Abstract
Background
Public support for evidence-based nutrition interventions can be an important determinant of government willingness to develop and implement such interventions. The aim of this study was to assess support for a broad range of nutrition interventions across seven countries: Australia, Canada, China, India, New Zealand, the United Kingdom, and the United States. Assessed interventions included those relating to food availability, affordability, reformulation, labelling, and promotion.
Methods
Approximately 1000 adults per country (total n = 7559) completed an online survey assessing support for 35 nutrition interventions/policies. ANOVA analyses were used to identify differences between countries on overall levels of support and by intervention category. Multiple regression analyses assessed demographic and diet-related factors associated with higher levels of support across the total sample and by country.
Results
Substantial levels of public support were found for the assessed interventions across the seven countries and five intervention categories. The highest levels were found in India (Mean across all interventions of 4.16 (standard deviation (SD) 0.65) on a 5-point scale) and the lowest in the United States (Mean = 3.48, SD = 0.83). Support was strongest for interventions involving food labelling (Mean = 4.20, SD = 0.79) and food reformulation (Mean = 4.17, SD = 0.87), and weakest for fiscal interventions (Mean = 3.52, SD = 1.06). Consumer characteristics associated with stronger support were higher self-rated health, higher educational attainment, female sex, older age, and perceptions of consuming a healthy diet.
Conclusion
The results indicate substantial support for a large range of nutrition interventions across the assessed countries, and hence governments could potentially be more proactive in developing and implementing such initiatives.
Similar content being viewed by others
Introduction
A large and growing body of evidence provides support for a wide range of nutrition policies to assist in addressing burgeoning rates of obesity and other diet-related diseases globally [1,2,3]. Such policies include those relating to food availability, affordability, reformulation, labelling, and advertising [3,4,5,6,7,8,9]. Many of these policies involve enhancing the healthiness of the broader food environment rather than primarily focusing on encouraging individuals to change their behaviours within obesogenic environments that do not support healthy dietary choices [10]. This upstream approach is strongly endorsed by the world’s leading health agencies [9, 11].
The state of the evidence and the scale of diet-related health problems raises the question of why the policy approaches recommended by national and international health agencies are not being uniformly implemented by governments [12, 13]. Political appetite to implement effective food policy is understood to be a key determinant of whether recommended policies are introduced [14]. In turn, governments’ willingness to introduce such policies is reliant on numerous factors, one of which can be the extent to which the general public supports implementation [15]. As well as motivating governments via constituent sentiment, public support can (i) assist governments to resist industry opposition to policies that enhance public health but constrain market freedoms, (ii) enhance community compliance post-implementation, and (iii) inform decisions about the order in which specific interventions will be introduced and assist in the development of communications designed to address concerns among less supportive population segments [16,17,18].
To date, most research investigating public support for nutrition policies has focused on individual, high-income countries and examined a limited number of policies. Few studies have included low- and middle-income countries, and very little prior research has attempted to compare public support for the same policies cross-nationally [19,20,21,22]. Work to date suggests that levels of support can be dependent on policy characteristics, especially the level of perceived intrusiveness and consumer characteristics such as age and sex. Policies that involve greater restrictions have been found to be less popular than those that focus on information provision [20, 23], and females and older people are likely to be more supportive of nutrition policies than males and younger people [12, 15, 24]. Little is known about the extent to which these findings may be relevant to a broader range of potential nutrition policies and more diverse cultural contexts.
The aim of the present study was to extend current evidence relating to public support for nutrition policies by assessing support outcomes for a large range of interventions across a diverse range of countries. The included interventions represented five food policy categories that have been identified as being critical for achieving healthy diets at the population level [9, 25, 26]: availability, affordability, labelling, promotion, and reformulation. The included countries were Australia, Canada, China, India, New Zealand (NZ), the United Kingdom (UK), and the United States (US). Some of these countries have received very little research attention in the policy support literature to date (e.g., China, India, NZ), while others have been the subject of previous research and thus provide a comparison point for the results of this study [12, 20, 23, 24, 27].
Methods
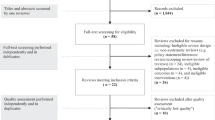
An ISO-accredited web panel provider (Pureprofile) was commissioned to recruit a minimum of 1,000 adults from each of the seven countries. This sample size was selected to enable within and between country analyses. As shown in Table 1, these countries exhibit variation across Hofstede’s cultural dimensions of individualism (the extent to which people prioritise themselves and their immediate families over the wider community), power distance (the extent to which there is unequal power distribution among members of society), and indulgence (the prioritisation of gratification over restraint) [28]. Each of these dimensions is likely to have implications for societal-level support for nutrition interventions that influence the food environment and affect people’s diets.
Quotas were applied to achieve samples within each country characterised by an approximately even number of males and females, an approximately even distribution across three age categories (18–34, 35–54, 55+ years), and at least two-thirds of the sample being in low and middle-income tertiles according to income distributions in each country. The latter requirement was designed to ensure appropriate representation of those on lower incomes who are often under-represented in survey research [29]. These quotas were met in most instances, notable exceptions being age distribution in India and income distribution in China. Likely reflecting the younger average age in India, only one in five respondents was in the 55+ years category. There were fewer low-income respondents from China compared to the other countries, compensated to some degree by a large proportion of middle-income participants. The sample profile (Table S1) and response rate data (Table S2) are provided in the supplementary materials. The study was approved by Curtin University Human Research Ethics Committee and respondents provided informed consent.
Respondents completed an online survey that included items on demographic characteristics, nutrition-related attitudes and behaviours, and extent of support for 35 nutrition interventions across the five topic areas of availability (n = 14 interventions), fiscal (n = 3), labelling (n = 5), promotion (n = 10), and reformulation (n = 3). The list of interventions was derived from recommendations commonly identified in key international papers and authoritative reports on policies for improving population diets (e.g., the NOURISHING database [11], the Lancet Commission on Obesity report [30], and the INFORMAS Food-EPI tool [31]). To optimise comparability across the proposed interventions, where possible the descriptions were kept neutral without specifying who would be responsible for implementation (e.g., government, food companies, other institutions) or how it would be implemented (e.g., through mandatory regulation, co-regulation, voluntary guidelines, local-level policy). Respondents indicated their support by selecting their level of agreement on a 5-point agreement scale (1 ‘Strongly disagree’ to 5 ‘Strongly agree’) for each intervention statement (see supplementary materials for item wording). Reflecting the differing policy environments in each country, the interventions were phrased in a manner for the agreement question to be relevant regardless of whether the intervention had already been implemented (e.g., ‘There should be regular public education campaigns about the importance of healthy eating’, ‘Supermarkets should be encouraged to promote healthy foods more heavily than unhealthy foods’). The survey instruments were presented in Mandarin and Hindi for respondents in China and India respectively, with English versions also made available for these respondents.
Data analyses
Analyses were undertaken using SPSS 27 [32]. Descriptive analyses were performed to assess the level of support for each intervention and by intervention category within each country and overall. ANOVA analyses were used to determine whether the countries differed in terms of overall support for the interventions and each intervention category. Eight multivariate regression analyses were conducted to identify individual-level variables associated with support across the 35 assessed interventions for each country separately and all countries combined. The following independent variables were included in the regression analyses: age (continuous), sex (1 = male, 2 = female), household income (continuous), education (continuous), perceived diet healthiness (1 “I eat a very unhealthy diet” to 4 “I eat a very healthy diet”), self-rated health (1 “Poor” to 5 “Excellent”), and BMI (assessed from self-reported height and weight; continuous). Given the number of analyses conducted, a significance level of p < 0.001 was applied (two-tailed), and all test assumptions were met.
Results
Overall, substantial levels of support were found across the seven countries and five intervention categories. The mean scores shown in Table 2 were all above the neutral scale midpoint of ‘3’, ranging from 3.04 (SD = 1.17) for fiscal interventions among US respondents to 4.27 (SD = 0.76) for labelling interventions among UK respondents. Of note was that the US respondents provided the lowest average scores for four of the five intervention categories and respondents from India the highest average scores for three. This was reflected in the US having the lowest ‘All initiatives’ composite mean (Mean = 3.48, SD = 0.83) and India the highest (Mean = 4.16, SD = 0.65).
On average, the labelling intervention category had the highest mean score (Mean = 4.20, SD = 0.79), followed by the reformulation category (Mean = 4.17, SD = 0.87) (Table 2). The promotion (Mean = 3.83, SD = 0.86) and availability (Mean = 3.71, SD = 0.88) intervention categories were mid-range. The lowest scoring category was fiscal interventions, although the mean of 3.52 (SD = 1.06) was still above the neutral midpoint. As shown in Table 3, this lower overall support for fiscal interventions disguises a substantial difference between support in most countries for taxing unhealthy foods (Mean = 3.18, SD = 1.36) and beverages (Mean = 3.28, SD = 1.38) versus support for the subsidisation of fruit and vegetables (Mean = 4.09, SD = 1.12).
At the individual intervention level, 13 of the 35 interventions were actively supported (i.e., by selecting ‘Agree’ or ‘Strongly agree’ on the 5-point agreement scale) by 75% or more respondents across the total sample (Tables 3–5). Three interventions received 75 + % support in the seven countries individually as well as overall, each of which related to specific nutrients: ‘The amount of added sugar in a packaged food should be reported on the label’, ‘The amount of trans fat in a packaged food should be reported on the label’, and ‘Manufacturers should reduce the amount of saturated fat in their products’. The highest levels of support for specific interventions within individual countries were found for ‘There should be regular public education campaigns about the importance of healthy eating’ (87% India, 86% China) and ‘Hospitals should provide only healthy foods to patients’ (87% India).
For most countries, there were few instances of only a minority of respondents expressing support for individual interventions. The notable exception was the US, where <50% of respondents supported 18 of the 35 assessed interventions. Individual interventions receiving the lowest levels of support were those relating to taxing unhealthy foods and beverages and restricting the products available in vending machines in locations such as workplaces, universities, and sporting venues (vending machines in hospitals and schools received majority support overall, albeit not among some individual countries).
The vending machine interventions were also the most polarising across countries. For example, ‘Vending machines containing unhealthy foods should not be allowed in sporting venues’ received support from 28% of respondents in the US versus 77% in India. The interventions with the most similar responses across countries were those relating to the reporting of saturated fat (Australia and India 77% vs Canada 83%) and trans fat (NZ and the US 75% vs 81% UK) on product labels.
The regression analyses results are presented in Table 6. Across the total sample, while most of the assessed variables were significantly associated with overall support, the largest effect sizes were found for higher self-rated health (β = 0.17) and educational attainment (β = 0.12). There were some notable country-specific differences. For example, female sex was a significant predictor of overall support in only Australia (β = 0.16), Canada (β = 0.11), and NZ (β = 0.14), and education was only significant for Australia (β = 0.11), China (β = 0.20), and India (β = 0.12). Perceived diet healthiness was related to policy support in all countries except China and India. BMI was not associated with level of support in any of the individual countries.
Discussion
This study across a diverse range of countries found majority support for most of the nutrition interventions examined. Consistent with the cultural dimensions outlined in Table 1, support was strongest in India and China and weakest in the US. India and China score high on power distance (indicating acceptance of authority), low on indulgence (suggesting a willingness to forego personal gratification), and low individualism (prioritising the well-being of the broader community). By comparison, the US is at the opposite end of the spectrum on these dimensions, which is reflected in the results of this and previous research examining public support for health-related interventions [17, 20, 22]. Cultural dimensions therefore appear to be a useful lens through which to assess uptake of nutrition policies [19]. However, it is noteworthy that Australia and the UK, for example, are high on individualism and indulgence, and NZ is especially low on power distance, yet respondents in these countries demonstrated markedly higher support for many of the interventions compared to the US. These findings may reflect the current food policy environments within these countries and the extent to which the populations are already accustomed (or not) to more interventionist nutrition policy (for country-specific information on current food policy contexts see the NOURISHING Framework [11]).
Similar to previous research, the interventions receiving the highest levels of support were those relating to labelling and reformulation [19, 21, 23, 33]. These approaches to improving the quality of the food supply involve the provision of information and modification of product content by manufacturers, and therefore are relatively low in terms of intrusiveness on consumers. By comparison, the interventions with the lowest levels of support were those pertaining to taxes on unhealthy foods and beverages (fiscal) and the contents of vending machines (availability), both of which have more direct impacts on consumers. The results relating to promotion interventions were generally mid-range, with those requiring the promotion of healthier options rated higher than those restricting the promotion of unhealthy options. These outcomes are consistent with previous work finding level of policy intrusiveness to be inversely related to level of support [19, 20, 34], highlighting the need to increase the public’s understanding of the importance and effectiveness of more intrusive interventions.
The lack of popularity of taxes has been noted elsewhere [12, 21, 24, 33], and policy makers face clear challenges in presenting this form of intervention to the general public in a manner that fosters greater acceptance. Taxes are also strongly opposed by the food industry [35], making it even more important to gain public approval to assist in overcoming the influence of industry lobbyists. Previous research has identified explicit hypothecation of food tax revenue to address health-related issues as a possible means of overcoming resistance among substantial sections of the population [24, 27]. This was not tested in the present study and constitutes an important focus for future research given the substantial and growing evidence that fiscal interventions have a key role to play in effective food policy [3,4,5, 9].
The finding of lower support for restrictions on vending machines is also worthy of further investigation. There is a noted lack of evidence relating to the way in which consumers across different countries respond to the idea of healthy vending machines [33]. Many people may rely on these food sources in locations (e.g., workplaces and education institutions) and at times (e.g., after hours) when other options are not readily available [36, 37]. In such situations, restricting the contents of vending machines may be construed as effectively eradicating choice, and more work may be needed across countries to increase consumer receptivity to such interventions.
Consistent with previous research, demographic factors such as being female, older, and more educated were significantly associated with higher intervention support levels across the total sample [12, 15, 24]. However, as per the limited prior work comparing predictors of support internationally [20, 22], these associations differed somewhat between countries. For example, older respondents were found to be more supportive of the assessed interventions in all countries except China and the US; females were more likely to express support in Australia, Canada, and NZ, but not the other four countries; and education level was only significant as a predictor of support in Australia, China, and India. It is therefore important to understand the role of demographic predictors in individual countries when assessing policy support.
The high levels of support found for most interventions in most countries indicates governments have high levels of support from their populations to take a more proactive stance in nutrition policy development and implementation. This in turn raises the issue of why evidence-based interventions with strong community support are not already in place. A well-recognised contributor to this situation is vigorous resistance from the food industry [13, 35, 38, 39], highlighting the importance of countries applying appropriate strategies and protocols to minimise industry interference in policy making. A further consideration is the logistical complexity associated with introducing and monitoring policies that require actions across sectors, such as those involving taxation, institutional food provisioning, and communications regulation [40]. Even just within the public sector, working towards integrated food policy will require coordination between government departments, including those that are unaccustomed to prioritising health, hence requiring strong political commitment [14].
The primary strength of this study was the involvement of sizeable samples recruited from seven countries, including those with varying cultural profiles and different levels of economic development. Such cross-cultural analyses enable observation of similarities and differences that can provide insights into potential leverage points for ongoing improvements in countries’ nutrition policies. The results can constitute groundwork for examining changes over time in response to differing patterns of intervention implementation.
An important limitation was use of a web panel provider for data collection and the resulting non-probability sample that is likely to have differed on some characteristics compared to the populations from which it was drawn. This is especially notable for China and India, where web panel use would have excluded involvement of those with lower literacy levels. Future research could use alternative participant recruitment methods to access a broader range of respondents. In addition, due to the number of interventions and countries included in the study, no attempt was made to account for the policy environments in each country and the associated differing levels of familiarity with the assessed interventions. This is an important area of future research as it would enable identification of how support changes at different stages of policy implementation. Another useful approach would be experiments to explore effective methods of communicating with the public about the benefits of nutrition policies to increase support, especially among less receptive population subgroups [15]. Finally, future work comparing policy support across countries would ideally include a larger number of low- and middle-income countries to provide greater insights into these important food policy contexts.
In conclusion, the results of this study indicate that populations across various countries are supportive of a large range of nutrition policies, and hence that governments can potentially be more proactive in this space. However, focused efforts are needed to increase support for some evidence-based policies, especially those relating to the application of taxes to unhealthy food products.
Data availability
The data are available from the first author upon reasonable request for non-commercial use.
References
Breda J, Castro LSN, Whiting S, Williams J, Jewell J, Engesveen K, et al. Towards better nutrition in Europe: Evaluating progress and defining future directions. Food Policy. 2020;96:101887.
Drewnowski A, Monterrosa EC, de Pee S, Frongillo EA, Vandevijvere S. Shaping physical, economic, and policy components of the food environment to create sustainable healthy diets. Food Nutr Bull 2020;41(2_suppl):74S–86S.
Lobstein T, Neveux M, Landon J. Costs, equity and acceptability of three policies to prevent obesity: A narrative review to support policy development. Obes Sci Pr. 2020;6:562–83.
Blakely T, Cleghorn C, Mizdrak A, Waterlander W, Nghiem N, Swinburn B, et al. The effect of food taxes and subsidies on population health and health costs: a modelling study. Lancet Public Health. 2020;5:e404–13.
Broeks MJ, Biesbroek S, Over EAB, van Gils PF, Toxopeus I, Beukers MH, et al. A social cost-benefit analysis of meat taxation and a fruit and vegetables subsidy for a healthy and sustainable food consumption in the Netherlands. BMC Public Health. 2020;20:643.
Gressier M, Sassi F, Frost G, Healthy. Foods and healthy diets. how government policies can steer food reformulation. Nutrients 2020;12:1992.
Hansen KL, Golubovic S, Eriksen CU, Jørgensen T, Toft U. Effectiveness of food environment policies in improving population diets: a review of systematic reviews. Eur J Clin Nutr. 2021;76:637–646.
Mytton OT, Boyland E, Adams J, Collins B, O’Connell M, Russell SJ, et al. The potential health impact of restricting less-healthy food and beverage advertising on UK television between 05.30 and 21.00h: A modelling study. PLOS Med. 2020;17:e1003212.
World Health Organization. Tackling NCDs: ‘Best buys’ and other recommended interventions for the prevention and control of noncommunicable diseases. World Health Organization; 2017.
Roberto CA. How psychological insights can inform food policies to address unhealthy eating habits. Am Psychol. 2020;75:265–73.
World Cancer Research Fund International. NOURISHING framework. 2022. Available from: https://www.wcrf.org/policy/policy-databases/nourishing-framework.
Watson WL, Sarich P, Hughes C, Dessaix A. Monitoring changes in community support for policies on obesity prevention. Aust N. Z J Public Health. 2021;45:482–90.
Zorbas C, Grigsby-Duffy L, Backholer K. Getting the price right: how nutrition and obesity prevention strategies address food and beverage pricing within high-income countries. Curr Nutr Rep. 2020;9:42–53.
Candel JJL, Pereira L. Towards integrated food policy: Main challenges and steps ahead. Environ Sci Policy. 2017;73:89–92.
Diepeveen S, Ling T, Suhrcke M, Roland M, Marteau TM. Public acceptability of government intervention to change health-related behaviours: a systematic review and narrative synthesis. BMC Public Health. 2013;13:756.
Giesbrecht N, Livingston M. Public perceptions and alcohol policies: Six case studies that examine trends and interactions. Drug Alcohol Rev. 2014;33:217–9.
Dekker MR, Jones A, Maulik PK, Pettigrew S. Public support for alcohol control initiatives across seven countries. Int J Drug Policy. 2020;82:102807.
UK Health Forum. Public health and the food and drinks industry: The governance and ethics of interaction. Lessons from research, policy and practice. London: UKHF; 2018. Available from: https://www.idrc.ca/sites/default/files/sp/Documents%20EN/ukhf-casebook-jan18.pdf.
Branson C, Duffy B, Perry C, Wellings D. Acceptable Behaviour? Public opinion on behaviour change policy. IPSOS MORI, London; 2012.
Kwon J, Cameron AJ, Hammond D, White CM, Vanderlee L, Bhawra J, et al. A multi-country survey of public support for food policies to promote healthy diets: Findings from the International Food Policy Study. BMC Public Health. 2019;19:1205.
Mazzocchi M, Cagnone S, Bech-Larsen T, Niedzwiedzka B, Saba A, Shankar B, et al. What Is the public appetite for health eating policies: evidence from a Cross-European Survey. Health Econ Policy Law. 2015;10:267–92.
Gómez-Donoso C, Sacks G, Vanderlee L, Hammond D, White CM, Nieto C, et al. Public support for healthy supermarket initiatives focused on product placement: a multi-country cross-sectional analysis of the 2018 International Food Policy Study. Int J Behav Nutr Phys Act. 2021;18:78.
Bhawra J, Reid JL, White CM, Vanderlee L, Raine K, Hammond D. Are young Canadians supportive of proposed nutrition policies and regulations? An overview of policy support and the impact of socio-demographic factors on public opinion. Can J Public Health Rev Can Sté Publique. 2018;109:498–505.
Eykelenboom M, van Stralen MM, Olthof MR, Renders CM, Steenhuis IH. Public acceptability of a sugar-sweetened beverage tax and its associated factors in the Netherlands. Public Health Nutr. 2021;24:2354–64.
Adams J, Hofman K, Moubarac JC, Thow AM. Public health response to ultra-processed food and drinks. BMJ. 2020;369:m2391.
Moodie R, Stuckler D, Monteiro C, Sheron N, Neal B, Thamarangsi T, et al. Profits and pandemics: prevention of harmful effects of tobacco, alcohol, and ultra-processed food and drink industries. Lancet Lond Engl. 2013;381:670–9.
Miller CL, Dono J, Wakefield MA, Pettigrew S, Coveney J, Roder D, et al. Are Australians ready for warning labels, marketing bans and sugary drink taxes? Two cross-sectional surveys measuring support for policy responses to sugar-sweetened beverages. BMJ Open. 2019;9:e027962.
Hofstede Insights [Internet]. 2022. Available from: https://www.hofstede-insights.com/country-comparison.
Mapes BM, Foster CS, Kusnoor SV, Epelbaum MI, AuYoung M, Jenkins G, et al. Diversity and inclusion for the All of Us research program: A scoping review. PLoS ONE. 2020;15:e0234962.
Swinburn BA, Kraak VI, Allender S, Atkins VJ, Baker PI, Bogard JR, et al. The global syndemic of obesity, undernutrition, and climate change: The Lancet Commission report. Lancet Lond Engl. 2019;393:791–846.
Vandevijvere S, Barquera S, Caceres G, Corvalan C, Karupaiah T, Kroker-Lobos MF, et al. An 11-country study to benchmark the implementation of recommended nutrition policies by national governments using the Healthy Food Environment Policy Index, 2015-2018. Obes Rev. 2019;20(S2):57–66.
IBM Corp. IBM SPSS Statistics for Windows, Version 27.0. Armonk, NY: IBM Corp. 2020.
Hagmann D, Siegrist M, Hartmann C. Taxes, labels, or nudges? Public acceptance of various interventions designed to reduce sugar intake. Food Policy. 2018;79:156–65.
Nuffield Council on Bioethics. Public Health: Ethical Issues. London; 2007.
Temple NJ. A comparison of strategies to improve population diets: government policy versus education and advice. J Nutr Metab. 2020;2020:1–6.
Onufrak SJ, Zaganjor H, Moore LV, Hamner HC, Kimmons JE, Maynard LM, et al. Foods consumed by US adults from cafeterias and vending machines: NHANES 2005 to 2014. Am J Health Promot 2019;33:666–74.
Utter J, McCray S. Vending machines in Australian hospitals: are they meeting the needs of the consumer? J Nutr Educ Behav. 2021;53:183–6.
Lauber K, Hunt D, Gilmore AB, Rutter H. Corporate political activity in the context of unhealthy food advertising restrictions across Transport for London: A qualitative case study. PLOS Med. 2021;18:e1003695.
Nestle M. A food lover’s love of nutrition science, policy, and politics. Eur J Clin Nutr. 2019;73:1551–5.
Clarke B, Kwon J, Swinburn B, Sacks G. Understanding the dynamics of obesity prevention policy decision-making using a systems perspective: A case study of Healthy Together Victoria. PLOS One. 2021;16:e0245535.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Contributions
SP conceptualised the study, managed data collection, assisted with data analysis and interpretation, and prepared the manuscript. LB conducted the data analysis and assisted with the preparation of the manuscript. All authors assisted with data interpretation and provided critical review of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
Approval was obtained from the University of New South Wales Human Research Ethics Committee.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pettigrew, S., Booth, L., Dunford, E. et al. An examination of public support for 35 nutrition interventions across seven countries. Eur J Clin Nutr 77, 235–245 (2023). https://doi.org/10.1038/s41430-022-01211-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-022-01211-5