Abstract
Voltage-gated sodium channel Nav1.7 robustly expressed in peripheral nociceptive neurons has been considered as a therapeutic target for chronic pain, but there is no selective Nav1.7 inhibitor available for therapy of chronic pain. Ralfinamide has shown anti-nociceptive activity in animal models of inflammatory and neuropathic pain and is currently under phase III clinical trial for neuropathic pain. Based on ralfinamide, a novel small molecule (S)-2-((3-(4-((2-fluorobenzyl) oxy) phenyl) propyl) amino) propanamide (QLS-81) was synthesized. Here, we report the electrophysiological and pharmacodynamic characterization of QLS-81 as a Nav1.7 channel inhibitor with promising anti-nociceptive activity. In whole-cell recordings of HEK293 cells stably expressing Nav1.7, QLS-81 (IC50 at 3.5 ± 1.5 μM) was ten-fold more potent than its parent compound ralfinamide (37.1 ± 2.9 μM) in inhibiting Nav1.7 current. QLS-81 inhibition on Nav1.7 current was use-dependent. Application of QLS-81 (10 μM) caused a hyperpolarizing shift of the fast and slow inactivation of Nav1.7 channel about 7.9 mV and 26.6 mV, respectively, and also slowed down the channel fast and slow inactivation recovery. In dissociated mouse DRG neurons, QLS-81 (10 μM) inhibited native Nav current and suppressed depolarizing current pulse-elicited neuronal firing. Administration of QLS-81 (2, 5, 10 mg· kg−1· d−1, i.p.) in mice for 10 days dose-dependently alleviated spinal nerve injury-induced neuropathic pain and formalin-induced inflammatory pain. In addition, QLS-81 (10 μM) did not significantly affect ECG in guinea pig heart ex vivo; and administration of QLS-81 (10, 20 mg/kg, i.p.) in mice had no significant effect on spontaneous locomotor activity. Taken together, our results demonstrate that QLS-81, as a novel Nav1.7 inhibitor, is efficacious on chronic pain in mice, and it may hold developmental potential for pain therapy.
Similar content being viewed by others
Introduction
Voltage-gated sodium channels (VGSCs or Navs) are responsible for the initiation and propagation of action potentials in neurons, and dysfunctional Navs are involved in a variety of diseases, including epilepsy, cardiac arrhythmias, and neuropathic pain [1,2,3,4,5]. The subfamily of Nav channels has consisted of ten members, Nav1.1–1.9 and Nax, based on their principal pore-forming α subunits in mammals [6]. As a tetrodotoxin (TTX)-sensitive channel, Nav1.7 encoded by SCN9A gene, is predominately expressed in primary afferent nociceptive and sympathetic neurons, playing an important role in the generation of action potentials and transmission of pain signals [7, 8]. Genetic gain-of-function mutations in Nav1.7 cause various pain conditions, including primary erythromelalgia, paroxysmal extreme pain disorder, and small-fiber neuropathy [9,10,11,12]. Conversely, patients with a loss-of-function mutation of Nav1.7 are in congenital insensitivity to pain [13,14,15]. These investigations indicate that Nav1.7 is critical for pain signaling, and targeting Nav1.7 by specific inhibition may hold therapeutic potential for chronic pain.
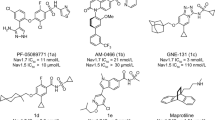
Nonselective Nav inhibitors, such as local anesthetic drug lidocaine, antiarrhythmic drug mexiletine, and antiepileptic drug carbamazepine, have been clinically used for the treatment of chronic pain, but they all exhibit limited efficacy with side effects [16,17,18,19,20]. Therefore, the identification of selective Nav1.7 inhibitor may hold promise for the development of effective analgesics with fewer adverse drug reactions. In recent years, several series of selective and potent Nav1.7 blockers, including PF-05089771, XEN402, and GDC0276, have been reported in clinical trials for the treatment of various pain disorders [1]. Although Nav1.7 small molecule inhibitors are actively pursued in clinical trials, there are no specific Nav1.7 inhibitors currently used for the treatment of pain yet [1, 21].
Ralfinamide, an α-aminoamide derivative, has been shown to exhibit anti-nociceptive activity in animal models of inflammatory and neuropathic pain [22,23,24,25]. As reported by the Adis Insight, ralfinamide is currently still in phase III clinical trial for neuropathic pain in the United Kingdom, Germany, Italy, Poland, Romania, and India (https://adisinsight.springer.com/drugs/800014979). However, ralfinamide is believed to mediate its anti-nociceptive effects through inhibition of ion channels, including Nav1.7, N-type Ca2+ channels, and NMDA receptors [23, 24, 26]. Therefore, it is necessary to improve the selectivity of drug candidate ralfinamide.
In this study, we report the electrophysiological and pharmacological characterization of a novel small molecule (S)-2-((3-(4-((2-fluorobenzyl) oxy) phenyl) propyl) amino) propanamide QLS-81 that was modified based on ralfinamide. QLS-81 shows a tenfold improvement of potency in inhibition of Nav1.7 current than ralfinamide. Our ex vivo and in vivo evaluations further demonstrate that QLS-81 is more efficacious in the alleviation of neuropathic and inflammatory pain than ralfinamide, thus possessing a developmental potential for therapy of chronic pain.
Materials and methods
Cell culture
Human Embryonic Kidney 293 (HEK293) cells stably expressing human Nav1.7 channels were cultured in DMEM (Thermo Fisher, Waltham, MA, USA) supplemented with 10% fetal bovine serum (Thermo Fisher, Waltham, MA, USA), 1% penicillin/streptomycin and 500 μg/mL G418 (Thermo Fisher, Waltham, MA, USA) at 37 °C in a humidified atmosphere of air with 5% CO2. The cells were removed from the culture flask and digested with 2.5 mg/mL trypsin (1:250, Thermo Fisher, Waltham, MA, USA) for 1 min. After centrifugation, cells were suspended and plated on a coverslip with a diameter of 12 mm in a 24-well tissue culture plate at low density. Electrophysiological recordings were carried out within 48 h.
Acutely isolated lumbar dorsal root ganglion (DRG) neurons were prepared from C57BL/6J mice (20–25 g, Beijing Vital River Laboratory Animal Technology Co., Ltd., China) as previously described [27, 28]. Briefly, DRGs (L3–L6) were dissected from the vertebral column and placed in ice-cold minced Ca2+-free Hank’s balanced salt solution. The ganglia were digested at 37 °C in a humidified CO2 incubator with collagenase type 2 (2 mg/mL, Worthington, Lakewood, NJ, USA) and neutral protease dispase II (7.5 mg/mL, Merck, Kenilworth, NJ, USA) for 30 min. Ganglia were then mechanically triturated and washed twice with DMEM supplemented with 10% fetal bovine serum. Thereafter, the DRG cells were plated on poly-D-lysine-coated glass coverslips before further culture for 24 h and used within 48 h.
Chemicals
The synthesis of QLS-81, (S)-2-((3-(4-((2-fluorobenzyl) oxy) phenyl) propyl) amino) propanamide with a molecular weight of 330 Da, was accomplished at Fudan University and its chemical structure was verified by MS and NMR analysis (patent application number: 202011082911.5). Compound QLS-81 was dissolved in dimethyl sulfoxide to obtain a stock solution of 50 mM and was stored at −20 °C. Ralfinamide was purchased from MedChemExpress LLC.
Electrophysiology
Nav1.7 stably transfected HEK293 cells were recorded using the whole-cell patch-clamp technique. Data were acquired at 10 kHz using a MultiClamp 700 A amplifier and pCLAMP 10.6 software (Molecular Devices, Sunnyvale, CA, USA). Patch pipettes were pulled with a horizontal micropipette puller (P-97, Sutter Instruments, USA) and fire-polished with MF-830 polisher (NARISHIGE, Japan). The recording electrodes had a resistance of 2–3 MΩ when filled with pipette solution (in mM): 75 CsF, 65 CsCl, 2.5 MgCl2, 5 EGTA, and 10 HEPES, pH 7.4 adjusted with CsOH. The extracellular bath solution was prepared as follows (in mM): 70 NaCl, 1 MgCl2, 1.8 CaCl2, 4 KCl, 10 glucose, and 10 HEPES, pH 7.4 adjusted with NaOH, osmolality adjusted to 310 mOsm with sucrose. Series resistances were compensated by 60%–80%.
Sodium currents were recorded from small or medium diameter DRG neurons under the voltage-clamp mode in a whole-cell configuration after 16–48 h of dissociation and plating. The TTX-resistant (TTX-R) sodium channel currents consisting mainly of Nav1.8 and Nav1.9 channel currents were recorded in the presence of 300 nM TTX in the external solution. The TTX-sensitive (TTX-S) sodium channel currents in DRG neurons were obtained by digital subtraction of the TTX-R sodium channel currents from the total currents. Pipettes (2–4 MΩ) were filled with solution containing (in mM): 130 CsCl, 9 NaCl, 1 MgCl2, 10 EGTA, 10 HEPES, adjusted to pH 7.3 with CsOH. The bath solution contained (in mM): 30 NaCl, 100 NMDG, 10 TEACl, 10 CsCl, 1 CaCl2, 2 MgCl2, 0.3 CdCl2, 3 4-aminopyridine, 10 HEPES, 10 glucose, adjusted to pH 7.4 with HCl. 4-Aminopyridine and CdCl2 were added to the bath solution to eliminate K+ current and Ca2+ current, respectively. For action potential recordings, the pipette solution contained (in mM): 136 K-gluconate, 10 NaCl, 1 MgCl2, 10 EGTA, 10 HEPES, 2 Mg-ATP, adjusted to pH 7.3 with KOH. The external solution was composed of (in mM): 140 NaCl, 5 KCl, 2 CaCl2, 1 MgCl2, 10 HEPES, 10 glucose, adjusted to pH 7.3 with NaOH. All recordings were made at room temperature and series resistance was compensated by 60%–80%.
Animals
Experimental protocols were approved by the Committee on Animal Care and Use Committee of Qingdao University. C57BL/6J mice (20–25 g) were purchased from the Beijing Vital River Laboratory Animal Technology Co., Ltd. Mice were housed in clear plastic cages with five per cage and had free access to water and food in a climate-controlled room on a standard 12 h light/dark cycle (lights off from 18:00 to 06:00). Those animals were habituated to the experimental conditions and handled for 2–3 days prior precedence to the experiments.
Mouse model of neuropathic pain induced by spared nerve injury
The model of chronic neuropathic pain induced by spared nerve injury (SNI) was established as previously described [29, 30]. Briefly, mice were anesthetized with intraperitoneal (i.p.) injection of chloral hydrate (8%) before exposure of sciatic nerve and its three terminal branches (sural, common peroneal, and tibial nerves) through an incision of biceps femoris. Both tibial and common peroneal nerves were ligated with the removal of about 2 mm section to prevent regeneration. For sham operation, the sciatic nerve was exposed in the same way without ligation and transection of the nerves. Mice under surgery were divided into six groups with ten animals in each group: vehicle control (saline) group, 10 mg/kg ralfinamide group, 5 mg/kg morphine group, and three QLS-81 treated groups with doses of 2 mg/kg, 5 mg/kg and 10 mg/kg. Drugs or compounds were given by i.p. injections once a day starting on day 8 after surgery. Mechanical nociceptive threshold was assessed before and after drugs on days 1, 3, 5, 7, and 10.
The response threshold to the mechanical stimulus was assessed as previously described [31, 32]. Briefly, von Frey filaments with different bending forces were applied through wire mesh floor to the midplantar surface of hind paws for 5 s per filament. The filaments were applied to start with the median stimulus (0.40) and continuing with smaller von Frey hair if mice exhibit a brisk paw withdrawal, flinching, lifting, or licking of left hind paw; otherwise, a next stronger filament was applied. The value of paw mechanical withdrawal threshold (PMWT) as minimal gram force eliciting withdrawal response was calculated based on six consecutive trials for every group of mice.
Mouse model of formalin-induced inflammatory pain
Formalin test was performed as previously described [33, 34]. Briefly, mice were intraperitoneally injected with QLS-81 (5 mg/kg, 10 mg/kg, and 20 mg/kg) or ralfinamide (10 mg/kg) for 1 h or morphine (10 mg/kg) for 15 min before 5% formalin (20 μL) was subcutaneously injected to the left hind paw. The time of licking injected paw was counted every 5 min. Phase I period was defined as 0–5 min and 6–45 min as Phase II.
Ex vivo recording of electrocardiograms in guinea pig hearts
Langendorff-isolated hearts were prepared as previously described [35]. Briefly, guinea pigs (male; 300–350 g) were intraperitoneally injected with heparin (1000 IU/kg) for 5–10 min before they were anesthetized with pentobarbital sodium (50 mg/kg). Isolated hearts were mounted onto a Langendorff-perfusion system and perfused with a modified Tyrode’s solution (mM): 119 NaCl, 25 NaHCO3, 4 KCl, 1.2 KH2PO4, 1 MgCl2, 1.8 CaCl2, and 10 D-glucose, equilibrated with 5% CO2 and 95% O2 with a flow rate of 8 mL/min at 37 °C. Hearts under perfusion were monitored for stability for 20 min before the commencement of experimental procedures. Electrocardiograms (ECG) of guinea pig hearts were continuously recorded with two ECG electrodes (ECG302, MappingLab Ltd., UK) positioned on the right atrium and left ventricle and analyzed using Emapscope4.0 software.
Measurement of locomotor activity
To assess the effect of QLS-81 on locomotion, 32 naive mice were randomly divided into four groups with each group of eight mice: vehicle control (saline) group, 10 mg/kg QLS-81 group, 20 mg/kg QLS-81 group, and 10% urethane group. Animals were transferred into the testing room at least 12 h prior to drug administration. After intraperitoneal administrations of drugs or vehicle for 2 h, mice were individually placed into a corner of each test chamber (length × width: 40 cm × 40 cm) for a 1-min acclimation before the spontaneous locomotor activity was recorded for 5 min using a tracking and computerized analysis system SMART 3.0 (Panlab, Barcelona, Spain). The apparatus was wipe-cleaned with 75% alcohol before the next testing.
Statistical analysis
Whole-cell patch-clamp recording data were analyzed with Clampfit 10.6 (Molecular Devices, USA). Statistical analyses were conducted using OriginPro 8.0 (Origin Lab, USA). The activation curve and steady-state inactivation curves were fitted by the Boltzmann function: y = A2 + (A1 − A2)/[1 + e(x − x0)/dx], where A is the amplitude of voltage-dependent sodium conductance, X0 is the voltage for half-maximal activation. The time constants for recovery from inactivation were fitted by a single exponential function: y = y0 + A1ex/t1. Dose-response curves were fitted with a logistic equation: y = A2 + (A1 − A2)/[1 + (x/IC50)p], A1 and A2 are fixed values of 0 and 1 corresponding to 0% and 100% current inhibition, x is the drug concentration. Statistical analyses were performed using paired/unpaired Student’s t-test. For multiple comparisons, data were analyzed using one-way ANOVA followed by Tukey test or two-way ANOVA followed by Bonferroni post hoc tests. Data points are expressed as the mean ± SEM. A value of P < 0.05 was considered to be statistically significant.
Results
Concentration-dependent inhibition of Nav1.7 current by compound QLS-81
The chemical structure of compound QLS-81 is depicted in Fig. 1a. To evaluate the inhibitory effect of QLS-81 on Nav1.7 current, we utilized a whole-cell patch-clamp recording assay and applied a double-pulse protocol consisting of a conditioning pulse and a test pulse both at 0 mV with 4 ms interval at −130 mV (Fig. 1b, top panel). Approximately 50% of Nav1.7 channels were still recorded at inactivated state after 4 ms repolarization at −130 mV. Perfusing QLS-81 (10 μM) resulted in inhibition of Nav1.7 channel at inactivated state about 72.4% ± 2.7%, as compared with inhibition of 27.9% ± 2.8% at activated state (Fig. 1b). Further administrations of different concentrations of QLS-81 caused a dose-dependent inhibition of Nav1.7 current with an IC50 value of 3.5 ± 1.5 μM (n = 3–11) measured at the second test pulse, as compared with 37.1 ± 2.9 μM (n = 5–8) for ralfinamide (Fig. 1c).
a Chemical structure of QLS-81: (S)-2-((3-(4-((2-fluorobenzyl) oxy) phenyl) propyl) amino) propanamide and ralfinamide. b Left panel, top, Nav1.7 currents stably expressed in HEK293 cells held at −130 mV were elicited by a double-pulse protocol consisting of a conditional pulse at 0 mV (15 ms) for channel activation and a test pulse at 0 mV (15 ms) for 50% channel inactivation. Left panel, bottom, representative current traces elicited by the second test pulse before and after application of QLS-81. The dashed line represents zero-current levels. Right panel, summary for normalized inhibition of activated and inactivated Nav1.7 currents by QLS-81. Paired t-test, ***P < 0.001, n = 10. c Inhibition of representative Nav1.7 current traces elicited by the test pulse (panel (b)) before and after QLS-81 (left panel) and ralfinamide (middle panel) at different concentrations. The dashed line represents zero-current levels. Right panel, curves were fitted using a logistic function for concentration-dependent inhibition of Nav1.7 by QLS-81 (black) with IC50 of 3.5 ± 1.5 μM (n = 3–11) and ralfinamide (red) with IC50 of 37.1 ± 2.9 μM (n = 5–8). d Representative current traces of Nav1.4 (left panel) and Nav1.5 (middle panel) elicited by the depolarizing potential at 0 mV (test pulse of a panel (b)) before and after different concentrations of QLS-81. The dashed line represents zero-current levels. Right panel, curves were fitted using the logistic function for concentration-dependent inhibition of Nav1.4 with IC50 of 37.3 ± 7.3 μM (n = 5) and Nav1.5 with 15.4 ± 1.6 μM (n = 5–8) by QLS-81. All data were expressed as the mean ± SEM.
We next evaluated the selectivity of QLS-81 over other Nav family members, including the skeletal Nav1.4 channel for muscle contraction and the Nav1.5 channel responsible for the generation of a cardiac action potential. Nav1.4 and Nav1.5 currents were recorded using the same double-pulse protocol as Nav1.7. QLS-81 caused a dose-dependent inhibition of Nav1.4 current with an IC50 of 37.3 ± 7.3 μM, which is about tenfold less potent than Nav1.7 current (Fig. 1d). Similarly, inhibition of Nav1.5 current gave rise to an IC50 of 15.4 ± 1.6 μM, which is about fivefold less potency as compared to inhibition of Nav1.7 current (Fig. 1d).
Hyperpolarization shift of Nav1.7 inactivation and prolongation of recovery from inactivation by QLS-81
We started evaluating the effect of QLS-81 on Nav1.7 channel gating kinetics, including voltage-dependent activation, voltage-dependent inactivation, and recovery from inactivation. Nav1.7 currents with robust and instantaneous voltage-dependent activation and rapid inactivation were elicited by a family of depolarization steps with holding potential at −140 mV followed by a series of 14-ms depolarizing pulses from −80 mV to +90 mV in a 10-mV increment (Fig. 2a). As shown in Fig. 2a, b, QLS-81 at 10 μM showed about 20% inhibition on Nav1.7 currents elicited by depolarizing potential to −10 mV that eliciting the maximal current from holding potential at −140 mV (Fig. 2a, b, inset panel). Transforming the I–V curves to G–V curves fitted with Boltzmann function revealed that QLS-81 (10 μM) had no obvious effect on activation gating of Nav1.7 with half activation voltage at −28.0 ± 0.4 mV, as compared with −26.8 ± 0.8 mV in the absence of QLS-81 (Fig. 2b). These results demonstrate a weak inhibition of Nav1.7 channels at open state by QLS-81.
a Top panel, a family of potentials from −80 mV to +90 mV in a 10-mV increment were applied from the holding potential at −140 mV for 14 ms with 1 s intervals. Bottom panels, representative Nav1.7 current traces without (left) or with (right) 10 μM QLS-81. b Normalized conductance versus voltage was plotted for Nav1.7 channels. Curves were fitted by Boltzmann function of half activation voltage (V1/2) for Nav1.7 channels with −26.8 ± 0.8 mV (control) and −28.0 ± 0.4 mV (QLS-81), n = 8. Inset, current–voltage (I–V) relationships with or without QLS-81 (10 μM) normalized with the maximum peak currents obtained from panel a. Paired t-test, *P < 0.05, **P < 0.01, and ***P < 0.001 vs. Control, n = 8. c Top panel, fast inactivation currents of Nav1.7 were elicited with starting by a holding voltage of −130 mV, a family of conditional pulses ranging from −160 mV to −20 mV (500 ms) in a 10-mV increment to cause channel inactivation before a 20 ms test pulse at −10 mV to assess the available non-inactivated channels. Bottom panel, a steady-state fast-inactivation curves of Nav1.7 channels were obtained by Boltzmann function with V1/2 of −89.0 ± 1.2 mV (QLS-81, circles) and the control value of −81.1 ± 0.4 mV (squares), n = 4. d Top panel, Voltage-dependent steady-state slow inactivation of Nav1.7 currents was measured using a series of 10 s pre-pulses, ranging from −130 to −20 mV in a 10-mV increment, followed by a 100 ms step to −140 mV to remove fast inactivation, and a 50 ms test pulse at −10 mV to assess the available non-inactivated channels. Bottom, steady-state slow-inactivation curves of Nav1.7 channels were obtained by Boltzmann function with V1/2 of −72.9 ± 4.4 mV (QLS-81, circles) and the control value of −46.3 ± 4.8 mV (squares), n = 6. e, f Top panels, a standard two-pulse protocol consisting of two depolarizing pulses to −10 mV lasting 50 ms for fast inactivation or 5 s for slow inactivation, and a variable duration step between two depolarizing steps at −120 mV (1–1024 ms for fast inactivation or 1–16384 ms for slow inactivation) for recovery. Bottom panels, channel recovery was determined by normalizing the current elicited from the second test pulse to the first conditioning pulse and plotted versus recovery time. The curves were fitted with a one-exponential function. QLS-81 (circles) delayed the Nav1.7 recovery from fast (e) and slow (f) inactivation with time constants of 14.2 ± 2.2 ms (n = 8) and 366.4 ± 37.1 ms (n = 5) as compared with control value of 5.0 ± 0.5 ms (n = 8) and 133.1 ± 17.2 ms (n = 5). All data were expressed as the mean ± SEM.
We further investigated the effect of QLS-81 on steady-state inactivation of Nav1.7 current, which is a gating process necessary for repetitive firing of action potentials and modulation of excitability of excitable cells [36]. Nav1.7 channel inactivation exists in two separate states: a fast inactivation occurring within milliseconds of activation, and a slow inactivation resulting from repetitive or prolonged stimulation [37]. To test the effect of QLS-81 on the channel inactivation, we applied a family of conditioning pulses of 500 ms for fast inactivation or 10 s for slow inactivation followed by a test pulse at −10 mV (Fig. 2c, d, top panels). Perfusion of QLS-81 at 10 μM caused a significant leftward shift of fast inactivation to −89.0 ± 1.2 mV from −81.1 ± 0.4 mV (Fig. 2c), and slow inactivation to −72.9 ± 4.4 mV from −46.3 ± 4.8 mV (Fig. 2d).
The recovery from inactivation correlates to the use-dependent inhibition determining a drug affinity and effect for inactivated sodium channels [36]. For the recording of recovery from inactivation, we utilized a standard two-pulse protocol consisting of a conditional depolarization pulse at −10 mV for 50 ms (for fast inactivation recovery) or 5 s (for slow inactivation recovery) and a variable interval at −120 mV before a test pulse at −10 mV (Fig. 2e, f, top panels). QLS-81 at 10 μM significantly prolonged the time constant of fast inactivation recovery to 14.2 ± 2.2 ms from 5.0 ± 0.5 ms (Fig. 2e), and the time constant of slow inactivation recovery to 366.4 ± 37.1 ms from 133.1 ± 17.2 ms (Fig. 2f). This increase of recovery time from slow inactivation by QLS-81 suggests some channels entering into a slow inactivated state during depolarization and resulting in accumulation of channels in a drug-modified state, thus leading to use/frequency-dependent inhibition [36].
Use-dependent inhibition of Nav1.7 currents by QLS-81
To test the use-dependent inhibition of Nav1.7 channels by QLS-81, we applied a series of depolarizing pulses at −10 mV for 20 ms with different frequencies of 3 Hz, 5 Hz, 10 Hz, and 30 Hz (Fig. 3a, top panel). As shown in Fig. 3a–d left panels, there was no obvious block of Nav1.7 channel at 3 Hz, 5 Hz, and 10 Hz or a weak inhibition (18%) of the current at 30 Hz in the absence of QLS-81. In contrast, Nav1.7 currents were frequency-dependently inhibited by about 6.3% ± 1.8% (3 Hz), 14.8% ± 6.8% (5 Hz), 32.6% ± 6.4% (10 Hz), and 83.3% ± 6.0% (30 Hz) by QLS-81 at 10 μM (Fig. 3a–d). This result is consistent with the earlier observation that inactivated Nav1.7 channels are more sensitive to the block by QLS-81 (Fig. 1b).
a–d HEK293 cells expressing Nav1.7 channels were held at −120 mV and depolarized to −10 mV for four different frequencies (3, 5, 10, and 30 Hz), with interval pulse potential set at −120 mV. Left panels, representative first (solid line) and last (dashed line) traces of Nav1.7 currents evoked by different frequencies in the absence (left) or presence (right) of QLS-81 (10 μM). Right panels, currents were normalized to the amplitude of the first pulse in the absence (open squares) or presence (open circles) of QLS-81. All data were expressed as the mean ± SEM. Paired t-test, *P < 0.05, **P < 0.01, and ***P < 0.001 vs. Control, n = 4–6.
Reduction of neuronal excitability through inhibition of native Nav current by QLS-81
We also examined the inhibitory effect of QLS-81 on native sodium currents in DRG neurons of small or medium size diameter. Native total sodium currents, TTX-R, and TTX-S Nav currents were elicited by a family of depolarization pulses from −80 mV to +40 mV in a 5-mV increment with a holding potential at −120 mV. Perfusion of QLS-81 (10 μM) significantly inhibited the total sodium current by about 26.1%, TTX-R Nav currents by about 15.1%, and TTX-S Nav currents by about 43.7% in a voltage-dependent manner (Fig. 4a). We also recorded the action potential firing induced by a train of depolarizing current steps from 0 to +300 pA in a 20-pA increment. QLS-81 significantly reduced the numbers of action potentials induced by injection of inward currents from 200 to 300 pA (Fig. 4b). QLS-81 also significantly increased the rheobase currents (depolarization current thresholds for eliciting the first action potential) from 177.1 ± 27.4 pA to 245.7 ± 44.7 pA, and also decreased the amplitude of action potentials induced by 300 pA current injection to 45.4 ± 7.2 mV from 59.7 ± 2.9 mV (Fig. 4c). These data demonstrate that QLS-81 suppresses the excitability of DRG neurons through inhibition of native Nav currents, thus suggesting its antinociceptive activity.
a Left and middle panels, representative total (top panel) currents, TTX-R (middle panel), and TTX-S (bottom panel) currents in DRG neurons of small or medium size diameter were elicited by a family of depolarizing voltage steps in a 5-mV increment from −80 mV to +40 mV with holding potential at −120 mV in the absence (open squares) or presence (open circles) of 10 μM QLS-81. Right panel, current–voltage (I–V) relationships of peak currents normalized with the maximum amplitude of Nav current obtained from left panels n = 7–8. b Representative traces of action potential (AP) induced by injection of different depolarizing currents without (left panel) or with (middle panel) QLS-81. Right panel, summary for the number of action potentials induced by increasing depolarizing currents with or without QLS-81 (10 μM). Paired t-test, *P < 0.05, and **P < 0.01 vs. Control, n = 9. c Left panel, representative traces of AP induced by injection of 300 pA depolarizing currents with (gray) or without (black) QLS-81 (10 μM). Middle panel, a summary of the depolarization current threshold for eliciting the first AP with or without QLS-81 (10 μM). Right panel, summary for the amplitude of induced APs by injection of 300 pA current with or without QLS-81. Paired t-test, *P < 0.05, and **P < 0.01 vs. Control, n = 9. All data were expressed as the mean ± SEM.
Anti-nociceptive effects of QLS-81 on SNI-induced neuropathic pain and formalin-induced inflammatory pain in mice
To evaluate any anti-nociceptive effect of QLS-81 on neuropathic pain, we established the mouse model of spinal nerve injury (SNI) and determined the ipsilateral PMWT at 0.04 ± 0.01 g for the group of SNI surgery on day 6, as compared with that of 1.32 ± 0.11 g for a sham-operated group of mice, indicating a successful establishment of a mouse model of mechanical allodynia. In contrast, intraperitoneal administrations of different doses of QLS-81 for 10 days resulted in a dose-dependent increase of PMWT to 0.30 ± 0.04 g (2 mg/kg), 0.56 ± 0.08 g (5 mg/kg), and 0.98 ± 0.11 g (10 mg/kg) on day 10 in response to mechanical stimuli, as compared with 0.03 ± 0.002 g for vehicle control and 0.58 ± 0.10 g for ralfinamide at 10 mg/kg (Fig. 5a and Table 1). In another group of positive control, intraperitoneal administration of morphine (5 mg/kg) also increased PMWT at 1.19 ± 0.07 g, which is comparable to QLS-81 at 10 mg/kg (Fig. 5a and Table 1).
a Top panel, a schematic time-course of paw mechanical withdrawal threshold (PMWT) measured by von Frey hair stimulation in a mouse model of SNI. Bottom panel, dose-dependent antinociception by QLS-81 (2, 5, and 10 mg/kg, i.p.), morphine (5 mg/kg), and ralfinamide (10 mg/kg) in SNI model. Two-way ANOVA followed by Bonferroni post hoc tests revealed a significant decrease of PMWT between-group sham and group vehicle, ***P < 0.001; a significant increase of PMWT in QLS-81 (2, 5, 10 mg/kg, i.p.) injected groups, compared with group vehicle, ##P < 0.01, ###P < 0.001; and also a significant difference between group QLS-81 (10 mg/kg) and group ralfinamide (10 mg/kg), $$$P < 0.001. All data were expressed as the mean ± SEM, n = 10–12. b Top panel, experimental design, and schedule for formalin test in a mouse model of inflammatory pain. Bottom panels, formalin-induced spontaneous pain behavior was divided into two phases and analyzed following subcutaneous (sc.) injection of formalin. QLS-81 (5, 10, and 20 mg/kg) dose-dependently attenuated the nocifensive behaviors induced by formalin at phase II (right) but not at phase I. One-way ANOVA followed by Tukey test, *P < 0.01 and ***P < 0.001 vs. vehicle, n = 10–12. All data were expressed as the mean ± SEM.
We also assessed the effect of QLS-81 on inflammatory pain induced by formalin in mice. Intraplantar injection of 5% formalin (20 µL) into the hind paw produced a strong nocifensive behavior characterized by paw licking and lifting. Intraperitoneal injections of QLS-81 at different doses showed a trend of antinociception in phase I with a total of paw licking time of 27.3 ± 6.0 s (5 mg/kg), 13.6 ± 4.9 s (10 mg/kg), and 16.3 ± 5.6 s (20 mg/kg), as compared with the vehicle group of 26.2 ± 5.7 s or 18.2 ± 4.0 s for ralfinamide. In contrast, QLS-81 exhibited a dose-dependent inhibition on nocifensive behavior in phase II with the paw licking time of 291.0 ± 46.2 s (5 mg/kg), 201.4 ± 30.3 s (10 mg/kg), and 164.8 ± 26.0 s (20 mg/kg), as compared with 392.8 ± 42.3 s for vehicle control, 294.9 ± 52.0 s for ralfinamide (10 mg/kg) or 29.0 ± 6.5 s for morphine (10 mg/kg) (Fig. 5b and Table 2). These results demonstrate the anti-nociception of QLS-81 in neuropathic pain and inflammatory pain.
Evaluation of QLS-81 for cardiac liability
For cardiac liability concern, we tested the effect of QLS-81 on hERG current stably expressed in HEK293 cells. Genetic loss-of-function mutations or drug inhibition of hERG channels can lead to long QT syndromes or sudden cardiac death [38]. As shown in Fig. 6a, QLS-81 only caused a weak inhibition of hERG current about 21.5% ± 2.6% at a high concentration of 100 μM. Using the electrical mapping technique, we further examined the effect of QLS-81 (10 μM) on cardiac ECG and found no obvious effects of QLS-81 on heart rate (HR), QT interval, PR interval, and QRS duration in guinea pig heart (Fig. 6b, c). These results suggest that QLS-81 may not impose a significant risk of cardiac arrhythmia.
a Left panel, representative hERG currents elicited by depolarization steps of +40 mV before repolarization to −40 mV. The dashed line represents zero-current levels. Right panel, a summary for hERG current inhibition of about 21.5% ± 2.6% by 100 μM QLS-81. Paired t-test, ***P < 0.001 vs. Control, n = 4. b Representative electrocardiograms (ECG) of ex vivo guinea pig heart in electrical mapping assay in the absence (black) or presence (gray) of QLS-81 (10 μM). c Summary for parameters of heart rate (HR), QT interval (the time from the start of the Q wave to the end of the T wave), PR interval (the time from the beginning of the P wave to the beginning of QRS complex) and QRS duration obtained from panel (b). One-way ANOVA, n = 5.
No obvious effect of QLS-81 on locomotion
Locomotor activity is commonly used for the evaluation of psychostimulative or sedative effects. We next tested the effect of QLS-81 on locomotion by assessing the total travel distance and average speed in the open field test. As depicted in Fig. 7, QLS-81 at 10 mg/kg (1663.6 ± 58.4 cm) and 20 mg/kg (1748.4 ± 74.3 cm) had no significant differences in the total travel distance, as compared with the vehicle group (1597.4 ± 67.9 cm). Similarly, QLS-81 at 10 mg/kg (5.6 ± 0.2 cm/s) and 20 mg/kg (5.8 ± 0.2 cm/s) also had no significant differences in the average speed, as compared with the vehicle group (5.3 ± 0.2 cm/s). Mice treated with urethane (10%) as a positive control caused a significant reduction of total travel distance (447.8 ± 83.6 cm) and the average speed (1.5 ± 0.3 cm/s). These results suggest that the QLS-81-mediated antinociceptive activity likely resulted from the inhibition of Nav channels, but not from the sedation effect.
a Representative traces of mouse travel in the open field test after injections of saline, QLS-81 (10 and 20 mg/kg, i.p.), and urethane (10%, i.p.). b The total distance traveled in the open field for 5 min after injections of saline, QLS-81 (10 and 20 mg/kg, i.p.), and urethane (10%, i.p.). c The mean travel speed in open field for 5 min after injection of saline, QLS-81 (10 and 20 mg/kg, i.p.) and urethane (10%, i.p.). One-way ANOVA followed by Tukey test, n = 6–8. All data were expressed as the mean ± SEM. ***P < 0.001 vs. Vehicle.
Discussion
In this study, we identified and characterized a novel small molecule compound QLS-81 that inhibits the Nav1.7 channel with several prominent characteristics. First, QLS-81 exhibits more potent inhibition on the inactivated state of the Nav1.7 channel than the open state. QLS-81 selectively inhibits Nav1.7 channel currents with tenfold potency than the prototype ralfinamide. Second, QLS-81 causes a significant leftward shift of voltage-dependent Nav1.7 inactivation and prolongs the recovery time from inactivation. QLS-81 also exhibits use-dependent inhibition on Nav1.7 current. Third, QLS-81 inhibits native sodium current and reduces firings in DRG neurons. Fourth, QLS-81 exhibits a strong anti-nociceptive effect on SNI-induced neuropathic pain and formalin-induced inflammatory pain with better efficacy than ralfinamide. All these observations suggest that QLS-81 may possess therapeutic potential for chronic pain.
Nav channels are essential for the initiation and propagation of action potentials in excitable cells [6]. Native sodium channels are heteromeric transmembrane proteins that consist of functional α subunits and one or more auxiliary β subunits. There are nine isoforms (Nav1.1–1.9) of α subunits in mammals encoded by nine genes (SCN1A–11A) that are expressed in different excitable tissues and dysfunction of these channels are involved in a variety of diseases, including epilepsy, cardiac arrhythmias, and neuropathic pain [1]. The Nav1.4 subtype is highly expressed in skeletal muscle and genetic mutations of Nav1.4 can cause diseases such as paramyotonia congenita, hyperkalemic periodic paralysis, and hypokalemic periodic paralysis [39, 40]. Although QLS-81 inhibits Nav1.4 with IC50 of 37 μM, it is about tenfold less potent than its inhibition of Nav1.7, which may suggest a less liability concern for skeletal muscles. Nav1.5 subtype is highly expressed in cardiac myocytes and inhibition of Nav1.5 is a liability concern for cardiac arrhythmias [41]. QLS-81 inhibits Nav1.5 current with IC50 of 15 μM and almost 100% inhibition at higher concentration (100 μM), which may impose a liability concern. To make sure this might be less likely, we further investigated the effect of QLS-81 on the hERG channel. QLS-81 even at the high concentration (100 μM) only caused about 21% inhibition of the cardiac hERG channel. In addition, we utilized another electrical mapping assay that evaluates the effect of QLS-81 (10 μM) on cardiac ECG and found no obvious effects of QLS-81 on HR, QT interval, PR interval, and QRS duration in guinea pig heart (Fig. 6b, c). Those results suggest that QLS-81 is less likely to impose any significant cardiac liability. QLS-81 has not been tested on other Nav subtypes such as Nav1.1, Nav1.2, Nav1.3, and Nav1.6 that are predominantly expressed in the central nervous system, and their genetic mutations are linked to epilepsy and CNS-related disorders [6]. Whether QLS-81 also inhibits these Nav subtypes remains to be further tested. In addition, our spontaneous locomotion test shows that mice treated with 20 mg/kg QLS-81 (i.p.) had no significant alteration in the total travel distance and the average speed, suggesting that QLS-81-mediated antinociception is unlikely the result from sedation effects.
QLS-81, modified based on ralfinamide, exhibits a more efficacious anti-nociceptive effect than ralfinamide in the mouse models of neuropathic pain and inflammatory pain likely through blocking Nav channel in DRG neurons. Ralfinamide has been reported to have anti-allodynic and anti-hyperalgesic effects in several animal models of chronic pain through (i) blocking Nav1.7 and Nav1.8 currents; (ii) inhibition of native Ca2+ currents in primary sensory neurons; (iii) antagonizing NMDA receptors; (iv) inhibition of substance P release from spinal cord synaptosomes [25]. Whether QLS-81 also targets Ca2+ channels or NMDA receptors remains to be further tested.
Design and identification of selective Nav1.7 inhibitors have been extremely challenging, because of the shared homology of pore-lining residues among the nine subtypes of mammalian Nav channels [42]. Although peptide toxins and small molecules specific to Nav1.7 inhibition have been identified and reported [43, 44], their clinical benefits of these toxin molecules have not been proven in patients [45]. Although we cannot completely rule out any potential off-target risk caused by QLS-81, QLS-81 is shown to be more potent and efficacious in antinociception than the drug candidate ralfinamide, which suggests its developmental potential for pain therapy.
In summary, we identified a novel small molecule QLS-81 that specifically inhibits the Nav1.7 channel and shows an improved potency and efficacy in comparison with drug candidate ralfinamide. QLS-81 may hold promise for the design of next-generation of Nav1.7 channel blocker and pain therapy.
References
Xu L, Ding X, Wang T, Mou S, Sun H, Hou T. Voltage-gated sodium channels: structures, functions, and molecular modeling. Drug Discov Today. 2019;24:1389–97.
Minett MS, Nassar MA, Clark AK, Passmore G, Dickenson AH, Wang F, et al. Distinct Nav1.7-dependent pain sensations require different sets of sensory and sympathetic neurons. Nat Commun. 2012;3:791.
Choi JS, Boralevi F, Brissaud O, Sanchez-Martin J, Te Morsche RH, Dib-Hajj SD, et al. Paroxysmal extreme pain disorder: a molecular lesion of peripheral neurons. Nat Rev Neurol. 2011;7:51–5.
Claes L, Del-Favero J, Ceulemans B, Lagae L, Van Broeckhoven C, De Jonghe P. De novo mutations in the sodium-channel gene SCN1A cause severe myoclonic epilepsy of infancy. Am J Hum Genet. 2001;68:1327–32.
Gardella E, Becker F, Moller RS, Schubert J, Lemke JR, Larsen LH, et al. Benign infantile seizures and paroxysmal dyskinesia caused by an SCN8A mutation. Ann Neurol. 2016;79:428–36.
Liu Y, Wang K. Exploiting the diversity of ion channels: modulation of ion channels for therapeutic indications. Handb Exp Pharmacol. 2019;260:187–205.
Alexandrou AJ, Brown AR, Chapman ML, Estacion M, Turner J, Mis MA, et al. Subtype-selective small molecule inhibitors reveal a fundamental role for Nav1.7 in nociceptor electrogenesis, axonal conduction and presynaptic release. PLoS One 2016;11:e0152405.
Dib-Hajj SD, Yang Y, Black JA, Waxman SG. The Na(V)1.7 sodium channel: from molecule to man. Nat Rev Neurosci. 2013;14:49–62.
Fertleman CR, Baker MD, Parker KA, Moffatt S, Elmslie FV, Abrahamsen B, et al. SCN9A mutations in paroxysmal extreme pain disorder: allelic variants underlie distinct channel defects and phenotypes. Neuron. 2006;52:767–74.
Waxman SG, Dib-Hajj S. Erythermalgia: molecular basis for an inherited pain syndrome. Trends Mol Med. 2005;11:555–62.
Yang Y, Wang Y, Li S, Xu Z, Li H, Ma L, et al. Mutations in SCN9A, encoding a sodium channel alpha subunit, in patients with primary erythermalgia. J Med Genet. 2004;41:171–4.
Baker MD, Nassar MA. Painful and painless mutations of SCN9A and SCN11A voltage-gated sodium channels. Pflug Arch. 2020;472:865–80.
Cox JJ, Reimann F, Nicholas AK, Thornton G, Roberts E, Springell K, et al. An SCN9A channelopathy causes congenital inability to experience pain. Nature. 2006;444:894–8.
Theile JW, Jarecki BW, Piekarz AD, Cummins TR. Nav1.7 mutations associated with paroxysmal extreme pain disorder, but not erythromelalgia, enhance Navbeta4 peptide-mediated resurgent sodium currents. J Physiol. 2011;589:597–608.
McDermott LA, Weir GA, Themistocleous AC, Segerdahl AR, Blesneac I, Baskozos G, et al. Defining the functional role of NaV1.7 in human nociception. Neuron. 2019;101:905–19.e8.
Alrashood ST. Carbamazepine. Profiles Drug Subst Excip Relat Methodol. 2016;41:133–321.
Hermanns H, Hollmann MW, Stevens MF, Lirk P, Brandenburger T, Piegeler T, et al. Molecular mechanisms of action of systemic lidocaine in acute and chronic pain: a narrative review. Br J Anaesth. 2019;123:335–49.
Singh S, Kerndt C, Zeltser R. Mexiletine. In: StatPearls. FL: Treasure Island; 2020.
Mulroy MF. Systemic toxicity and cardiotoxicity from local anesthetics: incidence and preventive measures. Reg Anesth Pain Med. 2002;27:556–61.
Nguyen PT, DeMarco KR, Vorobyov I, Clancy CE, Yarov-Yarovoy V. Structural basis for antiarrhythmic drug interactions with the human cardiac sodium channel. Proc Natl Acad Sci USA. 2019;116:2945–54.
Sun S, Jia Q, Zenova AY, Wilson MS, Chowdhury S, Focken T, et al. Identification of selective acyl sulfonamide-cycloalkylether inhibitors of the voltage-gated sodium channel (Nav) 1.7 with potent analgesic activity. J Med Chem. 2019;62:908–27.
Liang X, Yu G, Su R. Effects of ralfinamide in models of nerve injury and chemotherapy-induced neuropathic pain. Eur J Pharmacol. 2018;823:27–34.
Stummann TC, Salvati P, Fariello RG, Faravelli L. The anti-nociceptive agent ralfinamide inhibits tetrodotoxin-resistant and tetrodotoxin-sensitive Na+ currents in dorsal root ganglion neurons. Eur J Pharmacol. 2005;510:197–208.
Veneroni O, Maj R, Calabresi M, Faravelli L, Fariello RG, Salvati P. Anti-allodynic effect of NW-1029, a novel Na+ channel blocker, in experimental animal models of inflammatory and neuropathic pain. Pain. 2003;102:17–25.
Zhang SH, Blech-Hermoni Y, Faravelli L, Seltzer Z. Ralfinamide administered orally before hindpaw neurectomy or postoperatively provided long-lasting suppression of spontaneous neuropathic pain-related behavior in the rat. Pain. 2008;139:293–305.
Colombo E, Curatolo L, Caccia C, Salvati P, Faravelli L. 344 ralfinamide acts through nmda receptor complex: a central role for chronic pain treatment. Eur J Pain. 2007;11:S152–S3.
Du X, Hao H, Gigout S, Huang D, Yang Y, Li L, et al. Control of somatic membrane potential in nociceptive neurons and its implications for peripheral nociceptive transmission. Pain. 2014;155:2306–22.
Andersen PL, Doucette JR, Nazarali AJ. A novel method of eliminating non-neuronal proliferating cells from cultures of mouse dorsal root ganglia. Cell Mol Neurobiol. 2003;23:205–10.
Bourquin AF, Suveges M, Pertin M, Gilliard N, Sardy S, Davison AC, et al. Assessment and analysis of mechanical allodynia-like behavior induced by spared nerve injury (SNI) in the mouse. Pain. 2006;122:14.
Wang X, Zhang G, Qiao Y, Feng C, Zhao X. Crocetin attenuates spared nerve injury-induced neuropathic pain in mice. J Pharmacol Sci. 2017;135:141–7.
Bonin RP, Bories C, De, Koninck Y. A simplified up-down method (SUDO) for measuring mechanical nociception in rodents using von Frey filaments. Mol Pain. 2014;10:26.
Boccella S, Guida F, Palazzo E, Marabese I, de Novellis V, Maione S, et al. Spared nerve injury as a long-lasting model of neuropathic pain. Methods Mol Biol. 2018;1727:373–8.
Harton LR, Richardson JR, Armendariz A, Nazarian A. Dissociation of morphine analgesic effects in the sensory and affective components of formalin-induced spontaneous pain in male and female rats. Brain Res. 2017;1658:36–41.
Zhang Y, Peng D, Huang B, Yang Q, Zhang Q, Chen M, et al. Discovery of a novel Nav1.7 inhibitor from cyriopagopus albostriatus venom with potent analgesic efficacy. Front Pharmacol. 2018;9:1158.
Qiu B, Wang Y, Li C, Guo H, Xu Y. Utility of the JT peak interval and the JT area in determining the proarrhythmic potential of QT-shortening agents. J Cardiovasc Pharmacol Ther. 2019;24:160–71.
Wang Y, Mi J, Lu K, Lu Y, Wang K. Comparison of gating properties and use-dependent block of Nav1.5 and Nav1.7 channels by anti-arrhythmics mexiletine and lidocaine. PLoS One. 2015;10:e0128653.
Ghovanloo MR, Aimar K, Ghadiry-Tavi R, Yu A, Ruben PC. Physiology and pathophysiology of sodium channel inactivation. Curr Top Membr. 2016;78:479–509.
Sanguinetti MC, Tristani-Firouzi M. hERG potassium channels and cardiac arrhythmia. Nature. 2006;440:463–9.
Jurkat-Rott K, Holzherr B, Fauler M, Lehmann-Horn F. Sodium channelopathies of skeletal muscle result from gain or loss of function. Pflug Arch. 2010;460:239–48.
Huang S, Zhang W, Chang X, Guo J. Overlap of periodic paralysis and paramyotonia congenita caused by SCN4A gene mutations two family reports and literature review. Channels. 2019;13:110–9.
Song W, Shou W. Cardiac sodium channel Nav1.5 mutations and cardiac arrhythmia. Pediatr Cardiol. 2012;33:943–9.
Ahuja S, Mukund S, Deng L, Khakh K, Chang E, Ho H, et al. Structural basis of Nav1.7 inhibition by an isoform-selective small-molecule antagonist. Science. 2015;350:aac5464.
Bosmans F, Swartz KJ. Targeting voltage sensors in sodium channels with spider toxins. Trends Pharmacol Sci. 2010;31:175–82.
de Lera Ruiz M, Kraus RL. Voltage-gated sodium channels: structure, function, pharmacology, and clinical indications. J Med Chem. 2015;58:7093–118.
Murray JK, Ligutti J, Liu D, Zou A, Poppe L, Li H, et al. Engineering potent and selective analogues of GpTx-1, a tarantula venom peptide antagonist of the Nav1.7 sodium channel. J Med Chem. 2015;58:2299–314.
Acknowledgements
This work is supported by research grants from the Science and Technology Program of Guangdong (2018B030334001), the Ministry of Science and Technology of China (2018ZX09711001-004-006) awarded to KWW, and the National Natural Science Foundation of Shandong Province (ZR2020QH100).
Author information
Authors and Affiliations
Contributions
YNL, ARZ, and KWW conceived and designed the research; HLN, YNL, LYD, JW, and HJL performed experiments; DQX and YLZ designed and synthesized compound QLS-81; HLN and YNL analyzed data, prepared figures, and drafted manuscript; YNL, LMS, and KWW edited and revised manuscript; YNL, LMS, and KWW approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Rights and permissions
About this article
Cite this article
Niu, Hl., Liu, Yn., Xue, Dq. et al. Inhibition of Nav1.7 channel by a novel blocker QLS-81 for alleviation of neuropathic pain. Acta Pharmacol Sin 42, 1235–1247 (2021). https://doi.org/10.1038/s41401-021-00682-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41401-021-00682-9
Keywords
This article is cited by
-
Long noncoding RNA small nucleolar RNA host gene 5 facilitates neuropathic pain in spinal nerve injury by promoting SCN9A expression via CDK9
Human Cell (2024)
-
Naphthylisoquinoline alkaloids, a new structural template inhibitor of Nav1.7 sodium channel
Acta Pharmacologica Sinica (2023)
-
Suberoylanilide Hydroxamic Acid Ameliorates Pain Sensitization in Central Neuropathic Pain After Spinal Cord Injury via the HDAC5/NEDD4/SCN9A Axis
Neurochemical Research (2023)