Abstract
Study design
This is a retrospective, observational study.
Objectives
To evaluate organ dysfunction in patients with an acute traumatic spinal cord injury (ATSCI) above T6 using the Sequential Organ Failure Assessment (SOFA) score to determine its association with mortality.
Setting
The study was performed at the intensive care unit (ICU) of a tertiary hospital in the northwest of Spain.
Methods
The study included 241 patients with an ATSCI above T6 who had been admitted to the ICU between 1998 and 2017. A descriptive analysis of all variables collected was performed to compare the survivors with the non-survivors. In addition, a logistic regression model was used in the multivariate analysis to identify variables that were independently associated with mortality.
Results
The results revealed significant differences between the survivors and non-survivors in terms of their age, Charlson Comorbidity Index, Glasgow Coma Scale score on admission, APACHE II score, SOFA score on day 0 and day 4, and delta SOFA 4–0 (ΔSOFA 4–0). The results of this multivariate analysis identified the following variables as independent predictors of intra-ICU mortality: age (OR = 1.05; 95% CI: 1. 01–1.08), SOFA score on day 0 (OR = 1.42; 95% CI: 1.13–1.78), ΔSOFA 4–0 (OR = 1.53; 95% CI: 1.25–1.87), and fluid balance on day 4 (OR = 1.16; 95% CI: 1.00–1.35).
Conclusions
The SOFA score is useful for evaluating organ dysfunction in patients with an ATSCI above T6. After adjusting the analysis for conventional variables, organ dysfunction on admission, changes in organ function between day 4 and day 0 (ΔSOFA 4–0), and fluid balance on day 4 were seen to be independently associated with mortality in our study.
Similar content being viewed by others
Introduction
As in the case of other surgical or trauma patients, those with an acute traumatic spinal cord injury (ATSCI) above T6 are likely to develop multiple organ dysfunction, which undoubtedly has an impact on the mortality of this patient population [1, 2]. The multiple organ dysfunction syndrome is a sequential and biphasic (early vs. delayed) condition appearing after an aggression and classically described in critically ill patients [3]. Although several organ dysfunction scoring systems have been described to date, the Sequential Organ Failure Assessment (SOFA) score is one of the most commonly used tools in intensive care units (ICUs). While its prognostic relevance has been documented in other populations of critically ill patients [4,5,6], it has not been validated for patients with an ATSCI requiring admission to the ICU. The cardiovascular component of this SOFA is calculated based on the patient’s mean arterial pressure (MAP) levels and the need for treatment with vasoactive drugs. Previous studies performed with several populations of critically ill patients suggest the existence of a close relationship between the cardiovascular SOFA score and mortality [7, 8]. However, in this particular population, said score can be impacted by the treatment used to maintain the spinal cord perfusion pressure, which is one of the initial standards of care in this patient population.
Therefore, considering prognostic variables relating to the patient’s demographic characteristics, the injury, and the therapeutic management, the aim of this study was to determine whether the existence of organ dysfunction on admission and on day 4 as determined by the SOFA score was associated with mortality in a population of patients with an ATSCI above T6 who were admitted to ICU over a 20-year period.
Methods
We performed a retrospective, observational, follow-up study of patients diagnosed with an ATSCI above T6 who had been admitted to the ICU of the University Hospital Complex of A Coruña (northwest of Spain) between January 1998 and December 2017. This hospital is a reference center for the treatment of patients with acute spinal cord injuries and serves a population of 2,750,000 inhabitants. The study was approved by the Galician Clinical Research Ethics Committee with authorization code 2019/622.
Participants
A total of 241 adult (>18 years) patients with an ATSCI above T6 were admitted to the ICU over the established study period. The inclusion criterion of this study was chosen to focus our analysis on patients with an ATSCI whose injury level determined a risk of developing organ dysfunction (lesions below T6 do not cause neuromuscular respiratory failure nor neurogenic shock). Patients who (a) did not meet the above inclusion criteria, (b) were pregnant, (c) had “do not resuscitate” orders, and (d) whose cause of the shock was not spinal (e.g., hemorrhagic) were excluded from the study. This sample size allowed us to estimate the study parameters with a precision of ±6.3% and a safety of 95%.
Data collection
Data from the following variables were collected for all patients: sociodemographic characteristics (age, sex, and Charlson Comorbidity Index), injury (mechanism, affected neurological level [C1–C4, C5–C8, thoracic ≥ T6], American Spinal Injury Association [ASIA] Impairment Scale [AIS] grade, ASIA motor score, and existence of associated lesions as evaluated by the ISS), severity (Acute Physiology and Chronic Health Evaluation [APACHE II] score within the first 24 h and Glasgow Coma Scale [GCS] score on admission), any variable needed to calculate the SOFA score (Table 1), and the fluid balance on day 4. Intra-ICU mortality was also recorded to assess the prognosis.
Measurements
The SOFA score was measured on admission (SOFA score on day 0) and on the fourth day (SOFA score on day 4), and the difference between both values was calculated (ΔSOFA 4–0). Scores of the different SOFA components (cardiovascular, respiratory, hematological, hepatic, renal, and neurological) were calculated to determine the existence of organ system dysfunction. In sedated patients, the neurological component of the SOFA was scored on the basis of the patient’s clinical condition prior to the sedation.
Clinical care
The patients included in this study were admitted to the ICU to be monitored and receive organ support therapy, and were cared for by a multidisciplinary team of intensivists that was physically present 24 h a day. The injury level and grade were examined by specialist doctors of the spinal cord injury unit. Patients presenting with neurogenic shock throughout the study period were resuscitated with fluid replacement therapy and vasoactive drugs. The guidelines set forth over the last decade recommend maintaining a target MAP of 85 mmHg during the first week following the injury in order to achieve an adequate spinal perfusion pressure. The decision to perform tracheal intubation and initiate mechanical ventilation is made by the attending physician on the basis of the standard criteria applicable to this patient population. Based on the available evidence on corticosteroid therapy, only a small number of patients with this condition have received this treatment in recent years [9, 10].
Statistical analysis
A descriptive analysis of all variables collected was performed to compare the characteristics of the survivors with those of the non-survivors. After contrasting the normality of the data with the Kolmogorov–Smirnov test, the quantitative variables were compared using Student’s t-test or the Mann–Whitney test, and the qualitative variables were compared using the χ2 test.
In addition, a logistic regression model was used in the multivariate analysis to identify variables that were independently associated with mortality, calculating the associated odds ratio and their 95% confidence intervals. A forward stepwise strategy was applied whereby the variables associated with P values <0.20 in the bivariate analysis were included in this model. More specifically, the model was adjusted for the fluid balance on day 4 despite this parameter being of borderline statistical significance considering that its impact on mortality has been demonstrated in other populations of critically ill patients [11,12,13].
The impact of the existence of organ dysfunction on admission and on day 4 on mortality was evaluated based on receiver operating characteristic (ROC) curves and the area under the curve (AUC) together with its 95% confidence interval.
The analysis was performed with software SPSS 24.0 for Windows, setting the bilateral significance level at P < 0.05.
Results
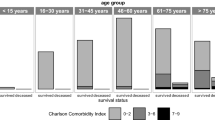
A total of 241 patients diagnosed with an ATSCI above T6 were admitted to the ICU between January 1998 and December 2017. Eighty three percent of the patients were admitted in the ICU in the 48 h following the injury. The mean age of the patients, of whom 77.6% were men, was 53.2 ± 20.1 years and their mean Charlson Comorbidity Index was 0.9 ± 1.7. The most frequent injury mechanism was falls (41.3%), followed closely by traffic accidents (35.3%). The most commonly affected neurological level was C5–C8 (39.9%), followed by C1–C4 (33.0%), and, finally, the thoracic level (27.0%). AIS A was the predominant injury grade (51.8%), the mean ASIA motor score was 35.9 ± 26.9, the mean ISS was 33.7 ± 12.7, and the mean GCS score on admission was 13.4 ± 3.3. The median APACHE II score was 1, and the median SOFA scores on day 0 and 4 were 5 and 4, respectively. Intra-ICU mortality in this group of patients was 12.4% (n = 30).
Univariate analysis of the intra-ICU mortality
A bivariate analysis was performed to identify variables associated with intra-ICU mortality. Its results revealed significant differences between the survivors and non-survivors in terms of their age, Charlson Comorbidity Index, GCS score on admission, APACHE II score, SOFA score on day 0, SOFA score on day 4, and ΔSOFA 4–0. The fluid balance on the fourth day was of borderline statistical significance. As shown in Table 2, the non-survivors were significantly older than the survivors (65.6 vs. 51.4 years; P < 0.001), had a higher comorbidity index (1.8 vs. 0.8; P = 0.003), a lower GCS score (12.3 vs. 13.5; P = 0.023), a higher APACHE II score (17.6 vs. 11.8; P < 0.001), a higher SOFA score on day 0 (7.1 vs. 5.0; P < 0.001), a higher SOFA score on day 4 (8.0 vs. 4.2; P < 0.001), and a higher ΔSOFA 4–0 (1.7 vs. –0.9; P = 0.001).
Mortality associated with the existence of organ dysfunction on admission and during the resuscitation phase
To determine which component of the SOFA has the greatest discriminatory capacity to predict intra-ICU mortality, we analyzed the area under the ROC curve of the total SOFA score on days 0 and 4, the ΔSOFA 4–0, and each of its components (Fig. 1).
The results of this analysis show that the cardiovascular component yielded the greatest AUC (0.607) of all components of the SOFA on admission.
As well as on admission, the existence of cardiovascular dysfunction on day 4 also played a crucial role in mortality, with an AUC of 0.772. The same was true for the ΔSOFA 4–0, in which case the cardiovascular component yielded an area under the ROC curve to predict mortality of 0.660.
Multivariate analysis of the intra-ICU mortality
A multivariate logistic regression analysis was performed to determine which variables were independently associated with higher intra-ICU mortality with a view to assess the relative contribution to mortality of organ dysfunction present on admission (SOFA score on day 0) and that developed during the resuscitation period and up to 4 days post trauma (ΔSOFA 4–0).
The results of this multivariate analysis identified the following variables as independent predictors of intra-ICU mortality: age (OR = 1.05; 95% CI, 1.01–1.08), SOFA score on day 0 (OR = 1.42; 95% CI, 1.13–1.78), ΔSOFA 4–0 (OR = 1.53; 95% CI, 1.25–1.87), and fluid balance on day 4 (OR = 1.16; 95% CI, 1.00–1.35). The model used to perform this analysis is shown in Table 3.
Mortality by age, SOFA score on day 0, ΔSOFA (4–0), and fluid balance on day 4
Figure 2 presents the mortality rates in relation to the variables identified as independent predictors of intra-ICU mortality. As shown in this figure, a third of the patients over the age of 80 passed away, whereas only 3.39% of those aged ≤35 years died, which demonstrates that an increase in age is associated with a gradual rise in the risk of death.
Mortality also increased from 5.71% among the patients with a SOFA score of 0–4 points on admission to 27.78% among those with a SOFA score ≥10 points at that same moment.
Furthermore, mortality also increased with a higher ΔSOFA during the resuscitation phase, from 6.45% among the patients with a ΔSOFA 4–0 of zero to 80% among the patients with a ΔSOFA 4–0 greater or equal to 6.
A three-phase distribution can be observed for the fluid balance on day 4, starting with an initial rise in mortality of 7.27% for a fluid balance <2.5 L, followed by a decrease to 4.84% for the 2.5–5 L range, and a final considerable increase with a fluid balance above 5 L.
Discussion
We used the SOFA score to quantify the number of cases of organ dysfunction on admission to the ICU (day 0) and after the resuscitation phase (day 4) in a cohort of 241 patients with an ATSCI above T6. This score allows us to evaluate changes in organ function over time based on simple parameters, is widely accepted in adult critical care units, and its association with mortality has been demonstrated in other populations of critically ill patients [4, 6, 14,15,16,17,18]. The findings of our study revealed the following.
First, in our case series, the SOFA score on day 0 was independently correlated with intra-ICU mortality following an adjustment for conventional variables. To our knowledge, this is the first study to prove the existence of an independent relationship between mortality in patients with an ATSCI above T6 and the existence of organ dysfunction on admission as determined by the SOFA score. Our data showed that higher SOFA scores on day 0 were associated with greater mortality rates ranging from 5.71% for SOFA scores <5 to almost 30% for SOFA scores >9 (Fig. 2). Particularly with respect to the individual components of the SOFA, the greatest discriminative power was observed for the cardiovascular system. Organ dysfunction presenting immediately after the traumatic event is probably related to a series of biological genetic and immune phenomena, the body’s cardiorespiratory ability to respond to the trauma, the presence of comorbidities, and the management approach applied prior to the patient’s hospitalization. This could suggest that all efforts aimed at applying an optimal pre-hospital and early therapeutic management may be of prognostic interest. In practical terms, this translates into special attention to injuries that may compromise the patient’s hemodynamics at the accident site itself, with the administration of fluids or vasopressors, if necessary, as well as appropriate intervention according to the oxygenation and ventilatory support that may be required [19, 20].The SOFA score on day 0 reflects the degree of dysfunction already present on admission and could be useful for stratifying patients and screening them for their inclusion in clinical trials.
Second, we measured the SOFA score on day 4 as an estimate of delayed organ dysfunction. Our analysis showed that changes (absence of improvement or worsening) in the degree of organ dysfunction during the post-traumatic resuscitation phase as determined by a comparison between the SOFA score on day 4 and the SOFA score on day 0 (ΔSOFA 4–0) are associated with mortality when considering conventional variables (demographic characteristics, type of injury, and ISS) and regardless of the existence of organ dysfunction on admission. The prognostic value of these changes in patients’ organ function following an insult has already been documented in other populations of critically ill patients [7, 17, 21,22,23,24].
Our results indicate that post-traumatic organ dysfunction does not invariably progress to multi-organ failure. However, the degree of organ function deterioration beyond the days immediately following the trauma has an impact on the survival of patients with an ATSCI above T6, and the ability of this parameter to distinguish between survivors and non-survivors is greater than that of the SOFA score on day 0. Thus, the likelihood of death increases from 6.45% among patients with a ΔSOFA 4–0 of zero to 80% among patients with a ΔSOFA 4–0 equal to or greater than 6. In this respect, changes in the cardiovascular and respiratory components of the SOFA provide a greater discriminative capacity to predict mortality in a population of patients with a low incidence of renal, hepatic, and hematologic dysfunction, therefore suggesting that strategies aimed particularly at achieving respiratory and cardiovascular optimization could have an impact on survival. Advanced cardiorespiratory monitoring tools (VolumeView® or PICCO®) can provide more precise information on the cause of the dysfunction and the components that may require intervention in terms of organ support. However, as in the case of other patient populations, the cumulative SOFA score obtained in our study proved to be better at discriminating said outcome than the individual scores [7, 25]. Still, the ability to independently analyze several organs and systems and to describe their individual dysfunction over time could allow to define groups of patients [4], as well as to modify time-dependent changes and the impact of novel therapies.
By documenting the role of organ dysfunction in the prognosis of patients with an ATSCI above T6 admitted to the ICU, we were able to identify other factors captured by the SOFA score other than conventional variables (demographic characteristics and type of injury) that might play a role in the particular pathological response of each patient to aggressions of this same magnitude and their mortality (e.g., genetic and physiological factors). Given that multi-organ failure is, at a very basic level, a cellular and molecular disease, attempts to understand and eventually treat this complex syndrome must not only include organ support, but also the use of this assessment scale [26].
Third, the administration of fluid replacement therapy is a determinant of mortality regardless of the patient’s severity. Although the administration of fluid replacement therapy during neurogenic shock resuscitation has classically been indicated as an empirical treatment based on static variables (central venous pressure or pulmonary capillary pressure), there is evidence that uncorrected hypovolemia results in an inadequate administration of vasopressor agents that can increase organ hypoperfusion and ischemia [27, 28]. In addition, overprescription of fluids can also compromise oxygen supply and has been associated with an increased rate of complications and greater mortality [12, 13, 27,28,29]. The results of our study show two trends in which mortality was greater among the patients with a fluid balance on day four <2.5 L and those with a balance >5 L. This suggests that intervening in the resuscitation process with hemodynamic optimization strategies (dynamic volume response rates, lactate, etc.) could avoid under-resuscitation and over-hydration with an impact on prognosis. Given that this approach has proved to be beneficial in other populations of unstable patients, the conduct of regulated studies in populations with neurogenic shock secondary to spinal cord injury would be highly relevant.
Cardiovascular and respiratory dysfunction have been shown to impact mortality in other neurotrauma populations [5, 30]. Clinicians caring for these patients, both before and during ICU admission, should be aware of the risk of organ dysfunction derived from an ATSCI above T6 in order to anticipate or recognize it. The findings of this study validate, for the first time ever, the use of the SOFA in this patient population as a tool to assess changes in organ function after injury onset and suggest that appropriate interventions (early and optimal) could improve the condition’s prognosis.
Study limitations
Despite being performed with the greatest methodological guarantees, our study might have some limitations, including, in the first place, the fact that the likelihood of death over a 20-year period could be related to changes in the management of this patient population throughout this time; second, that, because this was a single-center study, the analyzed sample might not be representative of other patients with the same condition; and, finally, the retrospective nature of this study, although the exhaustive patient records available in the ICU minimized the loss of data that would be expected in other studies of equal size.
Conclusions
Patients with an ATSCI above T6 exhibit an individual response in terms of the onset of organ dysfunction that can be measured with the SOFA and is correlated with survival. In addition to the conventional variables, changes in organ function and fluid balance within the first few days following the trauma also have a prognostic value, thus suggesting that interventions aimed at optimizing these two parameters might improve survival in this patient population.
Data availability
All relevant data are within this manuscript and raw data are archived by the authors.
References
Stein DM, Menaker J, McQuillan K, Handley C, Aarabi B, Scalea TM. Risk factors for organ dysfunction and failure in patients with acute traumatic cervical spinal cord injury. Neurocrit Care. 2010;13:29–39.
Kamp O, Jansen O, Lefering R, Meindl R, Waydhas C, Schildhauer TA, et al. Cervical spinal cord injury shows markedly lower than predicted mortality (>72h after multiple trauma) from sepsis and multiple organ failure. J Intensive Care Med. 2020;35:378–82.
Moore FA, Sauaia A, Moore EE, Haenel JB, Burch JM, Lezotte DC. Postinjury multiple organ failure: a bimodal phenomenon. J Trauma. 1996;40:501–10. discussion 10–2
Vincent JL, de Mendonça A, Cantraine F, Moreno R, Takala J, Suter PM, et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit Care Med. 1998;26:1793–800.
Zygun D, Berthiaume L, Laupland K, Kortbeek J, Doig C. SOFA is superior to MOD score for the determination of non-neurologic organ dysfunction in patients with severe traumatic brain injury: a cohort study. Crit Care. 2006;10:R115.
Ceriani R, Mazzoni M, Bortone F, Gandini S, Solinas C, Susini G, et al. Application of the Sequential Organ Failure Assessment score to cardiac surgical patients. Chest. 2003;123:1229–39.
Moreno R, Vincent JL, Matos R, Mendonça A, Cantraine F, Thijs L, et al. The use of maximum SOFA score to quantify organ dysfunction/failure in intensive care. Results of a prospective, multicentre study. Working Group on Sepsis related Problems of the ESICM. Intensive Care Med. 1999;25:686–96.
Peres Bota D, Melot C, Lopes Ferreira F, Nguyen Ba V, Vincent JL. The Multiple Organ Dysfunction Score (MODS) versus the Sequential Organ Failure Assessment (SOFA) score in outcome prediction. Intensive Care Med. 2002;28:1619–24.
Hadley MN, Walters BC. Introduction to the guidelines for the management of acute cervical spine and spinal cord injuries. Neurosurgery. 2013;72 Suppl 2:5–16.
Walters BC, Hadley MN, Hurlbert RJ, Aarabi B, Dhall SS, Gelb DE, et al. Guidelines for the management of acute cervical spine and spinal cord injuries: 2013 update. Neurosurgery. 2013;60 CN_suppl_1:82–91.
Acheampong A, Vincent JL. A positive fluid balance is an independent prognostic factor in patients with sepsis. Crit Care. 2015;19:251.
Bouchard J, Soroko SB, Chertow GM, Himmelfarb J, Ikizler TA, Paganini EP, et al. Fluid accumulation, survival and recovery of kidney function in critically ill patients with acute kidney injury. Kidney Int. 2009;76:422–7.
Boyd JH, Forbes J, Nakada TA, Walley KR, Russell JA. Fluid resuscitation in septic shock: a positive fluid balance and elevated central venous pressure are associated with increased mortality. Crit Care Med. 2011;39:259–65.
Antonelli M, Moreno R, Vincent JL, Sprung CL, Mendoça A, Passariello M, et al. Application of SOFA score to trauma patients. Sequential Organ Failure Assessment. Intensive Care Med. 1999;25:389–94.
Halonen KI, Pettilä V, Leppäniemi AK, Kemppainen EA, Puolakkainen PA, Haapiainen RK. Multiple organ dysfunction associated with severe acute pancreatitis. Crit Care Med. 2002;30:1274–9.
Huang SS, Chen YH, Lu TM, Chen LC, Chen JW, Lin SJ. Application of the Sequential Organ Failure Assessment score for predicting mortality in patients with acute myocardial infarction. Resuscitation. 2012;83:591–5.
Jones AE, Trzeciak S, Kline JA. The Sequential Organ Failure Assessment score for predicting outcome in patients with severe sepsis and evidence of hypoperfusion at the time of emergency department presentation. Crit Care Med. 2009;37:1649–54.
Basile-Filho A, Lago AF, Menegueti MG, Nicolini EA, Nunes RS, Lima SL, et al. The use of SAPS 3, SOFA, and Glasgow Coma Scale to predict mortality in patients with subarachnoid hemorrhage: a retrospective cohort study. Medicine (Baltimore). 2018;97:e12769.
Hawayek B, Lucasti C, Patel D, Maraschiello M, Kowalski J. Cardiac asystole following high spinal cord injury: a case report. J Spine Surg. 2021;7:233–7.
Hassid VJ, Schinco MA, Tepas JJ, Griffen MM, Murphy TL, Frykberg ER, et al. Definitive establishment of airway control is critical for optimal outcome in lower cervical spinal cord injury. J Trauma. 2008;65:1328–32.
Russell JA, Singer J, Bernard GR, Wheeler A, Fulkerson W, Hudson L, et al. Changing pattern of organ dysfunction in early human sepsis is related to mortality. Crit Care Med. 2000;28:3405–11.
Ferreira FL, Bota DP, Bross A, Mélot C, Vincent JL. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA. 2001;286:1754–8.
Levy MM, Macias WL, Vincent JL, Russell JA, Silva E, Trzaskoma B, et al. Early changes in organ function predict eventual survival in severe sepsis. Crit Care Med. 2005;33:2194–201.
Cabré L, Mancebo J, Solsona JF, Saura P, Gich I, Blanch L, et al. Multicenter study of the multiple organ dysfunction syndrome in intensive care units: the usefulness of Sequential Organ Failure Assessment scores in decision making. Intensive Care Med. 2005;31:927–33.
Vosylius S, Sipylaite J, Ivaskevicius J. Sequential Organ Failure Assessment score as the determinant of outcome for patients with severe sepsis. Croat Med J. 2004;45:715–20.
Deitch EA. Multiple organ failure. Pathophysiology and potential future therapy. Ann Surg. 1992;216:117–34.
Marik PE, Monnet X, Teboul JL. Hemodynamic parameters to guide fluid therapy. Ann Intensive Care. 2011;1:1.
Murakawa K, Kobayashi A. Effects of vasopressors on renal tissue gas tensions during hemorrhagic shock in dogs. Crit Care Med. 1988;16:789–92.
Murphy CV, Schramm GE, Doherty JA, Reichley RM, Gajic O, Afessa B, et al. The importance of fluid management in acute lung injury secondary to septic shock. Chest. 2009;136:102–9.
Zygun DA, Kortbeek JB, Fick GH, Laupland KB, Doig CJ. Non-neurologic organ dysfunction in severe traumatic brain injury. Crit Care Med. 2005;33:654–60.
Author information
Authors and Affiliations
Contributions
IE-A: literature search, study design, data collection, data interpretation, and drafting of this manuscript. RG: literature search, study design, data interpretation, and drafting of this manuscript. AMM: literature search, study design, and drafting of this manuscript. SPD: study design, data analysis, data interpretation, and drafting of this manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was approved by the Research Ethics Committee with authorization code: 2019/622.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Esmorís-Arijón, I., Galeiras, R., Montoto Marqués, A. et al. Organ dysfunction as determined by the SOFA score is associated with prognosis in patients with acute traumatic spinal cord injury above T6. Spinal Cord 60, 274–280 (2022). https://doi.org/10.1038/s41393-021-00701-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-021-00701-w