Abstract
Study design
Cross-sectional study
Objectives
To identify the prevalence of posttraumatic stress disorder (PTSD) among the individuals with traumatic spinal cord injury (TSCI) and to examine the relationships between demographic and clinical characteristics, and PTSD.
Setting
Spinal Injury Rehabilitation Center (SIRC) and Dhulikhel Hospital, Kathmandu University Hospital (DH, KUH), Kavrepalanchowk, Nepal.
Methods
Individuals above 18 years of age with TSCI of at least one month from trauma and admitted to SIRC and DH, KUH from June 2019 to May 2021 were included. The specific stress version of the PostTraumatic Stress Disorder Checklist (PCL), was utilized. To classify the neurological status of TSCI individuals, International Standard for Neurological Classification of Spinal Cord Injury (ISNCSCI) was used. Hierarchical multiple regression analysis between independent variables and normalized PCL score was done to evaluate the predictors of PTSD.
Results
Among 163 patients, the overall prevalence of PTSD was 27%, and the mean PCL score was 36 ± 13.9. Factors predictive of PTSD included gender, family type, ethnicity, and literacy rate. No significant association was found between the clinical characteristics and PTSD.
Conclusions
PTSD appears to be considerably prevalent among individuals with TSCI in Nepal. Females, individuals from nuclear families, individuals with lower literacy, and individuals from lower caste are significantly vulnerable to developing PTSD. However, clinical characteristics do not appear to be influential in the development of PTSD.
Similar content being viewed by others
Introduction
Traumatic spinal cord injury (TSCI) is associated with posttraumatic stress disorder (PTSD) [1,2,3]. According to the WHO, about 10% of the population in the world is facing mental health disorders, with even higher prevalence in the population with SCI [4]. The prevalence is reported in the range of 10 to 40% among individuals with SCI [5]. Delay in diagnosing PTSD can cause long-term consequences such as inability to return to work and increased health care and economic burden [6]; therefore, prompt recognition and treatment of PTSD among individuals with TSCI are of utmost importance.
Posttraumatic stress disorder, described in 1980 [7], is defined as a mental health condition caused by actual or threatened death or serious injury, or other threat to a person’s physical integrity. The symptomatic aftermath includes 17 symptoms divided among three symptom clusters, namely re-experience, avoidance/numbing, and arousal [8]. These symptoms should be present for more than 1 month, and the disturbance must cause clinically significant distress or impairment in social, occupational, or other important areas of functioning [8].
Studies on TSCI and PTSD exist in a sizable number. As shown in these studies, there is a higher prevalence and incidence of SCI among male individuals but females are at higher risk of developing PTSD [1]. Studies have also revealed various demographic factors like younger age at the time of event, being single, illiteracy and economic instability are associated with more PTSD symptoms in persons with SCI [4]. Evidences also suggest that various circumstances under which TSCIs occur are related to increased symptoms of acute and posttraumatic stress in such populations [9, 10]. In a study by Starr et al. 43–57% of patients with orthopedic injuries due to falls and road traffic injuries (RTIs) met the criteria for PTSD 1 year after injury [11]. According to a recent study in Nepal, the two major etiologies of spinal cord injury are fall from height (60%) and RTIs (17%), predominantly common in the age between 32 to 47 years, which highlights the possibility of high prevalence of PTSD among individuals with TSCI [12].
There are a very few studies reporting prevalence of PTSD in SCI individuals from a low or middle income country. In the recent systematic review of risk and vulnerability factors for PTSD among SCI individuals by Pollock et al. there were no studies from low income countries and from Asia which highlights the absence of similar studies from these regions [9]. Nepal is a lower-middle income country with multi-dimensionally poor population being 4.9 million people (17.4% of total population) [13]. Hence, this study would be important in highlighting the prevalence of PTSD in a unique population of Nepal on which similar study has not been done in the past. This study aims to evaluate the prevalence of PTSD among individuals with TSCI presenting to a tertiary care center or rehabilitation center, and assess the role of demographic and clinical characteristics in the development of PTSD in Nepal. Recognition of these factors will be helpful to identify and support individuals at higher risk of PTSD as early as possible.
Materials and methods
Study design and site
This is a prospective cross-sectional study done in Dhulikhel hospital, Kathmandu University Hospital (DH, KUH) and Spinal Injury Rehabilitation Center (SIRC), Sanga, Nepal. DH, KUH is a tertiary care center which is a major referral center for patients with spinal injuries. SIRC is a non-profit, inpatient rehabilitation center for individuals with spinal injury located in central Nepal which also provides peer counseling and psychology services as a part of standard care. It is the major referral center for spinal rehabilitation in Nepal.
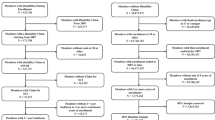
Inclusion criteria
All the individuals above 18 years of age with SCI of at least one month from trauma who were admitted in DH, KUH or SIRC from June 2019 to May 2021 were included in the study. However, individuals not consenting for the study; individuals with memory loss and cognitive dysfunction and; non-traumatic SCI were excluded.
Ethical clearance, tools and sample size calculation
Ethical clearance was obtained from Institutional Review Committee (IRC) of Kathmandu University School of Medical Sciences (KUSMS) [IRC-KUSMS approval number: 270/2021]. We utilized the specific stress version of the Post- Traumatic Stress Disorder Checklist (PCL), a 17-item self-report instrument corresponding to DSM-IV criteria (American Psychiatric Association, 1994) for PTSD, which has been translated and validated in Nepali language [14]. DSM-IV-TR criteria for PTSD includes a history of exposure to a traumatic event and symptoms from each of three subscale, namely re-experiences, avoidant, and arousal symptoms. The mean of the subscale was used to impute the missing values if only 1 item was missing. A dichotomous variable was created (PTSD, yes or no) using the following DSM-IV criteria: (a) at least 1 re-experience item, (b) at least 3 avoidance items, and (c) at least 2 arousal items. A standard total score of >44 [6] was used as an alternative to diagnose an individual with PTSD. To classify the neurological status of SCI individuals, International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) was used [15].
The sample size was calculated using a sample size formula for cross-sectional studies [16]. After assuming the level of confidence of the study of 95%, precision of 0.05 and expected prevalence of PTSD among traumatic spinal injured patients of 10%, the calculated sample size was 138 patients. Most individuals filled out the PCL by themselves, while those needing assistance were interviewed either by trained physiotherapists or by the treating doctor.
Statistical analysis
The collected data were entered and analyzed using IBM SPSS version 25.0 for Windows (SPSS Inc., Chicago, IL, USA). Normality of continuous variables was checked using the Shapiro-Wilk test. The continuous variables with normal distribution were presented as mean ± SD and non-normal variables were reported as median (interquartile range [IQR]). The total PCL score was converted into normal distribution by firstly transforming the total score into a percentile rank (resulting in uniformly distributed probabilities) and secondly the inverse-normal transformation to the results of first step was done to form a variable consisting of normally distributed z-scores [17]. We refer to this variable as the normalized PCL (N-PCL) score. Spearman correlation test was done for analyzing the correlation between independent variables and N-PCL score. One way analysis of variance (ANOVA) was used to evaluate the significance between the mean injury to interview time between individuals with and without disability card.
Hierarchical multiple regression analysis between independent variables and N-PCL score was done to evaluate the predictors of PTSD. Independent variables showing statistical significance with N-PCL score (Spearman’s correlation) in this study, and the variables that were found significant in previous literature were selected for hierarchical regression analysis. After controlling for participants’ gender in the first step, the main effect of social factors (social group, family type and educational status) was tested in the second step. In the third step, the main effect of trauma related factors (delay from injury to treatment, tetra/paraplegic status, and presence/absence of disability card) were tested. Delay from injury to treatment was defined as the time required for the patient to reach the tertiary care center from the time of traumatic event. Tetraplegia and paraplegia included motor complete patients in all the limbs or only the lower limbs respectively (AIS A and B). Issue of multi-collinearity was addressed by calculating the variance inflation factor (VIF). The VIF of all the included independent variables was less than 2. A value of P < 0.05 was considered significant.
Results
Demographics
A total of 163 individuals were included in the study. The majority (75.5%) were males with a mean age of 36.3 ± 12.4 years. Eighty-three (51.0%) patients were from joint families (family with more than two generations living together) and nearly 80% were married. Most of the participants (92.6%) had no regular income. Eighty-seven percent of patients were Hindu by religion and 18% had no formal education (Table 1).
Clinical characteristics
The most common SCI etiology was fall (72.4%) followed by road traffic accident (23.3%). Among the patients, five (3.1%) reported to have lost their relatives during the traumatic incident. The most common level of injury was T10. Majority of the patients were ASIA Impairment Scale (AIS) A (57.7%) followed by AIS C (18.4%). Using International Standard for Neurological Classification of Spinal Cord Injury (ISNCSCI), it was found that majority (64%) of the patients had T1-S4/5 injury with AIS A, B or C followed by 13.4% patients with C1–C4 injury with AIS A, B or C. Among the patients with AIS A and AIS B, 89 patients (54.6% of total) were paraplegic and 22 patients (13.5% of total) were tetraplegic; among them, only 22 (13.6%) patients had disability card, which is an identity card given by Government of Nepal (GoN) to the individuals with SCI. The mean injury to interview time was 84.7 ± 33.6 days. There was a statistically significant difference (One way ANOVA; F-value: 18.5, p < 0.01) between the mean injury to interview time between the individuals with disability card (111.9 ± 22 days) and without disability card (80.4 ± 33.5 days).The participants’ demographic and clinical characteristics along with their mean PCL scores are presented in Table 1.
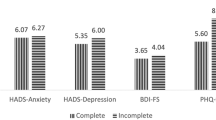
Table 1 shows a statistically significant correlation of N-PCL score with gender, education and presence of disability card. Female gender, lower education levels, and presence of a disability card were associated with higher N-PCL scores.
PTSD prevalence and predictors
The median total score of PCL was 34 (24–45) (mean = 36 ± 13.9), with 27% patients meeting the criteria for PTSD (Total score >44). The subscale medians were 11(8–17) (mean = 12.45 ± 5.3) for re-experience, 13(9–17) (mean = 13.5 ± 5.3) for avoidance, and 9(6–13) (mean = 10 ± 4.8) for arousal. The percentage of individuals diagnosed with PTSD according to DSM-IV criteria was 25.2%.
In response to the symptoms of persistent re-experience, 29.4% (mean = 3.06 ± 1.5), 23.3% (mean = 2.87 ± 1.49), and 24.5% (mean = 2.79 ± 1.56) reported to have been often bothered by memories of the event, upsetting dreams about event, and sudden experience of the event again, respectively. Of the symptoms of persistent avoidance, ‘lost interest in usual activities’ and ‘been less optimistic about future,’ was often reported by 22.1% and 18.4%, respectively. The mean and median of subscales of the PLC score of individuals with SCI are presented in Table 2.
The hierarchical multiple regression analysis is shown in Table 3 and the model summary in Table 4.
The analysis revealed that at step one, gender contributed significantly to the regression model (Female gender predicting higher N-PCL score), F (1, 99) = 11.32, p < 0.05) and accounted for 10.3% of the variation in N-PCL score (Table 4). Introducing the social factors (social group, family type and educational status) explained an additional 11.6% of variation in N-PCL score (lower social group, nuclear family type, and lower educational status predicting higher N-PCL score) and this change in R² was significant, F (3, 96) = 12.6, p < 0.001 (Table 4). All the four variables significantly predicted the N-PCL score with female gender and lower educational status being the most predicting variables (p < 0.001) (Table 3). However, adding trauma related factors (delay from injury to treatment, tetra/paraplegic status, and presence/absence of disability card) to the regression model explained only an additional 1.7% of the variation in N-PCL score and this change in R² was not significant, F (3,93) = 12.75, p = 0.57 (Table 4).
Discussion
Examining the prevalence of PTSD among individuals with TSCI, our study found more than one fourth (27%) meeting the diagnostic criteria. The percentage diagnosed with PTSD according to DSM-IV criteria was slightly lower, that is, 25.2%. In comparison to other studies e.g., Agar et al. [18] (24%), Craig et al. [4] (27%), Cao et al. [19] (24.9%), the reported prevalence in the present study is very similar. This suggests that Nepalese individuals with TSCI may have similar psychological coping mechanisms to trauma compared to individuals with TSCI in the other parts of the world. However, in the study done by Warren et al. the prevalence of PTSD in individuals with TSCI was 52% [20], which is noticeably higher. This discrepancy in the prevalence may be due to a smaller sample size (N = 24) in the study by Warren et al. thereby making this study less generalizable.
Gender was a significant predictor of PTSD in our study with a higher prevalence of PTSD among females (35%) compared to males (22%). This finding is similar to the studies by Otis et al. [1] and Hatcher et al. [10]. Though males are more likely to experience a potentially traumatic event than females, the female: male ratio in the prevalence of PTSD is approximately 2:1 [21]. This finding is also reiterated by a study that reported a higher level of re-experiencing, avoidance and arousal symptoms among females [22]. Higher prevalence of PTSD among females may be explained by the fact that they experience higher levels of associated pre-traumatic, peri-traumatic and posttraumatic risk factors compared to males [21].
Type of family was another significant predictor of PTSD in our study. Patients living in joint families had significantly lower chances (24%) of developing PTSD compared to patients living in nuclear families (47%). This is similar to the findings by Farooq et al. who had studied the prevalence of PTSD among earthquake survivors in Kashmir, Pakistan [23]. Similarly, Yuchang et al. found the prevalence of PTSD among 2010 earthquake survivors living in joint family was 3.8% compared to 67% among survivors living in nuclear family [24]. A joint family system may have acted as an important source of support to the individuals in the face of various adversities.
In Nepal, caste system, which was the practice during the feudal system based on the people’s profession, is still prevalent in many parts of the country. Consequently, individuals of lower caste face social discrimination. Our study showed a higher prevalence of PTSD among SCI individuals from lower castes; and in the absence of other comparable studies, the finding of this study may be noble in the Nepali context. However, in the study by Hatori et al. where PTSD was evaluated among 2015 earthquake survivors of Kathmandu, Nepal, a higher prevalence of PTSD was found among the lower caste individuals [25]. This finding could be due to the social discrimination faced by the lower caste individuals.
Literacy rate was another significant predictor of PTSD in our study. Individuals with lower literacy had higher prevalence of PTSD. This is similar to the finding by Kuiper et al. where individuals having higher PTSD symptoms were from primary/lower education background than with higher education [26]. Similarly, Tang et al., found lower educational status predicting higher prevalence of PTSD among adult earthquake survivors [27]. Individuals with higher levels of education may have greater social resources and broader coping methods which may lessen the impact of traumatic events compared to individuals with lesser educational status.
Another factor worth mentioning is the relationship of income with the occurrence of PTSD. Our study showed higher PCL score (suggesting higher prevalence of PTSD) in individuals with regular income compared to individuals with no regular income. This is in contrast to the study by Visser et al. who have shown higher prevalence of PTSD in individuals with lower income [28]. In Nepal, individuals with a regular income are probably the major responsibility bearers and the only income generators in their family. In a lack of proper social and financial security, TSCI to such patients can cause a severe financial crisis in the family. This may add up to the stress contributing to higher PTSD prevalence in such individuals.
Regarding the relationship of the clinical characteristics with PTSD, no significant association was found. Studies have suggested that individuals experiencing assaultive violence are at greater risk of PTSD [29]. However, all the individuals in our study had non assaultive trauma which may be the reason for the type of trauma not predicting the prevalence of PTSD among individuals with TSCI. Our study showed no correlation between relative loss and PTSD, though available studies have shown a strong relationship between them [28]. This may be due to a smaller number of individuals with relative loss (3.1%) making statistical comparison non-significant. Severity of neurological impairment and tetra/ paraplegia also did not show any correlation with PTSD prevalence among individuals with TSCI. Though presence or absence of disability card did not predict the occurrence of PTSD as per the hierarchical multiple regression analysis, the difference in the mean injury to interview time between the two groups was statistically significant with patients with disability card having longer injury to interview time. The mean PCL score for the individuals with disability card was also higher signifying higher occurrence of PTSD. The explanation for higher occurrence of PTSD among individuals with disability card could be related to a longer injury to interview time among them which suggests the possible delay in treatment and rehabilitation leading to higher PCL score.
One of the limitations in this study was the information about the PTSD stressors and the experience of traumatic events before the incidence of SCI of all the individuals were not taken. This could have created a confounding bias in the prevalence of PTSD among SCI individuals. Similarly, those individuals who were interviewed either by trained physiotherapists or by the treating doctor, there is a probability of occurrence of observer bias and/or interviewer bias. However, due to the same approach of data collection, response bias could be eliminated. In the context like Nepal, where the respondents are not educated formally, and thus have very limited knowledge of their problems, the use of self-reported measures would not yield the appropriate data. Further, this study being a cross- sectional study, it may also be difficult to derive a causal relationship between SCI and PTSD due to only a one-time measurement of PCL score.
In conclusion, PTSD appears to be considerably prevalent among individuals with TSCI. Females, individuals from nuclear families, individuals with lower literacy, and individuals from lower caste are significantly vulnerable to developing PTSD. However, clinical characteristics do not appear to be influential in the development of PTSD. It can be recommended that personal variables need to be examined closely in the identification of individuals at higher risk for PTSD for the purpose of early detection and treatment.
Data availability
The data set used in this study can be obtained from the corresponding author on request.
References
Otis C, Marchand A, Courtois F. Risk factors for posttraumatic stress disorder in persons with spinal cord injury. Top Spinal Cord Inj Rehabil. 2012;18:253–63.
Wengel PVT, De Haan Y, Feller RE, Oner FC, Vandertop WP. Complete traumatic spinal cord injury: current insights regarding timing of surgery and level of injury. Glob Spine J. 2020;10:324–31.
Ning G-Z, Wu Q, Li Y-L, Feng S-Q. Epidemiology of traumatic spinal cord injury in Asia: a systematic review. J spinal cord Med. 2012;35:229–39.
Craig A, Tran Y, Middleton J. Psychological morbidity and spinal cord injury: a systematic review. Spinal Cord. 2009;47:108–14.
Li J, Reinhardt JD, Feng X. Physical function, post-traumatic stress disorder, and quality of life in persons with spinal cord injury caused by the Wenchuan earthquake versus nondisaster trauma: a cross-sectional modeling study. Spinal Cord. 2020;58:616–25.
Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL). Behav Res Ther. 1996;34:669–73.
Corvalan JC, Klein D. PTSD: diagnosis, evolution, and treatment of combat-related psychological/psychiatric injury. Mo Med. 2011;108:296.
Courtois CA, Brown LS, Cook J, Fairbank JA, Friedman M, Gone JP, et al. Clinical Practice Guideline for the Treatment of Post-traumatic stress disorder (PTSD): American Psychological Association (APA); 2017. https://www.apa.org/ptsd-guideline/ptsd.pdf.
Pollock K, Dorstyn D, Butt L, Prentice S. Posttraumatic stress following spinal cord injury: a systematic review of risk and vulnerability factors. Spinal Cord. 2017;55:800–11.
Hatcher MB, Whitaker C, Karl A. What predicts post‐traumatic stress following spinal cord injury. Br J Health Psychol. 2009;14:541–61.
Starr AJ, Smith WR, Frawley WH, Borer DS, Morgan SJ, Reinert CM, et al. Symptoms of posttraumatic stress disorder after orthopaedic trauma. JBJS. 2004;86:1115–21.
Parajuli B, Acharya K, Shrestha D. Epidemiology of traumatic spinal cord injury in Nepal: A systematic review. Asian Med Sci. 2020;11:121–8.
National Planning Commission GON. Nepal Multidimensional Poverty Index: Analysis towards action. 2021. https://www.unicef.org/nepal/media/14346/file/MPI_Report_2021.pdf.
Muldoon OT, Acharya K, Jay S, Adhikari K, Pettigrew J, Lowe RD. Community identity and collective efficacy: A social cure for traumatic stress in post‐earthquake Nepal. Eur J Soc Psychol. 2017;47:904–15.
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med. 2011;34:535–46.
Charan J, Biswas T. How to calculate sample size for different study designs in medical research? Indian J Psychol Med. 2013;35:121.
Templeton GF. A two-step approach for transforming continuous variables to normal: implications and recommendations for IS research. Commun Assoc Inf Syst. 2011;28:4.
Agar E, Kennedy P, King NS. The role of negative cognitive appraisals in PTSD symptoms following spinal cord injuries. Behav Cogn Psychother 2006;34:437–52.
Cao Y, Li C, Newman S, Lucas J, Charlifue S, Krause JS. Posttraumatic stress disorder after spinal cord injury. Rehabil Psychol. 2017;62:178.
Warren AM, Reynolds M, Driver S, Bennett M, Sikka S. Posttraumatic stress symptoms among spinal cord injury patients in trauma: a brief report. Top Spinal Cord Inj Rehabil. 2016;22:203–8.
Christiansen DM, Hansen M. Accounting for sex differences in PTSD: A multi-variable mediation model. Eur J Psychotraumatol 2015;6:26068.
Ditlevsen DN, Elklit A. The combined effect of gender and age on post traumatic stress disorder: do men and women show differences in the lifespan distribution of the disorder? Ann Gen Psychiatry 2010;9:1–12.
Naeem F, Ayub M, Masood K, Gul H, Khalid M, Farrukh A, et al. Prevalence and psychosocial risk factors of PTSD: 18 months after Kashmir earthquake in Pakistan. J Affect Disord. 2011;130:268–74.
Jin Y, Wang G. Individual risk factors for PTSD in adolescents from the 2010 earthquake in Yushu: The predictor effect of rumination. Afr J Psychiatry 2014;17:1000144.
Hatori T, Bhandary NP. Posttraumatic stress disorder and its predictors in Kathmandu Valley residents after the 2015 Nepal Earthquake. Int J Disaster Risk Reduct 2022;69:102733.
Kuiper H, van Leeuwen C, Kopsky DJ, Stolwijk-Swüste JM, Post MWM. Post-traumatic stress disorder symptoms and pain intensity in persons with spinal cord injury. Spinal Cord. 2021;59:328–35.
Tang B, Deng Q, Glik D, Dong J, Zhang L. A meta-analysis of risk factors for post-traumatic stress disorder (PTSD) in adults and children after earthquakes. Int J Environ Res Public Health. 2017;14:1537.
Visser E, Gosens T, Den Oudsten BL, De Vries J. The course, prediction, and treatment of acute and posttraumatic stress in trauma patients: a systematic review. J Trauma Acute Care Surg. 2017;82:1158–83.
Breslau N. The epidemiology of posttraumatic stress disorder: what is the extent of the problem? J Clin Psychiatry. 2001;62:16–22.
Funding
University Grants Commission, Nepal, Funding ID: FRG-75/76-HS-16.
Author information
Authors and Affiliations
Contributions
Conception and design of study is done by BP, and KA; acquisition of data is done by BP, JS, RS and MM; and, analysis and interpretation of data is done by BP, KA, CCG, and RD. BP, KA, CCG, RD. JS, RS and MM are involved in drafting the paper. Revision of the paper critically for important intellectual content is done by BP, KA and CCG. All the authors approve the final version of the paper to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
Ethical approval was obtained from Institutional Review Committee (IRC) of Kathmandu University School of Medical Sciences (KUSMS) [IRC-KUSMS approval number: 270/2021].
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Parajuli, B., Acharya, K., Grooves, C.C. et al. Post-traumatic stress disorder among individuals with traumatic spinal cord injury in Nepal: a cross-sectional study. Spinal Cord Ser Cases 9, 13 (2023). https://doi.org/10.1038/s41394-023-00566-6
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-023-00566-6