Abstract
To further enhance the minimal invasiveness of Rezum treatment (RT), we sought to evaluate the advantages and feasibility of transurethral intraprostatic anesthesia (TUIA) via Schelin Catheter™ (SC). We enrolled 20 men with LUTS due to BPH, who underwent RT using TUIA via SC. Prior to the procedure, patients were asked to rate their pain on a numeric rating scale (NRS) numbered 0–10: with 0 being “No pain” and 10 being “Worst pain”. Median NRS score ranged from 0 to 3. No perioperative procedure-related complications were reported.
Similar content being viewed by others
The efficacy and safeness of Rezum treatment (RT) is widely described in literature for patients with moderate LUTS [1,2,3,4]. Despite initial concerns about indication in glands over 80 ml of volume and third lobe, Elterman et al. have just presented their 1-year outcomes after RT in 83 patients with median (IQR) prostate volume of 100 ml (88.5–115.0), 65% with median lobe. At 12 months IPSS, QoL and UFM improved by 59%, 70% and 59%, respectively, while erectile and ejaculatory function remained preserved, showing the efficacy of RT even in large glands without affecting sexual function, which is a relevant and desired outcome for all patients [5].
Due to these promising results, RT could stand out as the most effective and versatile minimally invasive surgical treatments procedure [6].
Contrary to the standardized technique protocol, anesthesia is performed according to surgeons' preference, ranging from general anesthesia and mild sedation to prostatic block, through a transrectal probe [7]. The first can affect operative time and it exposes patients to anesthesia-related complication, the latter has a certain discomfort due to the transrectal probe and a risk of infective complications.
To further enhance the minimal invasiveness of RT, we sought to evaluate the advantages and feasibility of local intraprostatic anesthesia delivered transurethrally (TUIA) via the Schelin Catheter™ (SC) [8].
TUIA, using topic injections of mepivacaine before TURP and high-energy microwave thermotherapy, showed less perioperative bleeding, reduced operative time and postoperative pain [9].
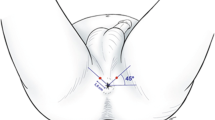
SC tool consists of a catheter provided with an operational channel equipped with a retractile needle and the standard drainage and balloon port (Fig. 1).
At first, the SC is inserted, and the balloon is filled with 10 cc of saline solution; the catheter is then stretched so the balloon rests against the bladder neck, allowing bladder voiding. Rotating the catheter a 20 ml of 1% anesthetic solution of mepivacaine or lidocaine is injected transurethrally into the prostate, according to the following scheme: 3–2–2 mL at 8 and 4 o’clock position; 3 ml at 10 and 2 o’clock position. After injections, the balloon can be deflated and SC removed in order to introduce the Rezūm™ device.
We enrolled 20 patients, with a median age of 67 (60–74) years. All patients had alfa-blocker therapy and were in an outpatient setting.
The median (IQR) prostate size was 75 ml (60–100), with a median Qmax 9 ml/s, median IPSS 23 (19–26) and QoL 4 (3–4).
Median TUIA and Rezūm™ operative time (range) were 3 (2–4) and 6 (5–9) min, respectively. All patients were discharged 4–6 h after the procedure.
Prior to the procedure, patients were asked to rate their pain on a numeric rating scale (NRS).
Pain scores were assessed at nine timepoints:
1. Preoperatively
2. Schelin Catheter insertion
3. LA infiltration
4. Rezūm™ probe insertion
5. Water Vapor Treatment (WVT)
6. Catheter insertion
7. Day 1
8. Day 7 catheter removal
9. Day 30 follow-up visit
Questionnaires were administered on the day of surgery as well as on 1st, 7th and 30th postoperative days to rate NRS of pain.
Median NRS reported was 1.5 at each time point except at points 1, 2, 3 and 5. Median NRS of pain was: 0 at preoperative stage; 2 during catheter insertion; 2.5 during LA infiltration; 3 during WVT. One out of 20 patients reported a NRS of 6 during WVT. No perioperative anesthesiologic and procedure-related complications were reported.
Median catheterization time was 7 days. No cases of AUR or UTI at 30 days postoperatively were recorded.
Our data reports for the first time in literature the use of TUIA using SC to improve pain control during RT.
Along with other technique refinements we have already described, such as postprocedure urethral stent, TUIA allows a further step forward towards micro-invasiveness [10].
This simple and effective approach showed several significant advantages from no or minimal patient discomfort to less theater and faster recovery time.
The latter is of paramount importance both during the COVID‐19 pandemic and even in a desirable postpandemic era where both availability of theater resources are scarce and waiting lists overloaded. Furthermore, utilization of theater and recovery time can be considered a surrogate marker for cost.
Another potential advantage is also the use of RT for patients not suitable for general anesthesia.
An interesting finding is that a low NRS of pain was observed at points 6–8, since in the early postoperative phase patients did not report catheter-related pain or discomfort. This can probably be explained by the preemptive analgesic effect that minimizes sensitization induced by noxious stimuli arising throughout the water vapor injections.
Limitations of our experience are related to the small sample size that may underpower the conclusions. Furthermore, patients were not randomly assigned to a control arm or placebo.
However, this is the first series of TUIA before RT was reported in literature. In our experience, this type of local anesthesia was safe and feasible. It shows full operative and postoperative pain control. Moreover, it allows a further shortening of hospitalization and treatment time.
Data availability
The original contributions presented in the study are included in the article. Further inquiries can be directed to the corresponding author.
References
McVary KT, Gittelman MC, Goldberg KA, Patel K, Shore ND, Levin RM, et al. Final 5-year outcomes of the multicenter randomized sham-controlled trial of a water vapor thermal therapy for treatment of moderate to severe lower urinary tract symptoms secondary to benign prostatic hyperplasia. J Urol. 2021;206:715–24.
Campobasso D, Siena G, Chiodini P, Conti E, Franzoso F, Maruzzi D, et al. Composite urinary and sexual outcomes after Rezum: an analysis of predictive factors from an Italian multi-centric study. Prostate Cancer Prostatic Dis. 2022.
Eredics K, Wehrberger C, Henning A, Sevcenco S, Marszalek M, Rauchenwald M, et al. Rezūm water vapor therapy in multimorbid patients with urinary retention and catheter dependency. Prostate Cancer Prostatic Dis. 2022;25:302–5. https://doi.org/10.1038/s41391-021-00462-w.
McVary KT, Holland B, Beahrs JR. Water vapor thermal therapy to alleviate catheter-dependent urinary retention secondary to benign prostatic hyperplasia. Prostate Cancer Prostatic Dis. 2020;23:303–8. https://doi.org/10.1038/s41391-019-0187-5.
Elterman D, Bhojani N, Vannabouathong C, Chughtai B, Zorn KC. Rezūm therapy for ≥80-mL benign prostatic enlargement: a large, multicentre cohort study. BJU Int. 2022;130:522–7.
Siena G, Tellini R, Cindolo L. Can Rezum stand out as the most versatile and better performing minimally invasive treatment for the management of LUTS related to BPH? Minerva Urol Nephrol. 2022;74:499–501.
Siena G, Cindolo L, Ferrari G, Maruzzi D, Fasolis G, Condorelli SV, et al. Water vapor therapy (Rezūm) for lower urinary tract symptoms related to benign prostatic hyperplasia: early results from the first Italian multicentric study. World J Urol. 2021;39:3875–80.
Schelin S. Transurethral resection of the prostate after intraprostatic injections of mepivacain epinephrine: a preliminary communication. Scand J Urol Nephrol. 2009;43:63–7.
Stenmark F, Brudin L, Stranne J, Peeker R. High-energy feedback microwave thermotherapy and intraprostatic injections of mepivacaine and adrenaline: an evaluation of calculated cell kill accuracy and responder rate. Scand J Urol. 2014;48:374–8.
Cindolo L, Ferrari R, Rabito S, Siena G, Spatafora P, Ferrari G. Rezum procedure with Exime® stent: a step forward to micro-invasiveness. Minerva Urol Nephrol. 2021;73:273–5.
Author information
Authors and Affiliations
Contributions
GS: project development, data collection, drafting of the manuscript. FS: critical revision of the manuscript, data collection. LC: critical revision of the manuscript, data collection.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Siena, G., Sessa, F. & Cindolo, L. Use of a Schelin Catheter for analgesia during Rezum treatment of the prostate. Prostate Cancer Prostatic Dis 27, 147–149 (2024). https://doi.org/10.1038/s41391-023-00644-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-023-00644-8