Abstract
Study design
Descriptive study.
Objectives
The study’s main objective was to describe the common targets of phenol neurolysis and review the safety and efficacy of the dose used for this spasticity management procedure in people with spinal cord injury (SCI).
Setting
An acute rehabilitation hospital.
Methods
Data from people with SCI who underwent phenol neurolysis procedures for spasticity management between April 2017 and August 2018 were included in this study. We collected demographics and phenol neurolysis procedure-related information.
Results
A total of 66 people with SCI and spasticity underwent phenol neurolysis of 303 nerves over 102 encounters. During these encounters, 97% of procedures were performed using both electrical stimulation and ultrasound guidance. The median (IQR) total volume of 6% aqueous phenol used per encounter was 4.0 (2.0–6.0) ml with a median (IQR) of 1.5 (1.0–2.3) ml per nerve. The most frequent target was the obturator nerve (33%), followed by the pectoral nerves (23%). Immediate post-phenol neurolysis improvement or reduction in spasticity was reported for 92% of all documented encounters. There was no documentation of any post-procedure-related adverse events in this cohort during this specified time frame.
Conclusions
Our findings suggest that phenol neurolysis can be safely used to manage spasticity in people with SCI under combined electrical stimulation and ultrasound guidance. Further research is required to assess the procedure’s safety, efficacy, and cost-effectiveness on patient-reported outcomes compared to other spasticity interventions.
Similar content being viewed by others
Introduction
Spasticity is a complication following an upper motor neuron injury and a major cause of disability seen in many conditions, including spinal cord injury (SCI). The prevalence of spasticity is up to 78% in people with SCI, and the presence of problematic spasticity requiring therapeutic interventions is seen in up to 49% of people with SCI [1, 2]. The definition of spasticity has evolved to include an umbrella of clinical signs and symptoms seen in various disease processes involving injury to upper motor neurons such as multiple sclerosis, stroke, brain injury, and spinal cord injury [3]. In recent years, spasticity has been defined as disordered sensorimotor control resulting from an upper motor lesion, presenting as intermittent or sustained involuntary activation of muscles resulting in an increase in tonic stretch reflexes (muscle tone), exaggerated tendon jerks, clonus, and spasms [4, 5]. Poorly controlled severe spasticity after SCI can result in multiple complications, including joint contractures, inability to participate in therapy, skin breakdown, decreased function, poor sleep, and poor quality of life [6,7,8,9].
The available therapeutic modalities for spasticity management include stretching, electrical stimulation, vibration, splinting, casting, braces, oral muscle relaxants, botulinum toxin injections, chemical neurolysis with phenol or alcohol, and intrathecal baclofen pump. The first-line treatment options for the management of focal spasticity are botulinum toxin injections, chemical neurolysis with phenol or alcohol and microsurgical selective peripheral neurotomy [10,11,12,13,14,15]. Phenol is a cost-effective option for treating spasticity compared to botulinum toxin injections and microsurgical procedures [11]. Despite this difference in cost, phenol is not used widely for spasticity management due to concerns for adverse effects such as loss of sensation and dysesthesias [10, 16]. Additionally, compared to botulinum toxin injections, the localization of target nerves for neurolysis could be technically challenging and requires advanced training and experience [11].
Phenol is typically used in 5–6% concentration for spasticity management, and at a concentration of 5% and above, phenol denatures protein resulting in axonal degeneration [17,18,19]. The effects of neurolysis last longer with 5–6% concentration. Phenol at <3% concentration causes demyelination and some axonal destruction, resulting in shorter-lasting effects compared to a 5–6% concentration [20]. The immediate local anesthetic effects of phenol result in instant spasticity relief [21, 22]. However, long-term and full effects may take 7–9 days after injections due to the time required for axonal degeneration, which may last 3–9 months depending on the target nerve (e.g., main nerve versus motor branch) and skill [22,23,24].
There are various case reports, case series, and retrospective studies reporting the utility of phenol or alcohol neurolysis in various conditions affecting upper motor neurons [20, 25,26,27,28,29]. However, literature on the utility of phenol neurolysis in people with spinal cord injury remains scarce. There are different characteristics in spasticity among various etiologies. This may lead to etiology-specific distributions of target nerves and phenol dosing. Therefore, we conducted a retrospective descriptive study of people with SCI and spasticity who received phenol neurolysis to manage spasticity. The study’s main objective was to describe the common targets of phenol neurolysis and review the safety and efficacy of the currently used dose and procedure for spasticity in people with SCI.
Methods
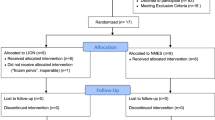
A single-center retrospective chart review was conducted to identify patients with spinal cord injury who underwent phenol neurolysis between April 2017 to August 2018 for the management of spasticity. This study was approved by the Institutional Review Board of the University of Texas Health Science Center at Houston.
Patients with SCI undergoing at least one phenol neurolysis procedure in inpatient or outpatient settings were included. The patient list was obtained from billing encounters using the current procedure codes (CPT), followed by the SCI diagnosis codes. The list was reviewed by two investigators to identify people with spinal cord injury. Data were collected by two investigators and audited by another investigator for accuracy. Data collection included demographics, neurological level of injury, the American Spinal Injury Association (ASIA) impairment scale (AIS), procedure setting, and guidance used. It included procedure-specific details such as targeted nerves or motor branches, the volume of phenol used, and effectiveness assessment following injection. Concomitant use of anti-spasticity oral medications, botulinum toxin injections, and intrathecal baclofen pump therapy at the clinical encounter was also recorded. Procedure-related data was gathered from procedure notes. Demographics data, SCI details, pre-post spasticity assessment, and adverse events related to the procedure, including pain, dysesthesias, swelling, loss of sensation, and pneumothorax while injecting pectoral nerves, were collected from the electronic medical records.
Descriptive analyses were performed to present baseline demographics and injection details. If normally distributed, continuous data were presented with mean and standard deviations (SD); otherwise, median and interquartile ranges (IQR) were reported. Totals, frequencies, and percentages were used to report categorical data.
To evaluate the effectiveness of phenol neurolysis for treating shoulder adductor and hip adductor spasticity, we assessed differences in the Modified Ashworth Scale (MAS) for these muscle groups before and up to 3 months after the procedure. These scores were extracted from clinic notes performed by treating physicians before and after neurolysis. The evaluation of MAS was performed by the treating physician. The Modified Ashworth Scale quantifies spasticity using a scale ranging from 0, 1, 1+, 2, 3, and 4 with a higher number indicative of increased severity. The scale was converted to the following numerical values: 0, 1, 2, 3, 4, 5 for calculating the change in score and reporting the baseline score. The converted scale was reported as converted MAS scale in the results section.
Results
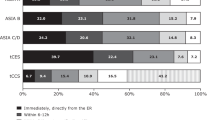
Patient demographics and injury characteristics
A total of 105 patients underwent phenol neurolysis in our institution between April 2017 to August 2018. Among these, 66 patients with SCI were included in this study, and 39 subjects with non-SCI diagnoses were excluded. There were 70% males with a mean (SD) age of 50 [17] years (Table 1). The etiology of SCI for most patients (88%) was traumatic and cervical level (61%) of injury was most common. Among cervical traumatic SCI, the majority of the people in the study had a neurological level of C1–C4 and AIS A–C impairment (Table 1). For the 12% non-traumatic SCI cases, diagnoses included transverse myelitis, myelopathy, and non-progressive mass lesions such as arachnoid cyst, epidural hematoma, and ependymoma. Among 66 patients, 52% had private insurance or private funding, and 46% had government funding (Medicare and Medicaid).
Visit and injection details
There were 102 encounters, of which 61% were in the outpatient setting, and 39% were in the inpatient setting (Table 2). The majority of treatments (n = 92, 90%) were performed by a physiatrist or trainees under the supervision of same physiatrists with over ten years of experience with the procedure. Electrical stimulation and ultrasound guidance were utilized in nearly all patient visits (n = 99, 97%). During the 102 clinical encounters, a total of 303 nerve or motor branches were injected.
There were 66 unique patients. Twenty patients received repeat injections during this time frame; 10 had phenol neurolysis twice, 6 were injected three times, 2 were injected four times, and 2 were injected five times either same or different nerves during the study time frame. Phenol neurolysis was most commonly injected in proximal large muscle groups compared to smaller distal muscle groups. Approximately two-thirds of the injections (n = 201, 66%) involved the lower extremity. The obturator nerve and motor branches (n = 101, 33%) to the hip adductors were the most commonly injected lower extremity nerves. Other common targets of the lower extremity were tibial motor branches to the gastrocnemius and soleus muscles (Table 3). One-third of the phenol neurolysis injections (n = 102, 34%) were performed on the upper extremities, and the most common targets included the medial and lateral pectoral nerves (n = 71, 23%) followed by musculocutaneous motor branches to the biceps brachii and brachialis muscles (Table 3).
A median (IQR) of 2 [2,3,4] nerves were injected during each encounter with a median (IQR) of 4 [2,3,4,5,6] ml dose in total per encounter. The total dose per encounter ranged from 0.2 to 20 ml. However, 93% of the patients received a total dose of ≤10 ml per encounter. During each encounter, phenol median dose (IQR) was 1.5 (1.0–2.3) ml per nerve or nerve branch. At the time of the clinical encounter, the most commonly reported concomitant treatment was oral baclofen (n = 79, 77%) followed by botulinum neurotoxin (n = 64, 63%).
Effect on spasticity
Information regarding the procedure’s immediate anesthetic effect was documented for most of the encounters (n = 94, 92%). An immediate benefit resulting in decreased spasticity in injected muscle groups was reported in all 94 encounters.
Most of the encounters post-injection MAS scores within 3 months of injections were not available to provide a change in score for various targets except for the hip adductors and shoulder adductors. For the lower extremity, 14 patients had documented MAS values for a total of 28 hip adductor muscle groups (right and left sides were counted separately). The mean (SD) pre-injection converted MAS scale score (see methods) value was 3.1 (0.8) with a mean (SD) reduction of 1.1 (1) post-procedure. The median (IQR) time between the procedure and post-injection patient assessment was 1.8 (1.4–2.0) months. For the upper extremity shoulder adductors and internal rotators, 5 patients had documented MAS values for a total of 8 muscle groups. The mean (SD) reduction in the converted MAS score was 1 (0.75). The median (IQR) time between the procedure and post-injection patient assessment was 1.3 (1.2–2.2) months.
Safety
Progress notes till discharge and clinical notes during the follow-up visits were reviewed. There were no procedure-related adverse or safety events documented during this study period.
Discussion
In this retrospective review, the majority of the participants were middle-aged, and males with a cervical level of injury, which is consistent with the current epidemiological distribution of SCI [30]. Twenty patients received repeat phenol injections to the same or different targets in our study. Unlike botulinum toxin injections, there is no wait period between initial and repeat phenol injections to various targets. However, one should allow at least 7–9 days to allow completion of axonal degeneration to see the full benefits of phenol prior to repeating injection to the same nerves [22].
Obturator nerve and pectoral nerves innervating large proximal muscles of lower and upper extremities such as hip adductors and shoulder adductors were frequent targets of phenol in people with SCI in this study. A recent study from our institution reported practice patterns of phenol neurolysis for spasticity management. It included people with stroke, traumatic and non-traumatic brain injury, spinal cord injury, and multiple sclerosis [28]. In this study, the most commonly injected targets were the sciatic motor branches to hamstrings and tibial motor nerves to ankle plantar flexors. These findings are likely due to a higher percentage of patients in this cohort suffering from stroke and brain injury. A similar finding was reported in another study of stroke patients from the same institution [31]. This variation in common targets of phenol neurolysis in stroke or brain injury and spinal cord injury could be due to differences in spasticity patterns of cortical and spinal origin.
The majority of the patients (93%) received ≤10 ml phenol dose per encounter. The median (IQR) dose per nerve was 1.5 ml (1–2.3). The average dose during each procedure was below the recommended dose reported in the current literature [20, 21, 31, 32]. The combined electrical stimulation and ultrasound guidance could have lowered the required dose [28, 33]. Other factors include injector preference, the severity of spasticity, and spasticity patterns involving mixed nerves that require multiple injections targeting multiple motor branches. For example, in this study obturator was the most common target, which requires one injection targeting either the main obturator nerve or anterior branch of the obturator nerve. In studies involving stroke and brain injury, sciatic nerve to hamstrings was the most common target, with multiple sensory branches innervating large sensory areas and multiple distal muscles besides target muscle (hamstrings). Therefore, to prevent complications and gain optimal relief of spasticity, one needs to target multiple motor branches to medial and lateral hamstrings, requiring a higher dose. The mean (SD) improvement in the MAS value was 1 (0.75) and 1.1(1) in the upper and lower extremities, respectively, and these findings are consistent with scarce data available on MAS scores in the current literature [33, 34]. Though there is no data on effect size and minimal clinically important difference (MCID) for MAS score in people with SCI, this change in MAS score in our study exceeds the MCID of 0.76 and 0.73 reported for upper and lower extremities in the stroke population [35].
There were no adverse events following phenol neurolysis in this cohort during this time frame. Most of these procedures in this study were performed under combined electrical stimulation and ultrasound guidance. A recently published study where most of the injections were performed under combined ultrasound and electrical stimulation guidance either reported no adverse events or <1% severe adverse events such as dysesthesias which is consistent with the findings of our study [28, 31]. Historical data suggests a higher incidence of adverse effects such as dysesthesias ranging from 4–22% following phenol or alcohol neurolysis when performed only under electrical stimulation guidance [17, 36,37,38,39,40]. However, there is a lack of direct evidence comparing outcomes of phenol neurolysis with and without ultrasound guidance, including adverse effects.
Data from our study suggest that phenol neurolysis can be safely utilized in people with spinal cord injury to manage problematic spasticity. In combination with electrical stimulation, ultrasound guidance can help reduce the dose and improve the localization of the target nerves, which may increase the safety margin of this procedure due to less spread to the adjacent vasculature and nerve bundles. There should be extra caution when injecting mixed nerves such as the musculocutaneous nerve, radial nerve, tibial nerve, sciatic nerves, and femoral nerves that carry sensory fibers for which neurolysis targets should be motor branches to prevent sensory complications such as dysesthesias and loss of sensation.
Individuals with cervical SCI often require management of problematic spasticity in all four extremities. Over time, untreated spasticity leads to a decline in function [41, 42]. Phenol neurolysis may be used alongside other treatment modalities such as botulinum neurotoxin, microsurgical selective peripheral neurotomy, intrathecal baclofen therapy, and oral medications for optimal spasticity management in all four extremities [17, 43]. Microsurgical selective neurotomy can produce similar results to phenol neurolysis [44]. However, this technique requires general anesthesia and is an invasive procedure compared to phenol neurolysis. These two factors likely increase this procedure’s costs and risks compared to phenol neurolysis. Given the lack of studies comparing outcomes, adverse effects, and costs of phenol neurolysis and microsurgical peripheral neurotomy, it is vital to conduct a study comparing these two procedures to improve the quality of care.
Additionally, there are some unique case scenarios where phenol neurolysis can be an excellent intervention with or without botulinum toxin injections in patients with severe spasticity of bilateral lower extremities for whom ITB therapy is not safe or accessible for the following reasons: due to ongoing active infection such as osteomyelitis, medical comorbidities which increase the risks associated with elective surgery, lack of financial resources for surgery and maintenance of ITB therapy, lack of access to ITB and for those unable to commit to the surgery and long-term maintenance required by this treatment. ITB is less effective in relieving spasticity of upper extremities compared to lower extremities in people with SCI [45]. In these scenarios, botulinum toxin alone is not enough to manage spasticity in multiple muscle groups of bilateral upper extremities in people with SCI due to dosing restrictions imposed by funding agencies or insurance companies. Proximal large muscle groups such as pectoralis major muscles and latissimus dorsi are innervated by pectoral and thoracodorsal nerves, which are motor nerves and safe targets for phenol neurolysis with no concern for sensory complications. Furthermore, ultrasound guidance improves the safety of this procedure due to direct visualization of the pleura and lungs under pectoralis major and latissimus dorsi. Similarly, in the lower extremity, hip adductors innervated by the obturator nerve are commonly involved large proximal muscle groups in people with SCI. Though the obturator nerve is a mixed nerve, its sensory innervation is confined to a very small area over the medial side of the thigh [46].
This study has several limitations. This study reports data from a single center, limiting the generalizability of the findings of this study. There were no children with spinal cord injury in our cohort, limiting the generalizability to the pediatric population with SCI. Pre and post-injection evaluations with MAS were not available for all patients, and a lack of a control group to compare outcomes. Additionally, we didn’t have data on the effects of phenol neurolysis on the range of motion, pain, activities of daily living, functional mobility, and quality of life. Although no adverse events were reported, it is possible that these events were not recorded or occurred within the time frame of this study. Although the procedure itself was found to be safe without any complications, long-term adverse events may be missing in the EMR.
Conclusion
In summary, our results suggest that phenol neurolysis in people with SCI is well tolerated with an immediate qualitative improvement documented by clinicians in the majority of the cases. No immediate adverse events following neurolysis were reported in this study using combined electrical and ultrasound guidance. However, there is a lack of data from large sample on objective quantitative measures on improvement of spasticity and its effect on functional outcomes following phenol neurolysis compared to other interventions in people with SCI. There is a need for a future randomized clinical trial comparing cost and clinical outcomes of phenol neurolysis compared to other interventions such as botulinum toxin injection and intrathecal baclofen therapy in people with SCI.
Data availability
Additional data are available from the corresponding author on reasonable request.
References
Holtz KA, Lipson R, Noonan VK, Kwon BK, Mills PB. Prevalence and effect of problematic spasticity after traumatic spinal cord injury. Arch Phys Med Rehabil. 2017;98:1132–8.
Maynard FM, Karunas RS, Waring WP 3rd. Epidemiology of spasticity following traumatic spinal cord injury. Arch Phys Med Rehabil. 1990;71:566–9.
Saulino M, Ivanhoe CB, McGuire JR, Ridley B, Shilt JS, Boster AL, et al. Best practices for intrathecal baclofen therapy: patient selection. Neuromodulation. 2016;19:607–15.
Malhotra S, Pandyan AD, Day CR, Jones PW, Hermens H. Spasticity, an impairment that is poorly defined and poorly measured. Clin Rehabil. 2009;23:651–8.
Pandyan AD, Gregoric M, Barnes MP, Wood D, Van Wijck F, Burridge J, et al. Spasticity: clinical perceptions, neurological realities and meaningful measurement. Disabil Rehab. 2005;27:2–6.
Adams MM, Hicks AL. Spasticity after spinal cord injury. Spinal Cord. 2005;43:577–86.
Rekand T, Hagen EM, Gronning M. Spasticity following spinal cord injury. Tidsskr Nor Laegeforen. 2012;132:970–3.
Skold C, Levi R, Seiger A. Spasticity after traumatic spinal cord injury: nature, severity, and location. Arch Phys Med Rehabil. 1999;80:1548–57.
Westerkam D, Saunders LL, Krause JS. Association of spasticity and life satisfaction after spinal cord injury. Spinal Cord. 2011;49:990–4.
Spasticity: diagnosis and management 2nd ed: New York: Demos Medical, 2016.; 2016
Elovic EP, Esquenazi A, Alter KE, Lin JL, Alfaro A, Kaelin DL, et al. Chemodenervation and nerve blocks in the diagnosis and management of spasticity and muscle overactivity. PM R. 2009;1:842–51.
Gracies JM, Elovic E, McGuire J, Simpson DM. Traditional pharmacological treatments for spasticity. Part I: Local treatments. Muscle Nerve Suppl. 1997;6:S61–91.
Kheder A, Nair KP. Spasticity: pathophysiology, evaluation and management. Practical Neurol. 2012;12:289–98.
Msaddi AK, Mazroue AR, Shahwan S, Al Amri N, Dubayan N, Livingston D, et al. Microsurgical selective peripheral neurotomy in the treatment of spasticity in cerebral-palsy children. Stereotact Funct Neurosurg. 1997;69:251–8.
Fan J, Milosevic R, Wang S. Selective peripheral neurotomy (SPN) as a treatment strategy for spasticity. Brain Sci Adv. 2020;6:30–41.
Gonnade N, Lokhande V, Ajij M, Gaur A, Shukla K. Phenol versus botulinum toxin a injection in ambulatory cerebral palsy spastic diplegia: a comparative study. J Pediatr Neurosci. 2017;12:338–43.
Escaldi S. Neurolysis: a brief review for a fading art. Phys Med Rehabil Clin N Am. 2018;29:519–27.
D’Souza RS, Hooten WM. Neurolytic Blocks. StatPearls. Treasure Island (FL)2021.
Felsenthal G. Pharmacology of phenol in peripheral nerve blocks: a review. Arch Phys Med Rehabil. 1974;55:13–6.
Horn LJ, Singh G, Dabrowski ER. Chemoneurolysis With Phenol and Alcohol: A “Dying Art” That Merits Revival. In: Brashear A, Elovic E, editors. New York: Springer Publishing Company; 2015. p. 109-28.
D’Souza RS, Warner NS. Phenol Nerve Block. StatPearls. Treasure Island (FL) 2021.
Zhang B, Darji N, Francisco GE, Li S. The time course of onset and peak effects of phenol neurolysis. Am J Phys Med Rehabil. 2021;100:266–70.
Sung DH, Han TR, Park WH, Je Bang H, Kim JM, Chung SH, et al. Phenol block of peripheral nerve conduction: Titrating for optimum effect. Arch Phys Med Rehabil. 2001;82:671–6.
Halpern D, Meelhuysen FE. Duration of relaxation after intramuscular neurolysis with phenol. JAMA. 1967;200:1152–4.
Akkaya T, Unlu E, Alptekin A, Gumus HI, Umay E, Cakci A, et al. Neurolytic phenol blockade of the obturator nerve for severe adductor spasticity. Acta Anaesthesiol Scand. 2010;54:79–85.
Awad EA. Phenol block for control of hip flexor and adductor spasticity. Arch Phys Med Rehabil. 1972;53:554–7.
Copp EP, Harris R, Keenan J. Peripheral nerve block and motor point block with phenol in the management of spasticity. Proc R Soc Med. 1970;63:937–8.
Karri J, Mas MF, Francisco GE, Li S. Practice patterns for spasticity management with phenol neurolysis. J Rehabil Med. 2017;49:482–8.
Mas MF, DiTommaso C, Li S. Phenol neurolysis for the management of shoulder spasticity in early recovery from traumatic. Brain Injury: A Case Report PM R. 2019;11:90–3.
National Spinal Cord Injury Statistical Center. Spinal Cord Injury Facts and Figures at a Glance. University of Alabama at Birmingham: Birmingham, Alabama. [Internet]. 2019. Available from: https://www.nscisc.uab.edu/Public/Facts%20and%20Figures%202019%20-%20Final.pdf.
Li S, Woo J, Mas MF. Early Use of phenol neurolysis likely reduces the total amount of botulinum toxin in management of post-stroke spasticity. Front Rehab Sci. 2021;2:729178. Published 2021 Sep 16. https://doi.org/10.3389/fresc.2021.729178.
Gaid M. Phenol nerve block for the management of lower limb spasticity. Adv Clin Neurosci Rehab. 2012;12:23–5.
Matsumoto ME, Berry J, Yung H, Matsumoto M, Munin MC. Comparing electrical stimulation with and without ultrasound guidance for phenol neurolysis to the musculocutaneous nerve. PM R 2018;10:357–64.
Kocabas H, Salli A, Demir AH, Ozerbil OM. Comparison of phenol and alcohol neurolysis of tibial nerve motor branches to the gastrocnemius muscle for treatment of spastic foot after stroke: a randomized controlled pilot study. Eur J Phys Rehabil Med. 2010;46:5–10.
Chen CL, Chen CY, Chen HC, Wu CY, Lin KC, Hsieh YW, et al. Responsiveness and minimal clinically important difference of Modified Ashworth Scale in patients with stroke. Eur J Phys Rehabil Med. 2019;55:754–60.
Karen SG, Chua K-HK. Clinical and functional outcome after alcohol neurolysis of the tibial nerve for ankle?foot spasticity. Brain Inj. 2001;15:733–9.
Kong KH, Chua KS. Neurolysis of the musculocutaneous nerve with alcohol to treat poststroke elbow flexor spasticity. Arch Phys Med Rehabil. 1999;80:1234–6.
Kong KH, Chua KS. Intramuscular neurolysis with alcohol to treat post-stroke finger flexor spasticity. Clin Rehabil. 2002;16:378–81.
Shafshak TS, Mohamed-Essa A. Phenol neurolysis for relieving intermittent involuntary painful spasm in upper motor neuron syndromes: a pilot study. J Rehabil Med. 2009;41:201–2.
Yadav SL, Singh U, Dureja GP, Singh KK, Chaturvedi S. Phenol block in the management of spastic cerebral palsy. Indian J pediatrics. 1994;61:249–55.
van Cooten IP, Snoek GJ, Nene AV, de Groot S, Post MW. Functional hindrance due to spasticity in individuals with spinal cord injury during inpatient rehabilitation and 1 year thereafter. Spinal Cord. 2015;53:663–7.
Tibbett J, Widerstrom-Noga EG, Thomas CK, Field-Fote EC. Impact of spasticity on transfers and activities of daily living in individuals with spinal cord injury. J Spinal Cord Med. 2019;42:318–27.
Viel E, Pellas F, Ripart J, Pelissier J, Eledjam JJ. [Peripheral neurolytic blocks and spasticity]. Ann Fr Anesth Reanim. 2005;24:667–72.
Sitthinamsuwan B, Chanvanitkulchai K, Phonwijit L, Nunta-Aree S, Kumthornthip W, Ploypetch T, et al. Surgical outcomes of microsurgical selective peripheral neurotomy for intractable limb spasticity. Stereotact Funct Neurosurg. 2013;91:248–57.
Burns AS, Meythaler JM. Intrathecal baclofen in tetraplegia of spinal origin: efficacy for upper extremity hypertonia. Spinal Cord. 2001;39:413–9.
Felten DL, O’Banion MK, Maida MS. 9 - Peripheral Nervous System. In: Felten DL, O’Banion MK, Maida MS, editors. Netter’s Atlas of Neuroscience (Third Edition). Philadelphia: Elsevier; 2016. p. 153-231.
Acknowledgements
We would like to acknowledge Jonathan Vandenberg, MD for his assistance in data collection.
Author information
Authors and Affiliations
Contributions
RK contributed to the study design, data collection, data analysis, and writing of the manuscript. AM contributed to the data collection, data analysis, and writing of the manuscript. EP contributed to the study design and was responsible for data collection. AS and SL were involved in study design and the manuscript preparation.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was approved by the Institutional Review Board of the University of Texas Health Science Center at Houston.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Korupolu, R., Malik, A., Pemberton, E. et al. Phenol neurolysis in people with spinal cord injury: a descriptive study. Spinal Cord Ser Cases 8, 90 (2022). https://doi.org/10.1038/s41394-022-00556-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-022-00556-0