Abstract
Penile intraepithelial neoplasia (PeIN) is classified as human papillomavirus (HPV)- and non-HPV-related. This classification is associated with distinct morphologic subtypes. The natural history and prognosis of PeIN subtypes are not well known. This study aims to evaluate clinicopathological features, HPV status, and outcome of PeIN subtypes. Eighty-two lesions from 64 patients with isolated PeIN were retrospectively reviewed. Mean age was 59 years. Lesions were multicentric in 34% of patients and affected glans (33%), shaft (26%), and foreskin (20%). Histologically, 22% of patients had coexisting lesions, classified as hybrid and mixed. HPV-related PeIN (97%) included basaloid (59%), warty (8%), warty-basaloid (8%), hybrid (19%) and mixed (3%) types. P16 and HPV positivity occurred in 99% and 82% of lesions, respectively. HPV 16 was more common in basaloid PeIN. Multiple genotypes were detected in 35%, more commonly in hybrid PeIN (P = 0.051). Positive margins occurred in 63% of excisions. PeIN recurred in 48% of excisions and 30% of overall repeated procedures, and progression to invasive carcinoma occurred in 2%. At follow-up, 86% of patients had no evidence of disease and 12% were alive with disease. Lichen sclerosus occurred in non-HPV and HPV-related PeIN (100% and 47%).
In conclusion, HPV-related and, more specifically basaloid PeIN were the predominant types and preferentially associated with HPV 16. While PeIN had a high recurrence rate, there was a slow and infrequent progression to invasive or metastatic carcinoma with multimodal treatments. Additional studies are needed to understand biology and natural history of PeIN.
Similar content being viewed by others
Introduction
Penile cancer is uncommon in the United States, with 2200 new cases and an estimated 460 deaths in 20211. In North America and Europe, penile cancer has a prevalence of 1 per 100,000, while the annual global burden is estimated at 26,000 cases2. The prevalence increases to 2–4 cases per 100,000 in Asia, Africa, and Latin America due to increased risk factors [e.g., chronic inflammation; penile trauma; lack of neonatal circumcision; tobacco use; lichen sclerosus (LS); poor hygiene; and sexually transmitted diseases, such as human papillomavirus (HPV) and human immunodeficiency virus (HIV)]3. Two pathways have been linked to the histogenesis of penile squamous cell carcinoma: an HPV-dependent pathway (associated with the oncogenic effect of the viral proteins E6 and E7 driving p16INK4a expression)4,5 and a non-HPV-dependent pathway (associated with chronic inflammatory conditions inducing immune dysregulation, such as phimosis, chronic inflammation, and LS, or with HER/PTEN/Akt activation)6,7. These pathways are associated with distinct morphologic features, owing to classification in non-HPV and HPV-related penile carcinoma8. The prevalence of HPV in penile carcinogenesis varies according to the detection methods and use of fresh versus paraffin-embedded tissue and is estimated to be 33–63% in developed countries9,10,11,12,13.
Penile intraepithelial neoplasia (PeIN) is the putative histologic precursor of penile squamous cell carcinoma8. PeIN is similarly classified as non-HPV-related (differentiated) and HPV-related (warty, basaloid, and warty-basaloid) subtypes8. Differentiated PeIN is more frequent in countries with elevated penile cancer incidence than warty and basaloid PeINs14. In a case series of 139 cases from Paraguay, PeIN was associated with invasive carcinoma in 78% of cases15. Conversely, PeIN was more frequently isolated in a National Cancer Institute Surveillance, Epidemiology, and End Results (SEER) database study in the USA16. This discrepancy is likely due to different geographic distribution of clinical and pathologic stages at presentation. Early and late-stage penile cancer is typical of Northern and Tropical countries, respectively, explaining the purported geographic variation17. PeIN and adjacent invasive lesions usually have similar morphology: differentiated PeIN is preferentially located in the foreskin and associated with keratinizing squamous carcinoma, whereas warty and basaloid variants are more likely to occur in the glans and in conjunction with invasive warty, basaloid, and warty-basaloid carcinomas15.
The natural history and prognostic significance of morphologic PeIN subtypes are not well known. This study aims to evaluate distribution, clinical and pathological features, HPV status, and genotype prevalence in PeIN subtypes, emphasizing prognostic significance and outcome in an American series.
Material and methods
Patients
Specimens obtained from 64 patients from 2002 to 2019 were retrospectively identified in the pathology database of the collaborating institutions (University of Alabama at Birmingham, Johns Hopkins University, and Vanderbilt University Medical Center). Cases with concurrent invasive carcinoma or carcinoma identified on resection immediately following the initial diagnostic procedure were excluded. Most patients underwent repeated procedures over time, but only one case per patient (index case) was re-reviewed for the study (typically the specimen obtained when the patient initially presented at each collaborating institution). Information regarding additional procedures and margin status performed either before or after the index ase was obtained from review of medical records. Five pathologists reviewed one representative hematoxylin and eosin-stained slide for each case (MSH, GAG, DFS, MJFN, and ALC) to confirm the histologic subtype and evaluate the immunohistochemistry. Subtyping was performed according to the World Health Organization 2016 classification8,18. Lesion distribution was obtained from medical records or presence of multiple involved biopsy sites. Unicentric PeIN was defined as one lesion present in a single anatomic site. Multicentric lesions were defined as multiple lesions separated by normal epithelium in the same anatomic compartment or located in distant epithelial compartments13. In some cases, multiple histologically heterogeneous variants coexisted in the same specimen. Multiple coexisting HPV-related variants in the same specimen were defined as hybrid (e.g., a basaloid PeIN adjacent to or separated from a warty-basaloid PeIN in the same specimen was classified as basaloid/warty-basaloid). Coexisting HPV-related and non-HPV-related variants in the same specimen were defined as mixed (e.g., a adjacent or separate basaloid and differentiated PeIN was classified as basaloid/differentiated). In this manuscript, “PeIN variant” (n = 64) will designate an isolated PeIN variant (differentiated, basaloid, warty, warty-basaloid), while “PeIN lesions” (n = 82) will describe coexisting lesions within the same specimen and encompassing, e.g., a hybrid or mixed PeIN.
Disease recurrence was defined as recurrence in the same anatomic site following clinical resolution after treatment or de-novo onset in a different anatomic site. Disease persistence was defined as clinical or pathologic persistence in the same anatomic location despite treatment. Disease progression was defined as development of invasive carcinoma or metastasis. Criteria for diagnosis of LS were previously described in a study of 200 cases19.
The study was approved by the Institutional Review Board at Vanderbilt University.
Immunohistochemistry
P16 immunohistochemistry was performed in all cases according to manufacturer instructions on 5 μm sections using a Leica‐Bond immunostainer (ENZ-ABS377-0100, Enzo Life Sciences, Farmingdale, NY, 1:100). Antigen retrieval was performed at pH 9 for 10 min. Immunostained slides were counterstained with hematoxylin. P16 positivity was defined as a continuous, en-bloc stain of atypical tumor cells, excluding parakeratotic or keratotic regions.
HPV genotyping
Type-specific polymerase chain reaction bead-based multiplex genotyping (TS-MPG) assays that combine multiplex polymerase chain reaction (PCR) and bead-based Luminex technology (Luminex Corp., Austin, TX) was performed in 56 cases, of which 40 yielded sufficient DNA, as previously described20,21,22,23. Cases with multiple PeIN lesions were analyzed as a whole. The multiplex type-specific polymerase chain reaction utilizes specific primers for the detection of 19 probable/high-risk (HR) alpha-HPV types (HPV 16, 18, 26, 31, 33, 35, 39, 45, 51, 52, 53, 56, 58, 59, 66, 68, 70, 73, and 82), and 2 low-risk (LR) alpha-HPV types (HPV 6, 11). Two primers for the amplification of beta-globin were also added as a positive control to ascertain the quality of the template DNA.
Statistical analysis
Categorical variables were described with relative frequencies and percentages. Continuous variables were reported as mean (SD) and/or median (range). Statistical significance was determined to be achieved based on a nominal level of α = 0.05 (two-sided, where applicable). Univariable logistic regression and Pearson’s χ-squared test were used to evaluate the association between pathologic variables and PeIN subtypes. Analysis of factors associated with disease outcomes was performed using logistic regression. Specifically, we compared the odds of recurrence/persistence between histology classifications (warty-basaloid/hybrid warty-basaloid vs. basaloid), margin status (positive vs. negative), and focality (multifocal vs. unifocal). For analyses involving more than one sample per individuals, we used generalized estimating equations with a working independence structure to account for within-subject correlation. Missing data were addressed using multiple imputation via chained equations with 50 iterations; results were aggregated using Rubin’s rules24. Statistical analysis was performed with Stata version 17 (StataCorp LLC, College Station, Texas) or R version 4.1.0.
Results
Clinical and pathologic characteristics
The clinical characteristics of the patient cohort are illustrated in Table 1. Briefly, the average age was 59 ± 14, years and 10 of 46 (22%) patients were non-white. Lesions arose primarily in the glans (21 of 64, 33%), shaft (17 of 64, 26%), and foreskin (13 of 64, 20%) and were multicentric in 18 of 53 (34%) patients with no significant difference across PeIN variants (P = 0.85). Predisposing factors were known in 43 patients, and included HIV (n = 9), lack of circumcision (n = 2), balanitis (n = 1), balanitis and delayed circumcision (n = 1), delayed circumcision (n = 1), buried penis (n = 1), phimosis and buried penis (n = 1), and immunosuppression (n = 2). There were no predisposing factors in 25 patients.
Eighty-two lesions were identified in 64 patients. Basaloid (38, 59%) and hybrid (12, 19%) were the most common HPV-related variants. Non-HPV-related (differentiated) PeIN was the least common variant (3%). Multiple histologic lesions in the same specimen were identified in 14 (22%) patients and included hybrid (12, 19%) and mixed (2, 3%) PeIN. The most common hybrid lesions were basaloid/warty (4 of 12, 33%) and basaloid/warty-basaloid (3 of 12, 25%). Mixed lesions included papillary basaloid/differentiated (1 of 2, 50%) and warty-basaloid/papillary basaloid/differentiated PeIN (1 of 2, 50%) (Table 2, Figs. 1–3).
A, B Penile intraepithelial neoplasia (PeIN), basaloid variant, characterized by full-thickness small, immature basaloid cells. P16 immunostain shows full-thickness positivity by immunohistochemistry (Magnification, X200). C, D PeIN, warty variant. There is hyperparakeratosis and koilocytosis. P16 stain is positive. HR-HPV 16 and HPV73 were positive in this case (Magnification, X200). E, F Differentiated PeIN with hyperkeratosis and parakeratosis, acanthosis, and basal atypia. p16 stain and HPV were negative. Lichen sclerosus with homogenization of the subepithelial collagen band is present in the right side of the image (Magnification, X200).
A PeIN, hybrid warty-basaloid and basaloid (Magnification, X100). B Detail of the surface warty features. C Detail of the lower layer basaloid features. D P16 positivity by immunohistochemistry is predominantly full thickness with sparing of the upper keratinizing layer. E Basaloid PeIN was also present in this lesion, continuous with the warty-basaloid area. F P16 expression in the lower two-thirds of the epithelium. This lesion was HR-HPV16 and 18 positive (Magnification, X200).
LS was identified in 37 of 78 (48%) HPV-related and 4 of 4 (100%) non-HPV-related PeIN lesions. LS was not associated with any specific PeIN subtype (P = 0.14) (Table 3).
P16 immunohistochemistry and HPV genotyping
Seventy-seven of 78 HPV-related lesions were p16 positive (99%). An exception was a p16 negative HR-HPV 16 positive basaloid PeIN (Fig. 4 and Tables 2, 4). All non-HPV-related PeINs (2 isolated differentiated PeINs, and two differentiated components of mixed PeINs) were HPV negative (HPV-related vs. non-HPV-related, P < 0.0001). HPV genotyping was performed in 56 of 64 cases. However, only 40 (71%), including two differentiated cases, yielded sufficient housekeeping gene DNA. Thus, the rate of HPV positivity within HPV-related PeIN variants was 31 of 38 (82%). P16 was positive in these cases, except for the basaloid PeIN mentioned above. Among p16-positive HPV-related PeIN, three basaloid, two warty, and two hybrid warty-basaloid (basaloid/warty-basaloid; basaloid/warty/warty-basaloid) were HPV negative.
Genotypes included seven HR- (16, 18, 31, 35, 53, 56, and 73) and one LR-HPV (11). HPV 16 (27 cases, 87%), and 18 (10 cases, 32%) were the most frequent genotypes. Single and multiple genotypes were detected in 20 (65%) and 11 (35%) cases, respectively. The HPV 16/18 combination was the most frequent (6 of 11, 54%). Pure basaloid PeIN was more likely to have one genotype (16 of 20, 80%) compared to other variants (pure basaloid vs. other, including warty, warty-basaloid, and hybrid warty-basaloid, P = 0.01; pure basaloid vs. warty, P = 0.051). Hybrid PeIN was more likely to have multiple genotypes (4 of 6, 67%), but this did not reach statistical significance (pure basaloid vs. hybrid warty-basaloid, P = 0.051).
Among HPV-positive cases, HPV 16 and 18 were similarly distributed in all PeIN variants (Table 4). Among warty PeINs, the only HPV-positive case had HPV 18.
Two cases had isolated differentiated PeIN and were both HPV and P16 negative.
Management, follow-up, and outcome
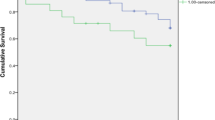
Follow-up was available in 42 of 64 patients (66%) (mean 37, median 30, range 1–154 months). A total of 22 patients were lost to follow up after the initial procedure. Overall, most patients (36 of 42, 86%) had no evidence of disease at last follow-up or were alive with disease (5 of 42, 12%), while 1 patient (2%) died of disease.
Management information after the initial diagnostic procedure is illustrated in the Supplementary Table. In the overall cohort of 64 patients, regardless of the type of procedure, recurrences were multiple and occurred despite repeated procedures (110 total procedures). A second procedure was performed in 27 of 40 (67%) patients with available information, a third in 13 of 25 (52%), and a fourth in 6 of 12 (50%) patients. One patient received up to 9 procedures due to persistent disease and refusal of medical advice for partial penectomy before he was lost to follow-up after seeking a referral to another tertiary center. After the initial procedure, 15 of 40 (38%) patients recurred, while additional 12 of 40 (30%) had persistent disease. Similarly, 11 (44%) and 3 (12%) of 25 patients recurred or had persistent disease after the second procedure, 6 (50%) and 1 (8%) of 12 after the third procedure, and 1 (17%) and 2 of 6 (34%) after the fourth procedure, respectively. Thus, the overall rate of recurrence and persistence episodes over time was 33 of 110 (30%) and 18 of 110 (16%), respectively, including a patient who progressed to invasive disease.
Subset analysis of excision procedures, including repeated procedures and excluding biopsies and isolated laser ablation, showed that a total of 57 procedures were performed over time in 37 patients. Of these, 19 (37%) resulted in negative and 33 (63%) in positive margins, while margins were not reported in 5. Remission occurred in 15 of 19 (79%) patients with negative margins, recurrence occurred in 4 (21%), patients and 1 patient was lost to follow-up after surgery. Among repeated procedures with positive margins, 14 (48%) resulted in recurrence, 6 (21%) resulted in persistent disease, and 9 (31%) were followed by remission, while in 4 cases follow-up was not available after surgery. In a subset analysis of patients who received an excision procedure, we did not have sufficient evidence that histologic classification was associated with odds of recurrence/persistence (OR = 2.50, 95% CI: [0.47, 13.3], P = 0.28). Positive margins (OR = 9.81, 95% CI: [2.38, 40.5], P = 0.002) and multifocality (OR = 4.28, 95% CI: [1.15, 16.0], P = 0.030) were associated with higher odds of recurrence or persistence.
Fourteen patients were treated with topical treatment (7 fluorouracil (FU), 2 imiquimod, 1 imiquimoid, podophylin, and FU, 1 FU and cryotherapy, 1 FU and imiquimod, 1 photoradiation, and 1 liquid nitrogen). Imiquimod 5% was administered from daily to twice weekly applications in cycles for up to one year. Fluorouracil was administered as one application for 5 days a week or every other day for 4–6 weeks, in some cases with multiple repeated cycles. Two patients received two repeated cycles with FU, 1 received a cycle with both FU and one with imiquimod. Of total 17 cycles with FU or imiquimod, 8 were followed by a subsequent procedure for a recurrence, while the remaining 9 were followed by remission. Both patients receiving radiation and liquid nitrogen did not experience recurrence or persistent disease.
Disease progression occurred in 1 of 42 (2%) patients, a 54-year-old Caucasian man, who initially underwent a local excision of a hybrid warty-basaloid (basaloid and warty-basaloid PeIN) with multiple positive margins, followed by treatment with topical fluorouracil for 4–6 weeks. The patient was diagnosed with biopsy-proven metastatic well-differentiated squamous cell carcinoma to the left inguinal lymph nodes 16 months after diagnosis and died from disease 32 months after diagnosis.
Discussion
We found that PeIN recurrence occurred in 30% of overall procedures despite multimodality treatment, while progression occurred in 1 patient (2%) with a hybrid basaloid and warty-basaloid morphology. This finding is noteworthy given the rate of positive margins after excision procedures (63%), which in all cases underwent additional repeated procedures or topical treatment. The median age of 59 years at diagnosis is ten years younger than that observed in invasive carcinoma cohorts, estimated at 68–69 years25,26. However, younger age of onset for invasive carcinoma has been reported in non-Hispanic Black patients due to racial/ethnic disparities27. HPV-related PeIN was most common in our North American series, likely due to the lower prevalence of predisposing factors, such as phimosis, lack of circumcision, and smoking. It is noteworthy that 9 of 22 patients were HIV-positive in our cohort. Similar findings were described by Soskin et al. in a French population, while no evidence of HIV infection was detected in a Paraguayan cohort14. These findings could be explained by the known association of HIV with HPV infection28,29. Similarly, Soskin et al. described a predominance of warty and basaloid PeIN in their French cohort and differentiated PeIN with LS in their Paraguayan cohort (LS, 32 vs. 13%). In our study, 100% of non-HPV-related and 47% of HPV-related PeINs had LS. The high prevalence of LS in HPV-related PeIN in our study is a novel finding. It is unclear whether this finding is associated with our cohort’s epidemiologic characteristics or the biological behavior of slow-progressing isolated PeIN.
A recent metanalysis of 71 studies from 1986 to 2017 showed a HPV DNA and p16 positivity prevalence of 79.8% and 49.5% in PeIN, respectively, with HPV 16 (69.8%), HPV 6 (18.4%), and HPV11 (6.8%) being the most common genotypes30. HPV genotypes are associated with PeIN morphology. Fernández-Nestosa et al. showed a greater HPV genotype variability in PeIN than in invasive carcinoma with up to 18 genotypes detected by laser capture microdissection-PCR. This variability was greater in warty and multicentric PeIN with 11 different HR and LR genotypes compared to basaloid and unicentric PeIN, usually associated with a single genotype13. A bias in the study from Fernandez-Nestosa et al. could be the elevated number of multicentric PeIN, making comparison problematic. In our study, HPV DNA was identified in 82% of HPV-related PeIN and 84% of p16-positive PeINs. These results reflect the literature findings, although our cohort had more HPV 18 than HPV 11. Similar to Fernandez-Nestosa et al.13, we found multiple genotypes, up to 8, in PeIN variants. Multiple genotypes were more frequent in hybrid (67%) than basaloid PeIN (20%) with a trend to statistical significance (P = 0.051), likely reflecting the heterogeneous composition of hybrid PeIN.
Three p16-positive basaloid, 2 warty and 2 hybrid warty-basaloid (basaloid/warty-basaloid; basaloid/warty/warty-basaloid) PeINs were HPV negative. Housekeeping DNA was detected in these HPV negative cases, indicating that the failure to detect viral genome was not caused by poor-quality DNA or insufficient template. Given the high sensitivity and specificity of type-specific PCR bead-based multiplex genotyping with a detection limit for HPV down to 10 copies of viral genome31, a possible explanation for these findings includes a false positive p16 stain, which has been reported in 5% of head and neck cancers32,33. In penile carcinoma, a concordance of 84% between HR-HPV detected by PCR and p16 immunohistochemistry has been reported34, similar to our results. Alternatively, the focal nature of PeIN lesions with scant residual lesional tissue available for this study could have determined a false negative result. Conversely, 1 basaloid PeIN with positive HR HPV 16 was negative for p16 (“mosaic” pattern). This finding could represent true absence of p16 expression due to an innocent bystander HPV infection, either caused by HPV infecting tissue adjacent to and co-sampled with the tumor or by virus integration and silencing, e.g., by promoter methylation or gene deletion with no active gene transcription35. The p16INK4A/cyclin D/Rb pathway can become disrupted due to allelic loss in the p16 region and/or promoter hypermethylation36,37, and inactivation of the tumor suppressor gene p16 due to genetic or epigenetic alterations can be associated with the absence of p16 immunostaining5.
Our study shows that PeIN lesions are often multiple, as previously reported13. In a previous study, warty/basaloid PeIN was more likely multifocal and heterogenous in 61% of cases, whereas differentiated and basaloid variants were more commonly unicentric13. Similarly, Fernandez-Nestosa et al. also reported a predominance of warty, followed by warty-basaloid and basaloid PeIN in their cohort of 33 PeIN lesions from 8 patients, 6 of whom had multiple lesions38. These findings could not be replicated in our study, where PeIN variants were equally uni- or multicentric.
There are few studies evaluating outcomes in penile precancerous lesions. A recent study from the Netherlands enrolled 380 patients with premalignant penile lesions. However, different histological classification criteria were applied, using the vulvar intraepithelial neoplasia grading system (PeIN I–III), and many lesions in this study were preputial, making this study not comparable with our series. The authors found disease progression in 26 patients, of whom 1 (2%) and 18 (7%) had grades I and III, respectively39. Sudenga et al. prospectively evaluated 3033 patients to detect subclinical HPV conversion to external genital lesions at 24-month follow-up. Among 1788 positive cases, 92 developed lesions (86 condylomas and 9 PeIN cases)40,41. In our cohort cumulative recurrence rate over time was 30%. Progression to invasive carcinoma was infrequent in our study and occurred in 1 of 42 patients in whom follow-up was available, despite the presence of positive margins in 33 specimens out of 57 repeated procedures. Multiple treatment modalities were applied, more frequently in those with positive margins, as expected. The infrequent progression in the setting of frequent positive margins suggests that PeIN may remain latent for many years or regress spontaneously, and that some forms can be cured with various topical or local treatments. Alternatively, isolated PeIN may represent a unique entity, dissimilar from PeIN associated with invasive carcinoma. Additional larger studies with molecular characterization may provide insights into the pathogenesis, biology, and natural history of PeIN.
Limitations of this study include its retrospective nature, the limited cohort of differentiated PeIN, the lack of uniform patient management and the limited follow-up available in some patients. However, despite these limitations, this is the first multi-institutional study in an American cohort evaluating the prognostic outcome of subtypes of isolated PeIN.
In summary, PeIN occurs earlier than invasive squamous cell carcinoma and most frequently as an HPV-related type in this American series. The morphological features of HPV-dependent PeIN are heterogeneous. Basaloid PeINs the most common variant preferentially associated with one HPV genotype, usually HPV 16. About a third of PeINs are multicentric, usually harboring multiples HPV genotypes. PeIN appears to have a slow progression with multimodal treatments. Disease recurred in 30% of overall repeated procedures with an average time-to-recurrence of 10 months, highlighting the need for close clinical follow-up in these patients. Due to the limited number of progression events, we could not definitively establish an association between a specific variant and disease progression; however, progression occurred in a hybrid (basaloid and warty-basaloid) PeIN. The relationship of LS with HPV-related PeIN and isolated PeIN needs further investigation.
Disclaimer
Where authors are identified as personnel of the International Agency for Research on Cancer/World Health Organization, the authors alone are responsible for the views expressed in this article and they do not necessarily represent the decisions, policy, or views of the International Agency for Research on Cancer/World Health Organization.
Data availability statement
All data generated or analyzed during this study are included in this published article and its Supplementary Information Files.
References
Siegel, R. L., Miller, K. D., Fuchs, H. E. & Jemal, A. Cancer statistics, 2021. CA Cancer J. Clin. 71, 7–33 (2021).
de Martel, C., Plummer, M., Vignat, J. & Franceschi, S. Worldwide burden of cancer attributable to HPV by site, country and HPV type. Int. J. Cancer 141, 664–670 (2017).
Pow-Sang, M. R., Ferreira, U., Pow-Sang, J. M., Nardi, A. C. & Destefano, V. Epidemiology and natural history of penile cancer. Urology 76, S2–S6 (2010).
Heidegger, I., Borena, W. & Pichler, R. The role of human papilloma virus in urological malignancies. Anticancer Res. 35, 2513–2519 (2015).
Ferreux, E. et al. Evidence for at least three alternative mechanisms targeting the p16INK4A/cyclin D/Rb pathway in penile carcinoma, one of which is mediated by high-risk human papillomavirus. J. Pathol. 201, 109–118 (2003).
Rubin, M. A. et al. Detection and typing of human papillomavirus DNA in penile carcinoma: evidence for multiple independent pathways of penile carcinogenesis. Am. J. Pathol. 159, 1211–1218 (2001).
Mannweiler, S. et al. Penile carcinogenesis in a low-incidence area: a clinicopathologic and molecular analysis of 115 invasive carcinomas with special emphasis on chronic inflammatory skin diseases. Am. J. Surg. Pathol. 35, 998–1006 (2011).
Moch, H., Cubilla, A. L., Humphrey, P. A., Reuter, V. E. & Ulbright, T. M. The 2016 WHO classification of tumours of the urinary system and male genital organs-part A: renal, penile, and testicular tumours. Eur. Urol. 70, 93–105 (2016).
Gregoire, L., Cubilla, A. L., Reuter, V. E., Haas, G. P. & Lancaster, W. D. Preferential association of human papillomavirus with high-grade histologic variants of penile-invasive squamous cell carcinoma. J. Natl Cancer Inst. 87, 1705–1709 (1995).
Miralles-Guri, C. et al. Human papillomavirus prevalence and type distribution in penile carcinoma. J. Clin. Pathol. 62, 870–878 (2009).
Backes, D. M., Kurman, R. J., Pimenta, J. M. & Smith, J. S. Systematic review of human papillomavirus prevalence in invasive penile cancer. Cancer Causes Control 20, 449–457 (2009).
Hernandez, B. Y. et al. Human papillomavirus genotype prevalence in invasive penile cancers from a registry-based United States population. Front. Oncol. 4, 9 (2014).
Fernandez-Nestosa, M. J. et al. Human Papillomavirus (HPV) genotypes in condylomas, intraepithelial neoplasia, and invasive carcinoma of the penis using laser capture microdissection (LCM)-PCR: a study of 191 lesions in 43 patients. Am. J. Surg. Pathol. 41, 820–832 (2017).
Soskin, A. et al. Warty/basaloid penile intraepithelial neoplasia is more prevalent than differentiated penile intraepithelial neoplasia in nonendemic regions for penile cancer when compared with endemic areas: a comparative study between pathologic series from Paris and Paraguay. Hum. Pathol. 43, 190–196 (2012).
Chaux, A. et al. Distribution and characterization of subtypes of penile intraepithelial neoplasia and their association with invasive carcinomas: a pathological study of 139 lesions in 121 patients. Hum. Pathol. 43, 1020–1027 (2012).
Rippentrop, J. M., Joslyn, S. A. & Konety, B. R. Squamous cell carcinoma of the penis: evaluation of data from the surveillance, epidemiology, and end results program. Cancer 101, 1357–1363 (2004).
Sanchez, D. F., Fernandez-Nestosa, M. J., Canete-Portillo, S., Rodriguez, I. & Cubilla, A. L. What is new in the pathologic staging of penile carcinoma in the 8th edition of AJCC TNM model: rationale for changes with practical stage-by-stage category diagnostic considerations. Adv. Anat. Pathol. 28, 209–227 (2021).
Cubilla, A. L. et al. The World Health Organisation 2016 classification of penile carcinomas: a review and update from the International Society of Urological Pathology expert-driven recommendations. Histopathology 72, 893–904 (2018).
Piris, A. et al. Topographical evaluation of penile lichen sclerosus reveals a lymphocytic depleted variant, preferentially associated with neoplasia: a report of 200 cases. Int. J. Surg. Pathol. 28, 468–476 (2020).
Gheit, T. et al. Development of a sensitive and specific multiplex PCR method combined with DNA microarray primer extension to detect Betapapillomavirus types. J. Clin. Microbiol. 45, 2537–2544 (2007).
Ruer, J. B. et al. Detection of alpha- and beta-human papillomavirus (HPV) in cutaneous melanoma: a matched and controlled study using specific multiplex PCR combined with DNA microarray primer extension. Exp. Dermatol. 18, 857–862 (2009).
Schmitt, M. et al. Bead-based multiplex genotyping of human papillomaviruses. J. Clin. Microbiol. 44, 504–512 (2006).
Hampras, S. S. et al. Natural history of cutaneous human papillomavirus (HPV) infection in men: the HIM study. PLoS ONE 9, e104843 (2014).
Rubin D. B. Multiple imputation for nonresponse in surveys. (Wiley: New York, 1987).
Hernandez, B. Y. et al. Burden of invasive squamous cell carcinoma of the penis in the United States, 1998–2003. Cancer 113, 2883–2891 (2008).
Hansen, B. T., Orumaa, M., Lie, A. K., Brennhovd, B. & Nygard, M. Trends in incidence, mortality and survival of penile squamous cell carcinoma in Norway 1956–2015. Int. J. Cancer 142, 1586–1593 (2018).
Huang, T. et al. Racial/ethnic disparities in penile squamous cell carcinoma incidences, clinical characteristics, and outcomes: a population-based study, 2004–2016. Urol. Oncol. 38, 688 e611–688 e619 (2020).
Kreuter, A. & Wieland, U. Human papillomavirus-associated diseases in HIV-infected men who have sex with men. Curr. Opin. Infect. Dis. 22, 109–114 (2009).
Sirera, G. et al. High prevalence of human papillomavirus infection in the anus, penis and mouth in HIV-positive men. AIDS 20, 1201–1204 (2006).
Olesen, T. B. et al. Prevalence of human papillomavirus DNA and p16(INK4a) in penile cancer and penile intraepithelial neoplasia: a systematic review and meta-analysis. Lancet Oncol. 20, 145–158 (2019).
Schmitt, M. et al. Abundance of multiple high-risk human papillomavirus (HPV) infections found in cervical cells analyzed by use of an ultrasensitive HPV genotyping assay. J. Clin. Microbiol. 48, 143–149 (2010).
Larsen, C. G. et al. Correlation between human papillomavirus and p16 overexpression in oropharyngeal tumours: a systematic review. Brit. J. Cancer 110, 1587–1594 (2014).
Kochanny S. et al. High-accuracy HPV testing versus p16 IHC using multiple clinically relevant outcomes: The University of Chicago Experience. J. Clin. Oncol. 36, 6020 (2018)
Cubilla, A. L. et al. Value of p16(INK)(4)(a) in the pathology of invasive penile squamous cell carcinomas: a report of 202 cases. Am. J. Surg. Pathol. 35, 253–261 (2011).
Albers, A. E., Qian, X., Kaufmann, A. M. & Coordes, A. Meta analysis: HPV and p16 pattern determines survival in patients with HNSCC and identifies potential new biologic subtype. Sci. Rep. 7, 16715 (2017).
Poetsch, M. et al. Alterations in the tumor suppressor gene p16(INK4A) are associated with aggressive behavior of penile carcinomas. Virchows Arch 458, 221–229 (2011).
Yanagawa, N., Osakabe, M., Hayashi, M., Tamura, G. & Motoyama, T. Detection of HPV-DNA, p53 alterations, and methylation in penile squamous cell carcinoma in Japanese men. Pathol. Int. 58, 477–482 (2008).
Fernandez-Nestosa, M. J. et al. Comparison of human papillomavirus genotypes in penile intraepithelial neoplasia and associated lesions: LCM-PCR study of 87 lesions in 8 patients. Int. J. Surg. Pathol. 28, 265–272 (2020).
Hoekstra, R. J., Trip, E. J., Ten Kate, F. J., Horenblas, S. & Lock, M. T. Penile intraepithelial neoplasia: Nomenclature, incidence and progression to malignancy in the Netherlands. Int. J. Urol. 26, 353–357 (2019).
Sudenga, S. L. et al. Genital human papillomavirus infection progression to external genital lesions: The HIM Study. Eur. Urol. 69, 166–173 (2016).
Fernandez-Nestosa, M. J. & Cubilla, A. L. Infectious disease: The natural history of HPV infection in men. Nat. Rev. Urol. 12, 478–480 (2015).
Funding
This study was supported by the Vanderbilt Institute for Clinical and Translational Research (VICTR) (VR53120, Dr. Giannico), CTSA award No. UL1 TR002243 by the National Center for Advancing Translational Sciences. Its contents are solely the responsibility of the authors and do not necessarily represent official views of the National Center for Advancing Translational Sciences or the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
G.A.G. and A.L.C. performed study concept, design, and development of methodology. G.A.G., M.M.S.H., M.O., T.G., M.H., M.T., C.N.P., S.C.P. and M.D.C.R.P. and provided data acquisition. A.J.S., G.A.G., M.M.S.H., A.L.C., D.F.S., M.J.F.N. provided analysis and interpretation of data. G.A.G. provided writing and review. A.L.C. provided revision. J.B.G., J.I.E., C.M.G. and L.L.G. provided critical review. All authors read and approved the final paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Straub Hogan, M.M., Spieker, A.J., Orejudos, M. et al. Pathological characterization and clinical outcome of penile intraepithelial neoplasia variants: a North American series. Mod Pathol 35, 1101–1109 (2022). https://doi.org/10.1038/s41379-022-01020-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41379-022-01020-y