), myopia, trauma, associated with retinal detachment, inability to keep prone position, residual epiretinal membrane all contribute to failed closure on the first attempt or the development of persistent macular holes [6], making FTMH diameter an important issue that can affect outcomes. Williamson and Lee reported closure rates in Gass stage 2 and stage 3 holes to be 73% and 56.3% respectively [14]. Ip et al. reported a closure rate of 56% in FTMHs with diameter greater than 400 µm [15]. As the closure rate is lower in large FTMHs, previous studies have examined modifications to the standard technique such as extended ILMP and autologous transplantation of ILM [6, 16]. Most of these techniques aim to stimulate an inflammatory process for inducing gliosis and hole closure. However, there is yet no general consensus regarding standard surgical treatment for large FTMH due to the lack of RCT with an adequate sample sizes.
Previous publications of extended ILMP with diameter ranging from 1.5 to 4 DD, have been described at all Gass stages FTMH [8,9,10] and have found no statistical difference in anatomical closure. Modi et al. demonstrated a significantly lower closure rate in patients who underwent extended 5-mm ILMP than those who underwent 3-mm ILMP (65% vs.80%), as well as worse visual outcome [9]. Due to the majority of these cases were stage 2 and 3 FTMHs, this suggests that the extended ILMP may be unnecessary for treatment of small to medium FTMHs. We hypothesize that there may be a minimum ILMP area for a set size of macular hole in order to permit hole closure [17].
This study is the first prospective RCT to evaluate the influence of EC-ILMP in large macular holes. We followed a new OCT-based classification system proposed by the International Vitreoretinal Traction Study Group which classifies FTMHs whose narrowest horizontal linear width are >400 um as “large macular holes” [18]. Our patients were enrolled from a single referral centre and operated on by one retina surgeon (SS).
The closure rate of FTMHs in our study was 64%, with 51.02% in the C-ILMP group and 76.47% in the EC-ILMP group. We hypothesized that a broader ILMP area would be better able to relieve the tangential mechanical forces on large FTMHs. The closure rate in the EC-ILMP group was lower than those reported in previous studies; mainly due to longer duration, lower preoperative VA and larger hole size [8, 10]. Previous studies in which ILMP was performed with a 1 DD radius 2 DD diameter) in large macular holes yielded anatomical success rate ranging from 70 to 91.6%. Furthermore, these studies demonstrated that inverted flap ILMP had statistically similar anatomical success and visual outcome to C-ILMP in large macular holes [19,20,21]. Michalewska et al. reported an 88% closure rate in patients undergoing C-ILMP and a mean duration of symptoms was 19 months (6 months–3.5 years), which was comparable to our study. However, the preoperative VA in previous study was much better (0.9 vs. 1.26 logMAR) [19]. Velez-Montoya et al. conducted a double-masked RCT to compare the surgical outcomes of inverted flap ILMP, free flap ILMP, and C-ILMP in large macular holes and found no significant differences in closure rates among groups. The closure rate in the C-ILMP group in that study was much higher than that found in our study (91.6%). When considering baseline data and clinical characteristics of their patients, the subjects in our study had much longer duration of symptoms (3.85 ± 1.8 vs. 10.20 ± 6.78 months) and lower preoperative VA (0.93 ± 0.5 vs. 1.25 ± 0.37 logMAR) [20]. Kannan et al. performed an RCT to compare the outcomes of inverted flap ILMP and C-ILMP in FTMH with MLD >600 µm and found no statistically significant difference between groups in term of anatomical success and functional outcomes. Macular hole closure was observed in 70% of patients in the C-ILMP group (higher than in our study), but duration of symptoms was not reported [21]. This suggests that there are many factors that can affect the surgical outcomes in cases of large FTMH such as duration of symptoms, preoperative VA, and hole size. In patients with chronic FTMH (>6 months), we found that the closure rate was significantly higher in the EC-ILMP group (p = 0.008) although the postoperative BCVA did not differ significantly. In large holes with preoperative MHCI ≤ 0.5, we found that EC-ILMP resulted in a significantly higher closure rate (p = 0.010) and better visual outcome (p = 0.003) than C-ILMP, findings comparable to those reported by Yao et al. [10]. This indicates that EC-ILMP had more benefit of anatomical outcome in chronic large FTMHs with MHCI ≤ 0.5. Although Michalewska et al. demonstrated that the most common closure type of FTMHs was U-type (53.45%), we found that V-type closure was the most common closure type of large idiopathic FTMHs (48.48%) [11]. In our study, U-type closures were most common in the C-ILMP group (44%) whereas V-type closures were most common in the EC-ILMP group (56.41%).
ILMP has a number of potential detrimental consequences, some of which relate to the surgeon’s experience. Swelling of the arcuate retinal nerve fibre layer or DONFL was the earliest short-term anatomical change on SD-OCT [22]. The DONFL is observed as small dimpling of the disaggregated nerve fibre layer on SD-OCT and dark dots or lines on the red free image that may be caused by irregularly distributed Muller cells following ILMP [23]. Steel et al. found that a greater ILMP area was associated with a greater number of dimples on en face OCT [17]. However, it is unclear whether it has functional consequences. We found no significant difference in DONFL detection postoperatively between C-ILMP and EC-ILMP groups at any follow-up visits (p = 0.466). However, en face OCT will provide more information than SD-OCT, especially with regard to the absolute number of dimples and their density.
A variety of morphologic changes occur after ILMP, including a movement of the fovea toward the optic nerve head, which has been associated with thickening of the nasal retina and thinning of the temporal retina [24]. Steel et al. demonstrated that a greater ILMP area was associated with greater change in DFD, but we did not find any statistically significant difference in DFD change between the C-ILMP and EC-ILMP groups [17]. The majority of cases (76%) showed the shortening of DFD postoperatively and we discovered that the retinal displacement was either toward or outward the optic disc. Change in DFD varied widely from −726 to +528 µm. Furthermore, the epiretinal membrane was not associated with more retinal displacement as was mentioned in a previous study [25].
Good postoperative VA is correlated with U-shape closure, normal foveal thickness and absence of photoreceptor layer defects [11]. The mean preoperative VA reported in large macular holes in previous publications has usually been ≤1 logMAR, but the mean preoperative VA in our patients was 1.25 ± 0.37 logMAR, which was the lowest baseline VA ever reported [19,20,21]. Visual improvement after C-ILMP with a 1 DD radius (2 DD diameter) has been reported as being between 0.16 and 0.21 logMAR [19,20,21]. In our study, the average visual improvement at 6 months was 0.35 ± 0.42 logMAR in the C-ILMP group. In patients with anatomical closure, VA improved by 0.50 ± 0.37 logMAR, although the mean postoperative CFT was only 152.24 ± 50.77 µm. We found that EC-ILMP provided significantly better visual outcome than C-ILMP in large holes with preoperative MHCI ≤ 0.5 (p = 0.003), but not in large FTMHs with MHCI > 0.5. However, we did not measure the length of postoperative photoreceptor layer defect in closed FTMH, which may be associated with visual outcome.
For recurrent or recalcitrant macular holes, early repeat vitrectomy with extension of the ILMP remains the optimal and most straightforward surgical technique to achieve secondary closure [6]. A recent meta-analysis showed that the probability of anatomical closure was 71–84% and that of ≥2 line visual improvement was 45–71% after the second procedure in FTMHs with primary failure [26]. Thus, for patients in whom primary macular hole closure has failed, repeated surgery should be considered. Unfortunately, only two patients with unclosed FTMH in the C-ILMP group decided to undergo the second operation. However, V-shape closures were achieved in these patients after reoperation with PPV and extending ILMP to the vascular arcade.
Large idiopathic macular holes present significant surgical challenges. Our study demonstrated that ILMP with a 2 DD radius resulted in a higher closure rate than that with a 1 DD radius, but there was no significant difference between the two in terms of visual outcome. Extended ILMP yielded better results in chronic large FTMH with MHCI ≤ 0.5. Advanced technology such as en face OCT, intraoperative OCT, and retinal vascularity programme analysis will provide more information regarding biomarkers, intraoperative change and the effect of ILMP on retinal pathology and morphology which may lead to a better understanding of predictive factors of surgical outcomes. Further studies are needed to evaluate the optimal surgical technique and minimum ILMP area in chronic large FTMH.
Summary
What was known before
-
Large full-thickness macular hole (FTMH) remains a challenge for retinal surgeons.
-
Many surgical techniques have been introduced to improve outcome such as extended internal limiting membrane peeling (ILMP) and inverted-flap ILMP.
-
There are many randomized controlled trial (RCT) of extended ILMP, but all publications included all stages of FTMH.
What this study adds
-
First RCT of extended ILMP in large FTMH.
-
Lowest baseline visual acuity ever been reported and >80% of cases are chronic FTMH (>6 months).
-
We also measured macular hole closure index (MHCI) and evaluate the consequence of ILMP such as change of disc-to-foveal distance and detection of dissociated optic nerve fibre layer (DONFL).
-
Extended ILMP could achieve higher closure rate especially in chronic large FTMH with MHCI < 0.5, but no significant difference in visual outcome.
References
Parravano M, Giansanti F, Eandi CM, Yap YC, Rizzo S, Virgili G. Vitrectomy for idiopathic macular hole. Cochrane Database Syst Rev. 2015;5:CD009080.
Almony A, Nudleman E, Shah GK, Blinder KJ, Eliott DB, Mittra RA, et al. Techniques, rationale, and outcomes of internal limiting membrane peeling. Retina. 2012;32:877–91.
Abdelkader E, Lois N. Internal limiting membrane peeling in vitreo-retinal surgery. Surv Ophthalmol. 2008;53:368–96.
Hecht I, Mimouni M, Blumenthal EZ, Barak Y. Sulfur hexafluoride (SF6) versus perfluoropropane (C3F8) in the intraoperative management of macular holes: a systematic review and meta-analysis. J Ophthalmol. 2019;2019:1820850.
Xia S, Zhao XY, Wang EQ, Chen YX. Comparison of face-down posturing with nonsupine posturing after macular hole surgery: a meta-analysis. BMC Ophthalmol. 2019;19:34.
Tam ALC, Yan P, Gan NY, Lam WC. The current surgical management of large, recurrent, or persistent macular holes. Retina. 2018;38:1263–75.
Al Sabti K, Kumar N, Azad RV. Extended internal limiting membrane peeling in the management of unusually large macular holes. Ophthalmic Surg Lasers Imaging. 2009;40:185–7.
Bae K, Kang SW, Kim JH, Kim SJ, Kim JM, Yoon JM. Extent of internal limiting membrane peeling and its impact on macular hole surgery outcomes: a randomized trial. Am J Ophthalmol. 2016;169:179–88.
Modi A, Giridhar A, Gopalakrishnan M. Comparative analysis of outcomes with variable diameter internal limiting membrane peeling in surgery for idiopathic macular hole repair. Retina. 2017;37:265–73.
Yao Y, Qu J, Dong C, Li X, Liang J, Yin H, et al. The impact of extent of internal limiting membrane peeling on anatomical outcomes of macular hole surgery: results of a 54-week randomized clinical trial. Acta Ophthalmol. 2019;97:303–12.
Michalewska Z, Michalewski J, Cisiecki S, Adelman R, Nawrocki J. Correlation between foveal structure and visual outcome following macular hole surgery: a spectral optical coherence tomography study. Graefes Arch Clin Exp Ophthalmol. 2008;246:823–30.
Spiteri Cornish K, Lois N, Scott N, Burr J, Cook J, Boachie C, et al. Vitrectomy with internal limiting membrane peeling versus vitrectomy with no peeling for idiopathic full-thickness macular hole. Cochrane Database Syst Rev. 2013;6:CD009306.
Zhao PP, Wang S, Liu N, Shu ZM, Zhao JS. A review of surgical outcomes and advances for macular holes. J Ophthalmol. 2018;2018:7389412.
Williamson TH, Lee E. Idiopathic macular hole: analysis of visual outcomes and the use of indocyanine green or brilliant blue for internal limiting membrane peel. Graefes Arch Clin Exp Ophthalmol. 2014;252:395–400.
Ip MS, Baker BJ, Duker JS, Reichel E, Baumal CR, Gangnon R, et al. Anatomical outcomes of surgery for idiopathic macular hole as determined by optical coherence tomography. Arch Ophthalmol. 2002;120:29–35.
Morizane Y, Shiraga F, Kimura S, Hosokawa M, Shiode Y, Kawata T, et al. Autologous transplantation of the internal limiting membrane for refractory macular holes. Am J Ophthalmol. 2014;157:861–9.
Steel D, Chen Y, Latimer J, White K, Avery P. Does internal limiting membrane peeling size matter? J Vitreoretin Dis. 2017;1:27–31.
Duker JS, Kaiser PK, Binder S, de Smet MD, Gaudric A, Reichel E, et al. The International Vitreomacular Traction Study Group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology. 2013;120:2611–9.
Michalewska Z, Michalewski J, Adelman RA, Nawrocki J. Inverted internal limiting membrane flap technique for large macular holes. Ophthalmology. 2010;117:2018–25.
Velez-Montoya R, Ramirez-Estudillo JA, Liano CSG, Bejar-Cornejo F, Sanchez-Ramos J, Guerrero-Naranjo JL, et al. Inverted ILM flap, free ILM flap and conventional ILM peeling for large macular holes. Int J Retin Vitreous. 2018;4:1–9.
Kannan NB, Kohli P, Parida H, Adenuga OO, Ramasamy K. Comparative study of inverted internal limiting membrane (ILM) flap and ILM peeling technique in large macular holes: a randomized-control trial. BMC Ophthalmol. 2018;18:177.
Gu C, Qiu Q. Inverted internal limiting membrane flap technique for large macular holes; a systemic review and single-arm meta-analysis. Graefes Arch Clin Exp Ophthalmol. 2018;256:1041–9.
Clark A, Balducci N, Pichi F, Veronese C, Morara M, Torrazza C, et al. Swelling of the arcuate nerve fiber layer after internal limiting membrane peeling. Retina. 2012;32:1608–13.
Ishida M, Ichikawa Y, Higashida R, Tsutsumi Y, Ishikawa A, Imamura Y. Retinal displacement toward optic disc after internal limiting membrane peeling for idiopathic macular hole. Am J Ophthalmol. 2014;157:971–7.
Rodrigues IA, Lee EJ, Williamson TH. Measurement of retinal displacement and metamorphopsia after epiretinal membrane or macular hole surgery. Retina. 2016;36:695–702.
Reid GA, McDonagh N, Wright DM, Yek JTO, Essex RW, Lois N. First failed macular hole surgery or reopening of a previously closed hole: Do we gain by reoperating?-A Systematic Review and Meta-analysis. Retina. 2020;40:1–15.
Acknowledgements
The authors would like to thank Dr. Watcharaporn Thongmee for illustrating the figures and Dr. Sasinun Pipatbanditsakul for helping in data collection. The authors would like to thank Dr. Kaewjai Thepsuthammarat, Clinical Epidemiology Unit, Faculty of Medicine, Khon Kaen University for statistical analyses. We would like to acknowledge Dr. Dylan Southard for the English language editing of this manuscript via the KKU Publication Clinic (Thailand).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sinawat, S., Srihatrai, P., Sutra, P. et al. Comparative study of 1 DD and 2 DD radius conventional internal limiting membrane peeling in large idiopathic full-thickness macular holes: a randomized controlled trial. Eye 35, 2506–2513 (2021). https://doi.org/10.1038/s41433-020-01259-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01259-2