Abstract
Background
To investigate the effect of cycloplegia on the ocular biometry and intraocular lens (IOL) power in different age groups.
Methods
This cross-sectional study enrolled 240 right eyes of 240 healthy volunteers. Three groups were formed (range to years; group 1: 50–60, group 2: 30–40 and group 3: 10–20, respectively). We measured keratometry, central corneal thickness (CCT), white-to-white (WtW) distance, anterior chamber depth (ACD), and axial lentgh (AL) both before and after cycloplegia. The IOL powers were calculated using Sanders–Retzlaff–Kraff/theoretical (SRK/T), Holladay 1 and Haigis formulas. AL-Scan (Nidek Co., Gamagori, Japan) was used for all measurements.
Results
There was a significant increased in keratometry, CCT, ACD, AL, and Holladay 1 after cycloplegia (p < 0.05), whereas WtW, SRK/T, and Haigis were not changed significantly in group 1 (p > 0.05). Keratometry, SRK/T, Haigis, and Holladay 1 significantly decreased; ACD and WtW significantly increased postcycloplegia (p < 0.05) but AL and CCT did not change significantly in group 2 (p > 0.05). Significant increased in ACD, CCT, WtW, and AL, significant decreased in SRK/T and Haigis were observed postcycloplegia (p < 0.05), while the changes in keratometry and Holladay 1 were not significant in group 3 (p > 0.05).
Conclusions
This study demonstrated there is significant difference in many ocular parameters and IOL power formulas before and after cycloplegia. Especially, ACD showed significant changes in all age groups. Therefore, to avoid refractive prediction errors the IOL power calculation formulas using the ACD should be considered.
Similar content being viewed by others
Introduction
Cataract extraction and intraocular lens (IOL) implantation is one of the most common surgeries performed worlwide [1, 2]. With the advances in IOL technology and use of premium IOLs, accurate measurement of ocular biometry and IOL power calculation has become essential for reaching the target refraction after cataract surgery. As a result of imprecise biometric measurements, clinicians may encounter unfavorable refractive outcomes [3]. Measurements of axial length (AL), anterior chamber depth (ACD), and keratometry are important parameters for determining effective lens position and IOL power calculation [4]. Several studies have showed that AL, ACD, and keratometry by optical biometry involve contact-free measurement, high resolution, user independence, high repeatability, and reliability [5,6,7].
A complete ophthalmologic evaluation includes dilated fundus examination. So usually, biometry is performed after fundus examination while pupils are dilated. Cycloplegia results in the backward movement of crystalline lens and decreased lens thickness (LT). In addition, the lens becomes flatter and ACD increases [8]. Many studies have reported changes in ocular parameters and IOL power after cycloplegia with different devices; Pentacam [9,10,11], anterior segment optical coherence tomography [12, 13], AL-Scan [14], Lenstar 900 [15,16,17], Aladdin [18], IOLMaster 500, and 700 [8, 16, 19].
To the best of the authors’ knowledge, only one study compared the effects of cycloplegia on ocular biometry and IOL power measurements in two different age groups using IOLMaster 700 [8]. Accordingly, this is the first study to investigate the effect of cycloplegia on the ocular biometry and IOL power in different three age groups using AL-Scan (Nidek Co., Gamagori, Japan).
Methods
Participants
This cross-sectional study enrolled 240 right eyes of 240 healthy volunteers. The study was conducted in accordance with the Declaration of Helsinki, and informed consent was obtained from each participant. This study was approved by the ethics committee of Izmir Katip Çelebi University (2020-GOKAE-0287). Three groups were formed in each group with 80 participants. Mean age was 54.09 ± 3.17 years (range 50–60) in group 1, 34.50 ± 3.02 years (range 30–40) in group 2 and 15.40 ± 2.87 years (range 10–20) in group 3. The number of men and women in the groups was equal. All participants underwent a complete ophthalmic examination including refraction, best-corrected visual acuity (BCVA), slitlamp biomicroscopy, intraocular pressure measurement, and fundus examination. Exclusion criteria included previous ocular surgery, retinal pathology, spherical equivalent refractive error > ±6.00 diopter (D), dry eye, corneal opacity, contact lens wear, cataract, glaucoma, diseases like pterygium, poor fixation, and BCVA of <20/25.
Measurements
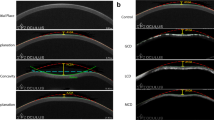
The AL-Scan employs partial coherence interferometry (830 nm) principle to measure the AL and calculates the keratometry using the reflected images over 2.4 and 3.3 mm diameters on the cornea. Pupil size and WtW is also measured from the obtained image of the anterior segment of the eye. ACD and CCT are obtained using the Scheimpflug principle. All measurements were performed at the same time of day (between 10:00 and 12:00 a.m.) to eliminate the effect of diurnal variation. All measurements with the AL-Scan were performed by the same experienced examiner and to create a smooth optical surface over the cornea, participants were asked to blink just before measurements were taken. Quality control criteria were fulfilled in accordance with the manufacturer’s recommendations. Three measurements were acquired before and after cycloplegia and the average was used for analysis. Cycloplegia was achieved using three drops of an eye solution containing 1% cyclopentolate separated by 5 min. After cycloplegia had been achieved and pupillary light reflex was absent, about 45 min later, the measurements were performed. The mean keratometry (over 2.4 mm diameters on the cornea), central corneal thickness (CCT), white-to-white (WtW) distance, ACD, AL readings were recorded both before and after cycloplegia. We completed IOL power calculations with the Sanders–Retzlaff–Kraff/theoretical (SRK/T), Holladay 1, and Haigis formulas both before and after cycloplegia. The refractive target was zero. A single-piece AcrySof IQ SN60WF (Alcon Inc., Fort Worth, Texas, USA) IOL was used to calculate IOL power with a manufacturer recommended A constant (for SRK/T: 119.0, for Holladay 1: 1.85 and for Haigis: a0 = −0.762, a1 = 0.227, a2 = 0.218).
Statistical analysis
Assessment of the normality of data using the Shapiro–Wilk test showed no normal distribution. Data were analyzed in SPSS 22.0 software (IBM Corp., Armonk, New York, USA) using the Wilcoxon signed-rank and Mann–Whitney U tests. A p value of <0.05 was considered statistically significant.
Results
Tables 1–3 show the results of mean keratometry, CCT, WtW, ACD, AL measurements, as well as of IOL power calculations, according to the SRK/T, Holladay 1, and Haigis formulas both before and after cycloplegia in all groups. Table 4 shows comparison of the changes in mean value differences between groups.
There was a significant increased in keratometry, CCT, ACD, AL, and Holladay 1 after cycloplegia (p < 0.05), whereas WtW, SRK/T, and Haigis were not changed significantly in group 1 (p > 0.05) (Table 1). Keratometry, SRK/T, Haigis, and Holladay 1 significantly decreased, ACD and WtW significantly increased postcycloplegia (p < 0.05) but AL and CCT did not change significantly in group 2 (p > 0.05) (Table 2). Significant increased in ACD, CCT, WtW and AL, significant decreased in SRK/T and Haigis were observed postcycloplegia (p < 0.05), while the changes in keratometry and Holladay 1 were not significant in group 3 (p > 0.05) (Table 3).
With and without cycloplegia altered the measurement of IOL power by >0.50 D in 4 cases calculated by SRK/T, 3 cases by Holladay 1 and 6 cases by Haigis formula in group 1, 4 cases by SRK/T, 12 cases by Holladay 1 and 8 cases by Haigis formula in group 2, 8 cases by SRK/T, 8 cases by Holladay 1, and 16 cases by Haigis formula in group 3.
Discussion
Cataract surgery has now become a refractive surgery with the use of premium lenses. There are many causes of refractive prediction errors after cataract surgery. As a 0.1 mm error in AL, ACD or keratometry will correspond to an error of about 0.27 D, 0.15 D, or 0.57 D, respectively in the spectacle plane by assuming normal eye size. Therefore, accuracy within 0.1 mm is requisite [4]. Norrby [20] and Olsen [4] reported that ACD after surgery is the major source of refractive prediction error (35.5% and 42%, respectively). When cycloplegia eliminated accommodation, the crystalline lens becomes flatter and moves posteriorly. Thereby LT decreases and anterior chamber deepens [21]. Many studies have shown that ACD increases after cycloplegia [3, 14, 15, 17, 22]. Similar to previous studies, we found that ACD was significantly increased after cycloplegia in all groups and the most increase was in the 10–20 age group. This result supports the hypothesis that with aging lenticular sclerosis, decrease elasticity of the lens capsule, increase lens size and weight reduce the response of the lens to cycloplegic agents [8]. Higashiyama et al. [23] reported a significant negative correlation between in LT and ACD. On the contrary, Arriola-Villalobos et al. [15] reported that changes in LT were not significant after pupil dilation with tropicamide 1% in an elderly cataract population (mean age, 74.71 ± 53). AL-Scan device has not the ability to measure LT. Therefore, we could not comment on this parameter in our study.
In our study in the 50–60 and 10–20 age groups, CCT showed a significant increase after cycloplegia (1.1 µm and 2.7 µm, respectively), but the increase was not significant in the 30–40 age group. Many studies have shown that CCT increases after cycloplegia [3, 8, 24,25,26]. The mechanism of increase in CCT is not clear. Chang et al. [26] argued, this change was attributed to the possible role of reflex tearing. Zeng and Gao [24] hypothesized that direct contact of Mydrin (contain tropicamide and phenylephrine) with the corneal epithelium destroys the integrity of the epithelium, which causes a resultant edema of the cornea. Some studies have reported a decrease in CCT after cycloplegia [11, 14]. Palamar et al. [11] assumed that topical cyclopentolate which is an atropin-like muscarinic receptor antagonist, presumably decreases the tear film thickness and causes decreased CCT measurements as systemic atropine does. Some studies reported no change in CCT following cycloplegia [15, 23, 27].
The sum of anterior aqueous depth and CCT is equal to ACD. Therefore, CCT and ACD are statistically dependent variables and the effect of CCT on ACD analysis should be considered.
One of the most interesting results in the present study was the elongation of AL after cycloplegia. In our study in the 50–60 and 10–20 age groups, AL showed a significant increase after cycloplegia (10 µm for both) but there was no change in the 30–40 age group. Similarly, Cheng and Hsieh [28] reported a significant increase in AL by 13 µm after application of 0.4% tropicamide. They hypothesize that a posterior shift of the lens-ciliary body diaphragm occurs after cycloplegia, and such a reaction may produce a compression force pushing toward the vitreous cavity, which may cause temporary elongation of the AL. These results appears to contradict the results from previous studies showing that AL may elongate during accommodation. Drexler et al. [29] reported increases in the AL of 12.7 and 5.2 µm during accommodation in emmetropic and myopic eyes, respectively. They proposed that the accommodatiaon-induced contraction of the ciliary muscle results decreasing the circumference of the sclera and leading to an elongation of the AL. Many previous studies reported that AL did not change significantly after cycloplegia [3, 8, 10, 14, 15, 17, 30, 31]. On the other hand, Gao et al. [32] observed AL decreased in myopic eyes after cycloplegia by atropine. They proposed that a backward movement of the apex of the flattened cornea happens during cycloplegia, which also results in an decrease in AL. However, they also reported that AL increased by 20 µm in hyperopic eyes after atropine use, and no clear explanation has been made for this result.
Can et al. [14] reported that cycloplegia did not affect IOL power calculations, with the exception of an increase of power >0.50 D in two cases using SRK/T formula with AL-Scan optical biometer in healthy volunteers with a mean age 33.12 ± 9.2 years. Huang et al. [17] reported that mean differences in IOL power as calculated by the Lenstar and the IOLMaster were between −0.08 and 0.0 D when obtained using the four different formulas (SRK/T, Holladay 1, Hoffer Q, and Haigis) with and without cycloplegia and were not significant (mean age 22.1 ± 4.7 years). In the present study, the mean differences in IOL power were between −0.08 and +0.02 D when obtained using SRK/T, Holladay 1, and Haigis formulas before and after cycloplegia. Our results are consistent with these of Huang et al. Statistically significant difference of about 0.1 D between before and after cycloplegia conditions could not cause clinical significance. A 0.1 D error in IOL power is equivalent to an error of about 0.067 D in refractive deviation in the spectacle plane [4]. Furthermore, Arriola-Villalobos et al. [15] reported IOL power was not change according to both SRK/T and Holladay 2 formulas after cycloplegia using Lenstar in patients with mean age of 74.71 ± 7.53 years. Özyol et al. [8] evaluated the effect of cyclopelgia in SRK/T, Holladay 2, and Haigis formulas with a mean age 30.1 ± 6.8 years, and reported only a significant decrease of 0.11 D only in Holladay 2 formula after cycloplegia.
Most IOL formulas only require AL and keratometry, such as SRK/T, Holladay, 1 and Hoffer Q. The Haigis formula uses AL, ACD, and keratometry [3]. In our study, with and without cycloplegia altered the measurement of IOL power by >0.50 D in 15 cases calculated by SRK/T, 21 cases by Holladay 1, and 30 cases by Haigis formula in all participants. The difference in ACD induced by cycloplegia in Haigis formula affect IOL power calculation. Therefore, we found the most variation in the Haigis formula.
Some studies have reported no significant change in mean keratometry following cycloplegia, while others showed a significant flattening effect [3, 15, 26, 28, 31]. This flattening was justified based on the paralysis of the ciliary muscle following cycloplegic agents which reduce its force on the sclera spur and lead to the corneal flattening [28]. In our study in the 50–60 age group, mean keraometry showed a significant decrease by 0.054 D and no significant change was in the 10–20 age group. Saitoh et al. [33] reported a 0.15 D decrease in keratometry after cycloplegia and Cheng et al. [28] reported a 0.032 D decrease. Unlike previous studies, we found a significant increase in mean keratometry by 0.055 D in the 30–40 age group. Although this difference was statistically significant, it was not clinically significant.
In the present study, the change in WtW was significant increased in the 30–40 and 10–20 age groups after cycloplegia but no significant difference was in the 50–60 age group. Similar to our results, Chang et al. [26], Arici et al. [10], and Arriola-Villalobos et al. [25] reported significant increasing of WtW after cycloplegia, although these changes appear to be unverifiable [3, 8, 30]. AL-Scan and many optical biometry devices use image analysis system for WtW measurement. The device digitally locates the limbus based on a sudden change in the contrast from paler sclera to darker cornea. Post dilation with iris bunching may make the difference between darker iris and paler sclera more obvious. In point of fact, the boundary between them is not very distinct and the contrast difference can vary depending on illumination and quality of the image. In such, a case could make WtW measurements after pupil dilation larger than those obtained previously [8, 34].
One limitation of this study was not evaluation according to the refractive error of the participants. Another, our study was limited to healthy participants and patients with cataracts could also be included in the study.
In conclusion, this study demonstrated that there was significant difference in many ocular parameters and IOL power formulas before and after cycloplegia. Especially, ACD showed significant changes in all age groups. Therefore, to avoid refractive prediction errors the IOL power calculation formulas using the ACD should be considered.
References
Behndig A, Montan P, Stenevi U, Kugelberg M, Lundström M. One million cataract surgeries: Swedish National Cataract Register 1992–2009. J Cataract Refract Surg. 2011;37:1539–45.
Lundström M, Pesudovs K. Questionnaires for measuring cataract surgery outcomes. J Cataract Refract Surg. 2011;37:945–59.
Ozcaliskan S, Yenerel NM. The effect of cycloplegia on biometric measurements using swept-source optical coherence tomography-based biometry. Clin Exp Optom. 2019;102:501–5.
Olsen T. Calculation of intraocular lens power: a review. Acta Ophthalmol Scand. 2007;85:472–85.
Santodomingo-Rubido J, Mallen EA, Gilmartin B, Wolffsohn JS. A new non-contact optical device for ocular biometry. Br J Ophthalmol. 2002;86:458–62.
Meyer F, Renard JP, Roux L, Rigal-Sastourne JC, Tuil A, Dot C. et al. Value of a new non-contact biometer for intraocular crystalline lens power calculation. J Fr Ophtalmol. 2001;24:1060–6.
Findl O, Kriechbaum K, Sacu S, Kiss B, Polak K, Nepp J, et al. Influence of operator experience on the performance of ultrasound biometry compared to optical biometry before cataract surgery. J Cataract Refract Surg. 2003;29:1950–5.
Özyol P, Özyol E, Baldemir E. Changes in ocular parameters and intraocular lens powers in aging cycloplegic eyes. Am J Ophthalmol. 2017;173:76–83.
Palamar M, Alkan Z, Egrilmez S, Yagci A. Influences of tropicamide on anterior segment parameters with Pentacam in healthy individuals. J Ocul Pharmacol Ther. 2013;29:349–52.
Arici C, Turk A, Ceylan OM, Kola M. The effect of topical 1% cyclopentolate on IOLMaster biometry. Optom Vis Sci. 2014;91:1343–7.
Palamar M, Egrilmez S, Uretmen O, Yagci A, Kose S. Influences of cyclopentolate hydrochloride on anterior segment parameters with Pentacam in children. Acta Ophthalmol. 2011;89:e461–465.
Mak H, Xu G, Leung CK. Imaging the iris with swept-source optical coherence tomography: relationship between iris volume and primary angle closure. Ophthalmology. 2013;120:2517–24.
Aptel F, Denis P. Optical coherence tomography quantitative analysis of iris volume changes after pharmacologic mydriasis. Ophthalmology. 2010;117:3–10.
Can E, Duran M, Çetinkaya T, Arıtürk N. The effect of pupil dilation on AL-Scan biometric parameters. Int Ophthalmol. 2016;36:179–83.
Arriola-Villalobos P, Díaz-Valle D, Garzòn N, Ruiz-Medrano J, Fernández-Perez C, Alejandre-Alba N, et al. Effect of pharmacologic pupil dilation on OLCR optical biometry measurements for IOL predictions. Eur J Ophthalmol. 2014;24:53–57.
Bakbak B, Koktekir BE, Gedik S, Guzel H. The effect of pupil dilation on biometric parameters of the Lenstar 900. Cornea. 2013;32:e21–24.
Huang J, McAlinden C, Su B, Pesudovs K, Feng Y, Hua Y, et al. The effect of cycloplegia on the lenstar and the IOLMaster biometry. Optom Vis Sci. 2012;89:1691–6.
McAlinden C, Gao R, Yu A, Wang X, Yang J, Yu Y, et al. Repeatability and agreement of ocular biometry measurements: Aladdin versus Lenstar. Br J Ophthalmol. 2017;101:1223–9.
Sheng H, Bottjer CA, Bullimore MA. Ocular component measurement using the Zeiss IOLMaster. Optom Vis Sci. 2004;81:27–34.
Norrby S. Sources of error in intraocular lens power calculation. J Cataract Refract Surg. 2008;34:368–76.
Yuan Y, Zhang Z, Zhu J, He X, Du E, Jiang K, et al. Responses of the ocular anterior segment and refraction to 0.5% tropicamide in chinese school-aged children of myopia, emmetropia, and hyperopia. J Ophthalmol. 2015;2015:612728.
Avdagic E, Lazzaro DR. Evaluation of the effect of cycloplegia on anterior chamber depth in cataract patients using optical low-coherence reflectometry. Eye Contact Lens. 2018;44(Suppl 1):59–61.
Higashiyama T, Iwasa M, Ohji M. Changes in the anterior segment after cycloplegia with a biometer using swept-source optical coherence tomography. PLoS ONE. 2017;14:e0183378. 12
Zeng Y, Gao JH. Effects of Mydrin eye-drops on central corneal thickness values in adult patients with myopia. Clin Exp Optom. 2017;100:151–4.
Arriola-Villalobos P, Almendral-Gómez J, Garzón N, Ruiz-Medrano J, Fernández-Pérez C, Martínez-de-la-Casa JM, et al. Effect of pharmacological pupil dilation on measurements and iol power calculation made using the new swept-source optical coherence tomography-based optical biometer. J Fr Ophtalmol. 2016;39:859–65.
Chang SW, Lo AY, Su PF. Anterior segment biometry changes with cycloplegia in myopic adults. Optom Vis Sci. 2016;93:12–18.
Arici C, Turk A, Ceylan OM, Kola M, Hurmeric V. Effects of 1% cyclopentolate hydrochloride on anterior segment parameters obtained with Pentacam in young adults. Arq Bras Oftalmol. 2014;77:228–32.
Cheng HC, Hsieh YT. Short-term refractive change and ocular parameter changes after cycloplegia. Optom Vis Sci. 2014;91:1113–7.
Drexler W, Findl O, Schmetterer L, Hitzenberger CK, Fercher AF. Eye elongation during accommodation in humans: differences between emmetropes and myopes. Investig Ophthalmol Vis Sci. 1998;39:2140–7.
Momeni-Moghaddam H, Maddah N, Wolffsohn JS, Etezad-Razavi M, Zarei-Ghanavati S, Akhavan Rezayat A, et al. The effect of cycloplegia on the ocular biometric and anterior segment parameters: a cross-sectional study. Ophthalmol Ther. 2019;8:387–95.
Adler G, Shahar J, Kesner R, Rosenfeld E, Fischer N, Loewenstein A, et al. Effect of pupil size on biometry measurements using the IOLMaster. Am J Ophthalmol. 2015;159:940–4.
Gao L, Zhuo X, Kwok AK, Yu N, Ma L, Wang J. The change in ocular refractive components after cycloplegia in children. Jpn J Ophthalmol. 2002;46:293–8.
Saitoh K, Yoshida K, Hamatsu Y, Tazawa Y. Changes in the shape of the anterior and posterior corneal surfaces caused by mydriasis and miosis: detailed analysis. J Cataract Refract Surg. 2004;30:1024–30.
Domínguez-Vicent A, Pérez-Vives C, Ferrer-Blasco T, Albarrán-Diego C, Montés-Micó R. Interchangeability among five devices that measure anterior eye distances. Clin Exp Optom. 2015;98:254–62.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tuncer, I., Zengin, M.Ö. & Yıldız, S. The effect of cycloplegia on the ocular biometry and intraocular lens power based on age. Eye 35, 676–681 (2021). https://doi.org/10.1038/s41433-020-01131-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01131-3
This article is cited by
-
Effects of atropine and tropicamide on ocular biological parameters in children: a prospective observational study
BMC Ophthalmology (2023)
-
Changes in ocular biological parameters after cycloplegia based on dioptre, age and sex
Scientific Reports (2022)