Abstract
Background
The increasing magnitude of the opioid crisis and rising rates of neonatal abstinence syndrome (NAS) diagnoses highlight the need for increased research into how maternal substance use during pregnancy can impact the neonatal immune profile and its functionality. We hypothesized that neonates with opioid exposure would have reduced proportions of some immune cells, an anti-inflammatory cytokine profile, reduced T cell proliferation, and monocyte bacterial killing activity compared to the control population.
Methods
The present study compares immune cell populations, inflammatory and anti-inflammatory cytokine and chemokine levels in the serum, and monocyte and T cell functional activity using umbilical cord samples from neonates with known opioid exposure during gestation and from control neonates without known exposure.
Results
Our findings demonstrated a significant reduction in neutrophils, decreased levels of inflammatory cytokines in the serum, and reduced IL-2 production during in vitro CD4+ T cell proliferation in neonates exposed to opioids compared to controls. The neutrophil findings were supported by retrospective analysis of an extended network of deidentified patient records.
Conclusions
This study is the first of its kind to evaluate differences in neonatal immunity as a result of opioid exposure in the human population that will inform continued mechanistic studies.
Impact
-
The opioid epidemic has become a public health crisis in the United States, and the corresponding incidence of neonatal abstinence syndrome (NAS) have risen accordingly.
-
New research is required to understand the short and long-term health impacts of opioid exposure to the neonate.
-
This is the first human study to investigate the immunologic profile and functionality in neonates with known opioid exposure in utero.
-
The abundance of neutrophils and the ratio of neutrophils to lymphocytes is significantly reduced along with inflammatory cytokines and chemokines following opioid exposure during pregnancy.
-
The immune profile in opioid-exposed neonates may promote susceptibility to infection.
Similar content being viewed by others
Introduction
Among the various social groups impacted by the opioid epidemic across the United States, rates of opioid use by pregnant women are rising alarmingly. Between 2000 and 2009, opioid use during gestation increased from 1.2 to 5.6 mothers per 1,000 live births.1 Concurrently, rates of neonatal abstinence syndrome (NAS), characterized by symptoms of withdrawal in newborns following in utero opioid exposure, have increased steeply. Incidence of NAS diagnosis was 1.2 neonates per 1000 live births in 2000, and 20 neonates per 1000 live births in 2016.1,2 While the illicit abuse of heroin has contributed to this increase, the use and misuse of prescription opioids, including buprenorphine, codeine, fentanyl, methadone, oxycodone, and morphine, are also substantial.3 A complex disorder, NAS can impact multiple systems in the newborn and require extensive hospitalization in neonatal intensive care units.1,4
With the rising incidence of NAS diagnoses, it is critical to elucidate the short-and long-term effects of the disorder. Some short-term neonatal outcomes described include premature delivery, low birth weight, jaundice, and feeding difficulties.4 Long-term outcomes are more scarcely documented but could include visual, motor, cognitive, behavioral, and infectious complications.5 Further, chart review studies have found increased diagnoses of general infectious and parasitic diseases among in utero opioid-exposed children in the first three years of life.6 Additional studies have found infectious causes to result in increased hospitalizations in the first three years of life among infants with NAS compared to those not diagnosed with NAS.7,8 Neonates have increased vulnerability and susceptibility to infection due to their developing immune system.9 Thus, we initiated the first comprehensive study of the impact of in utero opioid exposure on the neonatal immune profile and functionality.
Two separate studies investigated the hospital readmission of infants diagnosed with NAS and found that infectious etiologies were significant contributors.10,11 Furthermore, it is known that various immune cells, including lymphocyte and myeloid cell populations, express opioid receptors.12 Some research has investigated the impact of opioids on immunomodulatory processes, but these studies have primarily been in vitro or based on adult murine models in vivo. One investigation found significant decreases in the adult mouse serum concentrations of the pro-inflammatory cytokines interleukin (IL)-1β (IL-1β), IL-2, TNF-α, and IFN-γ and increases in the anti-inflammatory cytokines TGF-β1 and IL-10 after 24 h of treatment with heroin and morphine.13 Additionally, in vitro studies have identified deficits in monocyte chemotaxis, phagocytosis, oxidative burst, and neutrophil chemotaxis following opioid exposure.14,15,16,17 Since neonates are already limited in Th1 profiles with a Th2/T regulatory cell bias and have distinct functional differences compared to adult immune cells, additional opioid-driven deficits in immune function may significantly impact neonatal host response to infection and/or predispose to other immunological conditions.18,19,20 Thus, there is a critical need for a human neonate study to improve understanding of how the immune system is impacted following maternal opioid use during pregnancy. We sought to fill this gap in understanding.
Methods
Donor selection and blood collection
All donors were admitted to J.W. Ruby Memorial Hospital and provided informed consent under West Virginia University Institutional Review Board approval. All samples were deidentified upon collection. Umbilical cord blood was collected immediately following birth from male and female term neonates of mothers with and without known opioid use during pregnancy. Exclusion criteria included premature delivery, autoimmune diseases, and infectious diseases. We have classified the group without known opioid exposure as ‘control’. The study comprises a total of 30 donors (9 with known opioid exposure and 21 controls). The donor pool was split evenly by sex with 5 male and 4 female opioid-exposed donors; 11 control samples were male and 10 female. Donors in the control and opioid-exposed groups were born at a mean post-menstrual age of 39 weeks (range: 37–40 6/7 weeks for controls, 37–40 3/7 weeks for opioid-exposed). Donors in the control group had a mean birth weight of 3456 g (range: 2316–4445 g), while those in the opioid-exposed group had a mean birth weight of 3197 g (range: 2770–3720 g).
Sample preparation
Following collection, blood samples were immediately divided for subsequent experimental analysis. Prompt immunophenotyping required 1 mL of blood. Serum was obtained by centrifuging 3 mL of blood at 2,000 x g for 10 min and stored at −80 °C. Cord blood mononuclear cells (CBMCs) were isolated directly from the remaining volume of blood for use in monocyte killing and T cell proliferation assays as described previously.21
Immunophenotyping
To lyse erythrocytes, ammonium/chloride/potassium lysis buffer (ThermoFisher Scientific, Waltham, MA) was added to 1 mL of blood and incubated at room temperature for 15 min followed by centrifugation at 350 × g for 5 min. The remaining cells (105–106) were mixed with Fc receptor blocking reagent (Miltenyi Biotec, Bergisch Gladbach, Germany) and held at room temperature for 10 min prior to cell surface marker staining with fluorochrome-conjugated antibodies. Antibodies used for the panel included CD4-APC/Fire 750 (clone SK3) and CD16-Brilliant Violet 650 (clone 3G8) from BioLegend (San Diego, CA), CD25-ECD (clone B1.49.9), CD45-Pacific Blue (clone J33), HLA-DR-APC (clone Immu-357), CD127-APC/Alexa Fluor 700 (clone R34.34), CD8-PE (clone B9.11), CD14-PC5.5 (clone RMO52), CD56-PC7 (clone N901/NKH-1), CD19-FITC (clone J3-119) from Beckman Coulter (Brea, CA), and CD3-V500 (clone SP34-2) from BD Biosciences (Franklin Lakes, NJ). Immunolabeling was performed on a rotator for 30 min at room temperature protected from light. Cells were washed, resuspended in 4% paraformaldehyde (PFA; ThermoFisher Scientific), and stored at 4 °C until flow cytometric analysis. A control donor sample of CBMCs was prepared and stained with each single antibody in parallel with each composite donor analysis for use as a compensation control. All samples were analyzed on a LSRFortessa instrument (BD Biosciences) using FACS Diva version 8.0 software. A minimum of 30,000 events were analyzed per sample. Filter sets for each antibody analyzed are as follows: APC-Cy7 (651/779 nm excitation/emission), BV650 (405/645 nm ex/em), PE-Texas Red (567/615 nm ex/em), Pacific Blue (404/455 nm ex/em), APC (651/660 nm ex/em), Alexa Fluor 700 (696/719 nm ex/em), PE (566/574 nm ex/em), PE-Cy5.5 (566/671 nm ex/em), PE-Cy7 (566/778 nm ex/em), FITC (491/516 nm ex/em), and BV500 (415/500 nm ex/em). A schematic of the gating strategy used can be visualized in Supplementary Fig. 1.
Cytokine and chemokine profiling
Cytokine and chemokine profiling of donor sera was performed using multiplexed electrochemoluminescent detection reagents according to the manufacturer’s protocol (Meso Scale Discovery, Rockville, Maryland). The Human Pro-Inflammatory Panel 1 included the analytes IFN-γ, IL-1β, IL-2, IL-4, IL-6, IL-8, IL-10, IL-12p70, IL-13, and TNF-α. The Human Th17 Panel 1 included the analytes IL-17A Gen. B, IL-21, IL-22, IL-23, IL-27, IL-31, and MIP-3α. Protein concentrations were determined relative to standards assayed in parallel, and analyzed on a Meso QuickPlex SQ120 Reader.
In vitro monocyte killing assay
CD14+ monocytes were isolated from CBMCs using the human Miltenyi CD14+ isolation kit (Miltenyi Biotec) according to the manufacturer’s protocols. Automated magnetic separation was performed using an autoMACS Pro (Miltenyi Biotec). Monocytes (105 cells/well) were seeded in a black, clear-bottom 96-well cell culture plate (Eppendorf, Hamburg, Germany) and infected with Escherichia coli O1:K1:H7 that stably expresses luciferase as described previously.22 Luminescence readings were collected at 2, 4, 8, and 20 h post-gentamicin. Uninfected monocytes served as a negative control for background luminescence signal.
T cell proliferation assay
CD4+ T cells were isolated from CBMCs using the human Miltenyi CD4+ T Cell isolation kit (Miltenyi Biotec) following the manufacturer’s protocol. Automated magnetic separation was performed using an autoMACS Pro (Miltenyi Biotec). T cells were stained with CellTrace Violet (ThermoFisher Scientific) at 37 °C in 5% CO2 for 20 min as described previously.23 Staining was quenched by the addition of warmed 10% FBS in PBS. Cells were seeded in a 96-well cell culture plate (Corning, Corning, NY) in RPMI (VWR, Radnor, PA) supplemented with 10% human AB serum, 1 mM sodium pyruvate (ThermoFisher Scientific), 2 mM glutamine, 100 U/mL penicillin/streptomycin (ThermoFisher Scientific), 25 mM HEPES, and 0.05 mM mercaptoethanol (ThermoFisher Scientific), and incubated for 2 h at 37 °C. The T cells were stimulated with CD3/CD28 Dynabeads (ThermoFisher Scientific) at a ratio of 1 bead per 1 CD4+ T cell for 4 days. Beads were removed and the cells were resuspended in 4% PFA. Samples were analyzed on a LSRFortessa (BD Biosciences) using FACS Diva version 8.0 and FCS Express 6 (De Novo Software, Los Angeles, CA) software. Additionally, supernatants were collected each day of culture and analyzed using the human Ready-Set-Go! IL-2 ELISA (ThermoFisher Scientific) according to manufacturer’s instructions. Protein concentrations were determined relative to standards assayed in parallel.
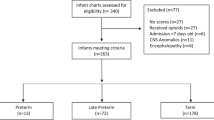
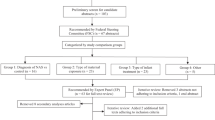
TriNetX
The TriNetX database, a large, network of deidentified electronic medical record data, allows for the scanning and collecting of information from over 50 different healthcare organizations across the United States and has been described previously.24 For the analysis presented here, two cohorts were generated and compared: infants less than 1 year of age with a diagnosis of NAS and infants less than 1 year of age that did not have a diagnosis of NAS. The ICD-10 diagnostic code for NAS is P96.1. Exploration of these cohorts allowed for comparison of demographics and blood laboratory values.
Statistical analysis
Statistical testing was performed using GraphPad Prism software version 9 (La Jolla, CA), R 4.1.1 (R Core Team, Vienna Austria), or the rms (Version 6.2-0) package. The threshold for statistical significance was set to alpha = 0.05. The details of the individual tests performed can be found in the figure legends.
Results
Immunophenotyping reveals a reduced population of neutrophils following in utero opioid exposure
To enumerate immune cell populations in control and opioid-exposed umbilical cord blood, we developed an 11-antibody flow cytometry panel and gating strategy (Supplementary Fig. 1). Immunophenotyping was performed on 18 total neonatal donors, including 9 with known in utero opioid exposure and 9 without known exposure. A total of 12 cell populations were measured for each donor, including total lymphocytes (sum of T and B cells), T cells, B cells, CD8+ T cells, CD4+ T cells, regulatory T cells (Tregs), neutrophils, eosinophils, natural killer (NK) cells, typical monocytes, intermediate monocytes, and atypical monocytes. Neutrophils and eosinophils were reported as a percentage of cells found in a high side scatter (SSChi) gate; the remainder of the cell populations are represented as a percentage of white blood cells (WBCs).
Among the populations analyzed, neutrophils were most impacted by opioid exposure with a significant decrease compared to the control group (Fig. 1g). Another granulocyte population with near significance were the increased proportion of eosinophils in the opioid-exposed group (Fig. 1h). In addition, there was a greater than twofold decrease in the percentage of typical monocytes in the group exposed to opioids during pregnancy (Fig. 1j). Though the differences did not achieve statistical significance, the increases in the proportions of total lymphocytes (Fig. 1a), T cells (Fig. 1b), and CD8+ T cells (Fig. 1d) per total WBCs are interesting and worthy of consideration for future investigation with expanded donor cohorts. Robust differences between the proportions of B cells, CD4+ T cells, Tregs, NK cells, intermediate monocytes, and atypical monocytes to total WBCs were not observed between the control and opioid groups.
Umbilical cord blood samples from 9 opioid-exposed donors and 9 control donors were used to characterize 12 immune cell populations. Total lymphocytes (a), T cells (b), B cells (c), CD8+ T cells (d), CD4+ T cells (e), regulatory T cells (f), NK cells (i), typical monocytes (j), intermediate monocytes (k), and atypical monocytes (l) are reported as the median with interquartile range or mean percentages of total white blood cells ± SE (j) for each study group. Neutrophils (g) and eosinophils (h) are reported as the median with interquartile range of total single scatter high (SSChi) cells for each study group. Group comparisons were made using Mann Whitney U test for non-parametric, unpaired testing (A-L, G-H) or unpaired, parametric t tests (j) as appropriate with statistical significance reported at the 95% confidence level (p < 0.05).
Neutrophil-to-lymphocyte ratios (NLR) have been used extensively in clinics as biomarkers for disease severity, with higher ratios usually associated with more severe inflammation and disease outcome.25,26,27 To determine whether opioid exposure affected NLRs in neonates, we performed a secondary analysis of cell populations that revealed a decreased NLR in the opioid-exposed group (Fig. 2a). To better understand the driving factor involved with this difference, additional ratios were compared, including a neutrophil to T cell ratio that was borderline significant (p = 0.0583), neutrophil to B cell ratio, neutrophil to CD8+ T cell ratio that was significantly different between groups (p = 0.040), and neutrophil to CD4+ T cell ratio (Fig. 2b–e). From these data, it is expected that reduced neutrophils and elevated CD8+ T cells most strongly characterized the opioid-exposed group compared to controls.
The neutrophil to lymphocyte ratio (NLR) (a), neutrophil to T cell ratio (b), neutrophil to B cell ratio (c), neutrophil to CD8+ T cell ratio (d), and neutrophil to CD4+ T cell ratio (e), was calculated and compared between study groups. Pairwise comparisons were made using unpaired, parametric t tests (a, b) or Wilcoxon rank-sum test (c–e) as appropriate with statistical significance reported at the 95% confidence level (p < 0.05). Data are reported as median with interquartile range (a, b) or the mean ± SE (c–e).
Opioid-exposed neonates have reduced serum concentrations of inflammatory cytokines
Since we determined there were differences in some important immune cell subsets in opioid-exposed neonates, we next wanted to analyze the cytokine and chemokine levels in opioid-exposed and control neonates. Both inflammatory and anti-inflammatory cytokine and chemokine concentrations in the serum (21 control, 9 opioid-exposed) were measured by electrochemiluminescent multiplex assay. The Pro-Inflammatory MSD panel analysis showed significant reductions in the levels of IL-10 (p = 0.039), IL-12p70 (p = 0.0039), IL-1β (p = 0.0039), IL-2 (p = 0.039), IL-4 (p = 0.0039), and IL-6 (p = 0.039) in the opioid group, represented as a decrease in the percent change relative to the control (Table 1, Fig. 3a). Additionally, an assessment of Th17-associated analytes demonstrated significant reductions in IL-22 (p = 0.039), IL-23 (p = 0.0039) and IL-31 (p = 0.0039) in the opioid group (Table 1, Fig. 3b). Collectively, this analysis demonstrates an environment that is less inflammatory and immune responsive following exposure to opioids in utero.
The concentration of individual cytokines and chemokines in the pro-inflammatory (a) or Th17 (b) MSD panel was measured in the serum by chemiluminescent multiplex assay as described in the “Methods”. The percent change of each opioid-exposed donor measurement was calculated relative to the control donor group mean. Data are reported as the median with interquartile range. Statistical significance at the 95% confidence interval was determined using one-sample sign test. *p < 0.05; **p < 0.01; ***p < 0.001; ****p < 0.0001. N = 30 donors (9 opioid, 21 control).
The ability of individual monocytes to kill bacteria was not affected by opioids
To determine whether opioid exposure affected the ability of neonatal immune cells to combat bacterial infection, we isolated CD14+ monocytes from opioid-exposed and control neonates. Using a previously described gentamicin protection assay, the ability of monocytes to kill E. coli O1:K1:H7 that stably expresses luciferase was measured.28,29 There were no significant differences in the ability of phagocytes from the respective donor groups to kill bacteria at 2, 4, 8, or 20 h post gentamicin (Fig. 4). However, RLU measurements and the corresponding percent viable bacteria values did decrease over time (p < 0.0001) with nearly all bacteria being killed by 20 h in both groups (Fig. 4). These results suggest that opioid exposure in utero did not have an effect on the ability of monocytes to kill bacteria.
CD14+ monocyte killing of luminescent E. coli O1:K1:H7 was measured in culture over time as described in the Methods. The percent viable bacteria were calculated by finding the proportion of relative luminescent units (RLU) at 2, 4, 8, and 20 h post-gentamicin treatment to the RLU reading immediately following 2 h of gentamicin treatment. Statistical testing was performed on control and opioid-exposed data by two-way repeated-measures ANOVA with Tukey’s multiple comparisons. Data are reported as the mean ± SE. N = 20 donors (7 opioid, 13 control).
Opioid exposure may have an impact IL-2 signaling mechanisms and T cell proliferation
Chronic opioid exposure has been shown to reduce T cell activity in adult mice.30 However, little is known about the effects of opioids on the proliferative mechanisms of these cells in human neonates. To address this gap in understanding, opioid-exposed (n = 8) and control (n = 12) CD4+ T cells were isolated, stained, and stimulated to proliferate using T activator CD3/CD28 DynaBeads™ for 4 days. Supernatants were collected each day to measure IL-2 production, and cells were fixed on day 4 for flow cytometric analysis of proliferation. Fig. 5a is a representative panel from a control donor; cells left unstained served as a negative control (blue) and those stained and fixed prior to stimulation serve as the time 0 no proliferation control (red). Flow cytometric data analyzed in FCS Express software generated a proliferative index value for each donor that was significantly different between opioid-exposed and controls in this proliferative index calculation (Fig. 5b). However, IL-2 analysis from each day in culture demonstrated a significant increase in the levels of IL-2 in the opioid-exposed group at day 2 post-stimulation compared to controls (Table 2, Fig. 5c). These data suggest that there could be an opioid-specific influence on the magnitude of IL-2 production during T cell proliferation.
CD4+ T cells were isolated and stimulated to proliferate in vitro as described in the “Methods”. a A representative proliferation histogram for control donor analyzed by flow cytometry is shown. Unstained T cells are shown in blue. T cells stained with CellTrace Violet but not stimulated are shown in red. Proliferative generations of stained T cells are indicated by distinct peaks in black. b Proliferative indices were calculated using FACSDiva software. Statistical testing of the mean ± SE was performed using an unpaired, parametric t test. c Supernatant from each day of culture was collected and the IL-2 concentration was measured by ELISA. The percent change in the opioid-exposed samples from the mean control IL-2 levels for each day was calculated and displayed as the mean ± SE. Statistical significance was determined in the 95% confidence interval using a one-sample t test; Asterisk represents p < 0.05. N = 20 donors (8 opioid, 12 control).
A large nationwide patient cohort analysis demonstrates a deficiency in neutrophils associated with NAS
To determine whether our immunological data is supported by trends in available clinical data, we utilized the TriNetX health research network to generate two patient cohorts across approximately 50 healthcare organizations in the United States. The first population consisted of individuals under 1 year of age that have been diagnosed with NAS (ICD-10 code P96.1; n = 913). The second population consisted of individuals under 1 year of age that had not been diagnosed with NAS (n = 431,451). Within both cohorts, individuals with detected lab values of interest were identified and compared. Similar to our smaller local patient cohort, neutrophils significantly reduced by approximately five-fold in the opioid-exposed group compared with the control population (Fig. 6c). In addition, a secondary analysis revealed that the ratio of immature granulocytes to total neutrophils was increased in NAS-diagnosed neonates (Supplementary Table 1). Immature to total neutrophil ratio (I/T ratio) has been proposed as a marker for early detection of neonatal sepsis, in which an increase in I/T ratio is a reasonable predictor of positive blood culture (sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of I/T ratio were 76.47%, 83.82%, 54.16%, and 93.44%, respectively), especially when used in conjunction with C-reactive protein (CRP) values.31 Our TriNetX data therefore suggests that NAS-diagnosed neonates may be at an increased risk for infection. There were no statistically significant differences between other cell populations or findings (Fig. 6). It is important to acknowledge that the TriNetX database does not permit search criteria narrower in age than under 1 year. However, a strength of this analysis is the documented NAS diagnosis that extends beyond opioid exposure. These data further speak to longer-term consequences of opioid exposure during pregnancy and suggest a prolonged neutrophil deficiency with important implications in host response to infection.
The TriNetX health research network database provided laboratory findings for individuals under 1 year of age with (n = 913) or without (n = 431,451) NAS diagnosis. Laboratory values included leukocytes (a), lymphocytes (b), neutrophils (c), eosinophils (d), monocytes (e), and C-reactive protein (f). Group comparisons were made using unpaired, parametric Welch’s t tests with statistical significance reported in the 95% confidence level (p < 0.05). Data is reported as the mean ± SE.
Discussion
In this study, we characterized the differences in immune profiles and functionality between newborns with known in utero opioid exposure and newborns without this exposure. The neonatal period is unique with a skew toward a Th2 and Treg profile along with increased abundance of anti-inflammatory cytokines compared to other age groups.32 Some published studies have focused on maternal alcohol use and risk of infection in the neonate.33,34 However, there is currently no published research addressing the impact of maternal opioid use on neonatal immunity. This is an alarming knowledge gap considering the increasing magnitude of the opioid epidemic and rising NAS diagnoses. Our study is the first of its kind to address this scientific void.
One of the intriguing findings that emerged from our study was the reduction in neutrophil counts observed in neonates exposed to opioids in utero. This was supported by an extensive number of infant medical records that included neutrophil values with a NAS diagnosis. This is particularly significant as newborns do not have developed adaptive immune responses and must rely heavily on neutrophils as a key innate effector.35 When considered with the trending reduction in monocytes in neonates with opioid exposure, a deficiency in circulating phagocytic responders may promote heightened susceptibility to infection. Additionally, of note was the trending elevation in eosinophils in the opioid-exposed group. Eosinophilia is associated with infection and stress during the neonatal period.36 Elevated eosinophil numbers are also triggered in adults exposed to opioids and has been associated with respiratory distress and pneumonia.37,38 The imbalance of granulocyte populations may have implications in the response to infection with susceptibility further heightened considering the already unique immune profile of a healthy neonate.39
We found the NLR, a biomarker for systemic inflammation, to be decreased in neonates exposed to opioids.40 This suggests that inflammation may be reduced in these patients, a finding supported by significant reductions in numerous cytokines. Additionally, opioids may promote an inability to respond to immunologic stimuli at the same magnitude. It is interesting that the anti-inflammatory cytokine IL-10 is also decreased alongside pro-inflammatory cytokines in our study. However, this is consistent with the role of IL-10 as an immunoregulator to balance the effects of inflammation.41 Studies in mice lacking IL-10 show that inflammation (specifically neuroinflammation) is enhanced compared to mice that can produce IL-10.42
In addition to measuring immune cell populations and cytokine and chemokine levels, we performed functional assays to compare cellular activities. Our bacterial clearance assay did not demonstrate a difference in the ability of monocytes to kill bacteria on a per cell basis between study groups. However, it is worth noting that our assay did not specifically compare rates of phagocytosis between study groups. Defects in uptake of bacteria by monocytes or granulocytic cells is possible. CD4+ T cells did not exhibit a difference in the capacity to proliferate in vitro. However, additional functional assays are warranted; overall qualitative functionality (i.e. IFN-γ, TNF-α, or IL-4 production) may differ. IL-2 concentration has been shown to correlate with T cell expansion.43 Therefore, since the increase in IL-2 was observed at day 2 in the opioid-exposed group, it is possible that proliferation indices at day 3 (rather than day 4) would demonstrate an increase compared with control that is compensated for over time in vitro. However, the in vivo environment may enhance a response that is minimized during the controlled environment in vitro. While some benefits of enhanced T cell proliferation could be rationalized, it is also possible that a predisposition to autoimmunity or exaggerated responsiveness during some conditions may result.
A limitation of this study is the size of the donor pool. If the sample size were further increased in subsequent analyses, it is possible that some trends may achieve enhanced statistical significance. It is also important to note that different types of opioids may vary in their ability to impact the immune system.44 Of the 9 opioid-exposed neonates studied in this body of work, 8 were exposed to buprenorphine, with an additional donor exposed to methadone. Although it is possible that results may vary for other opioids, it could also be considered a strength of our study that the opioid exposure was consistent. Additionally, the influence of other maternal factors cannot be excluded. For example, while our exclusion criteria included premature delivery, autoimmune diseases, and infectious disease, there are certainly other maternal and neonatal factors that could impact the composition and functionality of the neonatal immune system.
While limitations of this study have been discussed, it is also important to emphasize some very notable strengths. First, this study is the first to disseminate findings regarding the impact of opioids on the neonatal immune system. As such, even where there are not significant differences in profiles or activity levels observed between study groups, this observation in and of itself is novel. It is equally informative that there are no differences in CD4+ cells as it is that neutrophil levels are different. An additional strength is that we profiled at essentially the first moments of life before ex utero signals reshape the immune profile. Lastly, it was a significant strength of the study that the TriNetX data supported a key finding of reduced neutrophil levels in infant patients diagnosed with NAS and an extension of that observation with an elevated I/T ratio in the same population. These findings represented in an extensive network of patients across the U.S. validate observations obtained from our local donor pool.
It is tempting to speculate on mechanisms that may contribute to altering the immune environment. Our findings suggest the possibility of a direct influence of opioids on myeloid and lymphocyte precursors. Opioid exposure may also influence cell signaling downstream of opioid receptors that alters cytokine expression and signaling. β-arrestins downstream of the μ-opioid receptor function as a scaffold for recruitment of other molecules involved in signaling cascades.45 Interaction with β-arrestin 2 has been shown to prevent phosphorylation and degradation of IκBα which can prevent activation of NF-κB target genes.46,47 This is consistent with our serum cytokine data. An epigenetic reprogramming of some immune cells and immature progenitors is another possibility. Stable epigenetic modification to DNA has been reported following persistent opioid use, although not with neonatal cells.48 This also ushers in the requirement for duration of exposure. Some opioid-induced alterations may result from an epigenetic pre-programming of the cell, whereas others may require active opioid exposure and engagement of corresponding receptors. It is worth noting that although our findings regarding monocyte killing and T cell differentiation did not yield significant differences between study groups, these assays were performed in vitro in the absence of opioid exposure.
In summary, we have to our knowledge provided the first comprehensive report that describes the influence of opioid exposure during pregnancy on the neonatal immune profile. Continued mechanistic studies are necessary to further understand opioid influences on the immune response. Relevant findings have implications in pharmaceutical development and obstetrics/pediatric care.
Conclusions
To our knowledge, this is the first study to the influence of opioid exposure during pregnancy on the immune profile and functionality in human neonates. We have described notable reductions in neutrophil counts, altered neutrophil to T cell ratio, depleted levels of inflammatory mediators, and time-dependent IL-2 cytokine levels during in vitro CD4+ T cell proliferation. Neutrophil findings were corroborated by a larger cohort health record analysis. These preliminary findings can be used to guide future mechanistic studies to further elucidate the impact of opioid exposure on neonatal immunity.
References
Kocherlakota, P. Neonatal abstinence syndrome. Pediatrics 134, e547–e561 (2014).
Wachman, E. M., Schiff, D. M. & Silverstein, M. Neonatal abstinence syndrome: advances in diagnosis and treatment. JAMA 319, 1362–1374 (2018).
Anbalagan, S. & Mendez, M. D. in Statpearls (StatPearls Publishing Copyright © 2021, StatPearls Publishing LLC., 2021).
McQueen, K. & Murphy-Oikonen, J. Neonatal abstinence syndrome. N. Engl. J. Med. 375, 2468–2479 (2016).
Maguire, D. J. et al. Long-term outcomes of infants with neonatal abstinence syndrome. Neonatal Netw. 35, 277–286 (2016).
Arter, S., Lambert, J., Brokman, A. & Fall, N. Diagnoses during the first three years of life for children with prenatal opioid exposure and neonatal abstinence syndrome using a large maternal infant data hub. J. Pediatr. Nurs. 61, 34–39 (2021).
Ko, J. Y. et al. Maternal opioid exposure, neonatal abstinence syndrome, and infant healthcare utilization: a retrospective cohort analysis. Drug Alcohol Depend. 223, 108704 (2021).
Milliren, C. E., Melvin, P. & Ozonoff, A. Pediatric hospital readmissions for infants with neonatal opioid withdrawal syndrome, 2016-2019. Hosp. Pediatr. 11, 979–988 (2021).
Basha, S., Surendran, N. & Pichichero, M. Immune responses in neonates. Expert Rev. Clin. Immunol. 10, 1171–1184 (2014).
Uebel, H. et al. Reasons for rehospitalization in children who had neonatal abstinence syndrome. Pediatrics 136, e811–e820 (2015).
Witt, C. E. et al. Neonatal abstinence syndrome and early childhood morbidity and mortality in washington state: a retrospective cohort study. J. Perinatol. 37, 1124–1129 (2017).
Ninković, J. & Roy, S. Role of the mu-opioid receptor in opioid modulation of immune function. Amino Acids 45, 9–24 (2013).
Pacifici, R., di Carlo, S., Bacosi, A., Pichini, S. & Zuccaro, P. Pharmacokinetics and cytokine production in heroin and morphine-treated mice. Int. J. Immunopharmacol. 22, 603–614 (2000).
Menzebach, A. et al. [Morphine inhibits complement receptor expression, phagocytosis and oxidative burst by a nitric oxide dependent mechanism]. Anasthesiol. Intensivmed. Notfallmed. Schmerzther. 39, 204–211 (2004).
Miyagi, T. et al. Opioids suppress chemokine-mediated migration of monkey neutrophils and monocytes - an instant response. Immunopharmacology 47, 53–62 (2000).
Pérez-Castrillón, J. L., Pérez-Arellano, J. L., García-Palomo, J. D., Jiménez-López, A. & De Castro, S. Opioids depress in vitro human monocyte chemotaxis. Immunopharmacology 23, 57–61 (1992).
Yossuck, P., Nightengale, B. J., Fortney, J. E. & Gibson, L. F. Effect of morphine sulfate on neonatal neutrophil chemotaxis. Clin. J. Pain 24, 76–82 (2008).
Kim, S. K., Keeney, S. E., Alpard, S. K. & Schmalstieg, F. C. Comparison of L-selectin and Cd11b on neutrophils of adults and neonates during the first month of life. Pediatr. Res. 53, 132–136 (2003).
Le Garff-Tavernier, M. et al. Human Nk cells display major phenotypic and functional changes over the life span. Aging Cell 9, 527–535 (2010).
Velilla, P. A., Rugeles, M. T. & Chougnet, C. A. Defective antigen-presenting cell function in human neonates. Clin. Immunol. 121, 251–259 (2006).
Kraft, J. D. et al. Neonatal macrophages express elevated levels of interleukin-27 that oppose immune responses. Immunology 139, 484–493 (2013).
Seman, B. G., Povroznik, J. M., Vance, J. K., Rawson, T. W. & Robinson, C. M. A neonatal imaging model of gram-negative bacterial sepsis. J. Vis. Exp. 162, e61609 (2020).
Seman, B. G., Vance, J. K., Akers, S. M. & Robinson, C. M. Neonatal low-density granulocytes internalize and kill bacteria but suppress monocyte function using extracellular DNA. J. Cell. Sci. 134, jcs252528 (2021).
Topaloglu, U. & Palchuk, M. B. Using a federated network of real-world data to optimize clinical trials operations. JCO Clin. Cancer Inf. 2, 1–10 (2018).
Alkhatip, A. et al. The diagnostic and prognostic role of neutrophil-to-lymphocyte ratio in Covid-19: a systematic review and meta-analysis. Expert Rev. Mol. Diagn. 21, 505–514 (2021).
Hessami, K. et al. Gestational diabetes mellitus and inflammatory biomarkers of neutrophil-lymphocyte ratio and platelet-lymphocyte ratio: a systematic review and meta-analysis. Biomarkers 26, 491–498 (2021).
Song, M., Graubard, B. I., Rabkin, C. S. & Engels, E. A. Neutrophil-to-lymphocyte ratio and mortality in the United States general population. Sci. Rep. 11, 464 (2021).
Gleave Parson, M. et al. Murine myeloid-derived suppressor cells are a source of elevated levels of interleukin-27 in early life and compromise control of bacterial infection. Immunol. Cell Biol. 97, 445–456 (2019).
Seman, B. G. et al. Elevated levels of interleukin-27 in early life compromise protective immunity in a mouse model of gram-negative neonatal sepsis. Infect. Immun. 88, e00828-19 (2020).
Carpenter, G. W., Breeden, L. & Carr, D. J. Acute exposure to morphine suppresses cytotoxic T-lymphocyte activity. Int. J. Immunopharmacol. 17, 1001–1006 (1995).
Saboohi, E., Saeed, F., Khan, R. N. & Khan, M. A. Immature to total neutrophil ratio as an early indicator of early neonatal sepsis. Pak. J. Med. Sci. 35, 241–246 (2019).
Tsafaras, G. P., Ntontsi, P. & Xanthou, G. Advantages and limitations of the neonatal immune system. Front. Pediatr. 8, 5 (2020).
Gauthier, T. W. Prenatal alcohol exposure and the developing immune system. Alcohol Res. 37, 279–285 (2015).
Gauthier, T. W., Drews-Botsch, C., Falek, A., Coles, C. & Brown, L. A. Maternal alcohol abuse and neonatal infection. Alcohol Clin. Exp. Res. 29, 1035–1043 (2005).
Lawrence, S. M., Corriden, R. & Nizet, V. Age-appropriate functions and dysfunctions of the neonatal neutrophil. Front. Pediatr. 5, 23 (2017).
Juul, S. E., Haynes, J. W. & McPherson, R. J. Evaluation of eosinophilia in hospitalized preterm infants. J. Perinatol. 25, 182–188 (2005).
Eyüpoğlu, D., Ortaç Ersoy, E., Rollas, K. & Topeli, A. Acute eosinophilic pneumonia secondary to heroin inhalation. Tuberk. Toraks 65, 154–156 (2017).
Korpole, P. R., Al-Bacha, S. & Hamadeh, S. A case for biopsy: injectable naltrexone-induced acute eosinophilic pneumonia. Cureus 12, e10221 (2020).
Simon, A. K., Hollander, G. A. & McMichael, A. Evolution of the immune system in humans from infancy to old age. Proc. Biol. Sci. 282, 20143085 (2015).
Barker, T., Fulde, G., Moulton, B., Nadauld, L. D. & Rhodes, T. An elevated neutrophil-to-lymphocyte ratio associates with weight loss and cachexia in cancer. Sci. Rep. 10, 7535 (2020).
Iyer, S. S. & Cheng, G. Role of interleukin 10 transcriptional regulation in inflammation and autoimmune disease. Crit. Rev. Immunol. 32, 23–63 (2012).
Weston, L. L., Jiang, S., Chisholm, D., Jantzie, L. L. & Bhaskar, K. Interleukin-10 deficiency exacerbates inflammation-induced tau pathology. J. Neuroinflammation 18, 161 (2021).
Ghaffari, S. et al. Optimizing interleukin-2 concentration, seeding density and bead-to-cell ratio of T-cell expansion for adoptive immunotherapy. BMC Immunol. 22, 43 (2021).
Boland, J. W., Foulds, G. A., Ahmedzai, S. H. & Pockley, A. G. A preliminary evaluation of the effects of opioids on innate and adaptive human in vitro immune function. BMJ Support Palliat. Care 4, 357–367 (2014).
Ma, L. & Pei, G. Beta-arrestin signaling and regulation of transcription. J. Cell Sci. 120, 213–218 (2007).
Gao, H. et al. Identification of beta-arrestin2 as a G protein-coupled receptor-stimulated regulator of Nf-Kappab pathways. Mol. Cell 14, 303–317 (2004).
Witherow, D. S., Garrison, T. R., Miller, W. E. & Lefkowitz, R. J. Beta-arrestin inhibits Nf-kappab activity by means of its interaction with the Nf-kappaB inhibitor ikappaBalpha. Proc. Natl. Acad. Sci. USA 101, 8603–8607 (2004).
Nestler, E. J. Epigenetic mechanisms of drug addiction. Neuropharmacology 76, 259–268 (2014).
Acknowledgements
We thank the staff of J.W. Ruby Memorial Hospital and West Virginia University Medicine’s obstetrics and gynecology providers and specialists for their support in this study. This work was supported by the National Institute of General Medical Sciences, U54GM104942. We acknowledge additional funding support provided to the West Virginia University Flow Cytometry and Single Cell Core Facility by the following grants: WV CTSI grant GM104942, Tumor Microenvironment CoBRE grant GM121322 and NIH grant OD016165.
Author information
Authors and Affiliations
Contributions
All authors have met the Pediatric Research authorship requirements. Conceived and designed the study: S.M.A. and C.M.R. Developed the study protocol: S.M.A., K.B., and C.R. Screened and enrolled patients: S.M.A. Collected clinical data and samples: S.M.A. Performed laboratory experiments: N.W.M. and B.G.S. Analyzed the data: N.W.M., B.G.S., J.M.P. W.F, and C.R. Drafted the manuscript: N.M., B.S., and C.R. Critically reviewed, edited, and approved the manuscript: all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Informed consent
Written informed consent was obtained from pregnant mothers prior to participation in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Miller, N.W., Seman, B.G., Akers, S.M. et al. The impact of opioid exposure during pregnancy on the human neonatal immune profile. Pediatr Res 92, 1566–1574 (2022). https://doi.org/10.1038/s41390-022-02014-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02014-x