Abstract
To determine the epidemiological, histopathological, and clinical characteristics of patients diagnosed with penile cancer in the Brazilian state of Maranhão, the region with the highest incidence worldwide. One hundred and sixteen penile cancer patients were interviewed from July 2016 to October 2018. The majority of patients lived in a rural area (57%), worked in farming (58%), had a low level of schooling or no schooling (90%), and were married or in a stable relationship (74%). The mean age was 60.4 ± 16.51 years (range, 23–93 years). Phimosis (66%), poor/moderate genital hygiene (73%), history of sexually transmitted infections (55%), and zoophilia (60%) were found in the majority of patients. Most patients had their first sexual encounter at 16.2 ± 2.8 years (range, 10–25 years), and 75% had >6 sexual partners. The most common initial symptom was pruritus (37%), and most patients waited to seek treatment (average time to treatment, 18.9 months; range, 2–84 months). Human papillomavirus (HPV)-related histologies were observed in 62% of patients. Most patients had histological grades II or III (87%), stage ≥T2 disease (84%), and lymphadenopathy at admission (42%). Penectomy was performed in 96% of patients. The population with penile cancer in the region of highest incidence in the world is marked by low socioeconomic status, high prevalence of HPV infection, and phimosis. The delay in seeking treatment is related to a very high rate of advanced cancer and aggressive surgical treatment. The high prevalence of young patients was also a striking feature.
Similar content being viewed by others
Introduction
Penile cancer is uncommon in developed countries, and its incidence varies according to the demographic region and the circumcision status1,2. In the US and Europe, the age-standardized incidence rate (ASR) for 100,000 inhabitants is between 0.1 and 1.03. However, in less developed countries, including some countries in South America, Asia, and Africa, the incidence is alarmingly high1. In uncircumcised males, the cumulative lifetime risk for cancer of the penis is higher compared to the general population, corresponding to 1 in 600 men in the US2. Brazil has a high incidence, and the state of Maranhão, located in the northeastern region of the country, has the highest incidence of penile cancer in the world (ASR of 6.1 cases per 100,000 inhabitants)4.
The etiology of penile carcinoma remains unknown, and its mechanisms of development have not been completely elucidated. Phimosis, balanitis, smegma, precarious genital hygiene, smoking, history of sexually transmitted infections (STIs), and human papilloma virus (HPV) infection (present in approximately 50% of cases) are the main risk factors, and circumcision is an important protective factor5,6,7,8. Its incidence is higher in regions with lower socioeconomic level and schooling, given that the presence of risk factors tends to be higher in these locations9,10,11.
Maranhão is the poorest state in the country, with a per capita income of 155.59 USD and a Human Development Index of 0.63912. These factors, together with the high rate of rural inhabitants, distance from major health centers, and little or no schooling, provide the ideal characteristics for the development of penile cancer. Moreover, there is a high HPV prevalence in the general population of the state13. Therefore, the objective of this study is to determine the epidemiological, histopathological, and clinical characteristics of patients diagnosed with penile cancer in the region with the highest reported incidence worldwide. Understanding the profile of these patients can help devise strategies to change this reality.
Methods
A prospective, cross-sectional, descriptive study was performed between July 2016 and October 2018. A total of 116 patients with penile carcinoma treated at the University Hospital of the Federal University of Maranhão and the Aldenora Bello Cancer Hospital (HCAB) in the city of São Luís were included.
The data were collected by a single investigator using a questionnaire. Biopsy samples were analyzed by a uropathologist with 15 years of experience who performed complete paraffin inclusion of the lesion or a minimum of 40 blocks of paraffin for very advanced lesions.
The variables studied included age, marital status, schooling, occupation, residence, family income, smoking, alcoholism, characteristics of the foreskin, history of genital warts, genital hygiene14, history of STIs, sexual history, initial symptom and duration of symptoms, lymph node enlargement on admission, tumor size, topography, subtype (World Health Organization, 2018) and histological grade15 of the tumor, staging (TNM 8th Ed., 2017), type of surgery, and completion of lymphadenectomy. Information on alcohol intake, history of genital warts, history of STIs, initial symptoms, and zoophilia began to be collected after the study was underway, which explains the low number of cases evaluated. The criterion used to classify genital hygiene as poor/moderate was less than one genital wash with soap per day or presence of phimosis.
Data was arranged using Microsoft Excel 2010 and analyzed with Stata version 12.0 (Stata Corporation, College Station, TX, USA). Statistical analyses were performed using the Chi-square and Fisher’s exact test. The 95% confidence interval was calculated using logistic regression with a significance of p < 0.05. This work was in accordance with the principles of the 1964 Helsinki declaration and approved by the Research Ethics Committee of the Universidade Federal do Maranhão [process no. 43774215.7.0000.5086] and written informed consent was obtained from all patients.
Results
Sociodemographic aspects
Between 2016 and 2018, 116 patients were analyzed. Most lived in a rural area (57%), worked in farming (58%), had no schooling or studied only through primary school (90%), and were married or in a stable relationship (74%) (Table 1).
Clinical features
The mean age at diagnosis was 60.4 ± 16.51 years, with a predominance of men over 60 (54%); 22% were younger than 45. There was no relationship between age and advanced tumors (p = 0.65), high histological grade (p = 0.58), or HPV-related subtypes (basaloid, condylomatous, and mixed; p = 0.55). Fewer than half were smokers (41%), more than half had a history of phimosis (66%), and a minority were circumcised (24%). All the circumcised patients underwent the procedure in adulthood after presenting with symptoms. Most men had no genital warts (78%), had poor/moderate genital hygiene (73%), had a history of STIs (55%), and practiced zoophilia (60%). The average age at first sexual encounter was 16.2 years, and the number of lifetime sexual partners was >6 in 75% of patients. The average time from onset of symptoms to seeking treatment was 18. 9 months, and the most common symptom was pruritus (37%). Lymph node enlargement on admission was observed in 42% of the patients (Table 2).
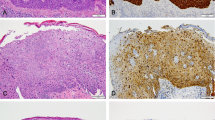
Histopathological and surgical aspects
All patients were diagnosed with squamous cell carcinoma. The average tumor size was 4.5 cm (largest diameter), with the most frequent location being the glans (47%). The usual subtype was that most commonly found in the samples (40%), but HPV-related types were more representative when considered together (62%). HPV subtype was not related to high histological grade (p = 0.16) or advanced tumor stage (p = 0.63). There was a predominance of histological grades II and III (87%). Partial penectomy was the most common surgical treatment (64%), and lymphadenectomy was performed in 52% of the patients (Table 3).
Discussion
Brazil has one of the highest incidences of penile cancer worldwide. This incidence is much higher than in the United States and Europe (0.4–0.6%)8,16, only resembling developing nations like India, African and others South American nations1,17. However, there is variability even within Brazil, where the highest number of cases is reported in the Northeast region18. The incidence in this region is 5.7%, surpassing the economically more developed region - Southeast (1.2%) - and the North (3.8%), the second poorest region19. The particularly high number of patients with penile cancer in Maranhão, which has the highest reported incidence worldwide, accounts for this state being the least developed region of Brazil and having high rates of HPV infection12,13.
The sociodemographic profile in this study were very similar to those of other localities in Brazil and worldwide10,18,19,20. The patients were mainly of low economic status and education and lived rurally. However, unlike most studies, there were significant numbers of patients living in urban and suburban areas. A similar profile was only found in the state of Pará21 and in Paraguay14, localities with similar sociodemographic aspects. This is probably due to the recent demographic transition that occurred in these regions, with migration of rural inhabitants to large centers in search of better living standards, employment, and healthcare. Despite living in developed regions, these patients have a similar socioeconomic profile to those in rural areas, leaving them vulnerable to the same risk factors for the development of neoplasia14.
Penile cancer is more common in older men1. However, it can occur in young men, and the incidence in men <45 years in Brazil is high (19.41%)18. Our data followed this trend, with 22% men being in this age range. There are few published studies on penile cancer in the young population, so it is unclear whether age is related to increased tumor aggressiveness22. In our sample, there was no relationship between age and advanced tumor stage, high histological grade, or HPV subtype. Nevertheless, our numbers are worrisome, since mutilating treatments, like emasculation and partial or total penectomy, have been instituted in sexually active men, subjecting them to physical sequelae, negative impact on welfare, psychological and sexual dysfunction23,24. We also saw a concerning delay in seeking treatment. The average interval from the onset of symptoms to first treatment was 18.9 months. Patients with penile cancer have the longest delay in seeking treatment, reaching more than 1 year in 15–50% of cases and the most common causes for this are fear, embarrassment, and social stigma17. Further, because Maranhão is the poorest state in the country, there is a serious structural and healthcare deficit, with difficulty in accessing adequate treatment. The result is a high number of men with advanced neoplasms and mutilating treatments.
A minority of patients in our sample were smokers (41%). Tobacco is an established risk factor for penile cancer and other neoplasms20,25,26. Hellberg et al.25 also noted that heavy smokers have a higher risk for penile carcinoma. Compared to other localities, Maranhão has the smallest proportion of smokers among patients with penile cancer (Rio de Janeiro10: 56.5%, Canada27: 50%, and Paraguay14: 76%). This indicates that penile cancer in Maranhão is more strongly related to other risk factors.
Phimosis, inflammatory conditions (balanitis and lichen sclerosus) and poor genital hygiene are relevant risk factors for cancer of the penis. The prevalence of phimosis in males in adulthood is over 3.4%28. Between patients with cancer of the penis, this prevalence is over 25–75%16,29, and its contribution can be attributed to the accumulation of smegma, higher incidence of HPV or as an isolated carcinogenic factor7,30,31,32. Genital lichen sclerosus was associated with malignant penile changes in 5.8%33 of cases and balanitis over 45%11. Conversely, circumcision, if performed in the neonatal period or up to adolescence, is an important protective factor34. In uncircumcised individuals, good genital hygiene is perhaps the most important protective measure6,35. In our study, the prevalence of phimosis was high, and the majority of circumcised men underwent the procedure in adulthood, after having symptoms of the disease. This profile is similar to the national tendency18: the prevalence of phimosis among men with penile cancer in Brazil is 60%, and only 13% of patients are circumcised. This is because of the low prevalence of circumcision in the general population (<20%)36. Neonatal circumcision is not normally performed in Brazil, and regions with worse access to healthcare have a lower rate of circumcision in childhood and adulthood37. By comparison, in the United States, where around 80.5% of the global population is circumcised, the incidence of penile cancer is very low38.
Factors related to sexual history are of fundamental importance in the development of penile cancer. HPV is present in 15–80% of cases, and condylomatous, basaloid, and mixed (with condylomatous and/or basaloid component) histologies are related to HPV infection39,40. The pivotal multinational study conducted by Castellsague et al.41 stratified the susceptible to acquiring HPV infection in men according to sexual behavior in high risk (individuals who had ≥6 sexual partners and a sexual debut before the age of 17), low risk (individuals reporting ≤5 partners and the first sexual experience at ≥17 years of age), and medium risk (other than low or high risk individuals). In our study, the prevalence of HPV-related subtypes was 60%; in men with 6 or more sexual partners, it was 75%, and in men who had their first sexual intercourse before the age of 17 was 59%. This is due to the very high prevalence of HPV in Maranhão; the state capital has the highest prevalence in Brazil (59.1%)13. Early onset of sexual activity and a large number of sexual partners contribute to this high prevalence.
The relationship between zoophilia and penile cancer was the subject of a recent study42. The authors consider zoophilia a risk factor and demonstrate that men who practiced sex with animals are two times more likely to develop cancer of the penis. They believe that microtraumas generated in the penis and contact with animal secretions are the causative factors. In our study, 60% of patients practiced zoophilia.
The signs and symptoms of penile cancer are varied. The most frequent initial sign is a change in the skin of the penis, such as nodules, ulcers, swelling, and color changes34. A few studies include pruritus as an initial symptom, and, when present, it is more commonly related to associated skin lesions, such as lichen sclerosus33,43. Interestingly, in our study, intense pruritus was the most common initial symptom and was described as the only initial symptom in 26.56% of patients. However, the presence of lichen sclerosus was extremely low (6%), which indicates the possibility of other causes in our sample that can explain pruritus.
The number of patients with characteristics of advanced disease, like lymph node enlargement on admission (41.8%), high histological grade (87%), and T stage ≥2 (82%) was high. These are higher than those in other Brazilian studies10,20 and studies in developed nations such as Finland44 and the USA45. Although histological subtypes related to HPV represented the major part of the sample, there was no significant relationship with high grade (p = 0.16) or advanced stage (p = 0.63). This can be explained by the less aggressive natural behavior of HPV-related tumors46,47.
Penectomy was performed in almost all cases, surpassing the proportion of patients undergoing radical surgery in other Brazilian regions (80.9%–93.1%)10,18, the United States (82.1%)45 and Canada (71%)27. The high proportion of penectomies over less invasive surgical alternatives, such as local tumor excision, is due to the large number of advanced tumors in our sample. Although penectomy is the gold standard therapy for penile cancer, its physical and psychosocial effects are devastating43. The number of lymphadenectomies was also high, irrespective of lymph node metastasis, because lymphadenectomy was performed prophylactically in some patients due to the difficulty in maintaining follow-up.
One limitation of this study is that it does not cover all hospitals in the state, and therefore may underestimate the actual number of cases. In addition, the low educational and socioeconomic level of some patients hampered the collection of reliable data in some cases, although these were excluded from the analysis. However, it was possible to determine important factors associated with cancer of the penis in a region of high incidence.
Conclusion
The population with penile cancer in the region with the highest worldwide incidence is marked by a high prevalence of HPV infection and phimosis. Together with the low socioeconomic level of the patients, these are leading factors for the development of the neoplasm. A delay in seeking treatment was related to the high frequency of advanced tumors and aggressive surgical treatment. The high prevalence of young patients was also a striking feature. The reduction through vaccination against HPV, early infant circumcision, hygiene measures, early diagnosis, and education can stop the advance of the neoplasm in the state.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Christodoulidou, M., Sahdev, V., Houssein, S. & Muneer, A. Epidemiology of penile cancer. Curr Probl Cancer. 39, 126–136 (2015).
Kochen, M. & McCurdy, S. Circumcision and the risk of cancer of the penis. A life-table analysis. Am J Dis Child. 134, 484–486 (1980).
Parkin, D. M. et al. Cancer Incidence in Five Continents, Vol. VI (IARC Press, Lyon, 1992).
Coelho, R. W. P. et al. Penile cancer in Maranhão, Northeast Brazil: the highest incidence globally? BMC Urology. 18, 50 (2018).
Barrasso, R., De Brux, J., Croissant, O. & Orth, G. High prevalence of papillomavirus-associated penile intraepithelial neoplasia in sexual partners of women with cervical intraepithelial neoplasia. N Engl J Med. 317, 916–23 (1987).
Maden, C. et al. History of circumcision, medical conditions, and sexual activity and risk of penile cancer. J Natl Cancer Inst. 85, 19–24 (1993).
Albero, G. et al. Male circumcision and prevalence of genital human papillomavirus infection in men? A multinational study. BMC Infect Dis. 13, 1–10 (2013).
Morris, B. J. et al. The strong protective effect of circumcision against cancer of the penis. Adv Urol. 2011, 812368 (2011).
Hakenberg, O. W. et al. Guidelines on penile cancer. UrowebOrg. 67, 142–150 (2015).
Koifman, L., Vides, A. J., Koifman, N., Carvalho, J. P. & Ornellas, A. A. Epidemiological aspects of penile cancer in Rio de Janeiro: evaluation of 230 cases. Int Braz J Urol. 37, 231–240 (2011).
Thuret, R. et al. A population-based analysis of the effect of marital status on overall and cancer-specific mortality in patients with squamous cell carcinoma of the penis. Cancer Causes Control. 24, 71–79 (2013).
IBGE. Panorama: população. https://cidades.ibge.gov.br/brasil/ma/panorama (2018).
Estudo Epidemiológico sobre a Prevalência Nacional de Infecção pelo HPV (POP-Brasil): Resultados preliminares (Associação Hospitalar Moinhos de Vento, Porto Alegre, 2017).
Chaux, A. et al. Epidemiologic profile, sexual history, pathologic features, and human papillomavirus status of 103 patients with penile carcinoma. World J Urol. 31, 861–867 (2013).
Velazquez, E. F. et al. Histologic grade and perineural invasion are more important than tumor thickness as predictor of nodal metastasis in penile squamous cell carcinoma invading 5 to 10 mm. Am J Surg Pathol. 32, 974–9 (2008).
Heller, D. S. Lesions and neoplasms of the penis: a review. J Low Genit Tract Dis. 20, 107–111 (2016).
Misra, S., Chaturvedi, A. & Misra, N. C. Penile carcinoma: a challenge for the developing world. Lancet Oncol. 5, 240–7 (2004).
Favorito, L. A. et al. Epidemiologic study on penile cancer in Brazil. Int Braz J Urol. 34, 587–91 (2008).
Brumini, R., Torloni, H., Henson, D. E., Gotieb, S. L. D. & Souza, J. M. P. Câncer no Brasil - Dados histopatológicos: 1976–80 (Ministério da Saúde, Rio de Janeiro, 1982).
do Couto, T. C., Barbosa, A. R. M., do Couto, M. C. & Dubourcq, B. F. Epidemiological study of penile cancer in Pernambuco: experience of two reference centers. Int. braz j urol. 40, 738–744 (2014).
Fonseca, A. G., Pinto, J. A. S. A., Marques, M. C., Drosdoski, F. S. & Fonseca Neto, L. O. R. Estudo epidemiológico do câncer de pênis no Estado do Pará, Brasil. Rev Pan-Amaz Saude. 1, 85–90 (2010).
Martins, V. A. et al. P16INK4a expression in patients with penile cancer. PLoS One. 13, e0205350 (2018).
Maddineni, S. B., Lau, M. M. & Sangar, V. K. Identifying the needs of penile cancer sufferers: a systematic review of the quality of life, psychosexual and psychosocial literature in penile cancer. BMC Urol. 9, 8 (2009).
Barros, E. N. & Melo, M. C. B. Câncer de pênis: perfil sócio-demográfico e respostas emocionais à penectomia em pacientes atendidos no Serviço de Psicologia do Hospital de Câncer de Pernambuco. Rev. SBPH. 12, 99–111 (2009).
Hellberg, D., Valentin, J., Eklund, T. & Nilsson, S. Penile cancer: is there an epidemiological role for smoking and sexual behaviour? Br Med J. 295, 1306–8 (1987).
Solsona, E., Algaba, F., Horenblas, S., Pizzocaro, G. & Windahl, T. EAU Guidelines on Penile Cancer. Eur Urol. 46, 1–8 (2004).
Beech, B., Izawa, J., Pautler, S., Chin, J. & Power, N. Penile cancer: perspective from a Canadian tertiary care centre. Can Urol Assoc J. 9, 315–9 (2015).
Morris, B. J., Matthews, J. G. & Krieger, J. N. Prevalence of phimosis in males of all ages: systematic review. Urology. S0090-4295, 30919–7 (2019).
Dillner, J. et al. Etiology of squamous cell carcinoma of the penis. Scand J Urol Nephrol Suppl. 205, 189–93 (2000).
Reddy, D. G. & Baruah, I. K. Carcinogenic action of human smegma. Arch Pathol. 75, 414–20 (1963).
Letendre, J., Saad, F. & Lattouf, J. B. Penile cancer: what’s new? Curr Opin Support Palliat Care. 5, 185–91 (2011).
Shabad, A. L. The experimental production of the penis tumours. Neoplasma. 12, 635–44 (1964).
Nasca, M. R., Innocenzi, D. & Micali, G. Penile cancer among patients with genital lichen sclerosus. J Am Acad Dermatol. 41, 911–914 (1999).
American Cancer Society. Signs and Symptoms of Penile Cancer https://www.cancer.org/cancer/penile-cancer/detection-diagnosis-staging/signs-symptoms.html (2018).
Schoen, E. J. Neonatal circumcision and penile cancer. Evidence that circumcision is protective is overwhelming. BMJ. 313, 46–47 (1996).
WHO/UNAIDS. Neonatal and child male circumcision: a global review (World Health Organization, Geneva, 2010).
Korkes, F., Silva, J. L. II & Pompeo, A. C. L. Circuncisão por motivos médicos no sistema público de saúde do Brasil: epidemiologia e tendências. Einstein. 10, 342–346 (2012).
Introcaso, C. E. et al. Prevalence of circumcision among men and boys aged 14 to 59 years in the United States, national health and nutrition examination surveys 2005-2010. Sex Transm Dis. 40, 521–525 (2013).
Griffiths, T. R. & Mellon, J. K. Human papillomavirus and urological tumours: I. Basic science and role in penile cancer. BJU Int. 84, 579–86 (1999).
Velazquez, E. F. et al. Protocol for the examination of specimens from patients with carcinoma of the penis. Arch Pathol Lab Med. 134, 923–929 (2010).
Castellsagué, X. et al. Male circumcision, penile human papillomavirus infection, and cervical cancer in female partners. New England Journal of Medicine. 346, 1105–1112 (2012).
Zequi, S. C. et al. Sex with animals (SWA): behavioral characteristics and possible association with penile cancer. A multicenter study. J Sex Med. 9, 1860–67 (2012).
Douglawi, A. & Masterson, T. A. Updates on the epidemiology and risk factors for penile cancer. Transl Androl Urol. 6, 785–790 (2017).
Maiche, A. G. Epidemiological aspects of cancer of the penis in Finland. Eur J Cancer Prev. 1, 153–8 (1992).
Jayaratna, I. S., Mitra, A. P., Schwartz, R. L., Dorff, T. B. & Schuckman, A. K. Clinicopathologic characteristics and outcomes of penile cancer treated at tertiary care centers in the Western United States. Clin Genitourin Cancer. 12, 138–42 (2014).
Chaux, A. et al. Distinctive immunohistochemical profiles of penile intraepithelial lesions - a study of 74 cases. Lab Investigation. 91, 184a (2011).
Stratton, K. L. & Culkin, D. J. A contemporary review of HPV and penile cancer. Oncology. 30, 245–249 (2016).
Author information
Authors and Affiliations
Contributions
C.B.V. and G.E.B.S. are the principal investigators and wrote the first version of the manuscript. A.T.J., J.C., R.C. and L.N. participated in the care and management of the patient and data collection. G.E.B.S. and I.C. performed pathological analysis and interpretation. J.P. and J.L. contributed to statistical analysis. I.C., F.S. and L.F. contributed to critical revision of important intellectual content of the manuscript. All authors contributed to the writing process and read and approved the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vieira, C.B., Feitoza, L., Pinho, J. et al. Profile of patients with penile cancer in the region with the highest worldwide incidence. Sci Rep 10, 2965 (2020). https://doi.org/10.1038/s41598-020-59831-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-59831-5
This article is cited by
-
A global approach to improving penile cancer care
Nature Reviews Urology (2022)
-
Clinicopathological characteristics of carcinoma penis over 10 years in a tertiary-level oncology center in Nepal: a retrospective study of 380 cases
International Urology and Nephrology (2022)
-
HPV infection and 5mC/5hmC epigenetic markers in penile squamous cell carcinoma: new insights into prognostics
Clinical Epigenetics (2022)
-
A comprehensive analysis of penile cancer in the region with the highest worldwide incidence reveals new insights into the disease
BMC Cancer (2022)
-
A cohort study among 402 patients with penile cancer in Maranhão, Northeast Brazil with the highest worldwide incidence
BMC Research Notes (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.