Abstract
Background
Three indicators of early childhood undernutrition and associated factors are evaluated among under-5 children in five National Family Health Surveys in India spanning 1992 to 2021.
Methods
Data for 533,495 children under 5 years of age (U–5) were analysed in the context of three commonly used indicators of early childhood undernutrition – wasting, stunting and underweight. In addition to descriptive and inferential statistics, binary logistic regression was used to estimate the effects of specific explanatory factors on the three indicators using adjusted odds ratios.
Results
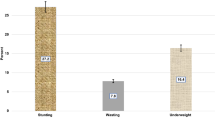
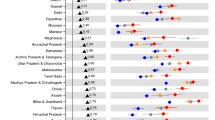
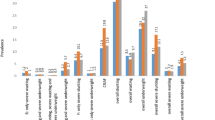
Over the three-decade interval, stunting was reduced by 22.1% in boys and 20.9% in girls, followed by underweight, 19.3% in boys and 17.4% in girls; wasting, in contrast, was reduced to a considerably lesser extent, 2.8% in boys and 0.9% in girls. Demographic, maternal and socioeconomic factors were associated with the incidence of early childhood undernutrition, specifically among young mothers and those with less education in low-income families, and among children from Scheduled Tribes or Scheduled Castes. Stunting and underweight declined significantly over the past three decades while wasting changed negligibly. The disparity in the occurrence of early childhood undernutrition was apparent throughout socioeconomic categories and regions of India.
Conclusions
The results highlight the need for special programs aimed at reducing waste among children and also the need for customized initiatives focused on the improvement of maternal education and wealth in addition to other ancillary factors related to regional variation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The NFHS datasets are available at https://dhsprogram.com/Data/.
References
UNICEF. UNICEF Data: Monitoring the situation of children and women: Malnutrition. UNICEF for every child 2021. Available from: https://data.unicef.org/topic/nutrition/malnutrition/.
UNICEF. Nutrition, for Every Child: UNICEF Nutrition Strategy 2020–2030. New York: UNICEF; 2020. https://www.unicef.org/reports/nutrition-strategy-2020-2030.
WHO. Nutrition. In: WHO, editor. 2018. Switzerland: World Health Organization; Available from: https://www.who.int/news-room/facts-in-pictures/detail/nutrition.
Jain I, Oberoi S, Jain A, Balgir RS, Sandhu MK, Lugani Y. Factors affecting the nutritional status of Anganwadi children: A cross-sectional study. J Fam Med Prim Care. 2020;9:4613–7. https://www.ncbi.nlm.nih.gov/pubmed/33209771.
Wells JC, Briend A, Boyd EM, Berkely JA, Hall A, Isanaka S, et al. Beyond wasted and stunted—a major shift to fight child undernutrition. Lancet Child Adolesc Health. 2019;3:831–4.
Griffiths P, Hindet A, Matthews Z. Infant and child mortality in three culturally contrasting states of India. J Biosoc Sci. 2001;33:603–22. https://www.ncbi.nlm.nih.gov/pubmed/11683227.
Chehab RF, Cross TL, Forman MR. The gut microbiota: a promising target in the relation between complementary feeding and child undernutrition. Adv Nutr. 2021;12:969–79. https://www.ncbi.nlm.nih.gov/pubmed/33216115.
Thurstans S, Sessions N, Dolan C, Sadler K, Cichon B, Isanaka S, et al. The relationship between wasting and stunting in young children: A systematic review. Matern Child Nutr. 2022;18:e13246. https://www.ncbi.nlm.nih.gov/pubmed/34486229.
Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, Evans DB, et al., editors. Disease Control Priorities in Developing Countries. 2006. 2nd ed. Washington (DC), New York.
UNICEF/WHO/WBG. Levels and trends in child malnutrition: key findings of the 2021 edition of the joint child malnutrition estimates. Geneva: World Health Organization; 2021. https://www.who.int/publications/i/item/9789240025257.
WHO. Underweight among children under 5 years of age (number in millions) (JME). 2022: World Health Organization; [cited 2022 20 Jul]. Available from: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/gho-jme-underweight-numbers-(in-millions).
IIPS, ICF. National Family Health Survey (NFHS-5): 2019-21 India. 2021. Mumbai: International Institute for Population Sciences (IIPS); Available from: https://dhsprogram.com/publications/publication-OF43-Other-Fact-Sheets.cfm.
WHO. Children: improving survival and well-being. 2020. World Health Organization. Available from: https://www.who.int/news-room/fact-sheets/detail/children-reducing-mortality.
von Grebmer K, Bernstein J, Resnick D, Wiemers M, Reiner L, Bachmeier M, et al. 2022 Global Hunger Index: Food Systems Transformation and Local Governance. Bonn and Dublin: Welthungerhilfe and Concern Worldwide; 2022. Available from: https://www.globalhungerindex.org/download/all.html.
Marotz LR. Health, Safety, and Nutrition for the Young Child. 8th ed. Belmont, USA: Wadsworth Cengage Learning; 2012.
Parízková J. Nutrition, Physical Activity, and Health in Early Life. 2nd ed. New York: CRC Press Taylor & Francis Group; 2010.
Arora C. Child Nutrition. Jaipur, India: ABD Publishers; 2009.
Blössner M, De Onis M, Prüss-Üstün A. Malnutrition: quantifying the health impact at national and local levels / Monika Blössner and Mercedes de Onis. Geneva: World Health Organization; 2005. https://apps.who.int/iris/handle/10665/43120.
Bharati S, Pal M, Bharati P. Determinants of nutritional status of pre-school children in India. J Biosoc Sci. 2008;40:801–14. https://www.ncbi.nlm.nih.gov/pubmed/18442431.
Kim J, Liu Y, Wang W, Blossom JC, Dwivedi LK, James KS, et al. Estimating the burden of child undernutrition for smaller electoral units in India. JAMA Netw Open. 2021;4:e2129416. https://www.ncbi.nlm.nih.gov/pubmed/34714345.
Rajia S, Sabiruzzaman M, Islam MK, Hossain MG, Lestrel PE. Trends and future of maternal and child health in Bangladesh. PLoS One. 2019;14:e0211875. https://www.ncbi.nlm.nih.gov/pubmed/30875380.
UN. The Sustainable Development Goals Report 2021. New York; 2021. Available from: https://unstats.un.org/sdgs/report/2021/.
Wachs TD. Multiple influences on children’s nutritional deficiencies: A systems perspective. Physiol Behav. 2008;94:48–60. https://www.ncbi.nlm.nih.gov/pubmed/18222500.
Elmighrabi NF, Fleming CAK, Dhami MV, Elmabsout AA, Agho KE. A systematic review and meta-analysis of the prevalence of childhood undernutrition in North Africa. PLoS One. 2023;18:e0283685. https://www.ncbi.nlm.nih.gov/pubmed/37023076.
Agabiirwe CN, Dambach P, Methula TC, Phalkey RK. Impact of floods on undernutrition among children under five years of age in low- and middle-income countries: a systematic review. Environ Health. 2022;21:98 https://www.ncbi.nlm.nih.gov/pubmed/36274126.
Buttner N, Heemann M, De Neve JW, Verguet S, Vollmer S, Harttgen K. Economic growth and childhood malnutrition in low- and middle-income countries. JAMA Netw Open. 2023;6:e2342654 https://www.ncbi.nlm.nih.gov/pubmed/37943556.
Ferdous F, Filteau S, Schwartz NB, Gumede-Moyo S, Cox SE. Association of postnatal severe acute malnutrition with pancreatic exocrine and endocrine function in children and adults: a systematic review. Br J Nutr. 2022;129:1–34. https://www.ncbi.nlm.nih.gov/pubmed/35504844.
NHM. Reproductive, Maternal, Newborn, Child and Adolescent Health (RMNCH+A): Ministry of Health & Family Welfare, Government of India; 2013 [Available from: https://nhm.gov.in/index1.php?lang=1&level=1&sublinkid=794&lid=168.
NHM. India Newborn Action Plan: Ministry of Health & Family Welfare. 2014, Government of India; [Available from: https://nhm.gov.in/index4.php?lang=1&level=0&linkid=153&lid=174.
NHM. Rashtriya Bal Swasthya Karyakram: Ministry of Health & Family Welfare. 2013, Government of India; [Available from: https://nhm.gov.in/index1.php?lang=1&level=4&sublinkid=1190&lid=583.
NHM. Janani Shishu Suraksha Karyakaram: Ministry of Health & Family Welfare. 2011, Government of India; [Available from: https://nhm.gov.in/index1.php?lang=1&level=3&sublinkid=842&lid=308.
Nguyen PH, Scott S, Headey D, Singh N, Tran LM, Menon P, et al. The double burden of malnutrition in India: Trends and inequalities (2006-2016). PLoS One. 2021;16:e0247856 https://www.ncbi.nlm.nih.gov/pubmed/33630964.
Soni A, Fahey N, Bhutta Z, Li W, Moore Simas T, Nimbalkar S, et al. Association of trends in child undernutrition and implementation of the National Rural Health Mission in India: A nationally representative serial cross-sectional study on data from 1992 to 2015. PLoS Med. 2022;19:e1003957 https://www.ncbi.nlm.nih.gov/pubmed/35395023.
Parameswaran N. Childhood undernutrition trends in India - What is our direction and speed? Indian J Pediatr. 2023;90:959–60. https://www.ncbi.nlm.nih.gov/pubmed/37592102.
WHO. WHO Child Growth Standards: Length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: Methods and development. Geneva: WHO Press; 2006. https://www.who.int/publications/i/item/924154693X.
Mahumud RA, Gow J, Sarker AR, Sultana M, Hossain G, Alam K. Distribution of wealth-stratified inequalities on maternal and child health parameters and influences of maternal-related factors on improvements in child health survival rate in Bangladesh. J Child Health Care. 2021;25:93–109. https://www.ncbi.nlm.nih.gov/pubmed/32207324.
Pravana NK, Piryani S, Chaurasiya SP, Kawan R, Thapa RK, Shrestha S. Determinants of severe acute malnutrition among children under 5 years of age in Nepal: a community-based case-control study. BMJ Open. 2017;7:e017084 https://www.ncbi.nlm.nih.gov/pubmed/28851796.
Sarker AR, Sultana M, Sheikh N, Akram R, Ali N, Mahumud RA, et al. Inequality of childhood undernutrition in Bangladesh: A decomposition approach. Int J Health Plann Manag. 2020;35:441–68. https://www.ncbi.nlm.nih.gov/pubmed/31702080.
Sheikh N, Akram R, Ali N, Haque SR, Tisha S, Mahumud RA, et al. Infant and young child feeding practice, dietary diversity, associated predictors, and child health outcomes in Bangladesh. J Child Health Care. 2020;24:260–73. https://www.ncbi.nlm.nih.gov/pubmed/31159554.
Sheikh N, Sultana M, Ali N, Akram R, Mahumud RA, Asaduzzaman M, et al. Coverage, timelines, and determinants of incomplete immunization in Bangladesh. Trop. Med. Infect. Dis. 2018; 3. https://doi.org/10.3390/tropicalmed3030072. Available from: https://www.ncbi.nlm.nih.gov/pubmed/30274468.
Sultana M, Sarker AR, Sheikh N, Akram R, Ali N, Mahumud RA, et al. Prevalence, determinants and health care-seeking behavior of childhood acute respiratory tract infections in Bangladesh. PLoS One. 2019;14:e0210433 https://www.ncbi.nlm.nih.gov/pubmed/30629689.
Subramanian SV, Nandy S, Irving M, Gordon D, Lambert H, Davey Smith G. The mortality divide in India: the differential contributions of gender, caste, and standard of living across the life course. Am J Public Health. 2006;96:818–25. https://www.ncbi.nlm.nih.gov/pubmed/16571702.
Vart P, Jaglan A, Shafique K. Caste-based social inequalities and childhood anemia in India: results from the National Family Health Survey (NFHS) 2005-2006. BMC Public Health. 2015;15:537 https://www.ncbi.nlm.nih.gov/pubmed/26044618.
Futschik A, Taus T, Zehetmayer S. An omnibus test for the global null hypothesis. Stat Methods Med Res. 2019;28:2292–304. https://www.ncbi.nlm.nih.gov/pubmed/29635962.
Ma Y, Hart JD, Janicki R, Carroll RJ. Local and omnibus goodness-of-fit tests in classical measurement error models. J R Stat Soc Ser B Stat Methodol. 2011;73:81–98. https://www.ncbi.nlm.nih.gov/pubmed/21339886.
Karlsson O, Kim R, Sarwal R, James KS, Subramanian SV. Trends in underweight, stunting, and wasting prevalence and inequality among children under three in Indian states, 1993–2016. Sci Rep. 2021;11:14137. https://doi.org/10.1038/s41598-021-93493-1.
WHO. Nutrition Landscape Information System (NLIS) country profile indicators: interpretation guide. Geneva: World Health Organization; 2010. https://apps.who.int/iris/handle/10665/44397.
WHO. Nutrition Landscape Information System (NLiS) country profile indicators: interpretation guide. 2nd ed. Geneva: World Health Organization; 2019. https://apps.who.int/iris/handle/10665/332223.
Li Z, Kim R, Vollmer S, Subramanian SV. Factors associated with child stunting, wasting, and underweight in 35 low- and middle-income countries. JAMA Netw Open. 2020;3:e203386 https://www.ncbi.nlm.nih.gov/pubmed/32320037.
Amadu I, Seidu AA, Duku E, Boadu Frimpong J, Hagan Jnr JE, Aboagye RG, et al. Risk factors associated with the coexistence of stunting, underweight, and wasting in children under 5 from 31 sub-Saharan African countries. BMJ Open. 2021;11:e052267 https://www.ncbi.nlm.nih.gov/pubmed/34930735.
Danso F, Appiah MA. Prevalence and associated factors influencing stunting and wasting among children of ages 1 to 5 years in Nkwanta South Municipality, Ghana. Nutrition. 2023;110:111996 https://www.ncbi.nlm.nih.gov/pubmed/37003173.
Tiwari I, Acharya K, Paudel YR, Sapkota BP, Kafle RB. Planning of births and childhood undernutrition in Nepal: evidence from a 2016 national survey. BMC Public Health. 2020;20:1788 https://www.ncbi.nlm.nih.gov/pubmed/33238952.
Akombi BJ, Agho KE, Hall JJ, Wali N, Renzaho AMN, Merom D Stunting, Wasting and underweight in Sub-Saharan Africa: A systematic review. Int J Environ Res Public Health. 2017; 14. https://doi.org/10.3390/ijerph14080863. Available from: https://www.ncbi.nlm.nih.gov/pubmed/28788108.
Khan S, Zaheer S, Safdar NF. Determinants of stunting, underweight and wasting among children < 5 years of age: Evidence from 2012–2013 Pakistan demographic and health survey. BMC Public Health. 2019;19:358 https://www.ncbi.nlm.nih.gov/pubmed/30935382.
Sahiledengle B, Mwanri L, Petrucka P, Kumie A, Beressa G, Atlaw D, et al. Determinants of undernutrition among young children in Ethiopia. Sci Rep. 2022;12:20945 https://www.ncbi.nlm.nih.gov/pubmed/36470914.
Beal T, Tumilowicz A, Sutrisna A, Izwardy D, Neufeld LM. A review of child stunting determinants in Indonesia. Matern Child Nutr. 2018;14:e12617 https://www.ncbi.nlm.nih.gov/pubmed/29770565.
Nwosu CO, Ataguba JE. Explaining changes in wealth inequalities in child health: The case of stunting and wasting in Nigeria. PLoS One. 2020;15:e0238191 https://www.ncbi.nlm.nih.gov/pubmed/32925960.
Odei Obeng-Amoako GA, Karamagi CAS, Nangendo J, Okiring J, Kiirya Y, Aryeetey R, et al. Factors associated with concurrent wasting and stunting among children 6–59 months in Karamoja, Uganda. Matern Child Nutr. 2021;17:e13074 https://www.ncbi.nlm.nih.gov/pubmed/32830434.
Chatterjee K, Sinha RK, Kundu AK, Shankar D, Gope R, Nair N, et al. Social determinants of inequities in under-nutrition (weight-for-age) among under-5 children: a cross sectional study in Gumla district of Jharkhand, India. Int J Equity Health. 2016;15:104 https://www.ncbi.nlm.nih.gov/pubmed/27391031.
Ghosh S, Varerkar SA. Undernutrition among tribal children in Palghar district, Maharashtra, India. PLoS One. 2019;14:e0212560 https://www.ncbi.nlm.nih.gov/pubmed/30811462.
Chowdhury MRK, Khan HTA, Mondal MNI, Kabir R. Socio-demographic risk factors for severe malnutrition in children aged under five among various birth cohorts in Bangladesh. J Biosoc Sci. 2021;53:590–605. https://www.ncbi.nlm.nih.gov/pubmed/32787991.
Mkhize M, Sibanda M. A review of selected studies on the factors associated with the nutrition status of children under the age of five years in South Africa. Int J Environ Res Public Health. 2020;17. https://doi.org/10.3390/ijerph17217973.
Liczbinska G, Gautam RK, Bharati P, Malina RM. Body size and weight status of adult Indian males born in the 1890s through 1950s: Age and secular change in the context of demographic, economic and political transformation. Am J Hum Biol. 2023;35:e23939. https://doi.org/10.1002/ajhb.23939.
Liczbinska G, Gautam RK, Bharati P, Malina RM. Regional variation in body size and estimated secular change among adult Indian males born in the 1890s-1950s. Anthropol Anz. 2024;81:219–32. https://doi.org/10.1127/anthranz/2023/1741.
Liczbinska G, Gautam RK, Bharati P, Malina RM. Variation in body size and weight status among Hindu and Muslim Indian males born in the 1890s through the 1950s. Sci Rep. 2024;14:4189. https://doi.org/10.1038/s41598-024-54637-1.
Acknowledgements
The authors would like to thank the Demographic and Health Surveys (DHS) for providing data. This study had no grant, technical or corporate support.
Author information
Authors and Affiliations
Contributions
PB conceived the presented idea. RNK, PB designed methodology. RNK was involved in data curation and performed the analysis. RNK, PB, and RKG were involved in data interpretation. RNK and AC drafted the manuscript. RKG and PB verified the analytical methods. GL and RMM contributed to the interpretation of the statistical analysis. PB, RKG, GL, and RMM critically reviewed and edited the manuscript. RNK, RKG, GL, and RMM finalized the manuscript. PB supervised the study. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The Demographic and Health Surveys (DHS) provided data for this study, which are available in the public domain. The DHS survey methodology and participant confidentiality were evaluated and approved by the ICF Institutional Review Board (IRB). Regarding the confidentiality of participants and the protection of human subjects, the ICF IRB abides by the standards set forth by the US Department of Health and Human Services. The DHS also obtained consent from the guardian of each participant. The use of the DHS data did not require additional ethical approval because it was already ethically approved.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kundu, R.N., Gautam, R.K., Chatterjee, A. et al. Nutritional status of infants and young children in India across three decades: Analysis of five national family health surveys. Eur J Clin Nutr (2024). https://doi.org/10.1038/s41430-024-01427-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41430-024-01427-7