Abstract
Purpose
Our aim is to compare foveal microvascular structure, foveal retinal thickness, and best-corrected visual acuity (BCVA) in children with a history of premature retinopathy (ROP) and healthy children. It is also evaluated whether microvascular structural changes in the course of ROP had resulted from treatment modalities of ROP or the disease itself.
Methods
This is a cross-sectional observational comparative study. Seventy-one children were analyzed in four different groups: children treated with bevacizumab (18), or laser (19) for ROP; or spontaneously regressed disease (18) and non-premature healthy children (16). We analyzed foveal avascular zone (FAZ) and vessel densities (VDs) of the superficial capillary plexus (SCP) and deep capillary plexus (DCP) at foveal and parafoveal region with optical coherence tomography angiography (OCT-A). Foveal thickness was measured by cross-sectional OCT. Correlations between FAZ area, foveal VD, central foveal thickness (CFT), BCVA, gestational age (GA), and birth weight (BW) were evaluated.
Results
After comparing of OCT-A parameters between all premature children (groups 1–3) and non-premature children (group 4), significant differences were found in VD-SCP (whole), VD-SCP (foveal), VD-SCP (parafoveal), CFT, and VD-DCP (foveal) (all p < 0.001). Significantly smaller FAZ area was also noted in ROP children. Higher foveal VD of SCP, DCP, and smaller FAZ area were significantly associated with lower GA and BW.
Conclusion
By using OCT-A, significant foveal microvascular anomalies were identified in children with ROP irrespective of the treatment option or spontaneous regression. There has been a correlation between microvascular anomalies, CFT, and a lower BCVA.
Similar content being viewed by others
Introduction
Retinopathy of prematurity (ROP) is a vasoproliferative retinal disorder that is one of the leading cause of childhood blindness worldwide [1]. The mechanism of this disease mainly includes the arrest of normal retinal vascular development that results in aberrant pathological retinal vascularization [2]. Conventional treatment of ROP has been established with ablative therapy including cryotherapy and laser photocoagulation of the avascular retina in order to halt disease progression [3, 4]. In pathogenesis of ROP, the role of vascular endothelial growth factor (VEGF) has been well recognized and later on, studies have shown a clear treatment benefit of intravitreal anti-VEGF injections in severe ROP cases resulting in prompt regression [5, 6].
After the use of optical coherence tomography (OCT) to image retinal structures in premature children, studies have revealed several abnormalities, including cystoid macular edema, retention of inner retinal layers at the foveal center, and absence of foveal depression [7, 8]. OCT angiography (OCT-A) is a relatively novel, fast, and noninvasive imaging modality to study blood flow within macula without need for an intravenous dye [9]. OCT-A can also be applied outside the macula, including anterior segment [10]. Apart from fluorescein angiography (FA), OCT-A specifically has been able to identify retinal capillary plexuses individually, including the superficial capillary plexus (SCP) and deep capillary plexus (DCP) [11]. Studies have shown novel findings regarding vascular changes in several retinal diseases such as age-related macular degeneration and diabetic retinopathy with OCT-A with higher sensitivity and specificity [12, 13].
Mintz-Hittner et al. [14] have analyzed foveal avascular zone (FAZ) of premature children aged between 1 and 17 years by using FA. They have concluded that a small FAZ area might be a predictive mark for prematurity. Similarly, recent studies have observed significantly smaller FAZ in ROP patients than in normal healthy subjects revealed by OCT-A [15, 16]. Moreover, higher foveal vessel density with significant correlations between gestational age (GA) and birth weight (BW) have been shown in the OCT-A examination of premature children [17]. In the present study, we aimed to assess foveal vascular structure of premature children by OCT-A and compare the OCT-A parameters between children who received treatment either with intravitreal bevacizumab (IVB) or laser, children with a history of spontaneously regressed ROP, and healthy term born children.
Methods
This is a cross-sectional observational comparative study conducted in Bakirkoy Dr. Sadi Konuk Training and Research Hospital, Istanbul, Turkey. The study was approved by the ethics committee of the same hospital and adhered to the tenets laid out in the Declaration of Helsinki. Routine screening examinations for ROP have been performed in all premature infants by indirect ophthalmoscopy with the help of a 28D condensing lens according to the established guidelines [18]. Definitive staging at the time of treatment was confirmed by two different retina specialists. Infants have been treated in accordance with the indications established by the Early Treatment for ROP Study [19]. Fundus images were recorded for most infants with the RetCam II Imaging System (Clarity Medical Systems, Pleasanton, CA, USA) before treatment.
All children with preterm birth and a diagnosis of ROP between May 2019 and August 2019 were invited to participate in the study. Sixteen non-premature healthy children with normal ophthalmologic examination were also included in the study. All participants underwent standard ophthalmologic examination including cycloplegic refraction, best-corrected visual acuity (BCVA) evaluation, slit-lamp examination, and fundus examination. Snellen BCVA was then converted into logMAR for analysis. Exclusion criteria included any retinal disorder other than ROP, media opacity preventing imaging, glaucoma, history of any ocular surgery, and receiving another treatment before anti-VEGF injection or after the primary treatment for reactivation of the disease. Furthermore, children with low cooperation during examinations and children with low vision that prevents ocular examinations were also excluded.
After the exclusion, participants were divided into four groups, namely group 1—premature children who received anti-VEGF treatment with a diagnosis of type 1 ROP or aggressive posterior ROP in zone 1 or posterior zone 2, group 2—children who received laser treatment with a diagnosis of type 1 ROP in zone 2, group 3—children with a history of spontaneously regressed ROP without any treatment, and group 4—age-matched, full-term (defined as GA over 39 weeks) healthy children with normal ocular examinations.
The anti-VEGF agent that had been used was 0.625 mg (0.025 mL) of bevacizumab (Avastin; Genentech, Inc., San Francisco, CA). Bevacizumab was injected 1 mm behind the temporal limbus via pars plicata with a 31-gauge needle taking care to avoid crystalline lens damage. This technique was based on previous literature data [5]. Laser photocoagulation had been performed with a 810-nm diode laser device (Iridex; Oculight SL, Mountain View, CA, USA) in neonatal intensive care unit under supervision of a neonatologist. Regression of the disease was noted in all patients in group 1 and group 2.
OCT-A analysis
The OCT-A using the split-spectrum amplitude-decorrelation angiography algorithm (RTVue XR Avanti with AngioVue; Optovue, Inc., Fremont, CA) was performed for all participants. A 6 mm × 6 mm rectangle scan centered on the fovea was performed.
After dilatation of pupil, imaging was done in an upright position without sedation. Motion correction to minimize artifacts in poor cooperative children was performed. Since the ability to fixate and maintain a stable head position during the OCT-A exam is necessary to obtain a good image quality, children who could not cooperate with the examination or those from whom poor imaging quality was obtained (signal strength index lower than 50) were excluded. Two consecutive measurements were obtained for each subject and the average value was analyzed. Each scan is automatically divided into segments by the software using the AngioVue module in order to visualize the SCP and DCP in the retina. The FAZ area was determined on the central fovea with a clinically visible distinct avascular area without crossing vessels in the full retina. The FAZ area was automatically selected and calculated (in millimeters squared—mm2). If the FAZ could not be calculated due to the presence of vessels on the fovea center, the FAZ area was recorded as zero. Spectral-domain (SD)-OCT B scans using the same instrument were used for assessment of foveal contour and central foveal thickness (CFT). CFT was defined as the average retinal thickness within the central 1-mm diameter ring. We obtained foveal and the parafoveal vessel density for the SCP and DCP using the built-in software. The “parafovea” is defined as an annulus centered on the fovea with inner and outer ring diameters of 1 and 3 mm, respectively. The whole, foveal, and parafoveal vessel densities (VDs) (as a percentage) of the SCP and DCP, the size of FAZ area (mm2), and CFT were analyzed.
Statistical analyses
Statistical Package for Social Sciences-21 was used for statistical analysis. Qualitative data were expressed as number and percentage, whereas continuous values were expressed as mean and standard deviation or median and range when appropriate. Chi-square and Fisher’s exact tests were used to compare the qualitative data. The distribution of the parameters was tested with either the Kolmogorov–Smirnov or Shapiro–Wilk tests. Depending upon the distribution of the parameters, one-way analysis of variance (ANOVA) with Tukey test as post hoc analyses or the Kruskal–Wallis with the Mann–Whitney U test with a post hoc analysis was used to compare the quantitative data. Statistical significance was assessed at levels of p < 0.05.
Results
A total of 71 children were evaluated during the study. There were 18 children (25.4 %), including 10 girls and 8 boys in group 1, 19 children (26.8 %), including 14 girls and 5 boys in group 2, 18 children (25.4 %), including 7 girls and 11 boys in group 3, and 16 children (22.4 %), including 10 girls and 6 boys in group 4. The sex distribution was similar between the groups (p = 0.188). No significant differences of GA and BW were observed between groups 1, 2, and 3 (p = 0.271, p = 0.072, respectively) except for group 4 (p < 0.001), which had significantly higher GA and BW. The mean ages at the time of OCT-A examination were similar between all groups in the study (p = 0.161). Demographic characteristics in the study were given in Table 1. Regarding disease characteristics, 6 children had zone 1 ROP and 12 children had posterior zone 2 ROP in group 1; all children in group 2 had zone 2 ROP. Four children had stage 2 ROP and 14 children had stage 3 ROP in group 1; 9 children had stage 2 ROP and 10 children had stage 3 ROP in group 2. The zone of ROP significantly differed between groups 1 and 2 (p = 0.006); ROP stage was similar between the two groups (p = 0.137).
There was a significant difference of BCVA between the groups (p < 0.001). Pairwise comparisons showed significantly worse BCVA in group 1 than in group 3 and group 4 (p = 0.022 and p = 0.004, respectively). The BCVA was also worse in group 2 compared to group 4 (p = 0.029). After comparison of BCVA between all children born prematurely (groups 1–3) and children born at term (group 4), it was found that BCVA was significantly better in term born children than in premature children (0.11 ± 0.12 vs 0.04 ± 0.05, p = 0.035). Refractive status (SE) did not significantly differ between the groups (p = 0.057). The BCVA and refractive status of children were summarized in Table 1.
Regarding OCT-A parameters, there were significant differences of VD-SCP (whole), VD-SCP (foveal), VD-SCP (parafoveal), CFT, VD-DCP (foveal), and FAZ area between the groups (p = 0.023, p = 0.009, p = 0.022, p < 0.001, p = 0.017, and p = 0.003, respectively). Post hoc analysis showed that VD-SCP (whole) was significantly lower in group 2 than in group 4 (p = 0.015). VD-SCP (foveal) was significantly higher in groups 1 and 3 compared to group 4 (p = 0.006, p = 0.040, respectively). VD-SCP (parafoveal) was significantly lower in group 1 than in group 4 (p = 0.033). The CFT was significantly thicker in groups 1–3 than in group 4 (p < 0.001, p < 0.001, and p = 0.007, respectively). VD-DCP (foveal) was significantly higher in groups 1 and 3 as compared to group 4 (p = 0.033, p = 0.022, respectively). FAZ area was significantly smaller in groups 1–3 than in group 4 (p = 0.019, p = 0.011, and p = 0.007, respectively). After comparing of OCT-A parameters between all premature children (groups 1–3) and healthy controls (group 4), it was found that VD-SCP (whole), VD-SCP (foveal), VD-SCP (parafoveal), CFT, VD-DCP (foveal), and FAZ area showed significant differences (p < 0.001, p = 0.001, p = 0.001, p < 0.001, p < 0.001, and p = 0.011, respectively). The OCT-A results obtained in the study were shown in Table 2. Figure 1 shows the distribution of FAZ area in each group.
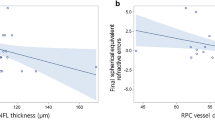
Correlation results are summarized in Table 3. There were significant correlations between GA, BW, BCVA, and OCT-A parameters. The foveal VDs of both SCP and DCP were significantly associated with lower GA and BW. A smaller FAZ area was significantly correlated to lower GA and BW. Furthermore, increased VD in foveal SCP and DCP was significantly correlated to higher logMAR BCVA indicating that worse visual acuity was associated with denser vasculature in SCP and DCP at fovea. Increased CFT was also correlated to a smaller FAZ area and higher foveal VD in SCP and DCP. Figure 2 depicts correlation status between VD-SCP (foveal), VD-DCP (foveal), FAZ, GA, and BW.
Discussion
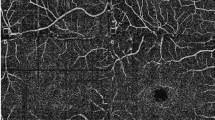
The present study compared differences in foveal microvascular structure by using OCT-A between eyes that had received treatment for ROP (either with IVB or laser), those had spontaneously regressed ROP and eyes of the age-matched, full-term healthy children. We found that SCP and DCP VDs and FAZ area significantly differed between premature and term children. The VDs of SCP and DCP were lower at parafoveal region whereas they were significantly higher at the fovea of premature children as compared to those of term ones (Fig. 3). The FAZ area was significantly smaller and CFT was significantly thicker in premature children compared to term children. We also noticed that differences in OCT-A parameters occured only between premature group (groups 1–3) and term group (group 4). Moreover, there were significant associations between GA, BW, and OCT-A parameters indicating that lower GA and BW were correlated with higher foveal VDs in SCP and DCP and smaller FAZ area. These findings may suggest that GA and BW play significant roles in foveal vascular development irrespective of treatment effect either with IVB or laser for ROP.
Optical coherence tomography angiography (OCTA) images of superficial capillary plexus (SCP), deep capillary plexus (DCP), Foveal avascular zone (FAZ) and cross-sectional OCT in anti-VEGF group (a–d), in laser group (e–h), in spontaneously regressed ROP group (i–l) and in nonpremature healthy children (m–p).
Studies have shown developmental abnormalities of fovea in preterm infants by using SD-OCT. It has been shown that existence of retinal layers other than outer nuclear layer in central part of fovea might induce a thicker central fovea in premature children [7]. Lee et al. [20] have observed that retinal layers in the macula remained thicker in laser and laser-treated + IVB-treated children compared to children who received IVB treatment as monotherapy. Investigators have proposed that destruction of peripheral avascular retina by laser, as opposed to IVB which allows normal retinal vascularization from the point of treatment, could block peripheral migration and reorganization of inner retinal cells leading to a higher CFT [20]. In the present study, although we found CFT significantly thicker in preterm children, we did not identify a significant difference of CFT between IVB-treated, laser-treated, and spontaneously regressed children.
Early researchers have assumed that fovea was initially completely vascularized and subsequently avascularized by vessel degeneration that formed the FAZ area. Mintz-Hittner et al. [14] have indicated that densely vascular meshwork at FAZ was regressed by apoptosis in all infants over 36 weeks of GA but apoptosis did not occur in premature infants under 30 weeks of GA rendering them with a small or absent FAZ. However, subsequent studies have shown that the foveal region is never vascularized [21]. Recently, it has been found that angiostatin, primarily a pigment epithelium-derived factor, is expressed in the foveal region to inhibit vascular growth [22]. VEGF plays an important role in the ingrowth of retinal vessels into the central fovea. Thus, an increased level of VEGF in the period of FAZ formation in ROP may disrupt the balance, resulting in a small or absent FAZ. Supportively, lower GA and BW were significantly associated with a smaller FAZ area in our study suggesting that ROP itself plays a role in smaller FAZ formation.
Lepore et al. [23] have demonstrated absence of FAZ in preterm children 9 months following treatment that predominantly occured in IVB-treated infants compared to laser-treated infants. In a recent study, Mansukhani et al. [24] have compared fluorescein angiography findings between infants treated with IVB and infants with spontaneous regression. They have concluded that abnormal vascular patterns in fluorescein angiography result from ROP process itself rather than as a result of IVB treatment. In our study, FAZ area was significantly smaller in premature children compared to healthy term children. This finding was in compatible with previous studies which indicated smaller FAZ in preterm children by using OCT-A [15,16,17, 25].
The importance of VEGF has been emphasized in retinal vessel growth into the fovea. It has been postulated that increased VEGF level during FAZ formation in ROP may play a role in smaller FAZ formation. Although previous reports have suggested that laser treatment may have a more favorable effect on foveal development by partial suppression of VEGF as compared to IVB, which results in complete suppression [16, 26], we did not identify a significant difference of FAZ and OCT-A parameters between IVB- and laser-treated children.
Chen et al. [17] have found significantly higher VD in foveal SCP and DCP in IVB-treated preterm children compared to healthy subjects. They also observed that SCP density was associated with suboptimal visual acuity results. Similarly, Falavarjani et al. [25] have reported significantly increased foveal VD in SCP in preterm children compared to healthy term children. Takagi et al. [16] have found lower VD of SCP in whole image scan in ROP group (52.6%) than in control group (53.9%). They also demonstrated higher foveal VD (35.7% vs 30.1%) with lower parafoveal VD (54.1 vs 56.4%) in SCP of ROP patients compared to control subjects. Our results regarding foveal and parafoveal VD in children with ROP history showed a clear resemblance to those in that study. In our study, children in ROP groups exhibit similar foveal and parafoveal VD of SCP and DCP with significantly higher foveal VD and lower parafoveal VD in SCP and DCP in preterm children than in control children. We believe that lower VEGF levels during vascular development of the parafoveal region as a result of suppression after anti-VEGF or laser therapy could be the responsible factor for lower parafoveal VDs.
Miki et al. [26] have assessed foveal vascular structure between laser-treated preterm children, preterm children with no history of ROP, and controls. Although they found a smaller FAZ in laser-treated children, they did not find an association between FAZ and visual acuity. Balasubramanian et al. [27] have evaluated visual function and OCT-A parameters between preterm children with no ROP history, preterm children who formerly received laser therapy, and term born controls. They found that poor visual acuity was correlated to increased foveal SCP-VD and DCP-VD and smaller FAZ. Similarly, our results showed a significant association of worse visual acuity with denser vasculature in SCP and DCP at fovea. But we could not identify a relationship between BCVA and FAZ area. The impact of foveal structural morphology and vascular abnormalities on visual function remain controversial. Studies have proposed the insignificance of foveal pit formation for visual performance where others have not [28, 29]. A study has demonstrated good visual acuity in patients with mild foveal hypoplasia without a distinct FAZ [30]. In the present study, we found significant relationship between a thicker central fovea with increased SCP-VD, DCP-VD, and smaller FAZ area.
In conclusion, we evaluated foveal as well as parafoveal vascular and structural changes in children with ROP in three different groups (laser treated, anti-VEGF treated, and spontaneously regressed). We also compared same parameters with non-premature healthy children. Through the use of OCT-A, we identified several foveal microvascular anomalies, including smaller FAZ, and increased central foveal VD in all eyes with ROP regardless of treatment option or whether it was treated or not. Furthermore, a correlation between foveal microvascular anomalies, CFT, and suboptimal visual acuity was demonstrated.
Limitations
The axial length, which is known to affect vessel density measurements on macular OCT-A, has not been evaluated in this study. However, we indirectly suggest that axial lengths could be similar in all groups because there was no significant difference in refraction between the groups (except myopic refraction in group 2 that had probably been resulted from laser therapy). Since premature children without ROP were not included in our study, it was not possible to distinguish whether the observed retinal vascular and structural changes were entirely resulted from ROP, or to some extent prematurity itself contributed. Patients with poor visual function were also excluded in the current study. In our opinion, further studies including eyes with poorer visual acuity are necessary to understand the role of foveal vascular abnormalities in visual outcomes.
Summary
What was known before
-
In the present study, we evaluated the foveal microvascular and structural changes in children with ROP in three different groups (treated with two different treatment modalities and spontaneously regressed) and compared their results with term born children.
-
We aimed to investigate whether the treatment modalities or disease itself is the responsible factor for those changes.
What this study adds
-
We evaluated foveal as well as parafoveal vascular and structural changes in children with ROP in three different groups (laser treated, anti-VEGF treated, and spontaneously regressed).
-
We also compared the changes them with full-term children.
-
Through the use of OCT-A, we identified several foveal microvascular anomalies, including smaller FAZ, and increased central foveal VD in all eyes with ROP regardless of treatment option and treated or not.
References
Leng Y, Huang W, Ren G, Cai C, Tan Q, Liang Y, et al. The treatment and risk factors of retinopathy of prematurity in neonatal intensive care units. BMC Ophthalmol. 2018;18:301. https://doi.org/10.1186/s12886-018-0973-1.
Hellström A, Smith LE, Dammann O. Retinopathy of prematurity. Lancet. 2013;382:1445–57.
Multicenter trial of cryotherapy for retinopathy of prematurity. Preliminary results. Cryotherapy for Retinopathy of Prematurity Cooperative Group. Arch Ophthalmol. 1988;106:471–9.
Early Treatment For Retinopathy Of Prematurity Cooperative Group. Revised indications for the treatment of retinopathy of prematurity: results of the early treatment for retinopathy of prematurity randomized trial. Arch Ophthalmol. 2003;121:1684–94.
Wu WC, Kuo HK, Yeh PT, Yang CM, Lai CC, Chen SN. An updated study of the use of bevacizumab in the treatment of patients with prethreshold retinopathy of prematurity in taiwan. Am J Ophthalmol. 2013;155:150–8.
Hwang CK, Hubbard GB, Hutchinson AK, Lambert SR. Outcomes after intravitreal bevacizumab versus laser photocoagulation for retinopathy of prematurity: a 5-year retrospective analysis. Ophthalmology. 2015;122:1008–15.
Erol MK, Ozdemir O, Turgut Coban D, Bilgin AB, Dogan B, Sogutlu Sari E, et al. Macular findings obtained by spectral domain optical coherence tomography in retinopathy of prematurity. J Ophthalmol. 2014;2014:468653. https://doi.org/10.1155/2014/468653.
Villegas VM, Capó H, Cavuoto K, McKeown CA, Berrocal AM. Foveal structure-function correlation in children with history of retinopathy of prematurity. Am J Ophthalmol. 2014;158:508–12.
Yeo JH, Chung H, Kim JT. Swept-source optical coherence tomography angiography according to the type of choroidal neovascularization. J Clin Med. 2019;8:1272.
Lee WD, Devarajan K, Chua J, Schmetterer L, Mehta JS, Ang M. Optical coherence tomography angiography for the anterior segment. Eye Vis. 2019;6:4.
Park JJ, Soetikno BT, Fawzi AA. Characterization of the middle capillary plexus using optical coherence tomography angiography in healthy and diabetic eyes. Retina. 2016;36:2039–50.
Ashraf M, Nesper PL, Jampol LM, Yu F, Fawzi AA. Statistical model of optical coherence tomography angiography parameters that correlate with severity of diabetic retinopathy. Investig Ophthalmol Vis Sci. 2018;59:4292–8.
You QS, Wang J, Guo Y, Flaxel CJ, Hwang TS, Huang D, et al. Detection of reduced retinal vessel density in eyes with geographic atrophy secondary to age-related macular degeneration using projection-resolved optical coherence tomography angiography. Am J Ophthalmol. 2019;S0002-9394:30461–1. https://doi.org/10.1016/j.ajo.2019.09.004.
Mintz-Hittner HA, Knight-Nanan DM, Satriano DR, Kretzer FL. A small foveal avascular zone may be an historic mark of prematurity. Ophthalmology. 1999;106:1409–13.
Nonobe N, Kaneko H, Ito Y, Takayama K, Kataoka K, Tsunekawa T, et al. Optical coherence tomography angiography of the foveal avascular zone in children with a history of treatment requiring retinopathy of prematurity. Retina. 2019;39:111–7.
Takagi M, Maruko I, Yamaguchi A, Kakehashi M, Hasegawa T, Iida T. Foveal abnormalities determined by optical coherence tomography angiography in children with history of retinopathy of prematurity. Eye. 2019;33:1890–6.
Chen YC, Chen YT, Chen SN. Foveal microvascular anomalies on optical coherence tomography angiography and the correlation with foveal thickness and visual acuity in retinopathy of prematurity. Graefes Arch Clin Exp Ophthalmol. 2019;257:23–30.
Section on Ophthalmology American Academy of Pediatrics, American Academy of Ophthalmology, American Association for Pediatric Ophthalmology and Strabismus. Screening examination of premature infants for retinopathy of prematurity. Pediatrics. 2006;117:572–6.
Retinopathy of Prematurity Cooperative Group. Revised indications for the treatment of retinopathy of prematurity: results of the early treatment for retinopathy of prematurity randomized trial. Arch Ophthalmol. 2003;121:1684–94.
Lee YS, See LC, Chang SH, Wang NK, Hwang YS, Lai CC, et al. Macular structures, optical components, and visual acuity in preschool children after intravitreal bevacizumab or laser treatment. Am J Ophthalmol. 2018;192:20–30.
Engerman RL. Development of the macular circulation. Investig Ophthalmol Vis Sci. 1976;15:835–40.
Böhm MR, Hodes F, Brockhaus K, Hummel S, Schlatt S, Melkonyan H, et al. Is angiostatin involved in physiological foveal avascularity? Investig Ophthalmol Vis Sci. 2016;57:4536–52.
Lepore D, Quinn GE, Molle F, Baldascino A, Orazi L, Sammartino M, et al. Intravitreal bevacizumab versus laser treatment in type 1 retinopathy of prematurity: report on fluorescein angiographic findings. Ophthalmology. 2014;121:2212–9.
Mansukhani SA, Hutchinson AK, Neustein R, Schetzer J, Allen JC, Hubbard GB. Fluorescein angiography in retinopathy of prematurity: comparison of infants treated with bevacizumab to those with spontaneous regression. Ophthalmol Retina. 2019;3:436–43.
Falavarjani KG, Iafe NA, Velez FG, Schwartz SD, Sadda SR, Sarraf D, et al. Optical coherence tomography angiography of the fovea in children born preterm. Retina. 2017;37:2289–94.
Miki A, Yamada Y, Nakamura M. The size of the foveal avascular zone is associated with foveal thickness and structure in premature children. J Ophthalmol. 2019;2019:8340729. https://doi.org/10.1155/2019/8340729.
Balasubramanian S, Borrelli E, Lonngi M, Velez F, Sarraf D, Sadda SR, et al. Visual function and optical coherence tomography angiography features in children born preterm. Retina. 2018. https://doi.org/10.1097/IAE.0000000000002301.
Marmor MF, Choi SS, Zawadzki RJ, Werner JS. Visual insignificance of the foveal pit: reassessment of foveal hypoplasia as fovea plana. Arch Ophthalmol. 2008;126:907–13.
Provis JM, Dubis AM, Maddess T, Carroll J. Adaptation of the central retina for high acuity vision: cones, the fovea and the avascular zone. Prog Retin Eye Res. 2013;35:63–81.
Pakzad-Vaezi K, Keane PA, Cardoso JN, Egan C, Tufail A. Optical coherence tomography angiography of foveal hypoplasia. Br J Ophthalmol. 2017;101:985–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vural, A., Gunay, M., Celik, G. et al. Comparison of foveal optical coherence tomography angiography findings between premature children with ROP and non-premature healthy children. Eye 35, 1721–1729 (2021). https://doi.org/10.1038/s41433-020-01161-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01161-x
This article is cited by
-
Retinal structure and visual pathway function at school age in children born extremely preterm: a population-based study
BMC Ophthalmology (2023)
-
Evaluation of macular microvascular structure with optical coherence tomography angiography in children with history of treatment for retinopathy of prematurity
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)