Abstract
We assessed the landscape of diagnostic pathology practice and how molecular classification could potentially impact management of patients with endometrial cancer by collecting patient samples, clinicopathologic data, and patient outcomes from EC patients diagnosed in 2016 at 10 Canadian tertiary cancer centers and 19 community hospitals. ProMisE molecular subtype (POLEmut, MMRd, p53abn, No Specific Molecular Profile (NSMP)) was assigned retrospectively. 1357 patients were fully evaluable including 85 POLEmut (6.3%), 380 MMRd (28.0%), 643 NSMP (47.4%), and 249 p53abn ECs (18.3%). Immunohistochemistry (IHC) for MMR proteins was undertaken at the time of primary diagnosis in 2016 in only 42% of the cohort (570/1357; range 3.5–95.4%/center). p53 IHC had only been performed in 21.1% of the cohort (286/1357; range 10.1–41.9%/center). Thus, based on the retrospective molecular subtype assignment, 54.7% (208/380) of MMRd EC had not been tested with MMR IHC (or MSI) and 48.2% (120/249) of p53abn ECs were not tested with p53 IHC in 2016. Molecular subtype diversity within histotypes was profound; most serous carcinomas were p53abn (91.4%), but only 129/249 (51.8%) p53abn EC were serous. Low-grade (Gr1-2) endometrioid carcinomas were mostly NSMP (589/954, 61.7%) but included all molecular subtypes, including p53abn (19/954, 2.0%). Molecular subtype was significantly associated with clinical outcomes (p < 0.001) even in patients with stage I disease (OS p = 0.006, DSS p < 0.001, PFS p < 0.001). Assessment of national pathologic practice in 2016 shows highly variable use of MMR and p53 IHC and demonstrates significant opportunities to improve and standardize biomarker reporting. Inconsistent, non-reflexive IHC resulted in missed opportunities for Hereditary Cancer Program referral and Lynch Syndrome diagnosis, and missed potential therapeutic implications (e.g., chemotherapy in p53abn EC, immune blockade for MMRd EC). Routine integration of molecular subtyping into practice can improve the consistency of EC pathology assessment and classification.
Similar content being viewed by others
Introduction
Endometrial carcinoma (EC) is the most commonly diagnosed gynecologic malignancy in the USA, Canada and Europe and the incidence and mortality continue to rise globally1. Traditional risk stratification systems have relied on histomorphological features that have been shown to be poorly reproducible, especially in high-grade tumors2,3,4,5,6 which has resulted in inconsistent surgical and adjuvant treatment7. Addressing this issue requires improved risk stratification based on objective and reproducible tumor characteristics.
The Cancer Genome Atlas molecular characterization of endometrial carcinoma identified four molecular subtypes based on genomic architecture. Application of surrogate biomarkers using a defined diagnostic algorithm allows for accurate and reproducible diagnosis of these molecular subtypes (POLE mutated (POLEmut), mismatch repair deficient (MMRd), p53 abnormal (p53abn) and, no specific molecular profile (NSMP)) in routine pathology practice8,9,10. Subsequent work has validated and confirmed the prognostic relevance of these molecular subtypes and has demonstrated excellent concordance in subtype diagnosis between diagnostic and hysterectomy specimens11,12. A critically important development is the emerging evidence of molecular subtype serving as a predictive biomarker, with data suggesting improved outcomes with specific therapies e.g. MMRd associated with significant benefit from immune checkpoint blockade therapy13, or p53abn ECs associated with improved outcomes when given adjuvant chemotherapy14. Furthermore, the very favorable prognosis of POLEmut EC, even when no adjuvant treatment is given15,16, has driven clinical trials for de-escalation of therapy in this molecular subtype17,18,19 and led to revised treatment guidelines in Europe20. There is an increasing appreciation of ability of these molecular features to guide more individualized treatment for EC patients, reducing overtreatment, undertreatment, and the use of ineffective therapies21.
The 5th edition of the WHO Classification of Female Genital Tumors has integrated molecular subtype into EC classification22. The European Society of Gynecological Oncology (ESGO), European Society for Radiotherapy and Oncology (ESTRO), and European Society of Pathology (ESP) have gone further and issued guidelines integrating molecular subtype and clinicopathologic variables to direct EC patients toward molecular subtype-specific care20. The National Comprehensive Cancer Network (NCCN)23 encourages the diagnosis of molecular subtype but does not provide molecular subtype directed adjuvant therapy recommendations. Given the prognostic8,9,10,11,12 and predictive13,14,15,16,24,25 information provided by molecular subtype, exceeding what is provided by conventional histomorphologic assessment, there is a trend toward adding molecular subtype diagnosis to routine practice. There remain controversies about what the potential benefit of reflex molecular subtype diagnosis will be in routine diagnostic care.
It is unknown to what extent pathologists have been using p53 and MMR immunostaining in the evaluation of ECs diagnosed in the era preceding molecular classification of EC. Understanding these baseline patterns of practice is important and can inform a move toward more consistent diagnostic practices and treatment of patients with EC, reducing the considerable variation in practice that currently exists in EC care7. Our aim was to assess the landscape of pathological practice in 2016 and how molecular classification could potentially impact management of patients with endometrial cancer.
Materials and methods
Case selection
All ECs diagnosed and/or treated in a single calendar year (2016) were requested from the institutional archives of participating institutions. Clinicopathologic data (including age, BMI, preoperative imaging and CA 125, FIGO stage, grade, histotype on the diagnostic biopsy and hysterectomy specimens, lymphovascular invasion (LVI), lymph node status, immunohistochemical findings, hypermethylation testing and outcome) were collected using a standardized tool (Excel or REDcap) as previously described7. All cases were reviewed by pathologists at participating sites for the selection of best EC tumor block for molecular analyses. Blocks were selected from biopsies or/and hysterectomy specimens. Hysterectomy specimens from patients who had undergone neoadjuvant treatment were excluded, as were cases with insufficient diagnostic material for the study protocol.
Final histomorphologic classification
Histomorphologic classification was based on the surgical pathology reports originating from each of the participating sites. For cases where no hysterectomy information was available (i.e., in cases where no hysterectomy was performed or hysterectomy data was unavailable), the final histotype was as per the diagnostic biopsy/curetting specimen. No systematic central H&E review of tumor histotype was undertaken, in keeping with our stated goal to capture a ‘snapshot’ of contemporary practice.
Immunohistochemistry
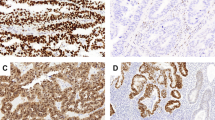
Immunohistochemical stains were performed on 4 µm thickness whole sections cut and stained in the clinical laboratory at Vancouver General Hospital. Immunohistochemistry (IHC) for p53, MSH6 and PSM2 was performed using the Dako Omnis automated immunohistochemistry instrument together with the Dako EnVision™ FLEX+ detection system (Agilent Technologies, Santa Clara, CA) per the manufacturer’s recommendations. Formalin-fixed, paraffin-embedded (FFPE) tumor tissue sections were cut onto charged glass slides, air dried for 10 min, and baked at 60 °C for 10 min. Slides were incubated with p53 (D07, mouse monoclonal antibody, 1:500 dilution, 30 min; Dako), PMS2 (EP51, rabbit monoclonal antibody, undiluted, 20 min; Dako) and MSH6 (EP46, rabbit monoclonal antibody, undiluted, 30 min; Dako).
p53 and/or MMR IHC markers performed for clinical purposes at participating sites were not repeated except when the result was reported as indeterminate, or was not clearly indicated in the accompanying surgical pathology report (e.g., reported as “positive” for p53). IHC performed in the context of the study (i.e., when not previously performed), was interpreted by a pathology research fellow and gynecologic pathologists (ET, CBG, JH). p53 immunostaining was classified as wild-type or abnormal (i.e., overexpression, null, or cytoplasmic staining)26. Mismatch repair IHC was recorded as intact or deficient. The presence of any degree of subclonal staining in centrally stained cases, defined as an abrupt transition between normal and abnormal staining in the setting of adequate internal control, was documented (% tumor cells on slide). In contrast to the abrupt transition between the different staining patterns seen in subclonal expression, poor specimen fixation, which can be a problem in hysterectomy specimens, typically results in a gradual transition in the staining pattern as you move from the well-fixed to less well-fixed areas. In cases of poor fixation, interpretation of staining was done on the well-fixed areas. ECs showing subclonal staining were classified as MMRd or p53abn if the abnormal staining pattern was observed in ≥10% tumor cells27.
Next generation sequencing
POLE mutation testing was performed by targeted next generation sequencing. Specifically, DNA was extracted from FFPE tumors using the Qiagen GeneRead DNA FFPE kit and sequencing was performed centrally (Vancouver), using the FindIt™ V4.0 panel from Canexia Health, with an assay cut-off of ≥5% VAF. POLE coverage included exons 9–14 of the exonuclease domain, however POLEmut assignment was limited to a list of 11 agreed upon pathogenic mutations27.
Final molecular classification
All ECs were classified into one of four molecular subtypes using the ProMisE 2019 algorithm in which POLE mutation status takes precedence over abnormal MMR or p53 immunostaining results. Cases with more than one molecular feature were classified in accordance with the segregation order and rationale described by Leon-Castillo et al.28 (Supplementary Fig. 1).
Statistical methods
Univariable associations between molecular subtype and clinicopathological parameters were evaluated using a Chi-squared or Fisher’s Exact test for binary and categorical variables and a Kruskal–Wallis test for continuous variables (BMI and age at surgery). Cases with missing values were removed from analyses and only complete cases were considered. In order to ensure that missing values were not associated with cohort or with subtype a missing value analysis was undertaken and significance of the association was assessed using Chi-squared tests. We obtained KM curves and we assessed the univariable effect of clinicopathological parameters, clinical phenotypes and molecular subtype. Furthermore, multivariate survival models (overall survival [OS], disease specific survival [DSS] and progression-free survival [PFS]) were fit to account for the effects of all known prognostic factors. Statistical significance was set at α = 0.05 and no attempts were made to adjust for multiple comparisons. All statistical analyses were done using R project for statistical computing. All patients in the survival analysis in this study cohort have a minimum of 2 years of potential follow-up7. Outcome data were randomly censored on December 31st of year 3 following the year in which they had their surgery, to ensure random censoring and minimize assignment bias.
Results
Study cohort
We identified 1459 ECs from 29 participating institutions (10 tertiary centers and 19 community centers) and in 1451 cases a representative block of tumor was submitted. Of these, 81 FFPE blocks contained insufficient tumor to complete immunohistochemical and/or mutational analysis needed for molecular classification as it was specified in the study protocol that at least 50% of tumor tissue in the block(s) had to be preserved and returned to the originating laboratory for potential future clinical use. We received ECs diagnosed in 2015 from one tertiary centre and this cohort was accepted in lieu of 2016 cases due to cost and resource considerations. Significant delays with material transfer agreements, ethics approval or workflow were experienced at two tertiary centers, resulting in truncated case collection for these sites; ~20% & 33% of ECs, respectively, from these sites were received when data collection was capped. In 12 cases, FFPE blocks received originated from patients who had received neoadjuvant treatment (chemotherapy or radiation) and were excluded. In a single case, MMR IHC was uninterpretable due to poor fixation. Thus, complete clinicopathologic and molecular data was available for cancers originating from 1357 patients. A flow chart of the institutional sources and samples obtained is depicted in Supplementary Fig. 2
The clinicopathologic characteristics of the final study cohort are shown in Table 1. The mean age at diagnosis was 64.9 (range 21.9–94.2) years. The average BMI was 33.1 (range 16.0–84.7). The FIGO stage distribution was as follows: 1064 (78.4%) stage I and 293 (21.6%) stages II–IV. LVI was observed in 30.1% of hysterectomy specimens (range 13.2–47.9%, by participating site).
Molecular subtypes
The most common molecular subtype identified was NSMP (643, 47.4%) followed by MMRd (380, 28%), p53abn (249, 18.3%) and POLEmut (85, 6.3%). Low grade (Gr 1 or 2) endometrioid histology was predominant in NSMP (589, 91.6%), MMRd (286, 75.3%) and POLEmut (60, 70.6%) subtypes and was observed in p53abn (19, 7.6%) ECs (Table 1). The molecular subtype distribution of tumors originating from tertiary (1037, 76.4%) vs. community-based (320, 23.6%) institutions is depicted in Fig. 1. Incidence of MMRd (28.4%, 26.6%) and POLEmut (6.5%, 5.6%) subtypes managed in tertiary cancer centers and community institutions were not significantly different. The relative percentage of NSMP (42.5% vs. 63.1%,) and p53abn (22.6% vs. 4.7%) ECs, however, did significantly differ between tertiary vs. community sites (p < 0.0001, for both).
Clinical practice variability
LVI status was reported for all ECs diagnosed in 2015/2016 in both community and tertiary centers. 30.8% of hysterectomy specimens were reported to be positive for LVI. The extent of LVI (focal vs. extensive) was specified in 47.3% of LVI positive cases (range 12.9–100.0% by participating site) with at least three different sets of criteria for this stratification used.
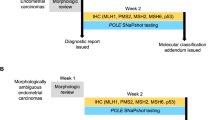
IHC for MMR and p53 were performed in a minority of tumors in 2016 (n = 570; 42.0% for MMR and n = 286; 21.1% for p53, respectively) (Fig. 2). In tertiary centers, IHC for MMR and p53 was performed in 44.7% and 24.4% of cases respectively whereas in community hospitals, MMR and p53 were assessed in 31.7% and 9.9% of cases respectively (p < 0.0001 for both MMR and p53).
Of 141 tumors with loss of MLH1 immunoexpression identified at the time of diagnosis 21/141 (14.9%) were not further evaluated for MLH1 hypermethylation, either by reflex testing initiated by the reporting pathologist or via directed hereditary cancer program (HCP) referral. Of the 254 patients referred to HCP, 15 (5.9%) were identified as having Lynch syndrome. In all, 13/380 (3.4%) MMRd ECs were identified as being Lynch syndrome associated.
Overall, 185 of 402 (46%) ECs with high grade (Gr 3) histology (140 serous, 262 non-serous) underwent p53 IHC staining on either the biopsy or the hysterectomy specimens at the time of diagnostic reporting, in 2016. 90 of 140 serous ECs (62.3%, range 31.3–92.9% by site), and 95 of 262 non-serous grade 3 ECs (36.3%) had p53 IHC performed in 2016, in the context of clinical care.
A wide variety of additional IHC stains, were reported by pathologists at both tertiary and community hospitals, including ER, PR, p16, vimentin, Ki67, Napsin A, CEA, AE1/AE3, PAX8, CK7, CK20 CD10, WT-1 and, others. For the 243 ECs where a complete account of IHC data was available, the average number of non-p53/non-MMR IHC stains performed was 3.85 per case, (range 1–17).
Molecular and histomorphologic correlates
All four ProMisE molecular subtypes were represented within each of the EC histologic categories, with the exception of clear cell carcinoma and dedifferentiated/undifferentiated carcinoma (Fig. 3). Low grade endometrioid EC were predominantly comprised of NSMP (589; 61.7%) and MMRd (286, 30.0%) molecular subtypes, however both POLEmut (60, 6.3%) and p53abn (19, 2.0%) low-grade ECs were also observed (Figs. 4–5). Amongst POLEmut low grade ECs 20% showed LVI and 16.7% presented with >FIGO stage 1 A at the time of hysterectomy (supplementary Table 1). High grade endometrioid EC encompassed a diverse mix of ProMisE subtypes including MMRd (72; 50.3%), p53abn (30; 21.0%), NSMP (26; 18,2%), and POLEmut (15; 10.5%). Serous ECs were predominantly p53abn (128; 91.4%), however MMRd (6; 4.3%), NSMP (5; 3.6%) and POLEmut (1; 0.7%) were also identified (Fig. 5). Similarly, carcinosarcomas showed a predominance of p53abn (37; 88.1%) subtype, though POLEmut (2; 4.8%), NSMP (2, 4.8%) and MMRd (1; 2.4%) ECs were also observed. The mixed ECs were most commonly p53abn (19; 47.5%) followed by MMRd (8; 20.0%), POLEmut (7; 17.5%) and NSMP (6; 15.0%). Clear cell carcinomas included NSMP (12; 63.2%) and p53abn (6; 36.8%) subtypes only, and dedifferentiated and undifferentiated ECs included p53abn (7; 43.8%), MMRd (7; 43.8%) and NSMP (2; 12.5%). Cases categorized as histotype ‘other’ were two p53abn ECs with neuroendocrine differentiation and one NSMP EC with low grade endometrioid histomorphology and adjacent adenosarcoma. The presence of LVI was significantly less frequent in patients with NSMP EC compared to other molecular subtypes (p < 0.001).
Outcomes
Molecular subtype was associated with clinical outcomes for the full cohort of ECs managed in both tertiary and community centers (OS p < 0.001, DSS p < 0.001, PFS < 0.001), and also when analysis was restricted to patients with FIGO stage I disease (n = 1027) (OS p = 0.006, DSS p < 0.001, PFS < 0.001) (Fig. 6). For patients with surgically staged FIGO stage 1 A disease, molecular subtype was significantly associated with PFS (but not OS or DSS) for cancers with myoinvasion (n = 461) (p = 0.038) and without myoinvasion (n = 304) (p = 0.008), with worse outcomes seen in p53abn EC, as expected.
Discussion
There is considerable variability in practice in all aspects of EC management, including pathology workup, surgical treatment, and adjuvant therapy post-hysterectomy2. This reflects the inadequacy of current risk assessment strategies to guide best treatment in an individual patient29. As such, even when using institutional or Society/Cancer Care guidelines23 such as NCCN23, oncologists may choose different treatments for patients with the same clinical and pathological risk factors. Some of the pathological variables used to guide risk stratification and treatment decisions, such as grade and histotype, suffer from suboptimal inter-observer reproducibility2,3,4,5,6, and are poor predictors of response to specific therapeutic interventions. With the recognition of four molecular subtypes of EC based on genomic architecture and diagnosed using surrogate markers, an opportunity to implement more personalized treatment of patients with EC became possible, with the ability to predict likelihood of response to specific therapies13,14,24.
In this study we have retrospectively assigned molecular subtype for a national cohort of patients diagnosed with EC in 2016. The distribution of molecular subtypes: 6.3% POLEmut, 28.0% MMRd, 47.4% NSMP and 18.3% p53abn, is consistent with findings in other unselected cohorts in which only pathogenic mutations in POLE served as the bases for classification30,31,32, with higher rates observed in studies of patients with high risk EC, or where POLEmut was sometimes diagnosed based on mutations that are now known to be non-pathogenic.
MMR testing was performed at the time of diagnosis in less than half of cases, with only 15 tumors (1.1% of the cohort, 3% of MMRd) shown to be Lynch syndrome-associated, when the expected number of Lynch syndrome-associated EC would be 3% of the total cohort and 10% of MMRd EC33,34. This highlights the need for routine MMRd testing in all EC cases, as per current guidelines20,23, to identify patients with EC arising secondary to Lynch syndrome. Not identifying women with Lynch syndrome is a missed opportunity to screen for syndrome-associated malignancies in these patients, and to prevent EC and other Lynch syndrome associated cancers in affected family members. Identifying MMR deficient status has additional predictive implications, enabling access to FDA-approved immune checkpoint blockade therapy, with possible increased response to radiotherapy, and with no demonstrable benefit of adding adjuvant chemotherapy13,14,24.
p53 IHC was reported in 21.1% of all ECs evaluated and in only 51.8% of tumors that were subsequently shown to be p53abn. While a majority of serous carcinomas were p53abn (91.4%), only half of p53abn EC were serous, and 7.6% were low-grade endometrioid. The 2020 ESGO/ESTRO/ESP guidelines classify p53abn EC with any myoinvasion as high-risk disease, agnostic of grade or histotype, and recommend adjuvant chemotherapy ± radiation20; contemporary pathology practice can improve detection of these highest molecular risk ECs by reflexively evaluating p53 IHC, as cases will be missed with the current practice of using p53 IHC at the discretion of the case pathologist.
Regarding additional IHC use (non-p53, non-MMR), it is difficult to infer practice patterns given the variability in reporting across different sites. For those cases where accurate numbers of IHC stains performed per case was available, an average of 3.85 additional non-p53/non-MMR stains were performed (range 1–17 per EC). While universal testing for MMR and p53 would be expected to increase the overall number of IHCs performed for EC, it is also possible that ancillary stains used to establish histotype (e.g., p16, Napsin A) could be used less frequently with transition to a new paradigm where molecular subtype rather than histotype is the main driver of treatment decisions, balancing the cost implications of this practice change.
Importantly, molecular subtype can be accurately evaluated on biopsy specimens, at the earliest point in care, and thus can potentially guide extent of surgery11,12,35,36,37. Characterization of EC molecular subtype is possible in almost all cases, the only exception being those where there is insufficient tissue for POLE testing.
No systematic central H&E review of tumor histotype was undertaken in this study, in keeping with our stated goal of capturing a ‘snapshot’ of contemporary medical practice. We recognized that the suboptimal inter-observer reproducibility of histotype assignment2,3,4,5,6 meant that any review diagnosis would be to some extent arbitrary and certainly subject to being revised on independent re-review. A contributor to the inter-observer variability in histotype diagnosis is highly variable discretionary use of ancillary p53 and MMRd IHC observed in this study. For example, wild type p53 staining is only evidence in support of a diagnosis of non-serous histotype if p53 staning has been performed, a decision that was highly subjective based on the findings in this cohort.
It is important to recognize that histotype and molecular subtype assignment are distinct classification strategies30. While there are correlations between histotype and molecular subtype, as demonstrated herein, an important distinction is that molecular subtype can influence diagnosis of histotype, but not vice versa. There has been evolution in the relationship between histotype and molecular subtype with some pathologists, for example, less likely to diagnose non-endometrioid histotype for MMRd or POLEmut EC38. It is possible that with reflex p53 and MMR immunostaining on all cases there could be improvement in reproducibility of histotype diagnosis. Were such an improvement in histotype diagnostic reproducibility to be seen, however, it would be based on determinants of molecular subtype i.e., p53 and MMR IHC and POLE sequencing, and would therefore be unlikely to result in histotype adding clinically relevant information beyond that provided by molecular subtype diagnosis.
Ongoing prospective molecular subtype-specific clinical trials will further delineate the predictive value of EC molecular subtype18,19,39. While we await Level I evidence, treatment decisions for individuals diagnosed with EC must still be made. At the time of writing this manuscript there is broad support for universal MMR testing, but this is inconsistently performed in many centers. Immunostaining for p53 is widely available but is used variably in EC, and mainly as a diagnostic marker for serous cancers. Pathogenic POLE mutation testing is not yet widely available and adds significant expense, but consideration has been given to a targeted strategy which restricts testing to cases where knowledge of POLE status could impact treatment. Two recent studies have shown that in 38% to 48% of all ECs, POLE testing could be omitted in patients with very low risk EC, where the finding of a mutation would not impact treatment as no further treatment would be given irrespective of POLE mutation status31,40. Future studies will establish whether FIGO grade and histotype designation hold up as clinically significant variables in specific EC subsets e.g., low-grade p53abn ECs and NSMP serous cancers. In addition, further research is needed to determine the molecular and clinical significance of subclonal p53 immunoexpression in the context of molecularly stratified ECs.
In summary, we show considerable variation in diagnostic pathology practice in an era before EC molecular subtype diagnosis became possible in clinical practice settings. In this series of 1357 cases from 2016, there were 208 MMRd not identified, representing a missed opportunity for Lynch Syndrome diagnosis as well as for the prediction of response or non-response to possible therapies. In addition, 120 EC subsequently shown to be p53abn were not tested in 2016. While most p53abn EC were non-endometrioid, and would have been considered high-risk based on histotype, there were 49 p53abn endometrioid EC (30 high-grade and 19 low-grade), where identification as high-risk could have potentially changed management. Finally, no POLEmut EC were diagnosed in 2016, as expected. The 85 POLEmut EC in this cohort included 15 high-grade endometrioid carcinomas and 10 non-endometrioid EC (1 serous, 2 carcinosarcomas, and 7 mixed EC), and of the 60 low-grade POLEmut EC, 12 showed LVI and 10 were stage IB or higher; in these patients the presence of a pathogenic POLE mutation could have influenced a decision to de-escalate therapy. Routine testing for these key molecular features could impact multiple aspects of EC patient care.
Data availability
Data will be made available in response to any reasonable request made to the corresponding author.
References
Sung, H, Ferlay, J, Siegel, RL, Laversanne, M, Soerjomataram, I, Jemal, A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 71, 209–249 (2021)
Soslow, RA, Tornos, C, Park, KJ, Malpica, A, Matias-Guiu, X, Oliva, E, et al. Endometrial Carcinoma Diagnosis: Use of FIGO Grading and Genomic Subcategories in Clinical Practice: Recommendations of the International Society of Gynecological Pathologists. Int J Gynecol Pathol 38 Suppl 1, S64–S74 (2019)
Hoang, LN, Kinloch, MA, Leo, JM, Grondin, K, Lee, CH, Ewanowich, C, et al. Interobserver Agreement in Endometrial Carcinoma Histotype Diagnosis Varies Depending on The Cancer Genome Atlas (TCGA)-based Molecular Subgroup. Am J Surg Pathol 41, 245–252 (2017)
Gilks, CB, Oliva, E, Soslow, RA. Poor interobserver reproducibility in the diagnosis of high-grade endometrial carcinoma. Am J Surg Pathol 37, 874–881 (2013)
Thomas, S, Hussein, Y, Bandyopadhyay, S, Cote, M, Hassan, O, Abdulfatah, E, et al. Interobserver Variability in the Diagnosis of Uterine High-Grade Endometrioid Carcinoma. Arch Pathol Lab Med 140, 836–843 (2016)
De Boer, SM, Wortman, BG, Bosse, T, Powell, ME, Singh, N, Hollema, H, et al. Clinical consequences of upfront pathology review in the randomised PORTEC-3 trial for high-risk endometrial cancer. Ann Oncol 29, 424–430 (2018)
Jamieson, A, Huvila, J, Thompson, EF, Leung, S, Chiu, D, Lum, A, et al. Variation in practice in endometrial cancer and potential for improved care and equity through molecular classification. Gynecol Oncol 165, 201–214 (2022)
Cancer Genome Atlas Research Network, Kandoth, C, Schultz, N, Cherniack, AD, Akbani, R, Liu, Y, et al. Integrated genomic characterization of endometrial carcinoma. Nature 497, 67–73 (2013)
Talhouk, A, Mcconechy, MK, Leung, S, Li-Chang, HH, Kwon, JS, Melnyk, N, et al. A clinically applicable molecular-based classification for endometrial cancers. Br J Cancer 113, 299–310 (2015)
Stelloo, E, Bosse, T, Nout, RA, Mackay, HJ, Church, DN, Nijman, HW, et al. Refining prognosis and identifying targetable pathways for high-risk endometrial cancer; a TransPORTEC initiative. Mod Pathol 28, 836–844 (2015)
Stelloo, E, Nout, RA, Naves, LC, Ter Haar, NT, Creutzberg, CL, Smit, VT, et al. High concordance of molecular tumor alterations between pre-operative curettage and hysterectomy specimens in patients with endometrial carcinoma. Gynecol Oncol 133, 197–204 (2014)
Talhouk, A, Hoang, LN, Mcconechy, MK, Nakonechny, Q, Leo, J, Cheng, A, et al. Molecular classification of endometrial carcinoma on diagnostic specimens is highly concordant with final hysterectomy: Earlier prognostic information to guide treatment. Gynecol Oncol 143, 46–53 (2016)
Green, AK, Feinberg, J, Makker, V. A Review of Immune Checkpoint Blockade Therapy in Endometrial Cancer. Am Soc Clin Oncol Educ Book 40, 1–7 (2020)
León-Castillo, A, De Boer, SM, Powell, ME, Mileshkin, LR, Mackay, HJ, Leary, A, et al. Molecular Classification of the PORTEC-3 Trial for High-Risk Endometrial Cancer: Impact on Prognosis and Benefit From Adjuvant Therapy. J Clin Oncol 38, 3388–3397 (2020)
Mcalpine, JN, Chiu, DS, Nout, RA, Church, DN, Schmidt, P, Lam, S, et al. Evaluation of treatment effects in patients with endometrial cancer and POLE mutations: An individual patient data meta-analysis. Cancer 127, 2409–2422 (2021)
Leon-Castillo, A, Horeweg, N, Peters, EEM, Rutten, T, Ter Haar, N, Smit, VTHBM, et al. Prognostic relevance of the molecular classification in high-grade endometrial cancer for patients staged by lymphadenectomy and without adjuvant treatment. Gynecol Oncol 164, 577–586 (2022)
Wortman, BG, Bosse, T, Nout, RA, Lutgens, LCHW, Van Der Steen-Banasik, EM, Westerveld, H, et al. Molecular-integrated risk profile to determine adjuvant radiotherapy in endometrial cancer: Evaluation of the pilot phase of the PORTEC-4a trial. Gynecol Oncol 151, 69–75 (2018)
Tailored Adjuvant Therapy in POLE-mutated and p53-wildtype Early Stage Endometrial Cancer (TAPER) [cited Jun 14 2021]. https://clinicaltrials.gov/ct2/show/NCT04705649
Bosse T, Powell M, Crosbie E, Leary A, Kroep JR, Han K, et al. Implementation of collaborative translational research (TransPORTEC) Findings in an international endometrial cancer clinical trials program (RAINBO) - Abstract #595. Int J Gynecol Cancer. 31 (2021).
Concin, N, Matias-Guiu, X, Vergote, I, Cibula, D, Mirza, MR, Marnitz, S, et al. ESGO/ESTRO/ESP guidelines for the management of patients with endometrial carcinoma. Int J Gynecol Cancer 31, 12–39 (2021)
Canadian AOP-ACDPNSC, Torlakovic, EE, Riddell, R, Banerjee, D, El-Zimaity, H, Pilavdzic, D, et al. Canadian Association of Pathologists-Association canadienne des pathologistes National Standards Committee/Immunohistochemistry: best practice recommendations for standardization of immunohistochemistry tests. Am J Clin Pathol 133, 354–365 (2010)
Female genital tumours WHO classification of tumours series, 5th ed.; vol. 4. 2020. [cited Feb 5 2022]. https://tumourclassification.iarc.who.int/chapters/34
NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines) Uterine Neoplasms Version 1.2022. [cited Feb 5 2022]. www.nccn.org
Reijnen, C, Küsters-Vandevelde, HVN, Prinsen, CF, Massuger, LFAG, Snijders, MPML, Kommoss, S, et al. Mismatch repair deficiency as a predictive marker for response to adjuvant radiotherapy in endometrial cancer. Gynecol Oncol 154, 124–130 (2019)
Jamieson, A, Bosse, T, Mcalpine, JN. The emerging role of molecular pathology in directing the systemic treatment of endometrial cancer. Ther Adv Med Oncol 13, 17588359211035959 (2021)
Singh, N, Piskorz, AM, Bosse, T, Jimenez-Linan, M, Rous, B, Brenton, JD, et al. p53 immunohistochemistry is an accurate surrogate for TP53 mutational analysis in endometrial carcinoma biopsies. J Pathol 250, 336–345 (2020)
León-Castillo, A, Britton, H, Mcconechy, MK, Mcalpine, JN, Nout, R, Kommoss, S, et al. Interpretation of somatic POLE mutations in endometrial carcinoma. J Pathol 250, 323–335 (2020)
León-Castillo, A, Gilvazquez, E, Nout, R, Smit, VT, Mcalpine, JN, Mcconechy, M, et al. Clinicopathological and molecular characterisation of ‘multiple-classifier’ endometrial carcinomas. J Pathol 250, 312–322 (2020)
Bendifallah, S, Canlorbe, G, Collinet, P, Arsène, E, Huguet, F, Coutant, C, et al. Just how accurate are the major risk stratification systems for early-stage endometrial cancer. Br J Cancer 112, 793–801 (2015)
Huvila, J, Pors, J, Thompson, EF, Gilks, CB. Endometrial carcinoma: molecular subtypes, precursors and the role of pathology in early diagnosis. J Pathol 253, 355–365 (2021)
Imboden, S, Nastic, D, Ghaderi, M, Rydberg, F, Siegenthaler, F, Mueller, MD, et al. Implementation of the 2021 molecular ESGO/ESTRO/ESP risk groups in endometrial cancer. Gynecol Oncol 162, 394–400 (2021)
Loukovaara, M, Pasanen, A, Bützow, R. Clinicopathologic vs. Molecular Integrated Prognostication of Endometrial Carcinoma by European Guidelines. Cancers (Basel) 14, 651 (2022)
Ryan, NAJ, Mcmahon, R, Tobi, S, Snowsill, T, Esquibel, S, Wallace, AJ, et al. The proportion of endometrial tumours associated with Lynch syndrome (PETALS): A prospective cross-sectional study. PLoS Med 17, e1003263 (2020)
Post, CCB, Stelloo, E, Smit, VTHBM, Ruano, D, Tops, CM, Vermij, L, et al. Prevalence and Prognosis of Lynch Syndrome and Sporadic Mismatch Repair Deficiency in Endometrial Cancer. J Natl Cancer Inst 113, 1212–1220 (2021)
Plotkin, A, Kuzeljevic, B, De Villa, V, Thompson, EF, Gilks, CB, Clarke, BA, et al. Interlaboratory Concordance of ProMisE Molecular Classification of Endometrial Carcinoma Based on Endometrial Biopsy Specimens. Int J Gynecol Pathol 39, 537–545 (2020)
Jamieson, A, Thompson, EF, Huvila, J, Leung, S, Lum, A, Morin, C, et al. Endometrial carcinoma molecular subtype correlates with the presence of lymph node metastases. Gynecol Oncol 165, 376–384 (2022)
Crosbie, EJ, Kitson, SJ, Mcalpine, JN, Mukhopadhyay, A, Powell, ME, Singh, N. Endometrial cancer. Lancet 399, 1412–1428 (2022)
Kang, EY, Wiebe, NJ, Aubrey, C, Lee, CH, Anglesio, MS, Tilley, D, et al. Selection of endometrial carcinomas for p53 immunohistochemistry based on nuclear features. J Pathol Clin Res 8, 19–32 (2022)
PORTEC-4a: Molecular Profile-based Versus Standard Adjuvant Radiotherapy in Endometrial Cancer (PORTEC-4a) [cited 14 May 2020]. https://clinicaltrials.gov/ct2/show/NCT03469674
Talhouk A, Jamieson A, Crosbie E, Taylor A, Chiu D, Leung S, et al. Targeted Molecular Testing in Endometrial Carcinoma; Validation of an amended testing protocal. Int J Gynecol Pathol (in press).
Acknowledgements
Samina Nazarali, Jamie Vanden Broek, Luiza Pontial, Parneet Sekhon, Jennifer Oncu, Jennifer Lin, Christine Chow and Monica Ta. This work was supported by the Michael Smith Foundation for Health Research, Innovation to Commercialization grant (JNM). This team has also been supported by the Canadian Institute for Health Research (JNM), the BC Cancer Foundation (Clinician Scientist Award (JNM)), Vancouver General Hospital Foundation, the Vancouver Coastal Health Research Institute, the Chew Wei Memorial Chair in Gynecologic Oncology (JNM). We are grateful for the continued support of this initiative from the Society of Gynecologic Oncologists of Canada (CoP, Translational Research).
Author information
Authors and Affiliations
Consortia
Contributions
EFT, CBG, and JNM co-contributed to study conceptualization, data curation, formal analysis, investigation, methodology, project administration, and writing of the original draft. CBG and JNM co-supervised. JNM acquired study funding. JH and AJ contributed to writing of the original draft. SL, DC, and AT provided data curation, formal statistical analysis, data validation & visualization. SW co-created the data collection tool & provided database management support. AL, JS, MM, and RA performed molecular studies & subsequent data analysis & validation. All other co-authors provided specimens and/or clinical data and contributed to paper review & editing.
Corresponding author
Ethics declarations
Competing interests
Dr. M. MKM, and R.A-H are employees, and Dr. DH is a founder and Chief Medical Officer of Canexia Health.
Ethics approval
Ethics approval from the University of British Columbia office of research ethics, and each collaborating institution, was obtained.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Thompson, E.F., Huvila, J., Jamieson, A. et al. Variability in endometrial carcinoma pathology practice: opportunities for improvement with molecular classification. Mod Pathol 35, 1974–1982 (2022). https://doi.org/10.1038/s41379-022-01165-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41379-022-01165-w
This article is cited by
-
Analysis of patients with endometrial carcinoma using the ProMise classifier: a pilot study from India
Archives of Gynecology and Obstetrics (2023)