Abstract
Anhedonia is a cardinal characteristic of depression which predicts worse treatment outcome and is among the most common residual symptoms following treatment. Behavioral Activation (BA) has been shown to be an effective treatment for depressed adults, and more recently, depressed adolescents. Given its emphasis on systematically and gradually increasing exposure to and engagement with rewarding activities and experiences, BA may be a particularly effective intervention for adolescents experiencing anhedonia and associated reward system dysfunction. In the present study, anhedonic adolescents (AA; n = 39) received 12 weekly sessions of BA and completed a multimodal (i.e., neural, behavioral, and self-report [ecological momentary assessment]) assessment of reward function at pre-treatment and post-treatment (as well as weekly self-report assessments of anhedonia). Typically developing adolescents (TDA; n = 41) completed the same measures at corresponding timepoints. Multilevel models tested pre-treatment reward-related predictors of anhedonia improvement, as well as change in reward measures over the course of BA. Analyses revealed significant reductions in anhedonia following BA treatment. Enhanced pre-treatment neural (striatal) reward responsiveness predicted greater anhedonia improvement. In contrast, baseline self-report and behavioral reward measures did not predict treatment outcome. A group x time interaction revealed greater increases in both reward- and loss-related neural responsiveness among AA relative to TDA adolescents. Consistent with a capitalization (rather than compensatory) model, pre-treatment neural – but not self-report or behavioral – measures of relatively enhanced reward responsiveness predicted better BA outcome. In addition to alleviating anhedonia, successful BA may also increase neural sensitivity to affectively salient (e.g., reward- and loss-related) stimuli among anhedonic youth.
Similar content being viewed by others
Introduction
Depression rates surge during the adolescent years, and by age 18, approximately 15% of youth will have developed major depressive disorder (MDD) [1]. A range of empirically supported interventions are available for depressed adolescents, including psychotherapeutic (e.g., Cognitive Behavioral Therapy; CBT) and pharmacological (e.g., Selective Serotonin Reuptake Inhibitors; SSRIs) treatment options. However, rates of non-response remain high, with approximately 40–50% of depressed adolescents failing to respond to these interventions [2,3,4]. Anhedonia (i.e., loss of interest or pleasure) is a core characteristic of depression experienced by at least 50% of depressed adolescents [5, 6], which predicts both worse treatment outcome [7, 8] and elevated risk of suicide attempt [9], and is among the most common residual symptoms following pharmacotherapy or psychotherapy [10,11,12]. Common antidepressants not only have modest effects on anhedonia but may even worsen positive affect and reward responsiveness in some individuals [13,14,15]. Of relevance, a recent re-analysis of two randomized clinical trials revealed that for depressed individuals treated with CBT or an SSRI, post-treatment deficits in positive emotions were substantially more common than residual negative affect [11]. Paralleling these findings, a recent neuroimaging study in depressed adolescents found that a course of CBT reduced neural hypersensitivity to negative stimuli but did not improve neural response to rewards [16]. In summary, our first-line treatments for depressed youth (e.g., CBT and SSRIs) fail to adequately target and alleviate anhedonia and underlying reward circuitry deficits, which may help account for their high treatment non-response rates.
Behavioral Activation (BA) is a brief behavioral intervention with accumulating evidence indicating that it significantly reduces depressive symptoms in adults [17,18,19] and adolescents [20,21,22]. BA focuses on gradually and systematically increasing exposure to and engagement with rewarding activities and experiences [23, 24]. In contrast to CBT, which focuses on identifying and changing negative patterns of thinking and behaviors that contribute to depression, BA is a relatively simpler approach which focuses specifically on modifying behaviors that contribute to the maintenance of depressive symptoms (e.g., social withdrawal, reduced engagement with activities that provide pleasure and/or a sense of accomplishment). The BA therapist works collaboratively with the client to help them counteract maladaptive avoidance patterns and to gradually re-engage with intrinsically rewarding and positively reinforcing activities. Given this emphasis, BA may be particularly effective at improving anhedonia and associated reward system dysfunction [18]. It is important to note that BA is a foundational component of CBT, and may, on average, play a greater role in contributing to depressive symptom change in adolescents relative to cognitive strategies [25].
Self-report anhedonia measures (e.g., the commonly used Snaith Hamilton Pleasure Scale; SHAPS) [26, 27] can assess the extent to which a given intervention successfully reduces anhedonia in adolescents. Beyond self-reported symptom change, BA may also help normalize neural and behavioral reward-related deficits which underlie anhedonia. More specifically, adolescents with elevated depression and anhedonia have been shown to have blunted response to rewards in the brain’s core reward circuitry, in particular the ventral (i.e., nucleus accumbens [NAcc]) and dorsal striatum (i.e., caudate, putamen) [28,29,30,31,32,33]. Moreover, a pattern of medial prefrontal cortex (mPFC) hyperreactivity during reward processing has also been observed among depressed relative to non-depressed adolescents [34]. In addition to concurrent associations, blunted striatal and heightened mPFC activation have been shown to prospectively predict future depressive symptoms in adolescents [35,36,37].
In addition to neural (i.e., striatal and mPFC) reward-related abnormalities, depression and, especially, anhedonia have also been linked to aberrant behavioral responses to reward. In particular, blunted reward learning (i.e., the ability to modify behavior based on past rewards) has been observed in both depressed and anhedonic participants relative to healthy controls [38,39,40], as well as never-depressed adolescents who are at elevated risk of developing depression (by virtue of a parental history of the disorder) [41]. A very commonly used task to assess reward learning is the Probabilistic Reward Task (PRT), which is designed to provide an objective measure of anhedonic behavior [28, 38, 42]. In adult samples, performance on the PRT has been found to: (1) correlate with current and predict future anhedonic symptoms [38,39,40], (2) correlate with mPFC and striatal activation to rewards as well as extrastriatal dopamine release [43, 44]; and (3) predict treatment outcome [40]. Importantly, the PRT has also been validated in youth as a measure of responsiveness to rewards [41, 45,46,47]. The extent to which a depressed or anhedonic adolescent is sensitive to rewards (as indexed by the PRT) may improve over the course of BA, given that this treatment specifically focuses on increasing exposure to and engagement with rewarding activities and experiences.
The present study
The present study recruited a sample of adolescents known to be at elevated risk of poor treatment outcome (i.e., with high levels of anhedonia) who were then enrolled in a 12-week BA trial with a multimodal (i.e., self-report, neural and behavioral) assessment of changes in anhedonia and reward system function. The overarching goal of this study was to address two related questions. First, do individuals with relatively high levels of anhedonia and associated reward system dysfunction derive greater benefit from BA than those with more intact reward function? According to a compensatory model, BA may be better suited to anhedonic individuals given that it may specifically target and improve deficits in reward function [18]. Framed from the perspective of the National Institute of Mental Health’s (NIMH) emphasis on experimental therapeutics [48], BA may directly engage and modify the “target” (i.e., underlying mechanism) of blunted reward system function (e.g., reduced striatal response to rewards) and thus may be particularly well-suited for individuals who enter treatment with greater deficits in this domain. Conversely, a capitalization model argues the opposite: Individuals with relatively intact reward system function may best be able to take advantage of an intervention that capitalizes on their existing strengths. For example, adolescents with elevated depressive or anhedonic symptoms but relatively intact positive affect (assessed via self-report) or greater sensitivity to rewards (assessed via a neural [e.g., striatal response to reward-related stimuli] or behavioral [e.g., PRT] task) may be better able to successfully engage with and take advantage of the reward-focused activities of BA
The evidence supporting compensatory vs. capitalization models is mixed, and no study has been conducted with adolescents receiving BA. In support of a compensatory model, an initial small study [49] in adults with (n = 12) vs. without (n = 15) MDD reported pre- to post-treatment increases (i.e., in the direction of normalization) in neural response to rewards in reward-related regions (e.g., dorsal striatum) among MDD participants who received BA. Of relevance, two electroencephalogram (EEG) studies in adults with anxiety and/or depression reported that blunted pre-treatment neural response to rewarding outcomes (but not the anticipation of rewards [50]) predicted greater depressive symptom improvement to CBT [50] and SSRI [51]. In contrast, other CBT studies [16, 52, 53], a trial of CBT vs. supportive therapy [54], as well as one study of the transdiagnostic Unified Protocol [55] yielded findings consistent with a capitalization model, such that patients who received a treatment matched to their relative strengths had the best outcomes. Notably, of the abovementioned studies that tested pre-treatment neural predictors of treatment outcome, all found evidence of neural response to rewarding outcomes predicting symptom improvement [16, 50, 51, 54]. Informed by these prior findings, we tested whether baseline self-report (ecological momentary assessment; EMA), neural and behavioral reward measures predicted improvement in anhedonia among anhedonic adolescents receiving BA. Given the limited and mixed evidence across existing studies (none of which focused on BA for adolescents), and the fact that both the compensatory and capitalization models provide equally compelling and plausible perspectives, we did not have a hypothesis about the direction of these effects (i.e., whether relatively blunted or heightened reward responsiveness would predict better BA outcomes for anhedonic adolescents).
Finally, and relatedly, we also tested the extent to which a course of BA was associated with pre- to post-treatment changes in self-report, neural and behavioral measures of reward function in anhehonic adolescents. We hypothesized that a 12-week course of BA would be associated with significant changes in self-report (i.e., decreased anhedonia), neural (i.e., increased striatal and decreased mPFC response to rewards) and behavioral (i.e., increased reward learning on the PRT) measures of reward function.
Methods and materials
Participants
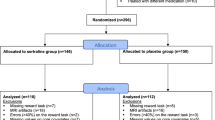
Adolescents (n = 41 typically developing [TDA]; n = 39 anhedonic adolescents [AA]) between the ages of 13–18 were recruited from the greater Boston area from January 2016 to November 2021 (see Table 1 for demographic and clinical characteristics). AA youth were required to have elevated anhedonia on both the SHAPS [27] (total score ≥ 3 based on original [binary] scoring) and on the anhedonia item from the depression module of the Schedule for Affective Disorders and Schizophrenia for School-Age Children (K-SADS [56]) (anhedonia item score > 1); whereas TDA youth reported no anhedonia on these measures. See Supplement for detailed inclusion and exclusion criteria. The clinical trial was pre-registered on clinicaltrials.gov (NCT02498925). The study was approved by the Mass General Brigham (MGB) IRB. Written informed consent was provided from participating parents and 18-year-old adolescents (those under 18 provided assent).
Procedure
During the initial session, participants were administered the K-SADS and completed self-report measures assessing anhedonia and depression symptoms. Participants also completed a brief “mock” MRI simulation session to familiarize themselves with the MRI procedure. For evidence of the benefits of mock scans in MRI studies with youth, see [e.g., ref. [57]. Eligible participants returned to the lab for an fMRI scan session (average days between visits = 11.56; SD = 8.89), which included a monetary reward fMRI task [31, 58,59,60]. Participants also completed a behavioral probabilistic reward task (PRT) [41, 45,46,47] on a desktop computer outside of the scanner and self-report questionnaires. After the scanning session, both groups of participants completed 5 days of EMA via the MetricWire smartphone app. Participants received two to three surveys per day from Thursday through Monday to sample affect on weekdays and weekends. For similar EMA designs in adolescents, see [29, 60,61,62]. Following the MRI scan, AA participants were offered 12 sessions of BA (one 60-minute session per week) based on an established treatment manual [24]. Participants completed self-report assessments of anhedonia (SHAPS) immediately prior to each BA session. A second scanning session, with identical fMRI protocol was conducted post-treatment for AA youth and at a corresponding timepoint for TDA youth. Participants completed a remote follow-up assessment (including the SHAPS) 3-months after their second scan (see supplement for details).
Measures
Self-report questionnaires
Participants reported anhedonia symptoms on the SHAPS [27], a 14-item self-report measure, as well as reported depression symptoms using the 20-item Center for Epidemiological Studies Depression (CES-D) measure [63]. The 9-item Behavioral Activation for Depression Scale – Short Form (BADS - SF) [64] measures the putative target of activity engagement over the past week. See Supplement for details.
Ecological momentary assessment
At each EMA assessment, youth completed items (1–5 scale) probing their current affect, with three each assessing positive affect (PA)(e.g., “happy,” “interested,” and “excited”) and negative affect (NA)(e.g., “sad,” “nervous,” and “angry”) [65]. The ratings for the positive and negative affect words were averaged to create PA and NA variables, respectively (see Supplementary Information).
Probabilistic Reward Task (PRT)
At both scanning sessions, adolescents completed the Probabilistic Reward Task [adapted from [38], which has been previously validated in adolescents [41, 45,46,47]. The task consists of two 100-trial blocks and is designed to assess reward learning (i.e., the ability to adapt behavior as a function of rewards received). See Supplement for a detailed description of the task.
fMRI reward task
The fMRI reward task is described in detail in Murray et al. [29] and in the Supplementary Information. Briefly, during the pre- and post-treatment fMRI scan, youth completed an event-related card-guessing task designed to assess brain responses to the anticipation and receipt of monetary reward and loss. The task included four 6.5-min blocks in which youth guessed whether the value of a card was higher or lower than 5. Based on the trial type (win, loss, neutral), youth won or lost money (win trials +$1.00, loss trails −$0.50, total earnings $16.00). Given the findings from relevant prior studies cited in the Introduction, we focused on neural response to win or loss (contrasted with neutral) outcomes. However, in the Supplement, we also report tests of neural responses to the anticipation of possible rewards vs. losses as predictors of anhedonia improvement and no significant findings emerged. See Supplement for additional details on the task and Supplementary Results.
MRI acquisition and processing
Twelve youth (TDA = 7; AA = 5; Χ2 (1, N = 80) = 0.05, p = 827) were scanned using a Siemens Tim Trio 3 Tesla MRI scanner equipped with a 32-channel coil, whereas the remaining youth were scanned using a Siemens Prisma 3 Tesla MRI scanner equipped with a 64-channel coil. Regardless of scanner, all functional images were acquired with the following parameters, TR = 720 ms, TE = 30 ms, FOV = 212 mm, multiband acceleration factor = 6, voxel size = 2.5 × 2.5 × 2.5. Scanner type was included as a covariate in all analyses. Standard preprocessing steps were used (see Supplement for details). Individual contrast images were used to create second-level random effects models using one-sample t-tests for the win > neutral and loss > neutral contrasts. Mean beta weights for the medial PFC (mPFC) and striatal (NAcc, caudate, and putamen) regions of interest (ROIs) were extracted for each contrast (see Supplement).
Analytic approach
Given the multilevel, longitudinal data structure, we used multilevel models (MLMs; via lme4 [66] and lmerTest [67] packages in R [vers. 4.1.0]) to test whether baseline neural (i.e., striatal and mPFC response to rewards or losses), behavioral (PRT reward learning) and self-report (EMA of PA and NA) measures predict improvement in anhedonia over the course of BA. Separate MLMs were run for neural, behavioral, and self-report predictors of outcome. Specifically, for neural predictors, ROIs included the right and left striatum (i.e., caudate, putamen and NAcc) and mPFC. To test whether striatal or mPFC response to wins and/or losses predicted BA outcome, a MLM simultaneously including StriatumWins × Time, StriatumLosses × Time, mPFCWins × Time, and mPFCLosses × Time interactions was modeled (Time centered to represent estimated post-treatment SHAPS scores, while adjusting for pre-treatment SHAPS and CES-D scores). To avoid multicollinearity due to the high correlation between right vs. left striatal response to wins (r = 0.67) and losses (r = 0.85), separate models were run for left and right striatal ROIs. Corresponding models were run for the behavioral (i.e., Reward Learning × Time) and EMA measures (PA × Time and NA × Time, included in the same model). In each model, intercepts and slopes were treated as randomly varying across patients. All available data were used, including from dropouts (n = 5 AA participants), rendering these intent-to-treat analyses. The above analyses (neural, behavioral and EMA tests) were Bonferroni corrected for multiple comparisons (p = 0.05/4 = 0.013).
To examine pre-treatment to post-treatment changes in reward measures, and consistent with our pre-registered (clinicaltrials.gov; NCT02498925) outcome measures, we first tested a Group (AA/TDA) × Time (baseline and session-to-session SHAPS scores) interaction via MLM to examine group differences in anhedonia change over time. Second, a Group (AA/TDA) × Time (Pre/Post) × Condition (Wins/Losses) interaction tested group differences in neural (striatal and mPFC) responses to wins vs. losses from the baseline to the post-treatment scan session. Finally, a Group (AA/TDA) × Time (Pre/Post) interaction tested group differences in our behavioral (reward learning) measure of reward from the baseline to the post-treatment assessment session. Bonferroni corrections were applied for multiple comparisons (p = 0.05/4 = 0.013). All models controlled for age, sex, antidepressant medication (on SSRI [n = 7] vs not), and scanner type (the latter for imaging analyses). As noted above, five AA participants and six TDA participants dropped out of the study prior to the second (post-treatment) assessment and scan session, and thus were excluded from the latter analyses.
Results
As expected, baseline anhedonia (SHAPS) scores were significantly higher in the AA group (mean = 36.18, SD = 5.85) relative to the TDA group (mean = 17.85, SD = 3.91), t(65.86, Satterthwaite for unequal variances) = 16.39, p < .001; Hedges’ g = 3.67. For comparison with clinically depressed samples, anhedonia severity for our AA adolescents was substantially higher relative to an MDD adolescent sample from a recent CBT trial [16] (SHAPS mean = 31.00; SD = 5.27; Hedges’ g = 0.90) and a large meta-analysis [68] of SHAPS scores among individuals with MDD (mean = 33.1; SD = 2.7; Hedges’ g = 1.12). The above values are based on continuous SHAPS total scores (i.e., range 14–56). In the original (binary) SHAPS scoring (i.e., range 0–14), a score of 3 or greater was used as a cutoff for anhedonia [27]. Our AA sample had a mean score over twice the cutoff (7.26; SD = 3.14). For comparison, the above two studies [16, 68] reported original (binary) SHAPS scores of 3.86 (SD = 3.26) and 5.8 (SD = 1.6), respectively.
BA outcomes
Intent-to-treat MLM analyses revealed a significant Group × Time (b = −0.63, t(82.77) = −5.46, p < 0.001) interaction indicating, as expected, significantly greater reductions in anhedonia (SHAPS) among the AA group relative to the TDA group (see Fig. 1). When focusing specifically on the AA group, there was a significant effect of Time (b = −0.54, t(37.3) = −5.54, p < 0.001) indicating reductions in anhedonia over the course of BA treatment. Among AA treatment completers, pre-treatment (Mean = 36.21; SD = 6.27) to post-treatment (Mean = 29.15; SD = 7.75) reductions in anhedonia represented a large effect (Hedges’ g = 0.82), which was maintained at a 3-month post-treatment follow-up (Mean = 27.21; SD = 6.78; Hedges’ g for pre-treatment to follow-up comparison = 0.95). Mean number of BA sessions completed was 11.2 (SD = 2.3; range = 2–12). Number of sessions completed did not significantly moderate the extent of anhedonia improvement (b = −0.09, p = 0.152). If the BA intervention was delivered as intended, then we would expect significant increases in activation levels, which in turn would relate to anhedonia improvement. As expected, a significant Group × Time interaction (b = 1.10, p < 0.001) emerged, driven by a significantly greater increase in BADS-SF activation subscale scores over time in the anhedonic group receiving BA relative to the control group. In addition, greater increases in BADS activation scores were associated with greater reductions in anhedonia in the anhedonic group (r = −0.45, p = 0.004). See Supplement for secondary trial outcomes, including significant reductions in total depressive symptoms.
Timepoints 1–2, 3–14, 15 and 16 represent the two baseline assessments, 12 BA sessions, the post-treatment assessment and the 3-month follow-up, respectively. Thicker blue line represents average change over time. Typically developing participants’ SHAPS scores (gold) are also plotted for comparison.
Prediction of BA Outcomes
Greater pre-treatment right striatal response to wins (b = −0.57, t(36.11) = −2.82, p = 0.008) but not losses (b = 0.14, t(35.55) = 0.92, p = 0.365) predicted greater improvement in anhedonia (Fig. 2). See Supplement for sensitivity analyses removing covariates and adding the follow-up timepoint, which yielded the same pattern of findings. Left striatal (ps > 0.07) and mPFC (ps > 0.50) response to wins or losses did not significantly predict change in anhedonia. When rank ordering the correlations between (1) all striatal (NAcc, caudate and putamen) and mPFC ROIs (for Win vs. Neutral and Loss vs. Neutral contrasts separately) and (2) anhedonia improvement (MLM-derived slope), the top five predictors were all reward-related (i.e., Win vs. Neutral) contrasts (see Fig. 3). Pre-treatment right caudate (r = 0.37, p = 0.026) and right NAcc (r = 0.29, p = 0.077) response to wins had the numerically strongest correlations with improvement in anhedonia. Contrary to our hypotheses, neither behavioral (Reward Learning × Time) nor EMA measures (PA × Time and NA × Time) predicted change in anhedonia (all ps > 0.58).
Changes in neural and behavioral response following BA
A Group x Time interaction (b = 0.74, t(61.00) = 2.19, p = 0.032) revealed relatively greater pre- to post-treatment increases in right striatal response across condition (i.e., to both rewards and losses) among the AA group relative to the TDA group (see Fig. 4) (within-group pre- to post-session scan Hedges’ g for rewards: AA = 0.26 vs. TDA = −0.32; losses: AA = 0.42 vs. TDA = −0.02). However, the latter finding (p = 0.032) did not survive our pre-defined Bonferroni-corrected threshold. The percentage of participants who exhibited pre- to post-treatment increases in right striatal response to (1) rewards was 62.5% vs. 32.3% in the AA vs. the TDA group, respectively (Χ2 (1, N = 63) = 4.62, p = 0.032) and (2) losses was 62.5% vs. 48.4% in the AA vs. the TDA group, respectively (Χ2 (1, N = 63) = 0.76, p = 0.382). The Group x Time interaction for the other measures (neural and behavioral reward learning variables) were not significant (ps > 0.15).
The bottom panels display subject-specific changes in right striatum responses to rewards (bottom two left panels) and losses (bottom two right panels). Subjects with a positive sloping line (i.e., indicating increases in striatal response to rewards/losses over time) are shown in turquoise, whereas negative sloping lines (or no change) are shown in red. Pre = pre-treatment MRI scan; Post = post-treatment (i.e., second) scan.
Discussion
The present study tested whether pre-treatment measures of reward function predicted anhedonia improvement among adolescents receiving an intervention putatively targeting reward system dysfunction (i.e., BA). In addition, we investigated the extent to which anhedonia and related reward dysfunction normalized over the course of BA. To our knowledge, this represents the first study of BA for anhedonic youth. Strengths of the study included (1) a multimodal assessment of reward system functioning, (2) well-validated neural [29, 31, 58,59,60] and behavioral [41, 45,46,47] measures of reward responsiveness in youth recommended by RDoC [69], (3) the use of smartphone-delivered EMA to acquire a more ecologically valid and real-world assessment of positive affective states in the daily lives of adolescents, (4) a follow-up assessment to examine the extent to which adolescents who received BA maintained their gains after completing treatment, and (5) recruitment of adolescents with a known risk factor of poor treatment outcome (i.e., high levels of anhedonia) [7, 8]. Highlighting the severity of anhedonia in our sample, and as described in more detail above, anhedonia scores for our AA adolescents were substantially higher relative to an adolescent MDD sample from a recent CBT trial [16] and a large meta-analysis [68] of anhedonia severity among individuals with MDD.
Multilevel modeling revealed that, among adolescents with high levels of anhedonia and depressive symptoms, pre-treatment neural – but not self-report or behavioral – measures of relatively enhanced reward responsiveness predicted greater improvement in anhedonia. It is important to highlight that our sample of teens were recruited for heightened anhedonia (and over 60% met criteria for MDD) and thus these findings indicate that individuals with relatively enhanced neural reward responsiveness experienced better BA outcome. This neural patten of findings is consistent with a capitalization (rather than compensatory) model. Namely, those individuals with a more intact neural response to rewards (relative to the other anhedonic adolescents in the sample) experienced better BA outcomes. These findings are generally consistent with several prior studies supporting a capitalization model [16, 52,53,54,55], but not with other research supporting a compensatory model [49,50,51]. However, given the substantial differences between the latter studies and the present study in sample (e.g., adults with depression or anxiety vs. anhedonic adolescents), imaging modality (e.g., EEG vs. fMRI), task (each used a different reward task) and intervention delivered (e.g., CBT, SSRI, or BA), it is very challenging to determine which study features contributed to the differences in findings.
It is also important to highlight that, similar to prior studies of pre-treatment neural predictors of response in depressed and/or anxiety disordered samples [16, 50, 51, 54], we tested the relation between relative striatal reward response (compared to the rest of the clinical sample) and treatment outcome. Conventionally, a “capitalization model” refers to an intervention interacting with or building on an individual’s existing strengths in a particular domain, which facilitates better treatment outcomes. Here, we did not assess “strengths” relative to the general population of adolescents. Instead, we recruited youth struggling with anhedonia (and associated reward system dysfunction) and found that those teens with relatively elevated striatal response to rewards had better outcomes.
Notably, when examining the pattern of findings across all the ROIs and contrasts, the reward-related striatal contrasts (i.e., neural response to rewards vs. neutral outcomes) exhibited the numerically strongest associations with improvement in anhedonia (see ordered rankings in Fig. 3). It may be that individuals with more responsive reward circuits are better able to actively engage in – and derive pleasure and positive reinforcement from – the reward-focused activities prescribed in BA (e.g., systematically increasing engagement in activities expected to stimulate pleasure and/or a sense of accomplishment). Alternatively, relatively heightened reward circuit sensitivity may be a general, intervention non-specific marker of one’s likelihood of experiencing improvement in anhedonia over time. In other words, it is unclear whether heightened striatal response to rewards represents a “prescriptive” (i.e., specific to BA or other similar reward-focused treatments) or general “prognostic” (i.e., intervention non-specific) predictor of anhedonia improvement. A future study with an active comparison condition (e.g., CBT or SSRI) is needed to test whether increased striatal reward response predicts better outcome to BA relative to these alternative interventions. It is also important to note that although heightened striatal response to rewards predicted anhedonic symptom change, it did not significantly predict overall depressive symptom change, highlighting some specificity (see Supplement).
It is worth emphasizing that the pattern of enhanced reward function predicting greater anhedonia improvement only emerged for our neural measure and was not observed for either self-report (EMA) or behavioral (PRT) reward measures. This pattern of findings will need to be replicated in a larger sample. Although speculative, it may be that our neural measure of reward-circuit (striatal) sensitivity – relative to a measure of self-reported momentary (EMA) PA or reward learning (PRT) – more directly probed a relevant dimension of reward functioning which signals one’s likelihood of benefiting from a reward-focused intervention. Interpreted in the context of the RDoC framework, a neural measure of “initial response to rewards” may more directly signal the likelihood that an adolescent will engage with and benefit from a reward-focused treatment like BA, relative to a teen’s tendency to adapt their behavior as a function of reward feedback (i.e., reward learning) or subjective experience of PA in day-to-day life. It is also worth noting that although neural response to rewarding outcomes predicted BA outcome, neural response to the anticipation of rewards did not (see Supplement) [also see [50, 54]. Future studies could test whether other relevant reward-related self-report (e.g., EMA measure of PA reactivity to naturally occurring rewards in daily life) and behavioral (e.g., willingness to expend effort for rewards [70]) measures do predict BA response in anhedonic adolescents.
Although there were significant reductions in self-reported anhedonia over the course of BA, we failed to find the expected pattern of improved reward response on our neural and behavioral measures. A significant effect (i.e., p < 0.05, but did not survive our Bonferroni-corrected threshold) did emerge for greater increases in striatal response to rewards and losses (small to moderate effect sizes) from the baseline to the final scan in the AA group relative to TDA adolescents. This effect was driven by increased pre- to post-treatment striatal response to rewards and losses in the AA group, as well as decreased striatal response to rewards (but not losses) for the TDA group (suggesting neural habituation to the monetary reward stimuli among controls). One interpretation of this finding is that BA does not specifically target reward responsiveness, but instead increases neural sensitivity to affectively salient (e.g., reward- or loss-related) stimuli in anhedonic individuals. The literature on anhedonia has traditionally emphasized blunted responses to rewarding stimuli and events. However, a growing body of research suggests that anhedonia is related to decreased sensitivity to both rewarding and negative stimuli and events [45, 46, 71,72,73], consistent with an “emotional context insensitivity” hypothesis [also see, [74]. Considering these findings, anhedonic adolescents who successfully engage in the prescribed activities of BA may experience a broader re-sensitization to affectively salient stimuli.
This study had several limitations. First, sample size was relatively small, and thus replication in a larger sample is needed. Second, the inclusion of a group of non-anhedonic adolescents (TDA group) who completed neural and behavioral assessments at timepoints corresponding to the AA group controlled for the effect of repeated assessments and task practice effects. However, a future study with an active control condition is needed to test the specificity of findings to BA vs. relevant alternative interventions (e.g., CBT or SSRIs) for the treatment of anhedonia in adolescents. Third, our sample was largely White and non-Hispanic females, limiting the generalizability of our findings. These limitations notwithstanding, this study provides initial evidence for a capitalization (rather than compensatory) model such that BA may be more helpful for anhedonic youth with relatively greater reward circuitry response. Research is needed to identify the most therapeutically beneficial intervention for adolescents with the opposite reward-circuitry pattern (i.e., more blunted reward circuit sensitivity). In addition to alleviating anhedonia, a brief course of BA may also increase neural sensitivity to salient (i.e., both reward- and loss-related) stimuli among anhedonic youth, but this effect may be relatively modest.
References
Avenevoli S, Swendsen J, He J-P, Burstein M, Merikangas KR. Major depression in the national comorbidity survey–adolescent supplement: prevalence, correlates, and treatment. J Am Acad Child Adolesc Psychiatry. 2015;54:37–44.e2.
Eckshtain D, Kuppens S, Ugueto A, Ng MY, Vaughn-Coaxum R, Corteselli K, et al. Meta-analysis: 13-year follow-up of psychotherapy effects on youth depression. J Am Acad Child Adolesc Psychiatry. 2020;59:45–63.
Weersing VR, Jeffreys M, Do M-CT, Schwartz KT, Bolano C. Evidence base update of psychosocial treatments for child and adolescent depression. J Clin Child Adolesc Psychol. 2017;46:11–43.
Walkup JT. Antidepressant efficacy for depression in children and adolescents: industry- and NIMH-funded studies. Am J Psychiatry. 2017;174:430–7.
Goodyer IM, Reynolds S, Barrett B, Byford S, Dubicka B, Hill J, et al. Cognitive behavioural therapy and short-term psychoanalytical psychotherapy versus a brief psychosocial intervention in adolescents with unipolar major depressive disorder (IMPACT): a multicentre, pragmatic, observer-blind, randomised controlled superiority trial. Lancet Psychiatry. 2017;4:109–19.
Orchard F, Pass L, Marshall T, Reynolds S. Clinical characteristics of adolescents referred for treatment of depressive disorders. Child Adolesc Ment Health. 2017;22:61–68.
Bringmann LF, Lemmens LHJM, Huibers MJH, Borsboom D, Tuerlinckx F. Revealing the dynamic network structure of the Beck Depression Inventory-II. Psychol Med. 2015;45:747–57.
McMakin DL, Olino TM, Porta G, Dietz LJ, Emslie G, Clarke G, et al. Anhedonia predicts poorer recovery among youth with selective serotonin reuptake inhibitor-treatment resistant depression. J Am Acad Child Adolesc Psychiatry. 2012;51:404–11.
Auerbach RP, Millner AJ, Stewart JG, Esposito EC. Identifying differences between depressed adolescent suicide ideators and attempters. J Affect Disord. 2015;186:127–33.
Nierenberg AA. Residual symptoms in depression: prevalence and impact. J Clin Psychiatry. 2015;76:e1480–e1480.
Dunn BD, German RE, Khazanov G, Xu C, Hollon SD, DeRubeis RJ. Changes in positive and negative affect during pharmacological treatment and cognitive therapy for major depressive disorder: a secondary analysis of two randomized controlled trials. Clin Psychol Sci. 2020;8:36–51.
Craske MG, Meuret AE, Ritz T, Treanor M, Dour H, Rosenfield D. Positive affect treatment for depression and anxiety: a randomized clinical trial for a core feature of anhedonia. J Consult Clin Psychol. 2019;87:457–71.
Landén M, Högberg P, Thase ME. Incidence of sexual side effects in refractory depression during treatment with citalopram or paroxetine. J Clin Psychiatry. 2005;66:8892.
McCabe C, Mishor Z, Cowen PJ, Harmer CJ. Diminished neural processing of aversive and rewarding stimuli during selective serotonin reuptake inhibitor treatment. Biol Psychiatry. 2010;67:439–45.
Price J, Cole V, Goodwin GM. Emotional side-effects of selective serotonin reuptake inhibitors: qualitative study. Br J Psychiatry. 2009;195:211–7.
Webb CA, Auerbach RP, Bondy E, Stanton CH, Appleman L, Pizzagalli DA. Reward-related neural predictors and mechanisms of symptom change in cognitive behavioral therapy for depressed adolescent girls. Biol Psychiatry Cogn Neurosci Neuroimaging. 2021;6:39–49.
Dimidjian S, Hollon SD, Dobson KS, Schmaling KB, Kohlenberg RJ, Addis ME, et al. Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the acute treatment of adults with major depression. J Consult Clin Psychol. 2006;74:658–70.
Forbes CN. New directions in behavioral activation: using findings from basic science and translational neuroscience to inform the exploration of potential mechanisms of change. Clin Psychol Rev. 2020;79:101860.
Stein AT, Carl E, Cuijpers P, Karyotaki E, Smits JAJ. Looking beyond depression: a meta-analysis of the effect of behavioral activation on depression, anxiety, and activation. Psychol Med. 2021;51:1491–504.
McCauley E, Gudmundsen G, Schloredt K, Martell C, Rhew I, Hubley S, et al. The adolescent behavioral activation program: adapting behavioral activation as a treatment for depression in adolescence. J Clin Child Adolesc Psychol. 2015;0:1–14.
Ritschel LA, Ramirez CL, Cooley JL, Edward, Craighead W. Behavioral activation for major depression in adolescents: results from a pilot study. Clin Psychol Sci Pr. 2016;23:39–57.
Tindall L, Mikocka‐Walus A, McMillan D, Wright B, Hewitt C, Gascoyne S. Is behavioural activation effective in the treatment of depression in young people? A systematic review and meta‐analysis. Psychol Psychother. 2017;90:770–96.
Martell CR, Dimidjian S, Herman-Dunn R. Behavioral activation for depression: a clinician’s guide. New York, NY: Guilford Press; 2013.
McCauley E, Schloredt KA, Gudmundsen GR, Martell CR, Dimidjian S. Behavioral activation with adolescents: a clinician’s guide. New York, NY: Guilford Publications; 2016.
Webb CA, Stanton CH, Bondy E, Singleton P, Pizzagalli DA, Auerbach RP. Cognitive versus behavioral skills in CBT for depressed adolescents: disaggregating within-patient versus between-patient effects on symptom change. J Consult Clin Psychol. 2019;87:484–90.
Leventhal AM, Unger JB, Audrain-McGovern J, Sussman S, Volk HE, Strong DR. Measuring anhedonia in adolescents: a psychometric analysis. J Pers Assess. 2015;97:506–14.
Snaith RP, Hamilton M, Morley S, Humayan A, Hargreaves D, Trigwell P. A scale for the assessment of hedonic tone the Snaith-Hamilton Pleasure Scale. Br J Psychiatry. 1995;167:99–103.
Auerbach RP, Admon R, Pizzagalli DA. Adolescent depression: stress and reward dysfunction. Harv Rev Psychiatry. 2014;22:139–48.
Murray L, Israel ES, Balkind EG, Pastro B, Lovell-Smith N, Lukas SE, et al. Multi-modal assessment of reward functioning in adolescent anhedonia. Psychol Med. 2022:1–10.
Keren H, O’Callaghan G, Vidal-Ribas P, Buzzell GA, Brotman MA, Leibenluft E, et al. Reward processing in depression: a conceptual and meta-analytic review across fMRI and EEG studies. Am J Psychiatry. 2018;175:1111–20.
Rappaport BI, Kandala S, Luby JL, Barch DM. Brain reward system dysfunction in adolescence: current, cumulative, and developmental periods of depression. Am J Psychiatry. 2020;177:754–63.
Borsini A, Wallis ASJ, Zunszain P, Pariante CM, Kempton MJ. Characterizing anhedonia: a systematic review of neuroimaging across the subtypes of reward processing deficits in depression. Cogn Affect Behav Neurosci. 2020;20:816–41.
Pizzagalli DA, Roberts AC. Prefrontal cortex and depression. Neuropsychopharmacology 2022;47:225–46.
Forbes EE, Dahl RE. Research review: altered reward function in adolescent depression: what, when and how? J Child Psychol Psychiatry. 2012;53:3–15.
Morgan JK, Olino TM, McMakin DL, Ryan ND, Forbes EE. Neural response to reward as a predictor of increases in depressive symptoms in adolescence. Neurobiol Dis. 2013;52:66–74.
Stringaris A, Vidal-Ribas Belil P, Artiges E, Lemaitre H, Gollier-Briant F, Wolke S, et al. The Brain’s response to reward anticipation and depression in adolescence: dimensionality, specificity, and longitudinal predictions in a community-based sample. Am J Psychiatry. 2015;172:1215–23.
Hanson JL, Hariri AR, Williamson DE. Blunted ventral striatum development in adolescence reflects emotional neglect and predicts depressive symptoms. Biol Psychiatry. 2015;78:598–605.
Pizzagalli DA, Jahn AL, O’Shea JP. Toward an objective characterization of an anhedonic phenotype: a signal-detection approach. Biol Psychiatry. 2005;57:319–27.
Pizzagalli DA, Iosifescu D, Hallett LA, Ratner KG, Fava M. Reduced hedonic capacity in major depressive disorder: evidence from a probabilistic reward task. J Psychiatr Res. 2008;43:76–87.
Vrieze E, Pizzagalli DA, Demyttenaere K, Hompes T, Sienaert P, de Boer P, et al. Reduced reward learning predicts outcome in major depressive disorder. Biol Psychiatry. 2013;73:639–45.
Belleau EL, Kremens R, Ang Y-S, Pisoni A, Bondy E, Durham K, et al. Reward functioning abnormalities in adolescents at high familial risk for depressive disorders. Biol Psychiatry Cogn Neurosci Neuroimaging. 2021;6:270–9.
Pizzagalli DA. Depression, stress, and anhedonia: toward a synthesis and integrated model. Annu Rev Clin Psychol. 2014;10:393–423.
Santesso DL, Dillon DG, Birk JL, Holmes AJ, Goetz E, Bogdan R, et al. Individual differences in reinforcement learning: behavioral, electrophysiological, and neuroimaging correlates. NeuroImage 2008;42:807–16.
Vrieze E, Ceccarini J, Pizzagalli DA, Bormans G, Vandenbulcke M, Demyttenaere K, et al. Measuring extrastriatal dopamine release during a reward learning task. Hum Brain Mapp. 2013;34:575–86.
Luking KR, Neiman JS, Luby JL, Barch DM. Reduced hedonic capacity/approach motivation relates to blunted responsivity to gain and loss feedback in children. J Clin Child Adolesc Psychol J Soc Clin Child Adolesc Psychol Am Psychol Assoc Div. 2017;46:450–62. 53
Luking KR, Pagliaccio D, Luby JL, Barch DM. Child gain approach and loss avoidance behavior: relationships with depression risk, negative mood, and anhedonia. J Am Acad Child Adolesc Psychiatry. 2015;54:643–51.
Boger KD, Auerbach RP, Pechtel P, Busch AB, Greenfield SF, Pizzagalli DA. Co-occurring depressive and substance use disorders in adolescents: an examination of reward responsiveness during treatment. J Psychother Integr. 2014;24:109–21.
Insel TR, Gogtay N. National Institute of Mental Health clinical trials: new opportunities, new expectations. JAMA Psychiatry. 2014;71:745–6.
Dichter GS, Felder JN, Petty C, Bizzell J, Ernst M, Smoski MJ. The effects of psychotherapy on neural responses to rewards in major depression. Biol Psychiatry. 2009;66:886–97.
Burkhouse KL, Kujawa A, Kennedy AE, Shankman SA, Langenecker SA, Phan KL, et al. Neural reactivity to reward as a predictor of cognitive behavioral therapy response in anxiety and depression. Depress Anxiety. 2016;33:281–8.
Burkhouse KL, Gorka SM, Klumpp H, Kennedy AE, Karich S, Francis J, et al. Neural responsiveness to reward as an index of depressive symptom change following cognitive-behavioral therapy and selective serotonin reuptake inhibitor treatment. J Clin Psychiatry. 2018;79:17m11836.
Cheavens JS, Strunk DR, Lazarus SA, Goldstein LA. The compensation and capitalization models: a test of two approaches to individualizing the treatment of depression. Behav Res Ther. 2012;50:699–706.
Norris LA, Rabner JC, Mennies RJ, Olino TM, Kendall PC. Increased self-reported reward responsiveness predicts better response to cognitive behavioral therapy for youth with anxiety. J Anxiety Disord. 2021;80:102402.
Sequeira SL, Silk JS, Ladouceur CD, Hanson JL, Ryan ND, Morgan JK, et al. Association of neural reward circuitry function with response to psychotherapy in youths with anxiety disorders. Am J Psychiatry. 2021;178:343–51.
Sauer-Zavala S, Cassiello-Robbins C, Ametaj AA, Wilner JG, Pagan D. Transdiagnostic treatment personalization: the feasibility of ordering unified protocol modules according to patient strengths and weaknesses. Behav Modif. 2019;43:518–43.
Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36:980–8.
de Bie HMA, Boersma M, Wattjes MP, Adriaanse S, Vermeulen RJ, Oostrom KJ, et al. Preparing children with a mock scanner training protocol results in high quality structural and functional MRI scans. Eur J Pediatr. 2010;169:1079–85.
Forbes EE, Olino TM, Ryan ND, Birmaher B, Axelson D, Moyles DL, et al. Reward-related brain function as a predictor of treatment response in adolescents with major depressive disorder. Cogn Affect Behav Neurosci. 2010;10:107–18.
Olino TM, McMakin DL, Morgan JK, Silk JS, Birmaher B, Axelson DA, et al. Reduced reward anticipation in youth at high-risk for unipolar depression: a preliminary study. Dev Cogn Neurosci. 2014;8:55–64.
Forbes EE, Hariri AR, Martin SL, Silk JS, Moyles DL, Fisher PM, et al. Altered striatal activation predicting real-world positive affect in adolescent major depressive disorder. Am J Psychiatry. 2009;166:64–73.
Forbes EE, Stepp SD, Dahl RE, Ryan ND, Whalen D, Axelson DA, et al. Real-world affect and social context as predictors of treatment response in child and adolescent depression and anxiety: an ecological momentary assessment study. J Child Adolesc Psychopharmacol. 2012;22:37–47.
Webb CA, Israel ES, Belleau E, Appleman L, Forbes EE, Pizzagalli DA. Mind-wandering in adolescents predicts worse affect and is linked to aberrant default mode network–salience network connectivity. J Am Acad Child Adolesc Psychiatry. 2021;60:377–87.
Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401.
Manos RC, Kanter JW, Luo W. The behavioral activation for depression scale–short form: development and validation. Behav Ther. 2011;42:726–39.
Laurent J, Catanzaro SJ, Joiner TE Jr., Rudolph KD, Potter KI, Lambert S, et al. A measure of positive and negative affect for children: scale development and preliminary validation. Psychol Assess. 1999;11:326–38.
Bates D, Mächler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. J Statistical Softw. 2014;67:1–48.
Kuznetsova A, Brockhoff PB, Christensen RHB. lmerTest package: tests in linear mixed effects models. J Stat Softw. 2017;82:1–26.
Trøstheim M, Eikemo M, Meir R, Hansen I, Paul E, Kroll SL, et al. Assessment of anhedonia in adults with and without mental illness: a systematic review and meta-analysis. JAMA Netw Open. 2020;3:e2013233.
Positive valence systems: workshop proceedings. National Institute of Mental Health NIMH. https://www.nimh.nih.gov/research/research-funded-by-nimh/rdoc/positive-valence-systems-workshop-proceedings. Accessed 20 June 2022.
Treadway MT, Buckholtz JW, Schwartzman AN, Lambert WE, Zald DH. Worth the ‘EEfRT’? The effort expenditure for rewards task as an objective measure of motivation and anhedonia. PLOS One. 2009;4:e6598.
Saxena A, Luking KR, Barch DM, Pagliaccio D. Individual differences in hedonic capacity, depressed mood, and affective states predict emotional reactivity. Motiv Emot. 2017;41:419–29.
Dowd EC, Barch DM. Anhedonia and emotional experience in schizophrenia: neural and behavioral indicators. Biol Psychiatry. 2010;67:902–11.
Burbridge JA, Barch DM. Anhedonia and the experience of emotion in individuals with schizophrenia. J Abnorm Psychol. 2007;116:30–42.
Watson R, Harvey K, McCabe C, Reynolds S. Understanding anhedonia: a qualitative study exploring loss of interest and pleasure in adolescent depression. Eur Child Adolesc Psychiatry. 2020;29:489–99.
Funding
This research was supported by NIMH K23MH108752 (CW). CW was partially supported by NIMH R01MH116969, NCCIH R01AT011002, the Tommy Fuss Fund and a NARSAD Young Investigator Grant from the Brain & Behavior Research Foundation. LM was supported by a grant from the National Institute of Drug Abuse (NIDA; T32 DA015036; PI: Dr. Lukas). DAP was partially supported by R37 MH068376, Wellcome Leap and by a Distinguished Investigator Award from the Brain and Behavior Research Foundation. EEF was supported by NIH R01 MH104418 and NIH R01 MH124900. The content is solely the responsibility of the author and does not necessarily represent the official views of NIH, Wellcome Leap or the Brain & Behavior Research Foundation.
Author information
Authors and Affiliations
Contributions
CW acquired funding for the project. CW, DP, and EF conceptualized the study. CW, AT, and LM acquired, processed, and analyzed the data. All authors contributed to interpretation of findings and drafting the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
Over the past 3 years, DAP has received consulting fees from Albright Stonebridge Group, Boehringer Ingelheim, Compass Pathways, Engrail Therapeutics, Neumora Therapeutics (formerly BlackThorn Therapeutics), Neurocrine Biosciences, Neuroscience Software, Otsuka, Sunovion, and Takeda; he has received honoraria from the Psychonomic Society and the American Psychological Association (both for editorial work) as well as Alkermes; he has received research funding from the Brain and Behavior Research Foundation, the Dana Foundation, Millennium Pharmaceuticals, and NIMH; he has received stock options from Compass Pathways, Engrail Therapeutics, Neumora Therapeutics, and Neuroscience Software; he has a financial interest in Neumora Therapeutics (formerly BlackThorn Therapeutics), which has licensed the copyright to the probabilistic reward task through Harvard University. DAP’s interests were reviewed and are managed by McLean Hospital and Partners HealthCare in accordance with their conflict of interest policies. DAP is on the editorial board of Neuropsychopharmacology. In the past 3 years, EEF received an honorarium from Society for Psychological Science for editing. No funding from these entities was used to support the current work, and all views expressed are solely those of the authors. The other authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Webb, C.A., Murray, L., Tierney, A.O. et al. Reward-related predictors of symptom change in behavioral activation therapy for anhedonic adolescents: a multimodal approach. Neuropsychopharmacol. 48, 623–632 (2023). https://doi.org/10.1038/s41386-022-01481-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41386-022-01481-4
This article is cited by
-
Neural sensitivity following stress predicts anhedonia symptoms: a 2-year multi-wave, longitudinal study
Translational Psychiatry (2024)