Abstract
Background
In observational and prospective cohort studies, intake of sugar-sweetened beverages (SSBs) and pure fruit juice (PFJ) has been associated with cardiovascular disease (CVD). Still, the causality of the connection has not yet been determined. Our objective was to uncover the relationship between SSBs/PFJ and CVD.
Methods
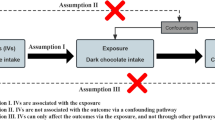
Genetically predicted causal associations between SSBs/PFJ (obtained in a published genome-wide association study) and six common CVDs (atrial fibrillation (AF), angina, heart failure (HF), acute myocardial infarction, hypertension, and coronary atherosclerosis) were assessed using MR analytic modeling. The primary analysis method utilized was the inverse variance weighted (IVW) method, complemented by additional methods such as the weighted median method, MR Egger regression, Cochran’s Q test, MR pleiotropy residual, funnel plot, Bonferroni correction, and others for MR analysis. To ensure the robustness of the findings, F-values were calculated as a complementary test to set looser thresholds for exposing genetic instrumental variables (P < 1e−5).
Results
The results of MR analysis suggested genetically causal associations between SSBs and AF (odds ratio (OR): 1.023; 95% confidence interval (CI) 1.007–1.038; P = 0.0039) as well as between PFJ and angina (OR: 0.968; 95% CI, 0.943–0.993; P = 0.0138) there was genetic causality. However, MR analysis showed no causal association between SSBs/PFJ and other CVD risks.
Conclusion
This study suggests that there may be a potential causal relationship between SSBs intake and AF and a causal negative association between PFJ intake and angina.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this published article and its additional files. All exposure data used in this study are included in the published article and its additional files, and all outcome data are available without restriction from the public database (https://gwas.mrcieu.ac.uk/).
References
Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990-2019: update from the GBD 2019 study. J Am Coll Cardiol. 2020;76:2982–3021.
Baman JR, Passman RS. Atrial fibrillation. J Am Med Assoc. 2021;325:2218.
Zhang J, Chen G, Wang C, Wang X, Qian ZM, Cai M, et al. Associations of risk factor burden and genetic predisposition with the 10-year risk of atrial fibrillation: observations from a large prospective study of 348,904 participants. BMC Med. 2023;21:88.
Brorsson B, Bernstein SJ, Brook RH, Werkö L. Quality of life of patients with chronic stable angina before and four years after coronary revascularisation compared with a normal population. Heart. 2002;87:140–5.
Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2020 update: a report from the American Heart Association. Circulation. 2020;141:e139–e596.
Welsh JA, Sharma AJ, Grellinger L, Vos MB. Consumption of added sugars is decreasing in the United States. Am J Clin Nutr. 2011;94:726–34.
Marriott BP, Hunt KJ, Malek AM, Newman JC. Trends in intake of energy and total sugar from sugar-sweetened beverages in the United States among children and adults, NHANES 2003-2016. Nutrients. 2019;11:https://doi.org/10.3390/nu11092004.
McGuire S. Scientific report of the 2015 Dietary Guidelines Advisory Committee. Washington, DC: US Departments of Agriculture and Health and Human Services, 2015. Adv Nutr. 2016;7:202–4.
Pacheco LS, Lacey JV Jr., Martinez ME, Lemus H, Araneta MRG, Sears DD, et al. Sugar-sweetened beverage intake and cardiovascular disease risk in the California Teachers Study. J Am Heart Assoc. 2020;9:e014883.
Ambrosini GL, Oddy WH, Huang RC, Mori TA, Beilin LJ, Jebb SA. Prospective associations between sugar-sweetened beverage intakes and cardiometabolic risk factors in adolescents. Am J Clin Nutr. 2013;98:327–34.
Wang D, Karvonen-Gutierrez CA, Jackson EA, Elliott MR, Appelhans BM, Barinas-Mitchell E, et al. Prospective associations between beverage intake during the midlife and subclinical carotid atherosclerosis: the Study of Women’s Health Across the Nation. PLoS One. 2019;14:e0219301.
Blumberg JB, Vita JA, Chen CY. Concord grape juice polyphenols and cardiovascular risk factors: dose-response relationships. Nutrients. 2015;7:10032–52.
Scheffers FR, Boer JMA, Gehring U, Koppelman GH, Vonk J, Smit HA, et al. The association of pure fruit juice, sugar-sweetened beverages and fruit consumption with asthma prevalence in adolescents growing up from 11 to 20 years: the PIAMA birth cohort study. Prev Med Rep. 2022;28:101877.
Herforth A, Arimond M, Álvarez-Sánchez C, Coates J, Christianson K, Muehlhoff E. A global review of food-based dietary guidelines. Adv Nutr. 2019;10:590–605.
O’Neil CE, Nicklas TA, Rampersaud GC, Fulgoni VL 3rd. 100% orange juice consumption is associated with better diet quality, improved nutrient adequacy, decreased risk for obesity, and improved biomarkers of health in adults: National Health and Nutrition Examination Survey, 2003-2006. Nutr J. 2012;11:107.
Fidler Mis N, Braegger C, Bronsky J, Campoy C, Domellöf M, Embleton ND, et al. Sugar in infants, children and adolescents: a position paper of the European Society for Paediatric Gastroenterology, Hepatology and Nutrition Committee on Nutrition. J Pediatr Gastroenterol Nutr. 2017;65:681–96.
Scheffers FR, Boer JMA, Verschuren WMM, Verheus M, van der Schouw YT, Sluijs I, et al. Pure fruit juice and fruit consumption and the risk of CVD: the European Prospective Investigation into Cancer and Nutrition-Netherlands (EPIC-NL) study. Br J Nutr. 2019;121:351–9.
Zhang Z, Zeng X, Li M, Zhang T, Li H, Yang H, et al. A prospective study of fruit juice consumption and the risk of overall and cardiovascular disease mortality. Nutrients. 2022;14:https://doi.org/10.3390/nu14102127.
Pan B, Ge L, Lai H, Wang Q, Wang Q, Zhang Q, et al. Association of soft drink and 100% fruit juice consumption with all-cause mortality, cardiovascular diseases mortality, and cancer mortality: a systematic review and dose-response meta-analysis of prospective cohort studies. Crit Rev Food Sci Nutr. 2022;62:8908–19.
Yarmolinsky J, Wade KH, Richmond RC, Langdon RJ, Bull CJ, Tilling KM, et al. Causal Inference in cancer epidemiology: what Is the role of Mendelian randomization? Cancer Epidemiol Biomark Prev. 2018;27:995–1010.
Sleiman PM, Grant SF. Mendelian randomization in the era of genomewide association studies. Clin Chem. 2010;56:723–8.
Lawlor DA, Harbord RM, Sterne JA, Timpson N, Davey Smith G. Mendelian randomization: using genes as instruments for making causal inferences in epidemiology. Stat Med. 2008;27:1133–63.
Skrivankova VW, Richmond RC, Woolf BAR, Davies NM, Swanson SA, VanderWeele TJ, et al. Strengthening the reporting of observational studies in epidemiology using mendelian randomisation (STROBE-MR): explanation and elaboration. Br Med J. 2021;375:n2233.
Cai D, Chen J, Wu Y, Jiang C. No causal association between tea consumption and 7 cardiovascular disorders: a two-sample Mendelian randomization study. Front Genet. 2022;13:989772.
Nordestgaard AT, Nordestgaard BG. Coffee intake, cardiovascular disease and all-cause mortality: observational and Mendelian randomization analyses in 95 000-223 000 individuals. Int J Epidemiol. 2016;45:1938–52.
Skrivankova VW, Richmond RC, Woolf BAR, Yarmolinsky J, Davies NM, Swanson SA, et al. Strengthening the reporting of observational studies in epidemiology using Mendelian randomization: the STROBE-MR statement. J Am Med Assoc. 2021;326:1614–21.
Zhong VW, Kuang A, Danning RD, Kraft P, van Dam RM, Chasman DI, et al. A genome-wide association study of bitter and sweet beverage consumption. Hum Mol Genet. 2019;28:2449–57.
Pierce BL, Burgess S. Efficient design for Mendelian randomization studies: subsample and 2-sample instrumental variable estimators. Am J Epidemiol. 2013;178:1177–84.
Zhu Y, Wang Y, Liu X, Wang Y, Cui Z, Liu F, et al. Genetically predicted osteoprotegerin levels and the risk of cardiovascular diseases: a Mendelian randomization study. Int J Cardiol. 2023;390:131233.
Wang S, Zhu H, Pan L, Zhang M, Wan X, Xu H, et al. Systemic inflammatory regulators and risk of acute-on-chronic liver failure: a bidirectional Mendelian-randomization study. Front Cell Dev Biol. 2023;11:1125233.
Yin Z, Chen J, Xia M, Zhang X, Li Y, Chen Z, et al. Assessing causal relationship between circulating cytokines and age-related neurodegenerative diseases: a bidirectional two-sample Mendelian randomization analysis. Sci Rep. 2023;13:12325.
Bulló M, Papandreou C, García-Gavilán J, Ruiz-Canela M, Li J, Guasch-Ferré M, et al. Tricarboxylic acid cycle related-metabolites and risk of atrial fibrillation and heart failure. Metabolism. 2021;125:154915.
Rejman K, Górska-Warsewicz H, Czeczotko M, Laskowski W. Nonalcoholic beverages as sources of nutrients in the average polish diet. Nutrients. 2020;12:https://doi.org/10.3390/nu12051262.
de Koning L, Malik VS, Kellogg MD, Rimm EB, Willett WC, Hu FB. Sweetened beverage consumption, incident coronary heart disease, and biomarkers of risk in men. Circulation. 2012;125:1735–1741, s1731.
Li X, Peng S, Wu X, Guan B, Tse G, Chen S, et al. C-reactive protein and atrial fibrillation: Insights from epidemiological and Mendelian randomization studies. Nutr Metab Cardiovasc Dis. 2022;32:1519–27.
Pol T, Hijazi Z, Lindbäck J, Oldgren J, Alexander JH, Connolly SJ, et al. Using multimarker screening to identify biomarkers associated with cardiovascular death in patients with atrial fibrillation. Cardiovasc Res. 2022;118:2112–23.
Vinson JA, Liang X, Proch J, Hontz BA, Dancel J, Sandone N. Polyphenol antioxidants in citrus juices: in vitro and in vivo studies relevant to heart disease. Adv Exp Med Biol. 2002;505:113–22.
Hyson DA. A review and critical analysis of the scientific literature related to 100% fruit juice and human health. Adv Nutr. 2015;6:37–51.
Kiss AK, Piwowarski JP. Ellagitannins, gallotannins and their metabolites—the contribution to the anti-inflammatory effect of food products and medicinal plants. Curr Med Chem. 2018;25:4946–67.
Ali M, Girgis S, Hassan A, Rudick S, Becker RC. Inflammation and coronary artery disease: from pathophysiology to Canakinumab Anti-Inflammatory Thrombosis Outcomes Study (CANTOS). Coron Artery Dis. 2018;29:429–37.
Vita JA. Polyphenols and cardiovascular disease: effects on endothelial and platelet function. Am J Clin Nutr. 2005;81:292s–297s.
Rossi I, Mignogna C, Del Rio D, Mena P. Health effects of 100% fruit and vegetable juices: evidence from human intervention studies. Nutr Res Rev. 2023;1–113. https://doi.org/10.1017/s095442242300015x.
Ford ES, Giles WH. Serum vitamins, carotenoids, and angina pectoris: findings from the National Health and Nutrition Examination Survey III. Ann Epidemiol 2000;10:106–16.
Acknowledgements
We sincerely thank all investigators for sharing the GWAS summary statistic data.
Funding
This research was funded by the Beijing University of Chinese Medicine New Teacher Initiation Fund Program (2023-JYB-XJSJJ003).
Author information
Authors and Affiliations
Contributions
HX and YL designed the study; HX and YL mined the data; YL researched the literature; HX analyzed the data; HX, YL, XG, SL, YF, WZ, and YZ wrote the paper. SY supervised and suggested revisions throughout. All authors read and approved the final paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study obtained all data from publicly available and accessible large-scale genome-wide association studies. All relevant studies used were approved by the appropriate ethical review boards. This study did not exceed the scope of the initial ethics committee approval.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xie, H., Liu, Y., Gu, X. et al. Association between sugar-sweetened beverages and pure fruit juice with risk of six cardiovascular diseases: a Mendelian randomization study. Eur J Clin Nutr (2024). https://doi.org/10.1038/s41430-024-01441-9
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41430-024-01441-9