Abstract
The voltage-gated sodium channel isoform NaV1.7 is highly expressed in dorsal root ganglion neurons and is obligatory for nociceptive signal transmission. Genetic gain-of-function and loss-of-function NaV1.7 mutations have been identified in select individuals, and are associated with episodic extreme pain disorders and insensitivity to pain, respectively. These findings implicate NaV1.7 as a key pharmacotherapeutic target for the treatment of pain. While several small molecules targeting NaV1.7 have been advanced to clinical development, no NaV1.7-selective compound has shown convincing efficacy in clinical pain applications. Here we describe the discovery and characterization of ST-2262, a NaV1.7 inhibitor that blocks the extracellular vestibule of the channel with an IC50 of 72 nM and greater than 200-fold selectivity over off-target sodium channel isoforms, NaV1.1–1.6 and NaV1.8. In contrast to other NaV1.7 inhibitors that preferentially inhibit the inactivated state of the channel, ST-2262 is equipotent in a protocol that favors the resting state of the channel, a protocol that favors the inactivated state, and a high frequency protocol. In a non-human primate study, animals treated with ST-2262 exhibited reduced sensitivity to noxious heat. These findings establish the extracellular vestibule of the sodium channel as a viable receptor site for the design of selective ligands targeting NaV1.7.
Similar content being viewed by others
Introduction
The voltage-gated sodium ion channel (NaV) isoform 1.7 has emerged as a high-interest target for the discovery of non-opioid pain therapeutics based on compelling validation from human genetics and preclinical studies1. NaV1.7 loss-of-function mutations result in whole-body insensitivity to pain; conversely, gain-of-function variants are associated with episodic extreme pain disorders and small fiber neuropathies2,3,4,5. Discovery of selective inhibitors of NaV1.7 has been challenging due to the structural conservation of off-target NaV isoforms (NaV1.1–1.6, NaV1.8 and NaV1.9), inhibition of which is likely to result in safety liabilities6,7,8.
NaVs are integral membrane proteins expressed in excitable cells that comprise a ~ 260 kD pore-forming α-subunit and up to two accessory β-subunits (Fig. 1A)9. The central pore of the α-subunit is encircled by four voltage-sensing domains (VSD I–IV). Channel gating occurs through protein conformational changes in response to membrane depolarization. At least nine discrete binding sites on the NaV α-subunit have been identified for peptides and small molecules that influence ion conductance10. The large majority of molecules that engage NaVs bind preferentially to a specific conformational state of the channel and show use-dependent activity. Clinical NaV inhibitors (e.g., bupivacaine, lidocaine, carbamazepine) are both state- and frequency-dependent agents that lodge in the intracellular pore of the α-subunit, a site that is highly conserved between isoforms. These drugs rely on local administration to achieve a margin between the desired pharmacodynamic effect and dose-limiting side effects. Certain investigational NaV inhibitors, such as peptide toxins isolated from venomous species, interact with VSDs to alter the kinetics or voltage dependence of channel activation or inactivation11,12. Similarly, a class of small molecule aryl and acyl sulfonamide compounds bind to an activated conformation of VSD IV and prevent recovery from inactivation (Fig. 1B)13,14,15,16. By contrast, cationic guanidinium toxins and peptide cone snail toxins inhibit ion conduction by sterically occluding the extracellular vestibule of the channel pore (Site 1). The former are a unique collection of small molecule natural products exemplified by saxitoxin and tetrodotoxin—high affinity, state-independent blockers against six of nine NaV subtypes (Fig. 1C)17.
(A) Cryo-EM structure of STX bound to human NaV1.7-β1-β2 complex (PDB: 6j8g) with GX-936 positioned approximately based on PDB: 5ek0 in Pymol version 2.0.4 (Schrodinger, New York, NY). (B) Representative NaV1.7 inhibitors that bind VSD IV. (C) Natural NaV inhibitors that bind to the extracellular vestibule18,19,20,21.
In the pursuit of isoform-selective inhibitors of NaV1.7, two binding sites, the cystine knot toxin site at VSD II and the sulfonamide site at VSD IV, have been heavily interrogated. Certain cystine knot toxins that engage VSD II such as HwTx-IV, Pn3a, and ProTx-II exhibit 6–1,000× selectivity for NaV1.7 over other channel isoforms. Potency and selectivity for this target have been improved with synthetic peptide toxin derivatives22,23,24,25,26. Among small, Lipinski-type molecules, only the aryl and acyl sulfonamides pioneered by Icagen/Pfizer and subsequently investigated by Amgen, Chromocell, Genentech/Xenon, Merck, and others have shown evidence of significant NaV1.7 isoform selectivity7,16. Within the sulfonamide series, selectivity levels are > 1,000× over certain off-target isoforms including the cardiac isoform, NaV1.5, but generally 10–50× against NaV1.2 and NaV1.6. Many but not all sulfonamide NaV1.7 inhibitors suffer from undesirable pharmaceutical properties, including high plasma protein binding (e.g. > 99.8%), cytochrome p450 inhibition, in vitro hepatotoxicity and high unbound clearance27,28, which have hindered clinical development. Although a number of candidates have been advanced to human testing, one compound has been discontinued after a Phase 2 study likely due to limited efficacy (PF-05089771); others have been discontinued after Phase 1 trials for reasons that may be related to safety liabilities such as elevated expression of liver transaminases and hypotension (GDC-0276)29,30.
Electrophysiology studies with naturally occurring Site 1 ligands against different wild-type and mutant NaV isoforms have identified the extracellular vestibule of NaV1.7 as a promising locus for selective inhibitor design31,32,33. The outer mouth of the channel is formed from residues that link the S5–S6 helices (referred to as pore loops) from each of the four domains. The domain III pore loop of human NaV1.7 contains a T1398/I1399 sequence motif that is not present in other human NaV subtypes (which contain MD at equivalent positions, Suppl Table 1)31. Comparison of the amino acid sequence of the domain III pore loop across species indicates that the sequence motif in hNaV1.7 is unique to primates. The half-maximal inhibitory concentration (IC50) value for saxitoxin (STX) is markedly altered (250-fold change) depending on the presence or absence of the T1398 and I1399 residues. Against rNaV1.4, the IC50 of STX is 2.8 ± 0.1 nM compared to 702 ± 53 nM for hNaV1.731. Introduction of the alternative domain III pore loop sequence by mutagenesis restores potency (hNaV1.7 T1398M/I1399D IC50 = 2.3 ± 0.2 nM). These findings suggest that it may be possible to capitalize on structural differences in the extracellular vestibule between hNaV isoforms to design NaV1.7-selective inhibitors.
Recent advances in the de novo synthesis of guanidinium toxin analogues have enabled systemic examination of the structure–activity relationship (SAR) properties that govern hNaV1.7 potency and isoform selectivity34,35,36,37. Prior to 2016, the binding orientation of STX proposed in the literature indicated that the C11 methylene carbon was positioned proximally to domain III pore loop residues38,39,40. SAR and mutant cycle analysis studies posited a revised pose in which the C13 carbamate moiety abuts DIII32. This revised binding pose was recently confirmed by cryoelectron microscopy (cryo-EM) structures of STX bound to NaVPaS and hNaV1.718,41. In the present study, analogues of STX substituted at both the C11 and C13 positions were investigated to understand the requirements for selective inhibition of hNaV1.7. These efforts led to the discovery of ST-2262, a potent and selective inhibitor of NaV1.7 that reduces sensitivity to noxious heat in a preliminary study in non-human primates (NHPs).
Results
Discovery of ST-2262
ST-2262 was discovered through a rational design strategy aimed at identifying derivatives of natural bis-guanidinium toxins that preferentially inhibit hNaV1.7 over other off-target hNaV isoforms31. Mutagenesis, homology modeling, and docking studies conducted prior to 2016 suggested that bis-guanidinium toxins orient in the outer mouth of the channel with the C11 methylene center positioned toward the domain III pore loop of NaV (Fig. 2A, Original pose)38,39,40. Exploration of substitution at C11 of decarbamoyl saxitoxin (dcSTX) led to the identification of a series of analogues bearing aryl amide groups at this site. Certain compounds, as exemplified by ST-282, show excellent potency against hNaV1.7 but minimal selectivity (~ 1:1) over off-target isoforms such as hNaV1.4 (Fig. 2B). The finding that hNaV1.7 isoform selectivity could not be achieved by modification of the C11 substituent led us to investigate SAR at alternative positions. These studies followed evidence that the proper binding orientation of STX is rotated ~ 180° from earlier models, thus placing the C13 substituent in close proximity to domain III (Fig. 2A, Revised pose)32.
(A) The consensus pose for binding of STX in the extracellular vestibule of NaV oriented C11 in proximity to the DIII pore loop prior to 201638. A revised pose based on mutant cycle analysis and recent cryo-EM structures orients the C13 carbamate near DIII32,41. (B) ST-2262 was discovered by a rational design strategy aimed at identifying functional groups that interact with the DIII T1398/I1399 sequence motif unique to primate NaV1.7. Values are mean (95% CI).
Derivatives of STX bearing amide, carbamate, ester, ether, and urethane substituents at the C13 position were prepared in an effort to identify compounds with improved selectivity for hNaV1.7. Insight from studies of a naturally-occurring STX C13 acetate congener, STX-OAc, helped guide selection of compounds for synthesis (Suppl Figure 1)32. The difference in potencies between STX and STX-OAc is striking considering that these two structures vary at a single position (NH2 → CH3). Following this lead, we explored substituents at C13 that could replace the hydrolytically unstable acetate group. Ultimately, the C13 succinimide was discovered as a suitable acetate isostere, which was paired with a C11 tetrahydronaphthyl amide to generate ST-2262, the focus of the present study.
ST-2262 is a potent and selective inhibitor of hNaV1.7
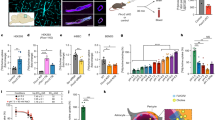
The potency of ST-2262 against hNaV1.7 stably expressed in HEK293 cells was assessed by manual patch clamp electrophysiology with a voltage-protocol that favors the resting state of the channel. Using a stimulation protocol with a holding potential of – 110 mV and a stimulus frequency of 0.33 Hz, the IC50 of ST-2262 against hNaV1.7 was measured at 0.072 µM (95% confidence interval (CI) 0.064–0.082) (Fig. 3A, Suppl Table 2). Potencies against off-target sodium channel isoforms (hNaV1.1–1.6, hNaV1.8) were determined following a similar protocol. Activity against hNaV1.9 was not evaluated due to the difficulty of expressing this subtype heterologously42. ST-2262 was determined to be > 200-fold selective over hNaV1.6 (IC50 = 17.9 µM, 95% CI 14.8–22.1), > 900-fold selective over hNaV1.3 (IC50 = 65.3 µM, CI 62.7–68.1), and > 1,000-fold selective over all other NaV isoforms tested. Similar IC50 values against the eight hNaV subtypes were obtained in an independent study using the PatchXpress automated electrophysiology platform (Suppl Table 3).
(A) Dose–response curves for the inhibitory effect of ST-2262 on NaV1.1–NaV1.8 stably expressed in CHO or HEK293 cells using a single-pulse (resting state) protocol with a 10 ms pulse from a holding potential of – 110 mV to voltage at peak activation (– 20 to + 10 mV). NaV1.X IC50 (in µM, mean, 95% CI). NaV1.1: > 100; NaV1.2: > 100; NaV1.3: 65.3, 62.7–68.1; NaV1.4: 80.7, 71.1–93.3; NaV1.5: > 100; NaV1.6: 17.9, 14.8–22.1; NaV1.7: 0.072, 0.064–0.082; NaV1.8: > 100. (B) Comparison of dose–response relationship of ST-2262 inhibition against NaV1.7 using different stimulation protocols: resting state; two-pulse protocol contained an 8 s conditioning step to the voltage at half-inactivation, followed by a 20 ms step to voltage at full activation (half-inactivation protocol)16; high frequency single-pulse protocol stimulated at 30 Hz. NaV1.7 IC50 (in µM, mean, 95% CI). Resting state: 0.123, 0.104–0.145; half-inactivation: 0.087, 0.056–0.120; high frequency: 0.112, 0.015–0.357. (C) Comparison of dose–response relationship of NaV1.7 inhibition against WT mNaV1.7 and M1407T/D1408I mNaV1.7 on a resting state protocol. mNaV1.7 IC50 (in µM, 95% CI). WT: 2.57, 2.30–2.87; M1407T/D1408I: 0.130, 0.055–0.307. (D) Comparison of dose–response of ST-2262 against transiently expressed hNaV1.7 WT, hNaV1.7 D1690N, and hNav1.7 T1398M/I1399D. IC50 (in µM, mean, 95% CI). WT: 0.039, 0.032–0.047; D1690N: > 100; T1398M/I1399D: 1.87, 1.47–2.39.
Exposure of hNaV1.1 and hNaV1.2 to high concentrations of ST-2262 (10–100 µM) resulted in a reduction of the rate of fast inactivation; a similar effect was noted, albeit to a lesser degree, with hNaV1.3 and hNaV1.4 (Suppl Figure 2). Lower concentrations of ST-2262 (1–3 µM), which remain sufficiently high to achieve > 90% inhibition of hNaV1.7, had no measurable effect on fast inactivation of hNaV1.1 and hNaV1.2. It is possible that elevated concentrations of ST-2262 result in a secondary mode of binding against these NaV subtypes, however, efforts have not been made to examine such a mechanism at this time. To our knowledge, changes in the rate of fast inactivation have not been observed with STX.
To investigate whether the potency of ST-2262 was dependent on the membrane holding potential or frequency of stimulus, an IC50 value was measured against hNaV1.7 using a two-pulse protocol with a pre-pulse to the voltage at half-inactivation (8 s step) and with a protocol that depolarizes the cell at high frequency (30 Hz stimulus). The potency of ST-2262 was not appreciably altered using either stimulation protocol (IC50 = 0.087 µM, 0.056–0.120 and IC50 = 0.112 µM, 0.015–0.357, respectively; Fig. 3B, Suppl Table 4). These results indicate that ST-2262 is a selective, use-independent inhibitor of hNaV1.7.
Species variation in potency and mutagenesis
The potency of ST-2262 was assessed against a panel of species variants of NaV1.7, including mouse, rat, and cynomolgus monkey (Suppl Table 5). Consistent with the hypothesis that NaV1.7 potency is affected by the presence of the T1398/I1399 sequence motif in the DIII pore loop, the IC50 of ST-2262 against cynoNaV1.7 (0.101 µM, 0.073–0.140) was similar to human. In contrast, ST-2262 was > 50 × less potent against mouse (IC50 = 3.78 µM, 3.23–4.43) and rat NaV1.7 (IC50 = 4.95 µM, 4.17–5.87) than the human ortholog. Affinity was restored within twofold of the hNaV1.7 potency by introduction of domain III MD-TI mutations to mouse NaV1.7 (IC50 = 0.130 µM, 0.055–0.307; Fig. 3C, Suppl Table 6).
Multiple lines of evidence suggest that ST-2262 binds to the extracellular vestibule of the sodium channel (i.e., Site 1) including: (i) the structural similarity of ST-2262 to natural bis-guanidinium toxin ligands, (ii) the state- and frequency-independent mode of NaV inhibition that is characteristic of extracellular pore blockers, and (iii) the influence of DIII pore loop residues on potency. To gain additional support that ST-2262 binds to the outer pore of NaV, we generated a point mutant of hNaV1.7, D1690N, at a position known to significantly destabilize binding of STX39. The domain IV residue D1690 forms a critical bridged hydrogen bond with the C12 hydrated ketone of STX39,41. We also measured potency against the hNaV1.7 T1398M/I1399D double mutant to directly confirm that the domain III TI sequence motif contributes to hNaV1.7 affinity31. The introduction of other point mutations to NaV1.7 was attempted (Y362S and E916A), but these variants proved challenging to express39,43. ST-2262 exhibited a > 1,000-fold loss in potency against hNaV1.7 D1690N (IC50 > 100 µM) and a ~ 48-fold loss against hNaV1.7 T1398M/I1399D (IC50 = 1.87 µM, 1.47–2.39) compared to the wild-type channel (IC50 = 0.039 µM, 0.032–0.047; Fig. 3D, Suppl Table 6). Collectively, these results indicate that ST-2262 binds to the extracellular vestibule of NaV1.7, displaying significant species variation in potency and isoform selectivity in large part due to molecular interactions with residues T1398 and I1399, which are unique to human and non-human primate NaV1.7 orthologs31,32.
ST-2262 increases withdrawal latency in a nonhuman primate model of thermal pain
Mice and humans with genetic NaV1.7 loss-of-function are profoundly insensitive to noxious heat2,3,44,45,46. To understand whether pharmacological block of NaV1.7 affects noxious thermal sensitivity, we conducted an initial evaluation (n = 4) of the effect of ST-2262 in a non-human primate (NHP) model of acute thermal pain. Experiments were approved by the Montana State University institutional animal care and use committee and performed in accordance with institutional, national, and international guidelines and regulations. It is not possible to study the influence of ST-2262 on acute thermal pain in rodents as this compound is > 50-fold less potent against NaV1.7 in species that lack the T1398/I1399 sequence motif (Suppl Table 5). A NHP model of acute thermal pain was identified that uses a heat lamp to deliver a stimulus to the dorsal surface of the hand of lightly anesthetized cynomolgus macaques and measures the time to withdrawal47. Prior to advancing ST-2262 into the NHP acute thermal pain model, a standard battery of preclinical assays was completed to evaluate ADME and pharmacokinetic properties of this compound in cynomolgus macaques (Suppl Table 7). Off-target activity of ST-2262 using a commercially available radioligand binding assay panel against 68 different targets was also measured (LeadProfilingScreen, Eurofins, Taipei, Taiwan). No hits were identified on the off-target panel, defined as > 50% inhibition with 10 µM ST-2262 (Suppl Table 8).
Male cynomolgus monkeys were anesthetized with propofol to a level in which the withdrawal reflex of the hand occurred at a consistent latency of approximately 3 s, a response time that was comparable to the detection of sharp pain from Aδ fibers when tested in prior studies on human volunteers48,49. The dorsal surface of the hand was exposed to a thermal stimulus that selectively activates Aδ-fiber nociceptors (Fig. 4A–C)47,50. The thermal stimulus was turned off at 5 s to prevent tissue damage. Heart rate was monitored throughout the study, and presentation of the noxious thermal stimuli consistently led to a transient increase in heart rate that peaked seconds after the stimulus and then returned to baseline (ΔHR). Acute noxious thermal stimuli transiently increase heart rate in human subjects; the percent change in heart rate correlates with subjective pain score51.
ST-2262 increases withdrawal latency and reduces thermal evoked heart rate increase in a non-human primate noxious heat model. (A,B) Individual subject data points showing changes in withdrawal latency (A) and transient change in heart rate (ΔHR) (B) following thermal stimuli. Bar graphs are expressed as mean ± SEM. **Dunnett’s multiple comparison test, compared to baseline, p < 0.01. (C) Plasma level concentration of ST-2262 in plasma at different doses. (D,E) A lower heating rate thermal stimulus was presented for a maximum of 20 s, which selectively activates C fibers47. In two subjects, the C-fiber-induced hand withdrawal response was replicable for testing. The efficacy endpoints measured were withdrawal latency (A) and heart rate change (B).
ST-2262 hydrochloride administered IV increased the withdrawal latency to noxious thermal stimuli (Fig. 4A). Efficacy was assessed in one subject at four dose levels (0.01, 0.05, 0.25, 1.25 mg/kg), in two subjects at the three higher dose levels (0.05, 0.25, 1.25 mg/kg), and in one additional subject at the highest dose level only (1.25 mg/kg). At the highest dose of 1.25 mg/kg, all four animals showed no hand withdrawal prior to the 5 s cut-off latency (Fig. 4A), a significant increase in withdrawal latency compared to baseline values (Mixed effects model: F(3,7) = 7.468, p < 0.05; 0.01 mg/kg was not included in this analysis because only one subject received this dose). The 1.25 mg/kg dose of ST-2262 also almost completely reduced ΔHR (Fig. 4B; Mixed effects model: F(3,7) = 6.654, p < 0.05.)
Plasma samples were obtained from animals to assess the PK/PD relationship between drug exposure and thermal withdrawal latency. We found that 0.25 mg/kg ST-2262 resulted in ~ 1,400 ng/ml in plasma at the 5 min time point (n = 2), which corresponds to 7× the IC50 value of ST-2262 against cynoNaV1.7, corrected for plasma protein binding (cyno PPB = 73.5%). The unbound exposure of drug was reduced to 3.4 × cynoNaV1.7 IC50 at the 30 min time point. At a dose of 1.25 mg/kg, the total plasma concentration was ~ 7,000 ng/ml at 5 min (n = 2), which corresponds to an unbound exposure of 32 × cynoNaV1.7 IC50, and was maintained above 15× cynoNaV1.7 IC50 for over 100 min (Fig. 4C). Lumbar CSF samples collected from two animals receiving the 1.25 mg/kg dose indicated that ST-2262 was peripherally restricted, with CSF:plasma ratios < 10–3 (n = 2; [ST-2262] 0.8, < 0.5 ng/ml in CSF).
By adjusting radiant heat parameters, the noxious heat model can be used to selectively assess responses to cutaneous C-fiber nociceptor activation, which produces a burning pain in volunteers48,49. The effect of ST-2262 on C-fiber induced hand withdrawal and heart rate change was investigated on two cynomolgus subjects47. As with the Aδ nociceptive response, 1.25 mg/kg ST-2262 completely abolished the C-fiber-mediated hand withdrawal and ΔHR (Fig. 4D,E). Collectively, these results are consistent with the hypothesis that pharmacological block of NaV1.7 reduces sensitivity to noxious heat, phenotypically analogous to studies of NaV1.7 loss-of-function in CIP patients2. In addition, analysis of the PK/PD relationship of ST-2262 in this model provides insight into the level of NaV1.7 target occupancy that may be necessary to achieve a pharmacodynamic effect. Recognizing the limited number of animals tested due to the challenge of working with non-human primates, additional work is warranted to further define the relationship between pharmacological inhibition of NaV1.7 and sensitivity to noxious thermal stimuli.
Discussion
The finding that humans lacking functional NaV1.7 exhibit an inability to experience pain raises the intriguing possibility that selective inhibitors of NaV1.7 may be potent analgesics1,2,3. In the present study, we describe the discovery and characterization of ST-2262, a selective pore blocker of hNaV1.7 advanced through rational modification of a natural small molecule toxin lead, STX. In whole cell voltage clamp recordings, ST-2262 exhibited > 200-fold selectivity for hNaV1.7 over hNaV1.1–1.6 and hNaV1.8. The selectivity of ST-2262 was not examined against hNaV1.9, a channel subtype that is difficult to express in heterologously. hNaV1.9 contains a residue in the domain I p-loop, S360, that confers resistance to STX and lacks the domain III threonine/isoleucine sequence motif that is essential for high potency of ST-2262 against hNaV1.7. Thus, inhibition of NaV1.9 by ST-2262 is unlikely42.
The properties of ST-2262 are in contrast to other preclinical and clinical inhibitors of NaV1.7, which preferentially bind to an inactivated conformation(s) of the channel52. Mutagenesis experiments indicate that specific residues in the extracellular pore of NaV1.7, including a two amino acid sequence variation in the domain III pore loop that is unique to primates, are required for ST-2262 binding to cyno- and human NaV1.731,39. These findings establish the extracellular vestibule of NaV1.7 as a viable receptor site for the design of potent and selective channel inhibitors.
Whereas congenital insensitivity to pain in humans is the result of complete and permanent NaV1.7 loss-of-function, inhibition by small molecule agents is incomplete and transient. This difference raises several important questions regarding the pharmacology of NaV1.7: (1) is transient inhibition sufficient for analgesia, (2) what level of target engagement is required for efficacy, and (3) what anatomic compartment(s) must be accessed? In light of the preliminary nature of the behavioral studies conducted with ST-2262, the present study does not yield definitive answers to these questions. Nevertheless, the finding that NHPs administered ST-2262 exhibited reduced sensitivity to noxious thermal stimuli is consistent with the view that transient inhibition of NaV1.7 is sufficient to produce analgesia45. Furthermore, recognizing that ST-2262 is a polar small molecule with low membrane permeability and therefore unlikely to reach efficacious concentrations in the CNS (analysis of CSF samples obtained during NHP experiments gave a CSF:plasma ratio of < 10–3), the observed effects on thermal withdrawal latency and ΔHR are likely the result of peripheral inhibition. Our findings, however, do not rule out an additional role for NaV1.7 at the central terminals of primary afferents or in dorsal horn neurons, as has been suggested53.
In the present study, the effect of ST-2262 on withdrawal latency to noxious heat was measured in NHPs at doses of 0.01, 0.05, 0.25 and 1.25 mg/kg IV. Doses of 0.05, 0.25 and 1.25 mg/kg resulted in unbound plasma concentrations of ST-2262 of 0.7×, 3.4× and 16× the IC50 value against cynoNaV1.7 at a time point 30 min following drug administration. Assuming a unitary Hill coefficient, which is consistent with the dose–response relationship for ST-2262 in whole cell recordings against cyno- and human NaV1.7, these unbound exposures correspond to 41%, 78% and 94% inhibition of NaV1.7, respectively. Further work to understand whether a similar relationship exists between NaV1.7 target occupancy and analgesic pharmacodynamic effects in other preclinical pain models is ongoing.
Conclusion
NaV1.7 remains a compelling target for the development of non-opioid analgesics based on evidence from human genetics and rodent knock-out studies2,3,44,45. A major challenge in the pursuit of safe and effective NaV1.7 inhibitors has been the identification of small molecules that are selective over off-target proteins, including other NaV isoforms, to achieve a suitable margin of safety. Prior efforts to develop high precision NaV1.7 inhibitors have largely focused on a class of aryl and acyl sulfonamides that bind preferentially to VSD IV and impede recovery from inactivation7. In the present study, we disclose ST-2262, a synthetic analogue of natural bis-guanidinium toxins that lodges in the extracellular vestibule of the channel (Site 1) and occludes ion passage. A preliminary PK/PD study involving intravenous administration of ST-2262 to four cynomolgus subjects demonstrated increased withdrawal latency to noxious heat. Collectively, our findings validate the extracellular mouth of the sodium channel as a tractable receptor site for selective ligand design and provide insight into the distribution and target occupancy requirements for drug efficacy mediated by inhibition of NaV1.7.
Data availability
Additional raw data are available from the corresponding author on reasonable request.
References
Dib-Hajj, S. D., Yang, Y., Black, J. A. & Waxman, S. G. The NaV1.7 sodium channel: From molecule to man. Nat. Rev. Neurosci. 14, 49–62 (2013).
Cox, J. J. et al. An SCN9A channelopathy causes congenital inability to experience pain. Nature 444, 894–898 (2006).
Goldberg, Y. et al. Loss-of-function mutations in the Nav1.7 gene underlie congenital indifference to pain in multiple human populations. Clin. Genet. 71, 311–319 (2007).
Yang, Y. et al. Mutations in SCN9A, encoding a sodium channel alpha subunit, in patients with primary erythermalgia. J. Med. Genet. 41, 171–174 (2004).
Faber, C. G. et al. Gain of function NaV1.7 mutations in idiopathic small fiber neuropathy. Ann. Neurol. 71, 26–39 (2012).
Payandeh, J. & Hackos, D. H. Selective ligands and drug discovery targeting the voltage-gated sodium channel Nav1.7. In Voltage-gated Sodium Channels: Structure, Function and Channelopathies, Vol. 246 (ed. Chahine, M.) 271–306 (Springer International Publishing, Berlin, 2018).
McKerrall, S. J. & Sutherlin, D. P. Nav1.7 inhibitors for the treatment of chronic pain. Bioorg. Med. Chem. Lett. 28, 3141–3149 (2018).
Mulcahy, J. V. et al. Challenges and opportunities for therapeutics targeting the voltage-gated sodium channel isoform NaV1.7. J. Med. Chem. https://doi.org/10.1021/acs.jmedchem.8b01906 (2019).
Ahern, C. A., Payandeh, J., Bosmans, F. & Chanda, B. The hitchhiker’s guide to the voltage-gated sodium channel galaxy. J. Gen. Physiol. 147, 1–24 (2016).
Stevens, M., Peigneur, S. & Tytgat, J. Neurotoxins and their binding areas on voltage-gated sodium channels. Front. Pharmacol. 2, 71 (2011).
Israel, M. R., Tay, B., Deuis, J. R. & Vetter, I. Sodium channels and venom peptide pharmacology. In Advances in Pharmacology, vol. 79, 67–116 (Elsevier, Amsterdam, 2017).
Bosmans, F. & Swartz, K. J. Targeting voltage sensors in sodium channels with spider toxins. Trends Pharmacol. Sci. 31, 175–182 (2010).
Wang, X. et al. Inhibitors of Ion Channels, Patent PCT/US2006/042882, 2006.
Fulp, A., Marron, B., Suto, M., J. & Wang, X. Inhibitors of Voltage-Gated Sodium Channels, Patent PCT/US2006/031390, 2006.
Kawatkar, A., S. et al. Bicyclic Deriatives as Modulators of Ion Channels, Patent PCT/US2006/017699, 2006.
McCormack, K. et al. Voltage sensor interaction site for selective small molecule inhibitors of voltage-gated sodium channels. Proc. Natl. Acad. Sci. 110, E2724–E2732 (2013).
Zhang, M.-M. et al. Cooccupancy of the outer vestibule of voltage-gated sodium channels by micro-conotoxin KIIIA and saxitoxin or tetrodotoxin. J. Neurophysiol. 104, 88–97 (2010).
Shen, H. et al. Structural basis for the modulation of voltage-gated sodium channels by animal toxins. Science 362, eaau2596 (2018).
Ahuja, S. et al. Structural basis of Nav1.7 inhibition by an isoform-selective small-molecule antagonist. Science 350, aac5464 (2015).
Alexandrou, A. J. et al. Subtype-selective small molecule inhibitors reveal a fundamental role for Nav1.7 in nociceptor electrogenesis, axonal conduction and presynaptic release. PLoS ONE 11, e0152405 (2016).
Varney, M. Roche: At the Forefront of R&D Innovation and Breakthrough Treatments. https://www.roche.com/dam/jcr:5c999124-c278-4549-8e94-4475cc741de1/en/2016_roche_cowen_presentation.pdf (2016)
Schmalhofer, W. A. et al. ProTx-II, a selective inhibitor of NaV1.7 sodium channels, blocks action potential propagation in nociceptors. Mol. Pharmacol. 74, 1476–1484 (2008).
Xiao, Y. et al. Tarantula huwentoxin-IV inhibits neuronal sodium channels by binding to receptor site 4 and trapping the domain II voltage sensor in the closed configuration. J. Biol. Chem. 283, 27300–27313 (2008).
Deuis, J. R. et al. Pharmacological characterisation of the highly NaV1.7 selective spider venom peptide Pn3a. Sci. Rep. 7, 40883 (2017).
Moyer, B. D. et al. Pharmacological characterization of potent and selective NaV1.7 inhibitors engineered from Chilobrachys jingzhao tarantula venom peptide JzTx-V. PLoS ONE 13, e0196791 (2018).
Flinspach, M. et al. Insensitivity to pain induced by a potent selective closed-state Nav1.7 inhibitor. Sci. Rep. 7, 39662 (2017).
McKerrall, S. J. et al. Structure- and ligand-based discovery of chromane arylsulfonamide Nav1.7 inhibitors for the treatment of chronic pain. J. Med. Chem. 62, 4091–4109 (2019).
Graceffa, R. F. et al. Sulfonamides as selective NaV1.7 inhibitors: Optimizing potency, pharmacokinetics, and metabolic properties to obtain atropisomeric quinolinone (AM-0466) that affords robust in vivo activity. J. Med. Chem. 60, 5990–6017 (2017).
McDonnell, A. et al. Efficacy of the Nav1.7 blocker PF-05089771 in a randomised, placebo-controlled, double-blind clinical study in subjects with painful diabetic peripheral neuropathy. Pain 159, 1465–1476 (2018).
Rothenberg, M. E. et al. Safety, tolerability, and pharmacokinetics of GDC-0276, a novel NaV1.7 inhibitor, in a first-in-human, single- and multiple-dose study in healthy volunteers. Clin. Drug Investig. https://doi.org/10.1007/s40261-019-00807-3 (2019).
Walker, J. R. et al. Marked difference in saxitoxin and tetrodotoxin affinity for the human nociceptive voltage-gated sodium channel (NaV1.7). Proc. Natl. Acad. Sci. USA 109, 18102–18107 (2012).
Thomas-Tran, R. & Du Bois, J. Mutant cycle analysis with modified saxitoxins reveals specific interactions critical to attaining high-affinity inhibition of hNaV1.7. Proc. Natl. Acad. Sci. USA 113, 5856–5861 (2016).
Tsukamoto, T. et al. Differential binding of tetrodotoxin and its derivatives to voltage-sensitive sodium channel subtypes (Nav1.1 to Nav1.7). Br. J. Pharmacol. 174, 3881–3892 (2017).
Fleming, J. J., McReynolds, M. D. & Du Bois, J. (+)-saxitoxin: A first and second generation stereoselective synthesis. J. Am. Chem. Soc. 129, 9964–9975 (2007).
Mulcahy, J. V., Walker, J. R., Merit, J. E., Whitehead, A. & Du Bois, J. Synthesis of the paralytic shellfish poisons (+)-gonyautoxin 2, (+)-Gonyautoxin 3, and (+)-11,11-dihydroxysaxitoxin. J. Am. Chem. Soc. 138, 5994–6001 (2016).
Andresen, B. M. & Du Bois, J. De novo synthesis of modified saxitoxins for sodium ion channel study. J. Am. Chem. Soc. 131, 12524–12525 (2009).
Walker, J. R., Merit, J. E., Thomas-Tran, R., Tang, D. T. Y. & Du Bois, J. Divergent synthesis of natural derivatives of (+)-saxitoxin including 11-saxitoxinethanoic acid. Angew. Chem. Int. Ed. Engl. 58, 1689–1693 (2019).
Lipkind, G. M. & Fozzard, H. A. A structural model of the tetrodotoxin and saxitoxin binding site of the Na+ channel. Biophys. J. 66, 1–13 (1994).
Penzotti, J. L., Fozzard, H. A., Lipkind, G. M. & Dudley, S. C. Differences in saxitoxin and tetrodotoxin binding revealed by mutagenesis of the Na+ channel outer vestibule. Biophys. J. 75, 2647–2657 (1998).
Tikhonov, D. B. & Zhorov, B. S. Modeling P-loops domain of sodium channel: Homology with potassium channels and interaction with ligands. Biophys. J. 88, 184–197 (2005).
Shen, H., Liu, D., Wu, K., Lei, J. & Yan, N. Structures of human NaV1.7 channel in complex with auxiliary subunits and animal toxins. Science 363, 1303–1308 (2019).
Goral, R. O., Leipold, E., Nematian-Ardestani, E. & Heinemann, S. H. Heterologous expression of NaV1.9 chimeras in various cell systems. Pflugers Arch. 467, 2423–2435 (2015).
Satin, J. et al. A mutant of TTX-resistant cardiac sodium channels with TTX-sensitive properties. Science 256, 1202–1205 (1992).
Gingras, J. et al. Global Nav1.7 knockout mice recapitulate the phenotype of human congenital indifference to pain. PLoS ONE 9, e105895 (2014).
Shields, S. D. et al. Insensitivity to pain upon adult-onset deletion of Nav1.7 or its blockade with selective inhibitors. J. Neurosci. 38, 10180–10201 (2018).
Minett, M. S. et al. Distinct Nav1.7-dependent pain sensations require different sets of sensory and sympathetic neurons. Nat. Commun. 3, 791 (2012).
Yeomans, D. C. et al. Recombinant herpes vector-mediated analgesia in a primate model of hyperalgesia. Mol. Ther. 13, 589–597 (2006).
Cooper, B. Y., Vierck, C. J. & Yeomans, D. C. Selective reduction of second pain sensations by systemic morphine in humans. Pain 24, 93–116 (1986).
Tzabazis, A. Z. et al. Selective nociceptor activation in volunteers by infrared diode laser. Mol. Pain 7, 18 (2011).
Yeomans, D. C., Pirec, V. & Proudfit, H. K. Nociceptive responses to high and low rates of noxious cutaneous heating are mediated by different nociceptors in the rat: behavioral evidence. Pain 68, 133–140 (1996).
Loggia, M. L., Juneau, M. & Bushnell, C. M. Autonomic responses to heat pain: Heart rate, skin conductance, and their relation to verbal ratings and stimulus intensity. Pain 152, 592–598 (2011).
Theile, J. W., Fuller, M. D. & Chapman, M. L. The selective Nav1.7 inhibitor, PF-05089771, interacts equivalently with fast and slow inactivated Nav1..7 channels. Mol. Pharmacol. 90, 540–548 (2016).
Alles, S. R. A. et al. Sensory neuron-derived NaV1.7 contributes to dorsal horn neuron excitability. Sci. Adv. 6, eaax4568 (2020).
Acknowledgements
Research reported in this publication was supported in part (60%) by an award to SiteOne Therapeutics from the National Institute of Neurological Disorders and Stroke of the National Institutes of Health under award number R44NS081887 and by the National Institutes of Health R01 GM117263-01A1 (JDB). HSH is supported by the Department of Defense (DoD) through the National Defense Science & Engineering Graduate (NDSEG) Fellowship Program and is a fellow of the Center for Molecular Analysis and Design (CMAD) at Stanford University. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Christine O’Rourke, DVM, DACLAM and the Montana State Animal Resource Center are gratefully acknowledged for assistance with animal studies.
Author information
Authors and Affiliations
Contributions
J.V.M., J.D.B., D.C.Y., H.P., and A.D. conceived of the study. H.P., J.T.B., A.D., H.S.H., G.L., D.M., X.Z., J.L., S.A., B.D.M., D.C.Y. and J.V.M. designed and performed experiments. J.T.B. and J.V.M. drafted the manuscript. J.D.B., D.C.Y., A.D. and B.D.M. critically revised the manuscript. All authors reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
H.P., J.T.B., A.D., G.L., D.M., X.Z. and J.V.M. are employees of and shareholders in SiteOne Therapeutics. D.C.Y. and J.D.B. are advisors to and shareholders in SiteOne Therapeutics.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pajouhesh, H., Beckley, J.T., Delwig, A. et al. Discovery of a selective, state-independent inhibitor of NaV1.7 by modification of guanidinium toxins. Sci Rep 10, 14791 (2020). https://doi.org/10.1038/s41598-020-71135-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-71135-2
This article is cited by
-
Structure of human NaV1.6 channel reveals Na+ selectivity and pore blockade by 4,9-anhydro-tetrodotoxin
Nature Communications (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.