Abstract
PGF is a devastating complication after allogeneic transplant. We retrospectively analyzed our haploidentical transplant registry to report the incidence and impact of DSA and anti-HLA on engraftment. 107 patients were identified. Median recipient-age of 22, median donor-age of 31. Sixty-two patients had AML (58%), 29 had ALL (27%), 16 (15%) had other malignancies. Sixty-one recipients (57%) had positive anti-HLA, 56 of them had the DSA results available, of these 17 patients had DSAs (15% of the total number of patients, or 28% of patients who have anti-HLA antibodies). The median cumulative MFI was 2062. Sixty-three percent of the DSA were against class-II HLA antigens. The OS, CIR, aGvHD, and cGvHD did not differ between patients with and without anti-HLA antibodies, nor between patients with and without DSA. The gender of the recipient and donor, as well as the gender mismatch between recipient and donor, were statistically associated with the incidence of anti-HLA antibodies. Three patients only developed GF (2.8%), one was primary (0.9%) and the other two secondary GF (1.9%). None of the GF cases was in patients with anti-HLA antibodies or DSA. The presence of anti-HLA or DSAs did not affect the outcomes including the incidence of PGF.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Raw data were generated at King Faisal Specialist Hospital and Research Center, Riyadh, KSA. Derived data supporting the findings of this study are available from the corresponding author [RE] upon request.
References
Ciurea SO, Bayraktar UD. “No donor”? Consider a haploidentical transplant. Blood Rev. 2015;29:63–70.
El Fakih, R., Arat, M., Aljurf, M. Donor Selection and Cell Dose in Haploidentical SCT. In: Demirer, T. editor. Haploidentical Stem Cell Transplantation. Stem Cell Biology and Regenerative Medicine. Humana Press, Cham; 2017. https://doi.org/10.1007/978-3-319-65319-8_2.
El Fakih R, Lazarus HM, Muffly L, Altareb M, Aljurf M, Hashmi SK. Historical perspective and a glance into the antibody-based conditioning regimens: a new era in the horizon? Blood Rev. 2021;52:100892.
Picascia A, Grimaldi V, Napoli C. From HLA typing to anti-HLA antibody detection and beyond: The road ahead. Transplant Rev. 2016;30:187–94.
Ciurea SO, De Lima M, Cano P, Korbling M, Giralt S, Shpall EJ, et al. High risk of graft failure in patients with anti-HLA antibodies undergoing haploidentical stem cell transplantation. Transplantation. 2009;88:1019.
Ciurea SO, Mulanovich V, Jiang Y, Bassett R, Rondon G, McMannis J, et al. Lymphocyte recovery predicts outcomes in cord blood and T cell–depleted haploidentical stem cell transplantation. Biol Blood Marrow Transplant. 2011;17:1169–75.
Ciurea SO, Thall PF, Milton DR, Barnes TH, Kongtim P, Carmazzi Y, et al. Complement-binding donor-specific anti-HLA antibodies and risk of primary graft failure in hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2015;21:1392–8.
Ciurea SO, Thall PF, Wang X, Wang SA, Hu Y, Cano P, et al. Donor-specific anti-HLA Abs and graft failure in matched unrelated donor hematopoietic stem cell transplantation. Blood J Am Soc Hematol. 2011;118:5957–64.
Yoshihara S, Maruya E, Taniguchi K, Kaida K, Kato R, Inoue T, et al. Risk and prevention of graft failure in patients with preexisting donor-specific HLA antibodies undergoing unmanipulated haploidentical SCT. Bone Marrow Transplant. 2012;47:508–15.
Chang Y-J, Zhao X-Y, Xu L-P, Zhang X-H, Wang Y, Han W, et al. Donor-specific anti-human leukocyte antigen antibodies were associated with primary graft failure after unmanipulated haploidentical blood and marrow transplantation: a prospective study with randomly assigned training and validation sets. J Hematol Oncol. 2015;8:1–10.
Spellman S, Bray R, Rosen-Bronson S, Haagenson M, Klein J, Flesch S, et al. The detection of donor-directed, HLA-specific alloantibodies in recipients of unrelated hematopoietic cell transplantation is predictive of graft failure. Blood, J Am Soc Hematol. 2010;115:2704–8.
Ruggeri A, Rocha V, Masson E, Labopin M, Cunha R, Absi L, et al. Impact of donor-specific anti-HLA antibodies on graft failure and survival after reduced intensity conditioning-unrelated cord blood transplantation: a Eurocord, Societe Francophone d’Histocompatibilite et d’Immunogenetique (SFHI) and Societe Francaise de Greffe de Moelle et de Therapie Cellulaire (SFGM-TC) analysis. Haematologica. 2013;98:1154.
Takanashi M, Atsuta Y, Fujiwara K, Kodo H, Kai S, Sato H, et al. The impact of anti-HLA antibodies on unrelated cord blood transplantations. Blood, J Am Soc Hematol. 2010;116:2839–46.
Brunstein CG, Noreen H, DeFor TE, Maurer D, Miller JS, Wagner JE. Anti-HLA antibodies in double umbilical cord blood transplantation. Biol Blood Marrow Transplant. 2011;17:1704–8.
Cutler C, Kim HT, Sun L, Sese D, Glotzbecker B, Armand P, et al. Donor-specific anti-HLA antibodies predict outcome in double umbilical cord blood transplantation. Blood J Am Soc Hematol. 2011;118:6691–7.
Gladstone DE, Zachary AA, Fuchs EJ, Luznik L, Kasamon YL, King KE, et al. Partially mismatched transplantation and human leukocyte antigen donor-specific antibodies. Biol Blood Marrow Transplant. 2013;19:647–52.
Takanashi M, Fujiwara K, Tanaka H, Satake M, Nakajima K. The impact of HLA antibodies on engraftment of unrelated cord blood transplants. Transfusion. 2008;48:791–3.
Anasetti C, Amos D, Beatty PG, Appelbaum FR, Bensinger W, Buckner CD, et al. Effect of HLA compatibility on engraftment of bone marrow transplants in patients with leukemia or lymphoma. N Engl J Med. 1989;320:197–204.
Patel R, Terasaki PI. Significance of the positive crossmatch test in kidney transplantation. N Engl J Med. 1969;280:735–9.
Bramanti S, Calafiore V, Longhi E, Mariotti J, Crespiatico L, Sarina B, et al. Donor-specific anti-HLA antibodies in haploidentical stem cell transplantation with post-transplantation cyclophosphamide: risk of graft failure, poor graft function, and impact on outcomes. Biol Blood Marrow Transplant. 2019;25:1395–406.
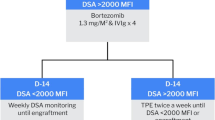
Ciurea SO, Cao K, Fernandez-Vina M, Kongtim P, Al Malki M, Fuchs E, et al. The European Society for Blood and Marrow Transplantation (EBMT) consensus guidelines for the detection and treatment of donor-specific anti-HLA antibodies (DSA) in haploidentical hematopoietic cell transplantation. Bone Marrow Transplant. 2018;53:521–34.
Ciurea SO, Mulanovich V, Saliba RM, Bayraktar UD, Jiang Y, Bassett R, et al. Improved early outcomes using a T cell replete graft compared with T cell depleted haploidentical hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2012;18:1835–44.
Morin-Papunen L, Tiilikainen A, Hartikainen-Sorri A. Maternal HLA immunization during pregnancy: presence of anti HLA antibodies in half of multigravidous women. Med Biol. 1984;62:323–5.
Vichinsky EP, Earles A, Johnson RA, Hoag MS, Williams A, Lubin B. Alloimmunization in sickle cell anemia and transfusion of racially unmatched blood. N Engl J Med. 1990;322:1617–21.
Ferrandiz I, Congy‐Jolivet N, Del Bello A, Debiol B, Trébern‐Launay K, Esposito L, et al. Impact of early blood transfusion after kidney transplantation on the incidence of donor‐specific anti‐HLA antibodies. Am J Transplant. 2016;16:2661–9.
Rees L, Kim JJ. HLA sensitisation: can it be prevented? Pediatr Nephrol. 2015;30:577–87.
Kernan NA, Flomenberg N, Dupont B, O’Reilly RJ. Graft rejection in recipients of T-cell-depleted HLA-nonidentical marrow transplants for leukemia. Identification of host-derived antidonor allocytotoxic T lymphocytes. Transplantation. 1987;43:842–7.
McCurdy SR, Kanakry JA, Showel MM, Tsai H-L, Bolaños-Meade J, Rosner GL, et al. Risk-stratified outcomes of nonmyeloablative HLA-haploidentical BMT with high-dose posttransplantation cyclophosphamide. Blood, J Am Soc Hematol. 2015;125:3024–31.
Giammarco S, Raiola AM, Di Grazia C, Bregante S, Gualandi F, Varaldo R, et al. Second haploidentical stem cell transplantation for primary graft failure. Bone Marrow Transplant. 2021;56:1291–6.
Wang Y, Chang Y-J, Xu L-P, Liu K-Y, Liu D-H, Zhang X-H, et al. Who is the best donor for a related HLA haplotype-mismatched transplant? Blood, J Am Soc Hematol. 2014;124:843–50.
Munchel A, Kesserwan C, Symons HJ, Luznik L, Kasamon YL, Jones RJ, et al. Nonmyeloablative, HLA-haploidentical bone marrow transplantation with high dose, post-transplantation cyclophosphamide. Pediatr Rep. 2011;3:43–7.
Raj K, Pagliuca A, Bradstock K, Noriega V, Potter V, Streetly M, et al. Peripheral blood hematopoietic stem cells for transplantation of hematological diseases from related, haploidentical donors after reduced-intensity conditioning. Biol Blood Marrow Transplant. 2014;20:890–5.
Bacigalupo A, Dominietto A, Ghiso A, Di Grazia C, Lamparelli T, Gualandi F, et al. Unmanipulated haploidentical bone marrow transplantation and post-transplant cyclophosphamide for hematologic malignanices following a myeloablative conditioning: an update. Bone Marrow Transplant. 2015;50:S37–S39.
Solomon SR, Sizemore CA, Sanacore M, Zhang X, Brown S, Holland HK, et al. Haploidentical transplantation using T cell replete peripheral blood stem cells and myeloablative conditioning in patients with high-risk hematologic malignancies who lack conventional donors is well tolerated and produces excellent relapse-free survival: results of a prospective phase II trial. Biol Blood Marrow Transplant. 2012;18:1859–66.
Rondón G, Saliba RM, Khouri I, Giralt S, Chan K, Jabbour E, et al. Long-term follow-up of patients who experienced graft failure postallogeneic progenitor cell transplantation. Results of a single institution analysis. Biol Blood Marrow Transplant. 2008;14:859–66.
Canaani J, Savani BN, Labopin M, Huang X-J, Ciceri F, Arcese W, et al. Impact of ABO incompatibility on patients’ outcome after haploidentical hematopoietic stem cell transplantation for acute myeloid leukemia-a report from the Acute Leukemia Working Party of the EBMT. Haematologica. 2017;102:1066.
Author information
Authors and Affiliations
Contributions
RE, MAA, and MA designed and performed the research, TE analyzed the data. RE wrote the first draft. All the co-authors revised and approved the final paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Altareb, M., Al-Awwami, M., Alfraih, F. et al. “Incidence and significance of donor-specific antibodies in haploidentical stem cell transplantation”. Bone Marrow Transplant 58, 680–686 (2023). https://doi.org/10.1038/s41409-023-01950-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-023-01950-4
This article is cited by
-
Donor specific antibodies (DSA): the only risk factor for primary graft failure?
Bone Marrow Transplantation (2024)