Abstract
This review aims to collect the proposed surgical techniques for treating full thickness macular hole (FTMH) refractory to pars plana vitrectomy and internal limiting membrane (ILM) peeling and to analyse and compare anatomical and functional outcomes in order to evaluate their efficacy. The articles were grouped according to the surgical techniques used. Refractory FTMH closure rate and best-corrected visual acuity (BCVA) gain were the two analysed parameters. Thirty-six articles were selected. Ten surgical technique subgroups were defined: autologous platelet concentrate (APC); lens capsular flap transplantation (LCFT); autologous free ILM flap transplantation (free ILM flap); enlargement of ILM peeling, macular hole hydrodissection (MHH), autologous retinal graft (ARG), silicon oil (SO), human amniotic membrane (hAM), perifoveal relaxing retinotomy, arcuate temporal retinotomy. Refractory FTMH closure rate was similar among subgroups, not significant heterogeneity emerged (p = 0.176). BCVA gain showed a significant dependence on surgical technique (p < 0.0001), significant heterogeneity among subgroups emerged (p < 0.0001). Three sets of surgical technique subgroups with a homogeneous BCVA gain were defined: high BCVA gain (hAM); intermediate BCVA gain (APC, ARG, LCFT, MHH, SO); low BCVA gain (free ILM flap, enlargement of peeling, arcuate temporal retinotomy). In terms of visual recovery, the most efficient technique for treating refractory FTMH is hAM, lens capsular flap and APC that allow to obtain better functional outcomes than free ILM flap. MHH, ARG, perifoveal relaxing and arcuate temporal retinotomy require complex and unjustified surgical manoeuvres in view of the surgical alternatives with overlapping anatomical and functional results.
难治性全层黄斑裂孔的手术治疗现状
摘要
本综述旨在总结玻璃体切除术和内界膜剥离术在处理难治性全层黄斑裂孔(FTMH)中的手术技巧, 分析并比较术后解剖和功能的不同, 以评估其疗效。本文根据已有的手术技术进行分组。以难治性FTMH的闭合率和最佳矫正视力(BCVA)的提高为2个分析指标。本综述共纳入36篇文献。手术技术分为10个亚组: 自体血小板浓缩(APC)、晶状体囊膜瓣移植(LCFT)、自体游离ILM瓣移植(游离ILM瓣)、ILM扩大剥离、黄斑裂孔水分离(MHH)、自体视网膜移植(ARG)、硅油(SO)、人羊膜(hAM)移植、中心凹周围区松解视网膜切开术、弧形颞侧视网膜切开术。各亚组间难治性FTMH闭合率相似, 未出现明显的异质性(p < 0.176)。最佳矫正视力的获益与手术技术有显著的相关性(p < 0.0001), 各亚组间也存在明显的异质性(p < 0.0001)。各种手术技术根据BCVA的获益定义为三个亚组: 高BCVA获益(hAM)、中等BCVA获益(APC、ARG、LCFT、MHH、SO)和低BCVA获益(游离ILM皮瓣、ILM扩大剥离、弧形颞侧视网膜切开术)。就视力恢复而言, 治疗难治性FTMH最有效的技术是hAM。与游离ILM皮瓣相比, LCF和APC可获得更佳的功能性恢复。针对各种手术方案具有重叠交叉的解剖和功能结果, MHH、ARG、中心凹周围区松解和弧形颞侧视网膜切开术需要复杂和未得到验证的手术操作。
Similar content being viewed by others
Introduction
Pars plana vitrectomy (PPV), epiretinal membrane (ERM) peeling and gas tamponade were proposed by Kelly and Wendel [1] for surgical repair of primary full thickness macular hole resulting in a 58% closure rate (FTMH) [1]. Improving vitreoretinal surgical techniques, understanding pathological mechanisms of FTMH better and introducing intraoperative adjuvant agents allowed surgeons to obtain better results, exceeding 90% of FTMH closure rate [2,3,4,5,6,7]. However, the greatest advancement in FTMH surgical treatment was obtained with the introduction of internal limiting membrane (ILM) peeling, with a primary FTMH closure rate ranging from 84 to 94% [8,9,10,11,12,13,14]. Currently, PPV with ILM peeling is the gold standard treatment for FTMH. Despite the macular hole closure rate being very high, a refractory FTMH may occur.
Definition of refractory full thickness macular hole (FTMH)
Refractory FTMH is a generic definition that includes both a “reopened FTMH”, an FTMH occurred after surgically induced closure, and “unclosed or persistent FTMH”, an FTMH that did not close at the end of surgery. Although some authors described a higher closure rate in reopened FTMH compared to unclosed FTMH, there is no evidence of different morphological appearance between them [15]. Few detailed studies about the morphology of refractory FTMH have been published. Some authors tried to classify primary FTMH closure patterns, leaving more doubts than certainties about the interpretations of the tomographic patterns reported in their studies [16, 17]. Imai et al. [16] defined three patterns of FTMH closure: “U type” with “normal foveal contour”, “V type” with “steep foveal contour” and “W type” with “foveal defect of neurosensory retina”. Kang et al. [17] defined two patterns of FTMH closure: “type 1” with “no interruption in the continuity of foveal tissue above the retinal pigment epithelial layer” and “type 2” with “an interruption in the continuity of foveal tissue” and retinal pigment epithelium (RPE) “denuded”, similar to “W type” described by Imai et al. Although “W type” and “type 2” are defined as FTMH closure patterns and many authors considered them as an anatomical success with less or no functional improvement, they are only partially repaired FTMH with bared RPE. In support of this, Hillenkamp et al. [18] defined two morphological patterns of refractory FTMH: a “type without cuff” that “appears flat and punched out without a distinct retinal cuff”, generally considered a flat FTMH, equivalent to type W and type 2 previously described, and a “type with cuff” “characterised by an elevated retinal cuff overlapping the hole” (Fig. 1).
Tomographic foveal patterns after surgically induced closure of full thickness macular hole (FTMH). a Restoration of foveal contour (dashed line) with integrity of outer retinal layers (ORL) (white arrows) equivalent to Imai’s “type U” and Kang’s “type 1”. b Thinned foveal floor with irregular foveal contour (dashed line) and interruption of ORL (white arrows), equivalent to Imai’s “type V” and Kang’s “type 1”. Patterns of full thickness macular hole (FTMH) refractory to pars plana vitrectomy and internal limiting membrane (ILM) peeling. c Refractory FTMH with elevated edges (dashed line) and bared retinal pigment epithelium (RPE) (white arrow), equivalent to Hillenkamp’s “type with cuff”. d Refractory FTMH with flat edges (dashed line) and bared RPE (white arrow), equivalent to Imai’s “type W”, Kang’s “type 2” and Hillenkamp’s “type without a cuff”. Tomographic images from the database of the department of Ophthalmology of University of Padova, Italy.
Incidence of refractory full thickness macular hole (FTMH)
D’Souza et al. [19] reported an incidence of refractory FTMH of 11.2% in 491 patients. Subsequently, in 2013, Jackson et al. [20] estimated a rate of 4.2% of refractory FTMH in 1078 eyes after PPV combined, in most cases, with ILM peeling (94.1%) and gas tamponade (93.5%). Surgical failure of primary FTMH may be the result of factors inherent to the clinical characteristics of FTMH or to the poor intraoperative and postoperative management. Ethnicity, FTMH size, FTMH duration, association with myopia, uveitis and trauma are all recognised clinical factors for surgical failure; factors depending on intra and postoperative management are: partial removal of epiretinal tractions, inadequate ILM peeling, insufficient gas tamponade and poor compliance of patient in keeping prone position [19, 21,22,23,24,25,26,27,28,29,30,31,32,33,34].
Surgical techniques for treating refractory full thickness macular hole (FTMH)
A FTMH refractory to PPV and ILM peeling is a challenge for surgeons and the several proposed surgical techniques are expression of the ongoing search for the best treatment. An enlargement of ILM peeling demonstrated that ILM has to be removed up to the vascular arcades [19, 35, 36]. Light silicon oil (SO) [37,38,39], heavy SO [40,41,42,43], blood derivatives, as whole blood (WB) or autologous platelet concentrate (APC), have been widely used, alone or combined with other procedures [15, 18, 44,45,46,47,48]. Recently, some authors proposed to place an autologous tissue graft into or over FTMH: as autologous free ILM flap transplantation (free ILM flap) [49,50,51,52,53,54,55,56,57,58,59,60,61], lens capsular flap (LCF) harvested from the anterior or posterior capsule [62, 63], autologous retinal graft (ARG) [64,65,66], human amniotic membrane (hAM) [67]. The rationale of using one of these tissue grafts was based on the hypothesis of their potential effect of inducing cell proliferation, of a potential role as a scaffold for the subsequent regeneration of the retinal layers (ILM, LCF and hAM) or even, concerning ARG, of its potential functional activation by the contact with RPE or with the edges of FTMH. From the originally proposed surgical techniques, different surgical variants have been implemented by the use of adjuvant agents for facilitating the positioning of the tissue graft and for reducing the risk of postoperative graft dislodgement [34,35,36,37,38,39,40,41,42,43,44,45]. Surgical techniques that are completely different from the previous cited as perifoveal relaxing retinotomy [68], arcuate temporal retinotomy [69] and macular hole hydrodissection (MHH) [70,71,72,73,74,75,76] are worth a stand-alone status. These techniques are based on the rationale of making the retina more elastic for inducing closure of FTMH.
Aim of study
This review aims to collect the various proposed surgical techniques for treating FTMH refractory to PPV and ILM peeling and to analyse and compare anatomical and functional outcomes in order to evaluate their efficacy.
Material and methods
The strategy of the study was based on the guidelines of preferred reporting items for systematic reviews and meta-analysis [77]. PubMed (the National Library of Medicine PubMed interface, www.pubmed.gov), Google Scholar, Web of Science, Scopus were the research engines for electronically searching and retrieving literature. In view of that institutional review board approval was not required.
Search methods
In the first research phase keywords “refractory full thickness macular hole” and “refractory macular hole” were used. In the advanced search, articles containing keywords similar to refractory, like “reopened”, “unclosed”, “failed repair”, combined to “full thickness macular hole” and “macular hole” were added. The known surgical techniques and those discovered during the current research (“autologous free internal limiting membrane flap transplantation”, “autologous retinal transplantation” or “neurosensory retinal graft”, “anterior or posterior lens capsular flap”, “autologous platelet concentrate”, “autologous serum”, “whole blood”, “enlargement of internal limiting membrane peeling”, “silicon oil” or “light silicon oil” or “heavy silicon oil” or “Densiron” tamponade, radial and peripheral retinotomy) associated with refractory (or similar keywords) “full thickness macular hole” or “macular hole” were collected.
Articles selection
The titles and the abstracts containing the keywords previously cited were reviewed. Articles published in mother language rather than English were excluded. Articles were collected until 28 February 2020.
Inclusion and exclusion criteria
Articles presenting clinical cases of at least two patients, retrospective or prospective, of refractory FTMH, after PPV with ILM peeling, having undergone further surgical attempts were reviewed. Articles where it was not clear if ERM or ILM were peeled during the first surgery for treating primary FTMH were excluded. A minimum of 3 months of follow-up was required to be included. Exclusion criteria were: single case reports, follow-up inferior to 3 months, indication for the first surgery different from FTMH, studies including patients affected by refractory FTMH associated with retinal detachment and early outpatient fluid-gas exchange for failed FTMH surgery.
Data collection and categorisation of studies
All the reports collected applying all keyword combinations in the electronic searching tool were examined by two reviewers (LT, IG). If insufficient information was obtained by the title or the abstract, the full text was examined in order to evaluate whether the inclusion criteria were met. In doubt cases, a discussion between the two reviewers and a third reviewer (RF) was required to solve the uncertainty. The following data were collected: author’s names, journal, publication’s year, number of eyes, gender (male/female), age (years), lens status (pseudophakic or phakic), preoperative maximum diameter of refractory FTMH (FTMH size, microns), preoperative best-corrected visual acuity (BCVA) converted to logarithm of minimum angle of resolution (logMAR), surgical technique, interval from the previous primary FTMH treatment to refractory FTMH treatment (surgical interval, months), tamponade agent used, rate of refractory FTMH closure (%), morphology of FTMH closure according to Imai et al. [16] and Kang et al. [17] criteria, postoperative BCVA (logMAR), BCVA gain (postoperative BCVA–preoperative BCVA), complications, follow-up (months). The articles were divided into subgroups according to the surgical technique used for treating refractory FTMH (surgical technique subgroups). For the articles reporting a series of patients in which one or more of them presented characteristics not meeting inclusion criteria of the current study, if available a selection of the only eligible patients, from the table of published data in the analysed article, was made and summary statistics were calculated. About the complications, only the failure of refractory FTMH surgery indirectly reported as closure rate (%) was analysed. The other complications collected were closely related to each surgical technique to be used for comparison among surgical technique subgroups.
Statistical analysis
The articles were grouped according to the surgical techniques used for treating refractory FTMH. Refractory FTMH closure rate and BCVA gain were the two parameters analysed among all articles and compared among the surgical technique subgroups. Summary statistics included means, standard deviation (SD) and 95% confidence interval (CI95%). Weighted value of means and standard errors (SE) for refractory FTMH closure rate and BCVA gain measures was calculated using both fixed- and random-effect models. Publication bias was evaluated through funnel plot symmetry and heterogeneity tests (Q index, I2 index). Possible factors (moderator variables) affecting visual outcomes using meta-regression analysis were investigated. A weighted linear regression model between BCVA gain and continuous quantitative variables was estimated and random-effects ANOVA models were applied. Post hoc multiple comparisons followed significant results of random-effects ANOVA analysis to investigate differences in BCVA gain among surgical techniques. No correction of p value was made because of the explorative aim of this analysis. p value was considered significant when <0.05. All the analyses were performed by SAS® 9.4 statistical software (SAS Institute, Cary, NC, USA). Forest plots and funnel plots were drawn by means of MedCalc® software (https://www.medcalc.org/index.php).
Results
The PubMed search returned a total of 412 articles after all keywords search combinations were applied. The flow chart, represented in Fig. 2, depicts the study selection process for the systematic review. Thirty-six articles fulfilled the eligibility criteria. Ten subgroups of surgical techniques for treating refractory FTMH were defined: APC subgroup (4 articles); subgroup of LCF transplantation (LCFT subgroup) (2 articles); free ILM flap subgroup (13 articles); enlargement of ILM peeling subgroup (3 articles); MHH subgroup (4 articles); ARG subgroup (2 articles); SO subgroup (5 articles); hAM subgroup (1 article); perifoveal relaxing retinotomy subgroup (1 article); arcuate temporal retinotomy subgroup (1 article). Supplementary information: Tables 1 and 2 report the demographic, preoperative and postoperative parameters of all 36 analysed articles divided in surgical technique subgroups.
Full thickness macular hole (FTMH) closure rate
Data from all the 36 included articles were used for analysing refractory FTMH closure rate. The meta-analyses revealed that, for the cumulative 404 operated eyes, refractory FTMH closure rate was 82.7% (334 eyes). When refractory FTMH closure rate was weighted on SE of each article, a similar closure rate of 82.3% (CI95% range from 78.3 to 85.7) for fixed effects and 82.7% (CI95% range from 78.5 to 86.6) for random effects was found. All articles included in the analyses fall inside the CI95%, a low grade and not significant heterogeneity among articles emerged (Q index = 42.6; p = 0.176; I2 index = 17.86% with CI95% ranged from 0 to 45.9). Forest and Funnel plots for closure rate analyses are presented in Figs. 3 and 4.
Best-corrected visual acuity (BCVA)
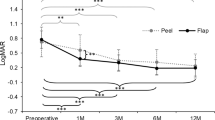
Thirty-two of 36 articles concurred for BCVA gain analysis, 4 articles were excluded (authors referred with ID numbers 19, 25, 35 did not report BCVA measurements at initial and final stages or quantitative BCVA change after surgery expressed with logMAR or Snellen scale; no SD measures were available from authors identified with ID number 20). Considering the non-weighted summary statistics from each study, mean preoperative BCVA was 1.18 ± 0.26 logMAR that improved to 0.74 ± 0.28 logMAR with a mean BCVA gain of 0.44 ± 0.21 logMAR. When BCVA gain was weighted on SE of each article, a mean BCVA gain of 0.428 ± 0.012 logMAR (CI95% range from 0.405 to 0.451; ANOVA test: p < 0.001) for fixed effects and 0.424 ± 0.036 logMAR (CI95% range from 0.354 to 0.494; ANOVA test: p < 0.001) for random effects was found. A statistically significant high heterogeneity among articles emerged (Q index = 196.03; p < 0.0001; I2 index = 84.19% with CI95% ranged from 0 to 45.9). Many articles included in the analyses fell outside the CI95% due to a high heterogeneity: three articles from APC subgroup (ID numbers 1, 2, 3); three articles from free ILM flap subgroup (ID numbers 11, 16); one article from enlargement of peeling subgroup (ID number 21); two articles from MHH subgroup (ID numbers 24, 26), one article from ARG subgroup (ID number 28), two articles from SO subgroup (ID numbers 30, 31), one article from hAM subgroup 1 (ID number 34). Forest and Funnel plots for BCVA analyses are presented in Figs. 5 and 6. Meta-regression analysis revealed a non-statistically significant correlation between BCVA gain and following parameters: age (p = 0.9233), gender (p = 0.7078), preoperative FTMH maximum size (p = 0.2225), lens status (p = 0.5224), surgical interval (p = 0.8383), follow-up (p = 0.9403) and tamponade (p = 0.9778). Although preoperative BCVA resulted in being related to BCVA gain (p = 0.0024), BCVA gain showed a significant dependence on surgical technique (p < 0.0001) demonstrating that the correlation between preoperative BCVA and BCVA gain was due to a confounding effect of the surgical technique. Three sets of surgical technique subgroups with a homogeneous BCVA gain were defined: high, intermediate and low BCVA gain set. The first set is represented only by hAM and it is associated with the highest BCVA gain equal to 0.99 logMAR. The second set is composed of ARG, MHH, SO, LCFT and APC/PRGF, with a range between 0.43 and 0.56 logMAR of BCVA gain. The last set includes free ILM flap, enlargement of peeling and arcuate temporal retinotomy, with the smallest BCVA gain (range, 0.12–0.27 logMAR).
Discussion
Idiopathic FTMH has a prevalence of less than 1% [78,79,80]. FTMH closure rate after standard surgical treatment, PPV and ERM-ILM peeling, is now well over 90% of cases. However, the closure rate decreases for FTMH with a size superior to 400 microns [8,9,10,11,12,13,14, 16, 27, 30, 44, 81,82,83,84,85,86,87,88]. Although FTMH has a low incidence and a low failure rate in treatment, the surgical techniques proposed for treating postoperative recurrence are numerous. From the current review, the closure rate of refractory FTMH is high and similar in all analysed surgical techniques, on the contrary functional improvement rate varies. hAM subgroup shows a functional recovery at least double compared to the other surgical technique subgroups, as shown by its widest scattering towards the left side of the funnel plot of BCVA gain (Fig. 6). The first observation concerns the comparison between hAM subgroup and the others using tissue graft: ARG, LCFT and free ILM flap subgroups. The positioning of tissue graft in the FTMH is the most important factor that differentiates hAM technique from the others. In the surgical techniques of LCFT and free ILM flap, it is not always possible to detect whether the tissue graft covers or fills FTMH. In the hAM technique, the tissue is placed in the subretinal space, below the edges of FTMH, in contact with the RPE cells. hAM placed in the subretinal space prevents contact between the vitreous and the RPE, stimulates the proliferation of RPE cells as was demonstrated in vitro by different authors [89, 90] and acts as a scaffold for retinal regeneration [91]. Furthermore, hAM technique has the advantage that does not require additional intraocular surgical procedures of harvesting the tissue flap, as needed by the LCFT, free ILM flap and ARG techniques. The free ILM flap is the technique that gives the poorest visual recovery. The authors of the current paper hypothesise that ILM compared to the other tissues used, LCF and ARG, is thinner and can dislodge more easily or not lie correctly inside the FTMH. Many authors proposed additional agents to help fixing the tissue graft into the MH, as viscoat, perfluorocarbon liquid (PFCL), autologous WB, APC. A small amount of viscoat can be injected into the vitreous chamber on the top of inverted ILM flap. Viscoat has a dual effect, adhesive and ballast to stabilise the flap during the fluid-air exchange. Viscoat can be left in place without causing any toxic effect to the retina [49, 66, 91, 92]. PFCL was very efficient for placing the tissue graft but some authors highlighted the risk of small PFCL bubbles remaining at the end of surgery [64]. Autologous WB and APC were used both for inducing FTMH closure (activating fibro-glial proliferation, migration and contraction of human retinal Müller cells) and as adjuvant to tissue graft techniques for them adhesive support [60, 63, 93]. On the other hand, both WB and APC can have a toxic effect on the photoreceptors due to a migration of blood into the subretinal space or to a release of free radicals and pro-inflammatory substances that affect tissue regeneration [92]. Regarding the ARG technique, interesting functional results were obtained, although less effective than the hAM technique and not much better than less surgically invasive ones (ILM flap and LCFT). In support of this finding, the authors who proposed ARG technique suggest performing it only when ILM flap technique is not possible to perform due to a previous very extensive ILM peeling, or when the LCFT is not possible to perform because the posterior capsule is not available, i.e., in phakic patients without indication of cataract surgery or in pseudophakic patients with an open posterior capsule [62, 66]. The same applies to MHH and arcuate temporal retinotomy techniques that induce iatrogenic retinal damage [76]. SO and enlargement of peeling techniques deserve a separate discussion. The enlargement of peeling is a surgical manoeuvre that should be performed in all cases of refractory FTMH in which the peeling area was not extended to the vascular arcades. The use of permanent tamponade, as SO, is indicated when there is an evidence that the patient has not maintained postoperative face-down position as recommended. In conclusion, this review showed that the proposed surgical techniques for the treatment of refractory FTMH give an overlapping anatomical success. On the other hand, there are significant differences in terms of visual recovery that would lead to suggest using the hAM technique as a first choice. LCFT or APC techniques allow to obtain better functional outcomes than the free ILM flap technique. MHH, ARG, perifoveal relaxing and arcuate temporal retinotomy are techniques that require complex and unjustified surgical manoeuvres in view of surgical alternatives that give overlapping anatomical and functional results. However, it should be pointed out that the results must be interpreted in the context of a review of articles that propose a large number of surgical treatments, some very recent, in development, not yet approved and with a number of extremely heterogeneous treated cases.
Change history
25 February 2022
A Correction to this paper has been published: https://doi.org/10.1038/s41433-021-01460-x
References
Kelly NE, Wendel RT. Vitreous surgery for idiopathic macular holes: results of a pilot study. Arch Ophthalmol. 1991;109:654–9. https://doi.org/10.1001/archopht.1991.01080050068031.
Glaser BM, Michels RG, Kuppermann BD, Sjaarda RN, Pena RA. Transforming growth factor-beta 2 for the treatment of full-thickness macular holes. A prospective randomized study. Ophthalmology. 1992;99:1162–72. https://doi.org/10.1016/s0161-6420(92)31837-8.
Liggett PE, Skolik DS, Horio B, Saito Y, Alfaro V, Mieler W. Human autologous serum for the treatment of full-thickness macular holes. A preliminary study. Ophthalmology. 1995;102:1071–6. https://doi.org/10.1016/S0161-6420(95)30909-8.
Korobelnik JF, Hannouche D, Belayachi N, Branger M, Guez JE, Hoang-Xuan T. Autologous platelet concentrate as an adjunct in macular hole healing: a pilot study. Ophthalmology. 1996;103:590–4. https://doi.org/10.1016/s0161-6420(96)30648-9.
Ezra E, Aylward WG, Gregor ZJ. Membranectomy and autologous serum for the retreatment of full-thickness macular holes. Arch Ophthalmol. 1997;115:1276–80. https://doi.org/10.1001/archopht.1997.01100160446010.
Thompson JT, Smiddy WE, Williams GA, Siaarda RN, Flynn HW, Margherio RR, et al. Comparison of recombinant transforming growth factor-beta-2 and placebo as an adjunctive agent for macular hole surgery. Ophthalmology. 1998;105:700–6. https://doi.org/10.1016/SO161-6420(98)94027-1.
Steel DH, Donachie PHJ, Aylward GW, Laidlaw DA, Williamson TH, Yorston D, et al. Factors affectiing anatomical and visual poutcome after macular hole surgery: findings from a large prospective UK cohort. Eye. 2020. https://doi.org/10.1038/s41433-020-0844-x.
Eckardt C, Eckardt U, Groos S, Luciano L, Reale E. Removal of the internal limiting membrane in macular holes. Clinical and morphological findings. Ophthalmologe. 1997;94:545–51. https://doi.org/10.1007/s003470050156.
Waich’ng S, Patton N, Ahmed M, Ivanova T, Baumann C, Charles S, et al. The Manchester large macular hole study: is it time to reclassify large macular holes? Am J Ophthalmol. 2018;195:36–42. https://doi.org/10.1016/j.ajo.2018.7.027.
Brooks HL Jr. Macular hole surgery with and without internal limiting membrane peeling. Ophthalmology. 2000;107:1939–48. https://doi.org/10.1016/S0161-6420(00)00331-6.
Kumagai K, Furukawa M, Ogino N, Uemura A, Demizu S, Larson E. Vitreous surgery with and without internal limiting membrane peeling for macular hole repair. Retina. 2004;24:721–7. https://doi.org/10.1097/00006982-200410000-00006.
Kwok AK, Lai TY, Wong VW. Idiopathic macular hole surgery in Chinese patients: a randomised study to compare indocyanine green-assisted internal limiting membrane peeling with no internal limiting membrane peeling. Hong Kong Med J. 2005;11:259–66.
Christensen UC, Kroyer K, Sander B, Larsen M, Henning V, Villumsen J, et al. Value of internal limiting membrane peeling in surgery for idiopathic macular hole stage 2 and 3: a randomised clinical trial. Br J Ophthalmol. 2009;93:1005–15. https://doi.org/10.1136/bjo.2008.151266.
Spiteri Cornish K, Lois N, Scott NW, Burr J, Cook J, Boachie C, et al. Vitrectomy with internal limiting membrane peeling versus no peeling for idiopathic full-thickness macular hole. Ophthalmology. 2014;121:649–55. https://doi.org/10.1016/j.ophtha.2013.10.020.
Valldeperas X, Wong D. Is it worth reoperating on macular holes? Ophthalmology. 2008;115:158–63. https://doi.org/10.1016/j.ophtha.2007.01039.
Imai M, Iijima H, Gotoh T, Tsukahara S. Optical coherence tomography of successfully repaired idiopathic macular holes. Am J Ophthalmol. 1999;128:621–7. https://doi.org/10.1016/S0002-9394(99)00200-7.
Kang SW, Ahn K, Ham DI. Types of macular hole closure and their clinical implications. Br J Ophthalmol. 2003;87:1015–9. https://doi.org/10.1136/bjo.87.8.1015.
Hillenkamp J, Kraus J, Framme C, Jackson TL, Roider J, Gabel VP, et al. Retreatment of full-thickness macular hole: predictive value of optical coherence tomography. Br J Ophthalmol. 2007;91:1445–9. https://doi.org/10.1136/bjo.2007115642.
D’Souza MJ, Chaudhary V, Devenyi R, Kertes PJ, Lam WC. Re-operation of idiopathic full-thickness macular holes after initial surgery with internal limiting membrane peel. Br J Ophthalmol. 2011;95:1564–7. https://doi.org/10.1136/bjo.2010-195826.
Jackson TL, Donachie PHJ, Sparrow JM, Johnston RL. United kingdom national ophthalmology database study of vitreoretinal surgery: report 2, macular hole. Ophthalmology. 2013;120:629–34. https://doi.org/10.1016/j.ophtha.2012.09.003.
Wendel RT, Patel AC, Kelly NE, Salzano TC, Wells JW, Novack GD. Vitreous surgery for macular holes. Ophthalmology. 1993;100:1671–6. https://doi.org/10.1016/s0161-6420(93)31419-3.
Fekrat S, Wendel RT, de La Cruz Z, Green WR. Clinicopathologic correlation of an epiretinal membrane associated with a recurrent macular hole. Retina. 1995;15:53–7. https://doi.org/10.1097/00006982-199515010-00010.
Thompson JT, Smiddy WE, Glaser BM, Sjaarda RN, Flynn HW Jr. Intraocular tamponade duration and success of macular hole surgery. Retina. 1996;16:373–82. https://doi.org/10.1097/00006982-199616050-00002.
Ryan EH, Gilbert HD. Results of surgical treatment of recent-onset full-thickness idiopathic macular holes. Arch Ophthalmol. 1994;112:1545–53. https://doi.org/10.1001/archopht.1994.01090240051025.
Kumar V, Banerjee S, Loo AV, Callear AB, Benson MT. Macular hole surgery with silicone oil. Eye. 2002;16:121–5. https://doi.org/10.1038/sj.eye.6700029.
Ip MS, Baker BJ, Duker JS, Reichel E, Baumal CR, Gangnom R, et al. Anatomical outcomes of surgery for idiopathic macular hole as determined by optical coherence tomography. Arch Ophthalmol. 2002;120:29–35. https://doi.org/10.1001/archopht.120.1.29.
Ullrich S, Haritoglou C, Gass C, Schaumberger M, Ulbig MW. Macular hole size as a prognostic factor in macular hole surgery. Br J Ophthalmol. 2002;86:390–3. https://doi.org/10.1136/bjo.86.4.390.
Kobayashi H, Kobayashi K, Okinami S. Macular hole and myopic refraction. Br J Ophthalmol. 2002;86:1269–73. https://doi.org/10.1136/bjo.86.11.1269.
Ikuno Y, Sayanagi K, Soga K, Oshima Y, Ohji M, Tano Y. Foveal anatomical status and surgical results in vitrectomy for myopic foveoschisis. Jpn J Ophthalmol. 2008;52:269–76. https://doi.org/10.1007/s10384-008-0544-8.
Michalewska Z, Michalewski J, Adelman RA, Nawrocki J. Inverted internal limiting membrane flap technique for large macular holes. Ophthalmology. 2010;117:2018–25. https://doi.org/10.1016/j.ophtha.2010.02.011.
Kumar A, Gogia V, Shah VM, Nag TC. Comparative evaluation of anatomical and functional outcomes using brilliant blue G versus triamcinolone assisted ILM peeling in macular hole surgery in Indian population. Graefes Arch Clin Exp Ophthalmol. 2011;249:987–95. https://doi.org/10.1007/s00147-010-1609-1.
Suda K, Hangai M, Yoshimura N. Axial length and outcomes of macular hole surgery assessed by spectral-domain optical coherence tomography. Am J Ophthalmol. 2011;151:118–27. https://doi.org/10.1016/ajo.2010.07.007.
Liu W, Grzybowski A. Current management of traumatic macular holes. J Ophthalmol. 2017:1–8. https://doi.org/10.1155/2017/1781352017.
Chandra A, Lai M, Mitry D. Ethnic variation in primary idiopathic macular hole surgery. 2017;31:708–12. https://doi.org/10.1038/eye.2016.296.
Che X, He F, Lu L, Zhu D, Xu X, Song X, et al. Evaluation of secondary surgery to enlarge the peeling of the internal limiting membrane following the failed surgery of idiopathic macular holes. Exp Ther Med. 2014;7:742–6. https://doi.org/10.3892/etm.2014.1477.
Hagiwara A, Baba T, Tatsumi T, Sato E, Oshitari T, Yamamoto S. Functional and morphologic outcomes after reoperation for persistent idiopathic macular hole. Eur J Ophthalmol. 2017;27:231–4. https://doi.org/10.5301/ejo.5000857.
Lai JC, Stinnett SS, McCuen BW. Comparison of silicone oil versus gas tamponade in the treatment of idiopathic full-thickness macular hole. Ophthalmology. 2003;110:1170–4. https://doi.org/10.1016/S0161-6420(03)00264-1.
Satchi K, Patel CK. Posterior chamber compartments demonstrated by optical coherence tomography, in silicone-filled eyes, following macular hole surgery. Clin Exp Ophthalmol. 2005;33:619–22. https://doi.org/10.1111/j.1442-9071.2005.01106.x.
Nowroozzadeh MH, Ashraf H, Zadmehr M, Farvardin M. Outcomes of light silicone oil tamponade for failed idiopathic macular hole surgery. J Ophthalmic Vis Res. 2018;13:130–7. https://doi.org/10.4103/jovr.jovr_22_17.
Saeed MU, Heimann H, Wong D, Gibran SK. Heavy silicone oil tamponade after failed macular hole surgery with perfluoropropane (C3F8): a report of five cases. Graefes Arch Clin Exp Ophthalmol. 2009;247:707–9. https://doi.org/10.1007/s00417-008-0965-6.
Rizzo S, Genovesi-Ebert F, Vento A, Cresti F, Miniaci S, Romanognoli MC. Heavy silicone oil (Densiron-68) for the treatment of persistent macular holes: Densiron-68 endotamponade for persistent macular holes. Greafes Arch Clin Exp Ophthalmol. 2009;247:1471–6. https://doi.org/10.1007/s00417-009-1131-5.
Lappas A, Heinrich Foerster AM, Kirchhof B. Use of heavy silicone oil (Densiron-68®) in the treatment of persistent macular holes. Acta Ophthalmol. 2009;87:866–70. https://doi.org/10.1111/j.1755-3768.2008.01371.x.
Cillino S, Cillino G, Ferraro LL, Casuccio A. Treatment of persistently open macular holes with heavy silicone oil (densiron 68) versus C2F6. A prospective randomized study. Retina. 2016;36:688–94. https://doi.org/10.1097/IAE.0000000000000781.
Paques M, Chastang C, Mathis A, Sahel J, Massin P, Dosquet C, et al. Effect of autologous platelet concentrate in surgery for idiopathic macular hole: results of a multicenter, double-masked, randomized trial. Platelets in macular hole surgery group. Ophthalmology. 1999;106:932–8. https://doi.org/10.1016/s0161-6420(99)00512-6.
Hoerauf H, Kluter H, Joachimmeyer E, Roider J, Framme C, Schlenke P, et al. Results of vitrectomy and the no-touch-technique using autologous adjuvants in macular hole treatment. Int Ophthalmol. 2001;24:151–9. https://doi.org/10.1023/a:102156680836.
Dimopoulos S, William A, Voykov B, Ziemssen F, Bartz-Schmidt KU, Spitzer MS. Anatomical and visual outcomes of autologous thrombocyte serum concentrate in the treatment of persistent full-thickness idiopathic macular hole after ILM peeling with brilliant blue G and membrane blue dual. Acta Ophthalmol. 2017;95:429–30. https://doi.org/10.1111/aos.12971.
Purtskhvanidze K, Frühsorger B, Bartsch S, Hedderich J, Roider J, Treumer F. Persistent full-thickness idiopathic macular hole: anatomical and functional outcome of revitrectomy with autologous platelet concentrate or autologous whole blood. Ophthalmologica. 2017;239:19–26. https://doi.org/10.1159/000481268.
Arias JD, Hoyos AT, Alcántara B, Sanchez-Avila RM, Arango FJ, Galvis V. Plasma rich in growth factors for persistent macular hole. Retin Cases Brief Rep. 2019. https://doi.org/10.1097/icb.0000000000000957.
Morizane Y, Shiraga F, Kimura S, Hosokawa M, Shiode Y, Kawata T. Autologous transplantation of the internal limiting membrane for refractory macular holes. Am J Ophthalmol. 2014;157:861–9. https://doi.org/10.1016/j.ajo.2013.12.028.
De Novelli FJ, Preti RC, Ribeiro Monteiro ML, Pelayes DE, Junqueira Nóbrega M, Takahashi WY. Autologous internal limiting membrane fragment transplantation for large, chronic, and refractory macular holes. Ophthalmic Res. 2015;55:45–52. https://doi.org/10.1159/000440767.
Gekka T, Watanabe A, Ohkuma Y, Arai K, Watanabe T, Tsuzuki A, et al. Pedicle internal limiting membrane transposition flap technique for refractory macular hole. Ophthalmic Surg Lasers Imaging Retin. 2015;46:1045–6. https://doi.org/10.3928/23258160-20151027-10.
Park SW, Pak KY, Pak KH, Byon IS, Lee JE. Perfluoro-n-octane assisted free internal limiting membrane flap technique for recurrent macular hole. Retina. 2015;35:2652–6. https://doi.org/10.1097/IAE.0000000000000754.
Dai Y, Dong F, Zhang X, Yang Z. Internal limiting membrane transplantation for unclosed and large macular holes. Graefes Arch Clin Exp Ophthalmol. 2016;254:2095–9. https://doi.org/10.1007/s00417-016-3461-4.
Pires J, Nadal J, Gomes NL. Internal limiting membrane translocation for refractory macular holes. Br J Ophthalmol.2016;101:377–82. https://doi.org/10.1136/bjophthalmol-2015-308299.
Guber J, Lang C, Valmaggia C. Internal limiting membrane flap techniques for the repair of large macular holes: a short-term follow-up of anatomical and functional outcomes. Klin Monbl Augenheilkd. 2017;234:493–6. https://doi.org/10.1055/s-0042-119694.
Ozdek S, Baskaran P, Karabas L, Neves PP. A modified perfluoro-n-octane-assisted autologous internal limiting membrane transplant for failed macular hole reintervention: a case series. Ophthalmic Surg Lasers Imaging Retin. 2017;48:416–20. https://doi.org/10.3928/23258160-20170428-08.
Primavera V, Centoducati T, Agea L, Zucchiatti I, Querques L, Querques G. Pilot evaluation of a new surgical technique for persistent or recurrent large macular holes. Ophthalmic Surg Lasers Imaging Retin. 2018;49:266–8. https://doi.org/10.3928/23258160-20180329-09.
Giansanti F, Tartaro R, Caporossi T, Bacherini D, Savastano A, Barca F, et al. An internal limiting membrane plug and gas endotamponade for recurrent or persistent macular hole. J Ophthalmo. 2019:1–6. https://doi.org/10.1155/2019/6051724.
Vieregge M, Valmaggia C, Scholl HPN, Guber J. Microstructural retinal regeneration after internal limiting membrane flap surgery for repair of large macular holes: a 1-year follow-up study. Int Ophthalmol. 2019;39:1277–82. https://doi.org/10.1007/s10792-018-0941-z.
Wu AL, Chuang LH, Chen KJ, Yeung L, Wang NK, Liu L, et al. Perfluoro-n-octane-assisted autologous internal limiting membrane plug for refractory macular hole surgery. Int Ophthalmol. 2019;39:2767–73. https://doi.org/10.1007/s10792-019-01123-7.
Soliman MK, Lingley AJ, Tuli R. Internal limiting membrane transposition for persistent macular holes using double layers of viscoelastic. Ophthalmic Surg Lasers Imaging Retin. 2019;50:401–3. https://doi.org/10.3928/23258160-20190605-11.
Chen SN, Yang CM. Lens capsular flap transplantation in the management of refractory macular hole from multiple etiologies. Retina. 2016;36:163–70. https://doi.org/10.1097/IAE.0000000000000674.
Peng J, Chen C, Jin H, Zhang H, Zhao P. Autologous lens capsular flap transplantation combined with autologous blood application in the management of refractory macular hole. Retina. 2018;38:2177–83. https://doi.org/10.1097/IAE.0000000000001830.
Grewal DS, Mahmoud TH. Autologous neurosensory retinal free flap for closure of refractory myopic macular holes. JAMA Ophthalmol. 2016;134:229–30. https://doi.org/10.1001/jamaophthalmol.2015.5237.
Wu AL, Chuang LH, Wang NK, Chen KJ, Liu L, Yeung L. Refractory macular hole repaired by autologous retinal graft and blood clot. BMC Ophthalmol. 2018;18:213. https://doi.org/10.1186/s12886-018-0898-8.
Chang YC, Liu PK, Kao TE, Chen KJ, Chen YH, Chiu WJ, et al. Management of refractory large macular hole with autologous neurosensory retinal free flap transplantation. Retina. 2019:1–6. https://doi.org/10.1097/IAE.0000000000002734.
Rizzo S, Caporossi T, Tartaro R, Finocchio L, Franco F, Barca F, et al. A human amniotic membrane plug to promote retinal breaks repair and recurrent macular hole closure. Retina. 2018. https://doi.org/10.1097/IAE.0000000000002320.
Reis R, Ferreira N, Meireles A. Management of stage IV macular holes: when standard surgery fails. Case Rep Ophthalmol. 2012;3:240–50. https://doi.org/10.1159/000342007.
Charles S, Randolph JC, Neekhra A, Salisbury CD, Littlejohn N, Calzada JI. Arcuate retinotomy for the repair of large macular holes. Ophthalmic Surg Lasers Imaging Retina. 2013;44:69–72. https://doi.org/10.3928/23258160-20121221-15.
Oliver A, Wojcik EJ. Macular detachment for treatment of persistent macular hole. Ophthalmic Surg Lasers Imaging. 2011;42:516–8.
Szigiato AA, Gilani F, Walsh MK, Mandelcorn ED, Muni RH. Induction of macular detachment for the treatment of persistent or recurrent idiopathic macular holes. Retina. 2016;36:1694–8. https://doi.org/10.1097/IAE.0000000000000977.
Wong R, Howard C, Orobona GD. Retina expansion technique for macular hole apposition report 2: efficacy, closure rate, and risks of a macular detachment technique to close large full- thickness macular holes. Retina. 2017;38:660–3.
Mohammed OA, Pai A. New surgical technique for management of recurrent macular hole. Middle East Afr J Ophthalmol. 2017;24:61–3. https://doi.org/10.4103/meajo.MEAJO_211_15.
Fotis K, Alexander P, Sax J, Reddie I, Kang CY, Chandra A. Macular detachment for the treatment of persistent full-thickness macular holes. Retina. 2019;39:104–7. https://doi.org/10.1097/IAE.0000000000002370.
Felfeli T, Mandelcorn ED. Macular hole hydrodissection: surgical technique for the treatment of persistent, chronic, and large macular holes. Retina. 2019;39:743–52. https://doi.org/10.1097/IAE.0000000000002013.
Frisina R, Tozzi L, Sabella P, Cacciatori M, Midena E. Surgically induced macular detachment for treatment of refractory full-thickness macular hole: anatomical and functional results. Ophthalmologica. 2019;242:98–105. https://doi.org/10.1159/000500573.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339. https://doi.org/10.1136/bmj.b2700.
Meuer SM, Myers CE, Klein BE, Swift MK, Huang Y, Gangaputra S, et al. The epidemiology of vitreoretinal interface abnormalities as detected by spectral-domain optical coherence tomography: the beaver dam eye study. Ophthalmology. 2015;122:787–95. https://doi.org/10.1016/j.ophtha.2014.10.014.
McCannel CA, Ensminger JL, Diehl NN, Hodge DN. Population-based incidence of macular holes. Ophthalmology. 2009;116:1366–9. https://doi.org/10.1016/j.ophtha.2009.01.052.
Sen P, Bhargava A, Vijaya L, George R. Prevalence of idiopathic macular hole in adult rural and urban south Indian population. Clin Exp Ophthalmol. 2008;36:257–60. https://doi.org/10.1111/j.1442-9071.2008.01715.x.
Tadayoni R, Gaudric A, Haouchine B, Massin P. Relationship between macular hole size and potential benefit of internal limiting membrane peeling. Br J Ophthalmol. 2006;90:1239–41. https://doi.org/10.1136/bjo.2006.091777.
Michalewska Z, Michalewski J, Nawrocki J. Diagnosis and evaluation of macular hole with the HRT 2 retina module [in German]. Ophthalmologe. 2007;104:881–8. https://doi.org/10.1007/s00347-007-1558-1.
Michalewska Z, Michalewski J, Cisiecki S, Adelman R, Nawrocki J. Correlation between foveal structure and visual outcome following macular hole surgery: a spectral optical coherence tomography study. Graefes Arch Clin Exp Ophthalmol. 2008;246:823–30. https://doi.org/10.1007/s00417-007-0764-5.
Christmas NJ, Smiddy WE, Flynn HW. Reopening of macular holes after initially successful repair. Ophthalmology. 1998;105:1835–8. https://doi.org/10.1016/S0161-6420(98)91025-9.
Gross JG. Late reopening and spontaneous closure of previously repaired macular holes. Am J Ophthalmol. 2005;140:556–8. https://doi.org/10.1016/j.ajo.2005.03.044.
Kusaka S, Sakagami K, Kutsuna M, Ohashi Y. Treatment of full-thickness macular holes with autologous serum. Jpn J Ophthalmol.1997;41:332–8. https://doi.org/10.1016/s0021-5155(97)00055-5.
Sheidow TG, Blinder KJ, Holekamp N, Joseph D, Shah G, Grand MG, et al. Outcome results in macular hole surgery: an evaluation of internal limiting membrane peeling with and without indocyanine green. Ophthalmology. 2003;110:1697–701. https://doi.org/10.1016/S0161-6420(03)00562-1.
Vine AK, Johnson MW. Thrombin in the management of full thickness macular holes. Retina. 1996;16:474–8. https://doi.org/10.1097/00006982-199616060-00002.
Liu Y, Silverman MS, Berger AS, Kaplan HJ. Transplantation of confluent sheets of adult human RPE. Invest Ophthalmol Vis Sci. 1992;33:2180.
Capeéans C, Piñeiro Ces A, Pardo M, Sueiro-López C, Blanco MJ, Domínguez F, et al. Amniotic membrane as support for human retinal pigment epithelium (RPE) cell growth. Acta Ophthalmol Scand. 2003;81:271–7. https://doi.org/10.1034/j.1600-0420.2003.00076.x.
Kiilgaard JF, Scherfig E, Prause JU, la Cour M. Transplantation of amniotic membrane to the subretinal space in pigs. Stem Cells Int. 2012;716968. https://doi.org/10.1155/2012/716968.
Glatt H, Machemer R. Experimental subretinal hemorrhage in rabbits. Am J Ophthalmol. 1982;94:762–73. https://doi.org/10.1016/0002-9394(82)90301-4.
Lai CC, Chen YP, Wang NK, Chuang LH, Liu L, Chen KJ, et al. Vitrectomy with internal limiting membrane repositioning and autologous blood for macular hole retinal detachment in highly myopic eyes. Ophthalmology. 2015;122:1889–98. https://doi.org/10.1016/j.ophtha.2015.05.040.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: Figures 3 and 5 were incomplete.
Rights and permissions
About this article
Cite this article
Frisina, R., Gius, I., Tozzi, L. et al. Refractory full thickness macular hole: current surgical management. Eye 36, 1344–1354 (2022). https://doi.org/10.1038/s41433-020-01330-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01330-y
This article is cited by
-
Autologous internal limiting membrane transplantation achieves anatomic closure and functional improvement in the treatment of large, persistent macular holes
International Journal of Retina and Vitreous (2024)
-
Platelet concentrates in macular hole surgery. A journey through the labyrinth of terminology, preparation, and application: a comprehensive review
Graefe's Archive for Clinical and Experimental Ophthalmology (2024)
-
Surgical classification for large macular hole: based on different surgical techniques results: the CLOSE study group
International Journal of Retina and Vitreous (2023)
-
Femtosecond laser-cut autologous anterior lens capsule transplantation to treat refractory macular holes
Eye (2023)
-
Comment on: Refractory full thickness macular hole: current surgical management
Eye (2023)