Abstract
The majority of contemporary allogeneic hematopoietic stem cell transplantation (HCT) procedures utilize partially HLA-mismatched stem cell grafts. Donor-specific anti-HLA antibodies (DSA) are associated with primary graft failure independent of the graft source, conditioning intensity and other patient and donor factors. Here we provide an update on testing and monitoring of DSA, review the impact of DSA on stem cell engraftment, and present promising desensitization modalities. Ultimately, we attempt to provide practical recommendations for DSA screening and mitigation strategies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Phelan R, Arora M, Chen M. Current Use and Outcome of Hematopoietic Stem Cell Transplantation: CIBMTR US Summary Slides. 2020.
Shaw BE, Jimenez-Jimenez AM, Burns LJ, Logan BR, Khimani F, Shaffer BC, et al. National Marrow Donor Program-Sponsored Multicenter, Phase II Trial of HLA-Mismatched Unrelated Donor Bone Marrow Transplantation Using Post-Transplant Cyclophosphamide. J Clin Oncol. 2021;39. https://doi.org/10.1200/JCO.20.03502.
Pidala J, Lee SJ, Ahn KW, Spellman S, Wang HL, Aljurf M, et al. Nonpermissive HLA-DPB1 mismatch increases mortality after myeloablative unrelated allogeneic hematopoietic cell transplantation. Blood. 2014;124. https://doi.org/10.1182/blood-2014-05-576041.
Ozdemir ZN, Civriz Bozdağ S. Graft failure after allogeneic hematopoietic stem cell transplantation. Transfus Apher Sci. 2018;57. https://doi.org/10.1016/j.transci.2018.04.014.
Gladstone DE, Bettinotti MP. HLA donor-specific antibodies in allogeneic hematopoietic stem cell transplantation: Challenges and opportunities. Hematology. 2017;2017. https://doi.org/10.1182/asheducation-2017.1.645.
Shaw BE, Mayor NP, Russell NH, Apperley JF, Clark RE, Cornish J, et al. Diverging effects of HLA-DPB1 matching status on outcome following unrelated donor transplantation depending on disease stage and the degree of matching for other HLA alleles. Leukemia. 2010;24. https://doi.org/10.1038/leu.2009.239.
Endres RO, Kleinman SH, Carrick DM, Steele WR, Wright DJ, Norris PJ, et al. Identification of specificities of antibodies against human leukocyte antigens in blood donors. Transfusion. 2010;50. https://doi.org/10.1111/j.1537-2995.2010.02589.x.
Morin-Zorman S, Loiseau P, Taupin JL, Caillat-Zucman S. Donor-specific anti-HLA antibodies in allogeneic hematopoietic stem cell transplantation. Front Immunol. 2016;7. https://doi.org/10.3389/fimmu.2016.00307.
Anasetti C, Amos D, Beatty PG, Appelbaum FR, Bensinger W, Buckner CD, et al. Effect of HLA Compatibility on Engraftment of Bone Marrow Transplants in Patients with Leukemia or Lymphoma. N Engl J Med. 1989;320. https://doi.org/10.1056/nejm198901263200401.
Taylor PA, Ehrhardt MJ, Roforth MM, Swedin JM, Panoskaltsis-Mortari A, Serody JS, et al. Preformed antibody, not primed T cells, is the initial and major barrier to bone marrow engraftment in allosensitized recipients. Blood. 2007;109. https://doi.org/10.1182/blood-2006-05-022772.
Takanashi M, Atsuta Y, Fujiwara K, Kodo H, Kai S, Sato H, et al. The impact of anti-HLA antibodies on unrelated cord blood transplantations. Blood. 2010;116. https://doi.org/10.1182/blood-2009-10-249219.
Cutler C, Kim HT, Sun L, Sese D, Glotzbecker B, Armand P, et al. Donor-specific anti-HLA antibodies predict outcome in double umbilical cord blood transplantation. Blood. 2011;118. https://doi.org/10.1182/blood-2011-05-355263.
Ottinger HD, Rebmann V, Pfeiffer KA, Beelen DW, Kremens B, Runde V, et al. Positive serum crossmatch as predictor for graft failure in HLA-mismatched allogeneic blood stem cell transplantation. Transplantation. 2002;73. https://doi.org/10.1097/00007890-200204270-00016.
Spellman S, Bray R, Rosen-Bronson S, Haagenson M, Klein J, Flesch S, et al. The detection of donor-directed, HLA-specific alloantibodies in recipients of unrelated hematopoietic cell transplantation is predictive of graft failure. Blood. 2010;115. https://doi.org/10.1182/blood-2009-09-244525.
Ciurea SO, Thall PF, Wang X, Wang SA, Hu Y, Cano P, et al. Donor-specific anti-HLAAbs and graft failure in matched unrelated donor hematopoietic stem cell transplantation. Blood. 2011;118. https://doi.org/10.1182/blood-2011-06-362111.
Ciurea SO, De Lima M, Cano P, Korbling M, Giralt S, Shpall EJ, et al. High risk of graft failure in patients with anti-hla antibodies undergoing haploidentical stem-cell transplantation. Transplantation. 2009;88. https://doi.org/10.1097/TP.0b013e3181b9d710.
Ciurea SO, Thall PF, Milton DR, Barnes TH, Kongtim P, Carmazzi Y, et al. Complement-Binding Donor-Specific Anti-HLA Antibodies and Risk of Primary Graft Failure in Hematopoietic Stem Cell Transplantation. Biol Blood Marrow Transplant. 2015;21. https://doi.org/10.1016/j.bbmt.2015.05.001.
Yoshihara S, Maruya E, Taniguchi K, Kaida K, Kato R, Inoue T, et al. Risk and prevention of graft failure in patients with preexisting donor-specific HLA antibodies undergoing unmanipulated haploidentical SCT. Bone Marrow Transplant. 2012;47. https://doi.org/10.1038/bmt.2011.131.
Chang YJ, Zhao XY, Xu LP, Zhang XH, Wang Y, Han W, et al. Donor-specific anti-human leukocyte antigen antibodies were associated with primary graft failure after unmanipulated haploidentical blood and marrow transplantation: A prospective study with randomly assigned training and validation sets. J Hematol Oncol. 2015;8. https://doi.org/10.1186/s13045-015-0182-9.
Xie Y, Parekh J, Tang Z, Wu D, Wu X Donor-Specific Antibodies and Primary Graft Failure in Allogeneic Hematopoietic Stem Cell Transplantation: A Systematic Review and Meta-Analysis. Transplant Cell Ther. 2021;27. https://doi.org/10.1016/j.jtct.2021.04.030.
Bray RA, Tarsitani C, Gebel HM, Lee JH. Clinical Cytometry and Progress in HLA Antibody Detection. 2011;103. https://doi.org/10.1016/B978-0-12-385493-3.00012-7.
Patel R, Terasaki PI Significance of the Positive Crossmatch Test in Kidney Transplantation. N Engl J Med. 1969;280. https://doi.org/10.1056/nejm196904032801401.
O’Rourke RW, Osorio RW, Freise CE, Lou CD, Garovoy MR, Bacchetti P, et al. Flow cytometry crossmatching as a predictor of acute rejection in sensitized recipients of cadaveric renal transplants. Clin Transplant. 2000;14. https://doi.org/10.1034/j.1399-0012.2000.140212.x.
Gatault P, Jollet I, Paintaud G, Magdelaine C, Bridoux F, Lebranchu Y, et al. Erratum to Very low residual concentrations of rituximab long after infusion still induce positive B-cell complement-dependent cytotoxicity-crossmatch. Hum. Immunol. 2013;76:1616-8. https://doi.org/10.1016/j.humimm.2014.12.014.
Milongo D, Vieu G, Blavy S, Del Bello A, Sallusto F, Rostaing L, et al. Interference of therapeutic antibodies used in desensitization protocols on lymphocytotoxicity crossmatch results. Transpl Immunol. 2015;32. https://doi.org/10.1016/j.trim.2015.04.004.
Gebel HM, Bray RA. HLA antibody detection with solid phase assays: Great expectations or expectations too great? Am J Transplant. 2014;14. https://doi.org/10.1111/ajt.12807.
Johnson CP, Schiller JJ, Zhu YR, Hariharan S, Roza AM, Cronin DC, et al. Renal Transplantation with Final Allocation Based on the Virtual Crossmatch. Am J Transplant. 2016;16. https://doi.org/10.1111/ajt.13606.
Wehmeier C, Hönger G, Schaub S Caveats of HLA antibody detection by solid-phase assays. Transpl Int. 2020;33. https://doi.org/10.1111/tri.13484.
Chen G, Sequeira F, Tyan DB Novel C1q assay reveals a clinically relevant subset of human leukocyte antigen antibodies independent of immunoglobulin G strength on single antigen beads. Hum Immunol. 2011;72. https://doi.org/10.1016/j.humimm.2011.07.001.
Loupy A, Lefaucheur C, Vernerey D, Prugger C, van Huyen JPD, Mooney N, et al. Complement-Binding Anti-HLA Antibodies and Kidney-Allograft Survival. N Engl J Med. 2013;369. https://doi.org/10.1056/nejmoa1302506.
Schaub S, Hönger G, Koller MT, Liwski R, Amico P. Determinants of C1q binding in the single antigen bead assay. Transplantation. 2014;98. https://doi.org/10.1097/TP.0000000000000203.
Gebel HM, Bray RA. A diagnostic “C” saw: The ups and downs of C1q testing. Curr Opin Organ Transplant. 2019;24. https://doi.org/10.1097/MOT.0000000000000659.
Peacock S, Kosmoliaptsis V, Bradley AJ, Taylor CJ. Questioning the added value of luminex single antigen beads to detect c1q binding donor HLA-specific antibodies. Transplantation. 2014;98. https://doi.org/10.1097/TP.0000000000000207.
Gallanagh M, Shaw O, Kaur H, Raj K. Successful engraftment in recipients of haploidentical stem cells with donor-specific antibodies: role of flow cytometric cross-match. Bone Marrow Transplant. 2019;54. https://doi.org/10.1038/s41409-018-0384-1.
Pereira J, Cretney C, Aster RH. Variation of class I HLA antigen expression among platelet density cohorts: A possible index of platelet age? Blood. 1988;71. https://doi.org/10.1182/blood.v71.2.516.bloodjournal712516.
Zhang R, He Y, Yang D, Jiang E, Ma Q, Pang A, et al. Combination treatment of rituximab and donor platelets infusion to reduce donor-specific anti-HLA antibodies for stem cells engraftment in haploidentical transplantation. J Clin Lab Anal. 2020;34. https://doi.org/10.1002/jcla.23261.
Yamashita T, Ikegame K, Kojima H, Tanaka H, Kaida K, Inoue T, et al. Effective desensitization of donor-specific HLA antibodies using platelet transfusion bearing targeted HLA in a case of HLA-mismatched allogeneic stem cell transplantation. Bone Marrow Transplant. 2017;52. https://doi.org/10.1038/bmt.2017.10.
Reverberi R, Reverberi L. Removal kinetics of therapeutic apheresis. Blood Transfus. 2007;5. https://doi.org/10.2450/2007.0032-07.
Padmanabhan A, Connelly-Smith L, Aqui N, Balogun RA, Klingel R, Meyer E, et al. Guidelines on the Use of Therapeutic Apheresis in Clinical Practice - Evidence-Based Approach from the Writing Committee of the American Society for Apheresis: The Eighth Special Issue. J Clin Apher. 2019;34. https://doi.org/10.1002/jca.21705.
Barge AJ, Johnson G, Witherspoon R, Torok-Storb B. Antibody-mediated marrow failure after allogeneic bone marrow transplantation. Blood. 1989;74. https://doi.org/10.1182/blood.v74.5.1477.bloodjournal7451477.
Ciurea SO, Al Malki MM, Kongtim P, Fuchs EJ, Luznik L, Huang XJ, et al. The European Society for Blood and Marrow Transplantation (EBMT) consensus recommendations for donor selection in haploidentical hematopoietic cell transplantation. Bone Marrow Transplant. 2020;55. https://doi.org/10.1038/s41409-019-0499-z.
Gergis U, Mayer S, Gordon B, Mark T, Pearse R, Shore T, et al. A strategy to reduce donor-specific HLA Abs before allogeneic transplantation. Bone Marrow Transplant. 2014;49. https://doi.org/10.1038/bmt.2014.11.
Leffell MS, Jones RJ, Gladstone DE. Donor HLA-specific Abs: To BMT or not to BMT? Bone Marrow Transplant. 2015;50. https://doi.org/10.1038/bmt.2014.331.
Choe H, Gergis U, Phillips A, Hsu JM, Sharma V, Shore TB, et al. Bortezomib and Immune Globulin Desensitization for Donor-Specific HLA Antibodies in Haplo-Cord Stem Cell Transplantation. Biol Blood Marrow Transplant. 2017;23. https://doi.org/10.1016/j.bbmt.2016.12.164.
Chang YJ, Xu LP, Wang Y, Zhang XH, Chen H, Chen YH, et al. Rituximab for desensitization during HLA-mismatched stem cell transplantation in patients with a positive donor-specific anti-HLA antibody. Bone Marrow Transplant. 2020;55. https://doi.org/10.1038/s41409-020-0928-z.
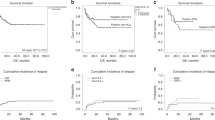
Ciurea SO, Al Malki MM, Kongtim P, Zou J, Aung FM, Rondon G, et al. Treatment of Allosensitized Patients Receiving Allogeneic Transplantation. Blood Adv. 2021. https://doi.org/10.1182/bloodadvances.2021004862.
Woodle ES, Tremblay S, Rossi A, Rojas CC, Alloway R, Roskin K, et al. Plasma cell targeting to prevent antibody-mediated rejection. Am J Transplant. 2020;20. https://doi.org/10.1111/ajt.15889.
Acknowledgements
The authors wish to thank Mia Gergis (Department of Psychology, Tufts University, Boston, Massachusetts) for her copywriting and editing contribution.
Author information
Authors and Affiliations
Contributions
BF: researched the topic and wrote the manuscript. AP and YH: contributed the sections on plasmapheresis, platelets transfusion and DSA monitoring. UG: conceptualized the topic, contributed the sections on DSA desensitization and provided senior guidance. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
File, B., Huang, Y., Peedin, A. et al. The impact of HLA donor-specific antibodies on engraftment and the evolving desensitization strategies. Bone Marrow Transplant 57, 526–531 (2022). https://doi.org/10.1038/s41409-022-01578-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-022-01578-w
This article is cited by
-
The impact of ageing on the distribution of preformed anti-HLA and anti-MICA antibody specificities in recipients from eastern China prior to initial HSCT
Immunity & Ageing (2024)
-
Acute mixed-lineage leukemia treated with desensitization therapy prior to HLA–haploidentical transplantation with high donor-specific antibodies
International Journal of Hematology (2024)
-
A Single Centre Experience of Effective Desensitization Strategy for Children with High Anti-HLA Donor-Specific Antibodies Undergoing Haploidentical Hematopoietic Stem Cell Transplantation
Indian Journal of Hematology and Blood Transfusion (2023)