Abstract
Background
Following removal of the eye, soft tissue changes of the eyelids and orbit may develop into an anophthalmic socket (AS) syndrome, which is often attributed to orbital volume deficiency. While adequate primary orbital volume replacement is nowadays standard of care, patients may still present with facial asymmetry. The aim of this study is to provide insights into these changes and their impact on patient quality of life (QoL).
Methods
Cross-sectional study of 59 patients with longstanding ocular prosthetic wear after enucleation or evisceration surgery. The alignment, function, and laxity of the eyelids of the anophthalmic side were compared to those of the fellow side. The QoL was assessed with a 4-item questionnaire specific for the prosthetic condition. The different aspects of AS syndrome were analysed in relation to disease-specific and prosthetic data and to the patient QoL scores.
Results
Clinical AS syndrome was prevalent in 53% of patients with acquired anophthalmia. The anophthalmic side was statistically significantly different from the fellow side for the known AS syndrome features such as superior sulcus depression, margin reflex distance 1, and enophthalmia, but also for new features such as levator muscle function and lagophthalmia (P < 0.05). The difference was correlated with duration of prosthetic wear, prior orbital radiotherapy, and size of the prosthesis (P < 0.05). QoL scores were not correlated to the separate features of AS syndrome, except for a positive correlation between wearing comfort of the prosthesis and upper eyelid ptosis (P < 0.05).
Conclusion
Patients with an ocular prosthesis show a relatively high prevalence of one or more distinct clinical features of AS syndrome, which do not negatively affect patient QoL. These findings underscore the importance to tailor prosthetic and surgical treatment to the patient’s perceived QoL rather than to the objective clinical findings.
Similar content being viewed by others
Introduction
Anophthalmic socket (AS) syndrome, also called post-enucleation socket syndrome, may develop following the removal of the eye and is characterized by the hallmark feature of superior sulcus depression, along with posterior displacement of the prosthesis, upper eyelid ptosis or retraction, and lower eyelid laxity [1]. In addition to the traumatic event of the loss and removal of the eye and despite of an optimally fitted ocular prosthesis, the development of AS syndrome causes new complications, all of which may adversely affect the quality of life (QoL) of the patient [2,3,4,5,6].
Orbital implants are used to correct orbital volume deficiency which is considered the leading cause of AS syndrome [7]. Research has focused on the optimal shape, size and material of the implant, surgical technique, and wrapping material to achieve adequate volume replacement with sufficient prosthesis motility and low implant extrusion rate [8, 9]. However, there is no consensus on the surgical management, and progression to AS syndrome is still frequently encountered. Moreover, the pathophysiology of AS syndrome remains elusive. In addition to inadequate volume replacement, orbital fat atrophy, changes in the superior rectus/levator muscle complex, gravitational burden of the orbital implant and prosthesis and implant migration have been postulated as underlying mechanisms of AS syndrome [10, 11].
The aim of this study is to gain insight in the clinical spectrum of AS syndrome in patients with primary orbital implants and to measure the impact on patient QoL.
Materials and methods
All patients who visited the Orbital and Ocular Prosthetic Unit at the University Hospitals Leuven between October 2018 and November 2019 were invited to participate in the study. The inclusion criteria were: older than 18 years of age, history of unilateral evisceration or enucleation with primary orbital implant, customized optimally fitted and properly maintained (i.e., polishing each 18 months) ocular prosthesis since 2 years or longer, and the ability to read and understand a questionnaire in Dutch. The exclusion criteria were: eye removal at early age (i.e., before 18 years of age), prior eyelid surgery, secondary orbital implant surgery, and severe orbital volume deficiency evidenced by a small orbital implant (i.e., spherical orbital implant diameter of 16 mm or less) and a large prosthesis (i.e., prosthetic volume of 3 mL or more) [8]. The study protocol adhered to the tenets of the declaration of Helsinki and was approved by the Ethical Committee and Institutional Review Board (B322201836522).
The following data were collected for each patient: eye history, surgical procedure, clinical features, duration of prosthetic wear, prosthetic features, and the scores of the QoL questionnaire (Table 1). One observer (SR) clinically examined the patients. Based on the presence of sunken upper eyelid with invaginated skin between the lower eyebrow and upper border of the prosthesis/globe, superior sulcus depression was graded as “none” when no visible invagination; “mild” in the case of an invaginated area of 1–2 mm vertically at the nasal aspect, “moderate” for an invaginated area of 3 mm vertically at the nasal aspect, and “severe” for an area of >3 mm vertically of invaginated skin involving the entire superior sulcus [12]. Palpebral fissure height was measured with a ruler as the distance between the upper and lower eyelid margin. The margin reflex distance (MRD) comprised the distance from the pupillary light reflex on the prosthesis/cornea to the upper eyelid margin (MRD1) and lower eyelid margin (MRD2). The levator muscle function was measured from the distance the upper lid margin elevates in millimeters from down gaze to up gaze while placing a finger on the patient’s brow to cancel out the effects of the frontalis muscle. The laxity of the upper eyelid was scored based on the visible exposed upper tarsal conjunctiva by lifting the lid with a finger: grade 0 for no conjunctival exposure; grade 1 for less than one third exposed conjunctiva; grade 2 for one third to one half exposed conjunctiva; and grade 3 for more than one half exposed conjunctiva [13]. The pinch test was used to evaluate the laxity of the lower eyelid. The anterior displacement by maximally pulling the lower eyelid from the globe/prosthesis was measured in millimeters with a Schirmer strip. The anterior position of the normal eye and ocular prosthesis was assessed with Hertel exophthalmometry.
The customized ocular prosthesis was measured as three parameters: size, in the three-dimensional axes with a digital Vernier caliper; weight, with a weighing scale; and volume, with Archimedes’ water displacement method. QoL specific for patients with an ocular prosthesis was assessed for the following four domains: functional abilities with single vision; wearing comfort of the ocular prosthesis; physical appearance and motility of the ocular prosthesis; and psychological well-being and social interactions. The assessment comprised a concise 4-item questionnaire written in Dutch. The questions were: “How do you rate the functioning with an eye prosthesis in general and more specific your visual functioning, how would you rate the physical appearance with your eye prosthesis, how would you rate the comfort with your eye prosthesis, how would you rate your personal feelings, and social functioning with your eye prosthesis”. Patients rated the answers on a gradual visual analogue scale (VAS) as a continuum ranging from 0 for “very poor” to 10 for “very good” [14]. Patients were asked to fill in the form individually and were assisted where needed.
The anophthalmic and fellow orbit were considered statistically significantly different when a P value of <0.05 (paired sample t test) was found for one or more of the following parameters: superior eyelid sulcus depression; upper eyelid laxity; marginal reflex distance; lagophthalmia; palpebral fissure height; levator muscle function; enophthalmia; and lower eyelid laxity. A clinically observable difference was determined as ≥1 grade for superior eyelid sulcus depression, and upper eyelid laxity; ≥1 mm for marginal reflex distance and lagophthalmia; ≥2 mm for palpebral fissure height, levator muscle function, enophthalmia, and lower eyelid laxity. Statistical correlation analysis was performed using the Spearman rank test for continuous and ordinal variables and the Kruskal–Wallis test for nominal variables.
Results
Of the 100 patients who presented between October 2018 and November 2019, 59 patients (59%) were included in the study. Of the 41 excluded patients (41%), 17 patients (17%) had prior eyelid surgery, 14 patients (14%) received secondary orbital implant insertion or exchange, 7 patients (7%) had the eye removed before 18 years of age, and 3 patients (3%) had an orbital implant of 16 mm or smaller, or a prosthetic volume of more than 3 mL. The patients’ characteristics are summarized in Table 2. The mean age was 59 years (range: 25–91 years). The patients had been wearing a regularly fitted and properly maintained customized ocular prosthesis for a mean period of 12 years (range: 2–63 years).
The anophthalmic side was statistically significantly different from the other side for the following clinical features of AS syndrome: superior eyelid sulcus depression, MRD1, levator muscle function, lid lag, and exophthalmometry. The clinically observable differences were: impaired levator muscle function (49 patients, 83%), superior eyelid sulcus depression (41 patients, 69%), upper eyelid ptosis (28 patients, 47%), upper eyelid retraction (14 patients, 24%), eyelid closure defect (31 patients, 53%), and enophthalmia (31 patients, 53%) (Table 3). The mean prosthetic volume was 2.2 mL with a mean weight of 2.3 g, and a mean size in height of 23.1 mm, width of 24.6 mm, and depth of 7.5 mm. The mean domain QoL VAS score related to the ocular prosthesis was 7.6 for functional abilities with single vision, 7.8 for comfort, 7.3 for physical appearance and motility, and 7.5 for psychological well-being and social interactions. Various clinical features of AS syndrome were significantly associated with disease- and prosthetic-specific data, such as prior orbital radiotherapy, duration of prosthetic wear, and size of the prosthesis (Table 4). None of the clinical aspects of AS syndrome were associated with QoL scores, except for upper eyelid ptosis, which was associated with increased perceived wearing comfort of the prosthesis. There was no association between the aetiology of the eye loss and the development of AS syndrome.
Discussion
To our knowledge, this is the first study to correlate clinical findings with QoL in patients with an ocular prosthesis. We demonstrated that clinical AS syndrome is prevalent in 53% of patients with acquired anophthalmia, with new findings of impaired levator muscle function and lagophthalmia, and that none of these features decreased patient QoL. The relatively high QoL of living with an ocular prosthesis is in line with a previously reported satisfaction rate of 78% [15], although inclusion bias from patients willing to participate in the study may confound the subjective scoring.
Sulcus superior depression and enophthalmos are typical clinical signs of orbital volume deficiency. We found no association between superior sulcus depression and implant size in our study cohort. While some degree of orbital volume loss is inevitably present despite optimally sized implants, other factors such as the position of the implant and the shape and volume of the prosthesis also play a role in the superior sulcus configuration [16, 17]. Kaltreider and Lucarelli demonstrated that 85% of patients with superior sulcus deformity and prosthetic enophthalmos were successfully corrected with adequate orbital volume replacement [8, 18]. Accurate sizing and posterior positioning of the implant remain imperative to reduce development of AS syndrome [16, 17]. Enophthalmos of the prosthesis at an average of 2 mm was encountered in 54% of our patients, which is in line with the study of Kaltreider and Lucarelli [8]. Routine generous volume correction, with a large-sized spherical orbital implant (i.e., 22 mm diameter or more) or with a bulky prosthesis, is however discouraged as it promotes new, or, increases preexisting lagophthalmia and eyelid closure defects, with negative impact on wearing comfort. However, lagophthalmia, present in 54% of our patients, was not associated to the size and volume of the prosthesis and implant. As the QoL for wearing comfort and physical appearance was not impaired in our study patients with sulcus superior depression and enophthalmos, we may conclude that surgeons and ocularists are more concerned about these clinical features of volume loss than the patients themselves [19].
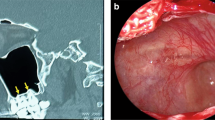
The levator muscle function was clearly impaired at the anophthalmic side, affecting 83% of the patients, and was not associated with eyelid malposition such as ptosis or retraction (Fig. 1). Kim and Khwarg postulated the relative changes in the levator muscle pathway and its reduced resting length as the mechanism of reduced levator function in anophthalmic sockets [20]. The push-up effect of a vertically enlarged prosthesis can shift the pivot point anteriorly and superiorly with subsequent correction of the eyelid malfunctioning and malpositioning. On the other hand, impaired levator function can also be caused by volume deficiency related to small orbital implants [17, 20]. Accordingly, positioning the implant deep into the orbit can improve the upper eyelid function and height [20, 21]. The possible role of the superior rectus muscle in impaired levator muscle function was not investigated in this study. Nevertheless, impaired function of the levator muscle did not negatively affect QoL.
Upper eyelid ptosis as part of AS syndrome is controversial [1]. While often considered a dominant feature of AS syndrome, ptosis is reportedly present between 2 and 25% of AS syndrome [21,22,23]. Conversely, upper lid retraction was described by Smit et al. as an aspect of loss of orbital volume, particularly in patients without an implant, and was attributed to the rotational backward tilting of the superior levator/rectus muscle complex [7]. In our series, ptosis was more prevalent than retraction and was not correlated with implant size. Repetitive manipulation of the eyelid to insert and remove the ocular prosthesis may stretch the muscular tissues [24]. Dehiscence of the levator muscle in this setting may be analogous to the pathogenesis of ptosis in prolonged contact lens wear, eye rubbing, and floppy eyelid syndrome [25, 26]. Because laxity of the anophthalmic upper eyelid was not associated with ptosis, altered positioning rather than elongation of the tissues seems to be the underlying mechanism. Prolonged prosthetic wear in predisposed patients is a possible other causative factor. In an effort to accommodate the height of the upper eyelid, the size and shape of the prosthesis can be adapted, however for ptosis, often at the expense of inducing lagophthalmia [27]. Interestingly, the presence of anophthalmic ptosis was associated with increased QoL for wearing comfort of the prosthesis. This may be explained by the small evaporation area from a reduced interpalpebral surface of the prosthesis. Retraction, on the other hand, was associated with prolonged prosthetic wear. The aetiology of this complication remains however unknown and is likely multifactorial. Orbital volume deficiency and the mechanical effects of the orbital implant and the prosthesis are significant contributory factors [21].
Laxity of the lower eyelid has been described as part of the AS syndrome and is believed to be derived from gravitational forces from the prosthesis, which alter the vectors of the lower eyelid and orbital septum [28]. In our study cohort, lower eyelid laxity was not highly prevalent (20%) as opposed to an incidence of 46% in the study of Kashkouli et al. [29]. Laxity was associated with a short history of prosthetic wear but not to a large prosthetic volume [18]. A possible explanation for the low prevalence of lower lid laxity is the small volume and reduced weight of the prosthesis in our study cohort, which was one of the inclusion criterions.
The limitations of this study are the cross-sectional design and the lack of data on orbital volume from volumetric imaging studies. Further, the absence of patients with a porous implant and dermis fat graft, and glass or stock eyes, in our study cohort precludes translation of the results to all patients with a prosthesis. In some patients information was lacking on the surgical technique and implant wrapping, which are factors that can influence the occurrence of AS syndrome. However, we believe the study cohort is a representative sample of patients with acquired anophthalmia without apparent socket complications.
In conclusion, most patients with acquired anophthalmia and a primary orbital implant have one or more distinct clinical features of AS syndrome without a negative impact on patient QoL. These findings underscore the importance to tailor prosthetic and surgical treatment to the patient’s perceived QoL rather than to objective clinical findings. It raises the awareness to introduce ocular prosthesis-specific QoL assessment in the daily clinical management of patients with anophthalmia.
Summary
What was known before
-
Despite adequate primary orbital volume replacement, AS syndrome still presents.
What this study adds
-
Clinical AS syndrome is prevalent in 53% of patients with acquired anophthalmia, but does not lower patient QoL.
-
New findings of impaired levator muscle function and lagophthalmia are introduced to the AS syndrome.
-
Duration of prosthetic wear, prior orbital radiotherapy, and size of the prosthesis are correlated to AS syndrome.
References
Vistnes LM. Mechanism of upper lid ptosis in the anophthalmic orbit. Plast Reconstr Surg. 1976;58:539–45.
McBain HB, Ezra DG, Rose GE, Newman SP. Appearance Research Collaboration (ARC). The psychosocial impact of living with an ocular prosthesis. Orbit. 2014;33:39–44.
Ahn JM, Lee SY, Yoon JS. Health-related quality of life and emotional status of anophthalmic patients in Korea. Am J Ophthalmol. 2010;149:1005–11.e1.
Goiato MC, dos Santos DM, Bannwart LC, Moreno A, Pesqueira AA, Haddad MF, et al. Psychosocial impact on anophthalmic patients wearing ocular prosthesis. Int J Oral Maxillofac Surg. 2013;42:113–9.
Pine NS, de Terte I, Pine KR. Time heals: an investigation into how anophthalmic patients feel about eye loss and wearing a prosthetic eye. J Ophthalmol Vis Sci. 2017;2:1018.
Rasmussen ML, Ekholm O, Prause JU, Toft PB. Quality of life of eye amputated patients. Acta Ophthalmol. 2012;90:435–40.
Smit TJ, Koornneef L, Zonneveld FW, Groet E, Otto AJ. Primary and secondary implants in the anophthalmic orbit. Preoperative and postoperative computed tomographic appearance. Ophthalmology. 1991;98:106–10.
Kaltreider SA, Lucarelli MJ. A simple algorithm for selection of implant size for enucleation and evisceration: a prospective study. Ophthalmic Plast Reconstr Surg. 2002;18:336–41.
Jordan DR. Porous versus nonporous orbital implants: a 25-year retrospective. Ophthalmology. 2018;125:1317–9.
Shah CT, Hughes MO, Kirzhner M. Anophthalmic syndrome: a review of management. Ophthalmic Plast Reconstr Surg. 2014;30:361–5.
Choi BH, Lee SH, Chung WS. Correction of superior sulcus deformity and enophthalmos with porous high-density polyethylene sheet in anophthalmic patients. Korean J Ophthalmol. 2005;19:168–73.
Liang L, Sheha H, Fu Y, Liu J, Tseng SC. Ocular surface morbidity in eyes with senile sunken upper eyelids. Ophthalmology. 2011;118:2487–92.
Liu DT, Di Pascuale MA, Sawai J, Gao YY, Tseng SC. Tear film dynamics in floppy eyelid syndrome. Investig Ophthalmol Vis Sci. 2005;46:1188–94.
Spiekermann C, Amler S, Rudack C, Stenner M. The visual analog scale as a comprehensible patient-reported outcome measure (PROM) in septorhinoplasty. Aesthetic Plast Surg. 2018;42:859–66.
Song JK, Oh J, Baek SH. A survey of satisfaction in anophthalmic patients wearing ocular prosthesis. Graefes Arch Clin Exp Ophthalmol. 2006;244:330–5.
Su GW, Yen MT. Current trends in managing the anophthalmic socket after primary enucleation and evisceration. Ophthalmic Plast Reconstr Surg. 2004;20:274–80.
Kaltreider SA, Shields MD, Hippeard SC, Patrie J. Anophthalmic ptosis: investigation of the mechanisms and statistical analysis. Ophthalmic Plast Reconstr Surg. 2003;19:421–8.
Kaltreider SA. The ideal ocular prosthesis: analysis of prosthetic volume. Ophthalmic Plast Reconstr Surg. 2000;16:388–92.
Smerdon DL, Sutton GA. Analysis of the factors involved in cosmetic failure following excision of the eye. Br J Ophthalmol. 1988;72:768–73.
Kim NJ, Khwarg SI. Decrease in levator function in the anophthalmic orbit. Ophthalmologica. 2008;222:351–6.
Shams PN, Selva D. ANZSOPS Eyelid Retraction in Anophthalmia Survey Group. Upper eyelid retraction in the anophthalmic socket: review and survey of the Australian and New Zealand Society of Ophthalmic Plastic Surgeons (ANZSOPS). Ophthalmic Plast Reconstr Surg. 2014;30:309–12.
Quaranta-Leoni FM. Treatment of the anophthalmic socket. Curr Opin Ophthalmol. 2008;19:422–7.
Jung SK, Cho WK, Paik JS, Yang SW. Long-term surgical outcomes of porours polyethylene orbital implants: a review of 314 cases. Br J Ophthalmol. 2012;96:494–8.
Leatherbarrow B, Kwartz J. Ocular prostheses. BMJ. 1991;302:1208.
Van den Bosch WA, Lemij HG. Blepharoptosis induced by prolonged hard contact lens wear. Ophthalmology. 1992;99:1759.
Dutton JJ. Surgical management of floppy eyelid syndrome. Am J Ophthalmol. 1985;99:557.
Mombaerts I, Groet E. Upper eyelid ptosis surgery using a preparatory ocular prosthesis. Ophthalmic Plast Reconstr Surg. 2009;25:90–3.
Nolan WB III, Vistnes LM. Correction of lower lid laxity in the anophthalmic orbit: a long-term follow-up. Plast Reconstr Surg. 1983;72:289–93.
Kashkouli MB, Zolfaghari R, Es'haghi A, Amirsardari A, Abtahi MB, Karimi N, et al. Tear film, lacrimal drainage system, and eyelid findings in subjects with anophthalmic socket discharge. Am J Ophthalmol. 2016;165:33–8.
Author information
Authors and Affiliations
Contributions
SR, IM has contributed to the conception of the work, analysis and interpretation of the data, and writing of the paper. All authors have contributed significantly and are in agreement with the content of the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ruiters, S., Mombaerts, I. The prevalence of anophthalmic socket syndrome and its relation to patient quality of life. Eye 35, 1909–1914 (2021). https://doi.org/10.1038/s41433-020-01178-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01178-2
This article is cited by
-
Komplikationen der anophthalmischen Orbita – Therapie und Nachsorge
Die Ophthalmologie (2023)
-
Post-enucleation socket syndrome—a novel pathophysiological definition
Graefe's Archive for Clinical and Experimental Ophthalmology (2022)