Abstract
Vaccination is one of the most successful medical interventions that has saved the life of millions of people. Vaccination is particularly important in patients with multiple myeloma, who have an increased risk of infections due to the disease-inherent immune suppression, and because of the immune suppressive effects of therapy. Hence, all appropriate measures should be exploited, to elicit an effective immune response to common pathogens like influenza, pneumococci, varicella zoster virus, and to those bacteria and viruses (haemophilus influenzae, meningococci, and hepatitis) that frequently may pose a significant risk to patients with multiple myeloma. Patients after autologous, and specifically after allogeneic transplantation have severely reduced antibody titers, and therefore require a broader spectrum of vaccinations. Response to vaccination in myeloma often is less vigorous than in the general population, mandating either measurement of the postvaccination antibody titers and/or repeating the vaccination. Here, we compile the existing data on vaccination in multiple myeloma and provide recommendations for clinical practice.
Similar content being viewed by others
Introduction
Infections remain the most common cause of morbidity and mortality in multiple myeloma besides the disease itself [1, 2]. The risk of infection is increased already at the stage of MGUS [3], and is even higher in patients with active disease when starting anti-myeloma therapy. One population-based study has estimated a tenfold higher risk for viral and a sevenfold higher risk for bacterial infections in multiple myeloma [4]. Severe humoral and cellular immune suppression, particularly during episodes of uncontrolled disease, account mainly for the increased susceptibility for infections. This predisposition is aggravated by the negative consequences of anti-myeloma therapy associated with severe immune suppression including impaired T-cell function and antibody production. Sensitizing the patient’s own immune system against frequent pathogens by vaccination during phases with no or little immunosuppression seems a logical approach in curbing the infection risk. Here, we review the risk of myeloma patients for infections possibly preventable by vaccinations, the available vaccines, their benefits and limitations, and provide recommendations for clinical practice.
Methodology
Relevant literature published after 2000 was identified and reviewed using Medline, Cancerlit, and the Cochrane library. Recent studies presented at ASH, EHA, and EBMT were additionally taken into account. Following data extraction and assessment, a preliminary version was generated and revised by the authors. Comments and suggestions have been incorporated in the paper resulting in a final version, which has been approved by all authors.
Vaccination studies in myeloma are limited often by small numbers of enrolled patients and by laboratory outcome measures, which usually consist of evaluation of antibody titers only, and less frequently by proving clinical effectiveness (Table 1). Moreover, several recommendations are made in analogy to those made for the general population, or for similar diseases. International institutions, such as the center of disease control and prevention (CDC) [5], the World Health Organization (WHO) [6], or professional societies such as National Comprehensive Cancer Network (NCCN®) [7] and other published recommendations for vaccinations, either for the general population, for people aged 65 or older, for patients with impaired immune system [5], or for patients treated with autologous or allogeneic stem cell transplantation [7]. We needed to abstain from grading the recommendations for their strength of evidence, as suggested by the European Society of Microbiology and Infectious Disease [8], because of lack of data from randomized trials in patients with multiple myeloma. This is in accordance with a recent critical review of the Infectious Disease Society of America (IDSA) pointing to the suboptimal strength of scientific evidence for the majority of recommendations, which nevertheless are based on observational studies, clinical experience, and reports of expert committees [9].
Immune suppression in multiple myeloma
Efficient anti-infective defense requires a complex interplay between antigen recognition, antibody response, cellular defense, and humoral factors such as complement. Depressed antibody production against common pathogens has been documented in MGUS patients and is even more pronounced in patients with multiple myeloma, and particularly in those with active disease [10]. The immune dysfunction is further aggravated by varying degrees of lymphopenia, neutropenia, and reduced opsonization and functional impairment of phagocytosis and intracellular killing [10]. Myeloma therapy frequently contributes to cytopenia and immune suppression and may lead to significant disruption of mucosal barriers. Immune senescence may add to immune deficiency in the majority of myeloma patients diagnosed at higher age, as both antibody and cellular response have been shown to be impaired in elderly people [11, 12].
Viruses
Influenza
Influenza virus usually is transmitted through droplets and contact with contaminated surfaces. A person may be infectious before and during symptoms. Influenza spreads around the world in yearly outbreaks, resulting in about three to five million cases of severe illness and about 290,000–650,000 deaths, particularly in young children and in elderly people [13], especially in those with comorbidities or severe immunosuppression. Hemagglutinin and neuraminidase expressed on the membrane of influenza virus are important targets of vaccines, because the former mediates binding of virus to target cells and entry into their genome, and the latter promotes binding to target cells and the release of progeny virus from infected cells [14].
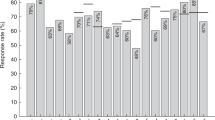
Influenza viruses show a high mutational activity, which requires adaptation of the composition of vaccines in yearly intervals. The trivalent influenza vaccines comprise two serotypes of influenza A and one of influenza B. The quadrivalent vaccine comprises a second serotype of influenza B. Vaccination with influenza induces a humoral immune response against hemagglutinin and less pronounced against neuraminidase glycoproteins [15], particularly the latter protect against intracellular uptake when exposed to the same virus type [16]. Although exposure to live influenza virus creates a strong CD4 T-cell effector response, vaccines usually elicit poor cellular immunity [17]. Clinical studies show seroconversion after vaccination in about 70–80% of patients with malignancies [18, 19] and a Cochrane review on 2275 patients with malignancies revealed a significant, albeit limited reduction in mortality in cancer patients receiving different types of influenza vaccines [20]. In myeloma, a study published two decades ago reported poor response to influenza vaccine [21]. Only 19% of patients developed protective antibody titers to all three strains and 10% against two viral strains of the vaccine. In another study in patients with solid tumors and hematologic malignancies including 15 patients with multiple myeloma, protective titers were obtained in 27% of patients [22], with little further increase after a second boost. However, it is unclear whether a hemagglutinin titer of 1:40 is the right cutoff distinguishing between a clinically relevant protection or not. A more recent study by Hahn et al. [23] showed preexisting humoral immunity against one or more influenza serotypes in 9–19% of the patients. After a single vaccination, the frequency of patients with ‘sufficient’ titers to one strain rose by 20–40%. After a second vaccine boost, the number of patients with assumed protective titers nearly doubled. Two doses of influenza vaccine were automatically given 30 days apart in another study [24]. Rates of seroprotection against all three strains increased from baseline 4% to 49%, and 65% following one, and two doses, respectively [24]. Hence, as influenza antibody testing with the hemagglutination inhibition assay is not established as routine procedure, we recommend that patients without documented immune response should automatically be vaccinated twice within a 4-week interval [25]. No correlation between myeloma therapy or treatment intensity, and seroconversion has been observed in the study by Nordoy [18], while in the study by Branagan et al. [24] active disease requiring therapy, less than partial response, and conventional chemotherapy were associated with lower likelihood for a serological response.
Vaccination with trivalent and the newer quadrivalent influenza vaccines is recommended for all patients with MGUS, SMM, and multiple myeloma, their family members and their care givers [26]. The recommendation for patients is supported by WHO [27], CDC [28] and by NCCN® [29], all of them propose influenza vaccinations in immunocompromised individuals (Table 2). Vaccinating health care providers in long-term care units is supported by the WHO [30], the CDC [31], and by data from a recent review [32], but studies documenting a significant benefit in acute care units are not available. The vaccination should be planned before the start of treatment [33] and before the beginning of a new influenza season, or in a period after the end of treatment with deep response to myeloma therapy.
Varicella zoster
Patients treated with proteasome inhibitors [2], daratumumab [34], high-dose melphalan followed by autologous stem cell transplantation (ASCT) [2], and high doses of glucocorticosteroids [2] have a higher risk for varicella zoster virus (VZV) reactivation. Reactivation of latent virus residing in sensory ganglions leads to active virus production, spread alongside the axons down to the area of skin innervated by that ganglion, inflammation, blisters, and pain [35]. One large study on 9253 myeloma patients reported a hazard ratio of 14.8 for VZV reactivation compared to the general population [4]. Vaccines consisting of live-attenuated herpes virus [36], although found to be safe and active in myeloma patients, were generally not recommended in patients with multiple myeloma with frequently impaired immune system. Inactivation of VZV precludes any potential risk of reinfection. A recent randomized study with a gamma-irradiated and thereby inactivated VZV vaccine was found active in a large group, including around 45% with myeloma of autologous stem cell transplant recipients, dosed once 5–60 days before and three times (30, 60, and 90 days) after ASCT. The vaccination reduced VZV reactivations (8 vs. 21%) significantly during a 2.3–2.4 year follow-up period) and postherpetic complications. The vaccine was safe with no difference in AEs other than in local injection site reactions [37]. A new adjuvanted recombinant VZV glycoprotein E vaccine reduced the risk for VZV reactivation by 97% in elderly individuals of the general population and was well tolerated [38]. A trial with two doses of this vaccine in patients with hematological malignances, including 132 patients with multiple myeloma during or after immunosuppressive therapy, showed a humoral immune response in 80.2% of vaccinated patients with practicably no conversion (0.8%) in those receiving placebo [39]. Only two patients of the active study drug group developed VZV reactivation, as compared to 14 of the placebo arm during a 13 months follow-up period.
Based on these results, a proactive position favoring the use of the recombinant VZV glycoprotein E vaccine over the live-attenuated VZV vaccine seems justified practically in all patients with multiple myeloma, as many of them will receive ASCT and almost all treatment with immunosuppressive drugs. Patients should receive two doses 2–6 months apart. This strategy should be complemented by conventional prophylaxis with acyclovir or valaciclovir for further risk reduction. This is of particular importance in patients receiving proteasome inhibitors, or anti-CD38 antibodies.
Hepatitis A virus
Vaccination with an inactivated hepatitis A vaccine is recommended in nonimmune patients traveling to endemic regions (Southeast Asia, Mediterranean countries, Africa, Middle and South America). Patients should receive two doses given at least 6 months apart to achieve long lasting protection [40], which can be attained in up to 95% of the general population. Prophylaxis with intravenous immunoglobulins is an alternative option for those exposed for only a limited period. Protective anti-hepatitis A antibody titers have been detected in all five immunoglobulin products tested [41, 42].
Hepatitis B virus
Patients planned for therapy with proteasome inhibitors, immunomodulatory drugs, high-dose dexamethasone, monoclonal antibodies, and/or stem cell transplantation should be screened for hepatitis B by testing for HBs-Ag and anti-HBc antibodies [43]. In case of negative HBs-Ag and positive anti-HBc results, patients should be tested for hepatitis B DNA. In patients without evidence of hepatitis B infection, no further action is needed unless the patient lives in, or travels to, areas endemic for hepatitis B or patients who have sexual partners with chronic hepatitis B infection. In those individuals, vaccination with hepatitis B is recommended. In case of HBs-Ag positivity and/or positive hepatitis B DNA, antiviral therapy should be administered [41] concomitantly to anti-myeloma treatments with significant T-cell immunosuppressive activity. The third generation antiviral nucleoside analogues entecavir or tenofovir, are highly active, with almost no risk for developing resistance and are well tolerated, and thus recommended for those patients [44, 45]. Antiviral prophylaxis should be continued for several months and preferably until completion of anti-myeloma therapy, but exact figures from randomized trials are not available. Up to now, the newer and possibly more potent antiviral drugs such as entecavir, adefovir or tenofovir have not systematically been studied in multiple myeloma, but it can be anticipated that those new drugs will be associated with a lower risk for resistance development.
Hepatitis C virus
The same diagnostic procedures recommended for patients subjected to highly immunosuppressive therapy should be applied for hepatitis C screening. Patients with detectable disease documented by hepatitis C virus RNA should receive therapy with direct-acting antivirals, if possible before start of myeloma therapy. In spite of intensive research, there is no vaccine available today [46].
Measles, mumps, and rubella
Vaccination against measles, mumps, and rubella (MMR) is routinely provided by most health care systems of developed countries and there are no reports indicating that patients with multiple myeloma are at greater risk than the general population to develop clinically relevant disease induced by the aforementioned viruses. MMR vaccination usually leads to live long protection, but antibody levels and avidity may wane by up to 25% after 20 years of follow-up [47]. Nevertheless, after allogeneic transplantation, the probability of becoming seronegative was 60% for measles, 73% for mumps, and 52% for rubella in one study [48], which mandates either revaccination of those patients after a safety time period (>24 months) after transplantation or antibody testing against these viruses. Current available vaccines are live-attenuated and should not be used during the first 2 years following ASCT [49].
Bacteria
Pneumococci
Streptococcus pneumonia species are common members of the bacterial flora colonizing the mouth and throat in 5–10% of healthy individuals and are a leading cause of pneumonia, otitis media, blood stream infection including sepsis and bacterial meningitis. The risk for developing a pneumococcal infection is increased in individuals with reduced IgG synthesis, impaired phagocytosis and defective bacterial clearance and higher age [50]. Over 90 serotypes have been identified [51], and two types of vaccines are commonly used to protect against the most important serotypes. The conjugate PCV13 (13-valent pneumococcal conjugate vaccine) vaccine contains purified capsular polysaccharide from 13 serologic strains conjugated to a mutant of diphtheria toxoid (CRM197). The coupling of the T-cell independent pneumococcal polysaccharide antigens to a carrier protein transforms them into T-cell dependent antigens [52] that are more immunogenic than those of the polysaccharide vaccine PV23. This latter vaccine induces antibody production in a T-cell independent manner by acting directly on B cells resulting usually in less efficient antibody production compared to T-cell dependent PCV vaccines.
Pneumococci vaccines have been evaluated in the general population, and in MGUS, SMM, and MM patients. A large randomized study employing a PCV13 vaccine showed 45% fewer episodes of vaccine-type community-associated pneumonia and invasive infections in adults aged ≥65 years [53]. Subsequent to this finding, conjugate vaccines have become the vaccine of choice in elderly individuals. In myeloma patients, substantial antibody responses were observed in about 30–60% of cases to either PCV13 or PPSV23 vaccines. In one study, a response to PV23 vaccination before ASCT was noted in 33% of patients, with a response rate of 73% in those who achieved a CR [54]. Similarly, in another trial, higher antibody responses were reported in patients with well-controlled disease, but antibody titers decreased within few months in most patients [52], an observation reported in another series as well [55]. In MGUS, a high response rate to a PCV13 vaccine was found [56], and in one of these studies, a reasonable correlation between IgG antibody response to four serotypes and opsonophagocytic capacity, but this correlation was not seen in patients with MM [57], where IgG antibodies without opsonophagocytic capacity were observed as well [10]. A study in elderly individuals of the general population aged 70 years or older showed that antibody response to several serotypes can be boosted by using higher doses of PCV7, but this benefit was associated with more adverse events [58], and data supporting this strategy in patients with multiple myeloma are not available as yet. As both PCV13 and PPSV23 vaccine were found to protect against pneumococcal disease in the general population [59, 60], patients should be vaccinated with PCV13 (in case of no previous PCV13 vaccination) followed by PCV23 after 2 months or an even longer interval. PPSV23 vaccination should be repeated in 5-year intervals but antibody response to a boost with PPSV23 may be lower than after primary vaccination [51].
Haemophilus influenzae
Haemophilus influenzae is a common gram-negative human-restricted bacterial pathogen that frequently colonizes the nasopharynx. It can cause local infections, such as otitis media and sinusitis and after breaching the epithelial barriers, it can result in invasive disease, including pneumonia, meningitis, and sepsis [61]. More than 50% of patients with MM lack protective anti-haemophilus influenzae (Hib) antibodies and serum bactericidal activity against Hib is absent in 70% of patients [62]. Vaccination with haemophilus influenzae is recommended in all patients with asplenia and should be considered in patients with MM, although data on the clinical efficacy are limited. One study showed antibody response in 71% of patients vaccinated after ASCT [63].
Meningococci
Low immunoglobulin levels, complement deficiencies, asplenia, and the diagnosis of multiple myeloma are among other well established risk factors for meningococcal disease [64]. One study reported a hazard ratio of 16.6 for patients with MM for developing meningococcal disease compared to controls [2].
Tetravalent capsular polysaccharide conjugate vaccines with improved immunogenicity targeting serotypes A,C,Y,W-135, and protein-based, capsular polysaccharide-free recombinant vaccines targeting serogroup B [64] are available for clinical use. The latter are now widely used for population vaccination programs as serogroup B accounts for the majority of cases [65].
An expert group [8] recommended to use the conjugated tetravalent conjugated vaccine and to consider vaccination against serogroup B as well in asplenic patients with hematological diseases. This seems reasonable in patients with MM in general, and particularly in those with splenectomy [66], complement deficiency and possibly also in the post-hematopoietic stem cell transplant setting.
Diphteria, pertussis, tetanus, and polio
Data on the relevance of vaccination with these pathogens are scarce in conventionally treated patients with MM. In lymphoma and AML patients, significantly more patients lacked protective antibody titers against tetanus and diphtheria after intensive therapy [67]. In patients receiving an allotransplantation a significant loss of antibody protection against tetanus and polio was reported [68, 69]. Pertussis may cause infections in adults, but data on reappearance of pertussis in myeloma patients are limited; noteworthy, protective antibody titers often are decreased in patients after allotransplantation [70]. Overall, there is little information on the immunity against these pathogens in myeloma patients, but vaccination with these antigens is recommended in patients after allogeneic transplantation.
Autologous and allogeneic transplantation
Antibodies for various pathogens including pneumococci, haemophilus, and measles are significantly reduced after autologous [71, 72] and more so after allogeneic stem cell transplantation [73]. Transplanted patients have a higher risk for virus reactivation and develop a more severe course of viral infections [74]. These and other findings prompted the IDSA to consider recipients of allotransplantation as never vaccinated [75], highlighting the need for a full vaccination program. Several recommendations have been published by international and national societies for patients after stem cell transplantation [48, 49]. The NCCN® Guidelines for patients after autologous and allogeneic stem cell transplantation are shown in Table 3. Patients should be vaccinated with vaccines administered during early childhood, and pneumococci, haemophilus influenzae and meningococci, influenza and recombinant VZV vaccine [29]. Due to the poor immune response after allogeneic transplantation, vaccination should be repeated in short intervals (4-week intervals) for most pathogens. The CDC recommends vaccination with MMR in patients 24 months after allogeneic transplantation and without signs of graft versus host disease [5]. There is some inconsistency regarding the appropriate timing of the vaccinations. As patients are prone to increased infection risk shortly after transplantation, some experts recommend to administer seasonal influenza vaccine already a few months after ASCT. A second vaccination should be considered to increase antibody response [76]. Timing vaccination relatively early after transplantation is supported by data showing comparable response rates to PCV vaccination in patients who were vaccinated 3 or 9 months after the transplant [77]. Hence, there are relevant arguments for starting some vaccinations, like influenza and PCV13, already about 3 months after autologous transplantation, but it should be kept in mind that official organizations take a more conservative approach favoring a longer interval between autologous transplantation and vaccination as shown in Table 3 [29].
Monoclonal antibodies, T-cell engagers (BiTEs), CAR-T cells
A small series of patients with RRMM treated with daratumumab showed a similar vaccination response to PCV13 and PPV23, Haemophilus influenza, and seasonal influenza compared to patients receiving non-daratumumab containing regimes [78]. Similar responses likely are to be expected for other CD38 monoclonal antibodies. No information is available for the other above-mentioned treatments. Patients subjected to treatment with BiTEs or CAR-T cells usually are heavily pretreated and often present with severely compromised bone marrow reserve and long lasting impairment of anti-infective immune response. Ideally, patients should be vaccinated before start of rescue therapy with the entire spectrum of vaccines listed in Table 2, with influenza, VZV, and vaccination against encapsulated bacteria (pneumococci, haemophilus influenzae, and meningococci) being most important.
Disease status and vaccination
Common reasoning suggests that patients should be vaccinated before transformation into active myeloma at MGUS or SMM stage, or during remission when there is no or only minor immune suppression by active disease, but scientific support for this notion is available in CLL patients only [79]. Limited evidence suggests that patients on lenalidomide maintenance show an enhanced antibody response from the immune stimulatory effects induced by IMiDs [80], but a recent study in patients on lenalidomide maintenance was unable to confirm this [63]. In patients on daratumumab therapy, a similar vaccination response was reported compared to patients receiving non-daratumumab containing therapy [78]. Patients with scheduled chemotherapy should be vaccinated at least 2 weeks before initiation of chemotherapy [5], upon achievement of best response, 3–6 months after completion of chemotherapy or autologous transplantation, and 6–24 months after allogeneic transplantation. Vaccination with inactivated or live vaccines should not be given either before or about 3 months after treatment with intravenous immunoglobulin therapy because of concerns about effectiveness of vaccines [5].
Family members, close patient contacts, and health care workers
Persons in close contact with the patient should receive all age- and exposure appropriate vaccines and should specifically be vaccinated against influenza, and those aged 65 years or older against pneumococci (Table 4). Patient contacts should be aware that there is a small risk of transferring live vaccines with the exception of MMR [5] to the patient. Studies from several countries show significant immunity gaps against many vaccine-preventable diseases in health care providers highlighting the need for uniform recommendation. Immunity against the spectrum of pathogens vaccinated against during childhood should be ascertained. This is particularly relevant for mumps, rubella, and measles [81, 82]. In case of inadequate antibody response, revaccination is recommended. In addition, health care workers should be vaccinated against hepatitis B, and regularly against influenzae, and depending on specific situations against other pathogens listed in Table 4.
Contraindications, precautions, and side effects
Severely immunosuppressed patients should not receive live vaccines. Myeloma patients, if not in sustained well-controlled remission, are considered immunosuppressed, and thus are not candidates for life vaccines. Vaccination should also be withheld in an individual who had a severe allergic reaction after a previous dose or vaccine component. Vaccination should be deferred in patients with uncontrolled disease, ongoing infections, or other acute illnesses. Presently, there are no contraindications for vaccinating patients with a previous episode of infection with the same class of pathogens the vaccine should provide protection for. For example, vaccination with PCV13 is recommended in a patient even if he had a previous episode of pneumococcal pneumonia, because the vaccine contains serotypes the patient might not have been exposed to.
Modern vaccines usually are very well tolerated. Local reactions, such as areas of redness, swelling, pain, and infrequently induration, may occur at the injection site. Such reactions may increase in severity with each subsequent injection. Very rarely, general reactions such as fever, chills, feeling tired, headache, muscle and joint aches are encountered. Neurological side effects, including Guillain–Barre syndrome (after influenza vaccination), anaphylaxis, bronchospasm, laryngeal edema, generalized collapse, and prolonged unresponsiveness have previously been reported as very rare complications with an incidence of about 1/1,000,000 [83, 84].
Limitations
Many of the available data have been published before the introduction of novel myeloma drugs and treatment strategies, which nowadays result in higher response rates and deeper responses, reducing or even obviating myeloma induced immune suppression. Several studies included small patient numbers, making it difficult to evaluate the validity of their findings. Almost all studies reporting response to vaccination provide data on antibody response only; there is no validation whether a rise in antibody titer to ≥1:40 correlates with the assumed clinical protection, nor are data available on the impact of opsonophagocytic activity on clinical efficacy. Cellular immunity is usually not assessed. Randomized trials providing the scientific evidence for vaccination recommendations in multiple myeloma are available for a few indications only; most of the recommendations rely on clinical observations, consensus of experts, published by international or national societies, observational studies, and on analogies drawn from the general population. In spite of these limitations, thorough review of the existing data and balancing the weight of evidence within a group of experts of the disease likely provides relevant information for clinical care. This was our main objective, which we hope to have accomplished.
Conclusion
Infections are the second major cause of mortality in multiple myeloma, mandating optimization of measures for prevention of infections. Vaccination is one of the greatest achievements of medical research, which has saved the life of millions of people, and an effective preventive strategy in patients with multiple myeloma. Ongoing research has led to the development of genetically engineered VZV vaccines obviating the need of using attenuated live vaccines, and further improvements in efficacy and safety of other vaccines can be expected for the near future. Still, in real world clinical practice, the entire potential of a comprehensive vaccination policy is underused. This work aims to provide the necessary medical background and recommendations for an optimal vaccination strategy in myeloma patients likely to benefit from this important preventive measure.
References
Alemu A, Singh M, Blumberg C, Richards JO, Oaks MK, Thompson MA. Multiple myeloma vaccination patterns in a large health system: a pilot study. J Patient Cent Res Rev. 2017;4:53–9.
Brioli A, Klaus M, Sayer H, Scholl S, Ernst T, Hilgendorf I, et al. The risk of infections in multiple myeloma before and after the advent of novel agents: a 12-year survey. Ann Hematol. 2019;98:713–22.
Kristinsson SY, Tang M, Pfeiffer RM, Bjorkholm M, Goldin LR, Blimark C, et al. Monoclonal gammopathy of undetermined significance and risk of infections: a population-based study. Haematologica. 2012;97:854–8.
Blimark C, Holmberg E, Mellqvist UH, Landgren O, Bjorkholm M, Hultcrantz M, et al. Multiple myeloma and infections: a population-based study on 9253 multiple myeloma patients. Haematologica. 2015;100:107–13.
National Center for Immunization and Respiratory Diseases, General Best Practice Guidelines for Immunization: Best Practices Guidance of the Advisory Committee on Immunization Practices (ACIP): Altered Immunocompetence. 2019. https://www.cdc.gov/vaccines/hcp/acip-recs/general-recs/immunocompetence.html. Accessed 1 Mar 2020.
World Health Organisation: Vaccines and Immunization; recommendations for routine immunization. 2019. https://www.who.int/immunization/policy/immunization_tables/en/. Accessed 1 Mar 2020.
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in OncologyTM. Prevention and Treatment of Cancer-Related Infections. 2020. https://www.nccn.org/professionals/physician_gls/pdf/infections.pdf. Accessed 1 Mar 2020.
Rieger CT, Liss B, Mellinghoff S, Buchheidt D, Cornely OA, Egerer G, et al. Anti-infective vaccination strategies in patients with hematologic malignancies or solid tumors-Guideline of the Infectious Diseases Working Party (AGIHO) of the German Society for Hematology and Medical Oncology (DGHO). Ann Oncol. 2018;29:1354–65.
Khan AR, Khan S, Zimmerman V, Baddour LM, Tleyjeh IM. Quality and strength of evidence of the Infectious Diseases Society of America clinical practice guidelines. Clin Infect Dis. 2010;51:1147–56.
Karlsson J, Andreasson B, Kondori N, Erman E, Riesbeck K, Hogevik H, et al. Comparative study of immune status to infectious agents in elderly patients with multiple myeloma, Waldenstrom’s macroglobulinemia, and monoclonal gammopathy of undetermined significance. Clin Vaccine Immunol. 2011;18:969–77.
Sasaki S, Sullivan M, Narvaez CF, Holmes TH, Furman D, Zheng NY, et al. Limited efficacy of inactivated influenza vaccine in elderly individuals is associated with decreased production of vaccine-specific antibodies. J Clin Investig. 2011;121:3109–19.
Murasko DM, Bernstein ED, Gardner EM, Gross P, Munk G, Dran S, et al. Role of humoral and cell-mediated immunity in protection from influenza disease after immunization of healthy elderly. Exp Gerontol. 2002;37:427–39.
Iuliano AD, Roguski KM, Chang HH, Muscatello DJ, Palekar R, Tempia S, et al. Estimates of global seasonal influenza-associated respiratory mortality: a modelling study. Lancet. 2018;391:1285–300.
Suzuki Y. Sialobiology of influenza: molecular mechanism of host range variation of influenza viruses. Biol Pharm Bull. 2005;28:399–408.
Chen YQ, Wohlbold TJ, Zheng NY, Huang M, Huang Y, Neu KE, et al. Influenza infection in humans induces broadly cross-reactive and protective neuraminidase-reactive antibodies. Cell. 2018;173:417–29.e410.
Krammer F, Fouchier RAM, Eichelberger MC, Webby RJ, Shaw-Saliba K, Wan H, et al. NAction! How can neuraminidase-based immunity contribute to better influenza virus vaccines? mBio. 2018;9:e02332–17.
Devarajan P, Bautista B, Vong AM, McKinstry KK, Strutt TM, Swain SL. New insights into the generation of CD4 memory may shape future vaccine strategies for influenza. Front Immunol. 2016;7:136.
Nordoy T, Aaberge IS, Husebekk A, Samdal HH, Steinert S, Melby H, et al. Cancer patients undergoing chemotherapy show adequate serological response to vaccinations against influenza virus and Streptococcus pneumoniae. Med Oncol. 2002;19:71–8.
Pollyea DA, Brown JM, Horning SJ. Utility of influenza vaccination for oncology patients. J Clin Oncol. 2010;28:2481–90.
Bitterman R, Eliakim-Raz N, Vinograd I, Zalmanovici Trestioreanu A, Leibovici L, Paul M. Influenza vaccines in immunosuppressed adults with cancer. Cochrane Database Syst Rev. 2018;2:Cd008983.
Robertson JD, Nagesh K, Jowitt SN, Dougal M, Anderson H, Mutton K, et al. Immunogenicity of vaccination against influenza, Streptococcus pneumoniae and Haemophilus influenzae type B in patients with multiple myeloma. Br J Cancer. 2000;82:1261–5.
Sanada Y, Yakushijin K, Nomura T, Chayahara N, Toyoda M, Minami Y, et al. A prospective study on the efficacy of two-dose influenza vaccinations in cancer patients receiving chemotherapy. Jpn J Clin Oncol. 2016;46:448–52.
Hahn M, Schnitzler P, Schweiger B, Kunz C, Ho AD, Goldschmidt H, et al. Efficacy of single versus boost vaccination against influenza virus in patients with multiple myeloma. Haematologica. 2015;100:e285–8.
Branagan AR, Duffy E, Albrecht RA, Cooper DL, Seropian S, Parker TL, et al. Clinical and serologic responses after a two-dose series of high-dose influenza vaccine in plasma cell disorders: a prospective, single-arm trial. Clin Lymphoma Myeloma Leuk. 2017;17:296–304.e292.
de Lavallade H, Garland P, Sekine T, Hoschler K, Marin D, Stringaris K, et al. Repeated vaccination is required to optimize seroprotection against H1N1 in the immunocompromised host. Haematologica. 2011;96:307–14.
Dolan GP, Harris RC, Clarkson M, Sokal R, Morgan G, Mukaigawara M, et al. Vaccination of healthcare workers to protect patients at increased risk of acute respiratory disease: summary of a systematic review. Influenza Other Respir Viruses. 2013;7 Suppl 2: 93–6.
World Health Organization, Geneva 2019: Global influenza strategy 2019–2030. https://www.who.int/influenza/global_influenza_strategy_2019_2030/en/. Accessed 27 Nov 2019.
Centers for Disease Control and Prevention, National Center for Immunization and Respiratory Diseases (NCIRD). 2019. https://www.cdc.gov/flu/prevent/vaccinations.htm. Accessed 27 Nov 2019.
Referenced with permission from the NCCN Guidelines for Prevention and Treatment of Cancer-Related Infections V.1.2020. National Comprehensive Cancer Network, Inc. 2019. All rights reserved. Accessed 4 Mar 2020. www.NCCN.org. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way.
World Health Organisation: Recommendations for routine immunization - summary tables, table 4. 2019. https://www.who.int/immunization/policy/Immunization_routine_table4_FR.pdf?ua=1. Accessed 28 Feb 2020.
Centers for Disease Control and Prevention, National Center for Immunization and Respiratory Diseases (NCIRD). 2016. https://www.cdc.gov/vaccines/adults/rec-vac/hcw.html. Accessed 28 Feb 2020.
Maltezou HC, Poland GA. Immunization of health-care providers: necessity and public health policies. Healthcare. 2016;4:47.
Alemu A, Richards JO, Oaks MK, Thompson MA. Vaccination in multiple myeloma: review of current literature. Clin Lymphoma Myeloma Leuk. 2016;16:495–502.
Drgona L, Gudiol C, Lanini S, Salzberger B, Ippolito G, Mikulska M. ESCMID Study Group for Infections in Compromised Hosts (ESGICH) Consensus Document on the safety of targeted and biological therapies: an infectious diseases perspective (Agents targeting lymphoid or myeloid cells surface antigens [II]: CD22, CD30, CD33, CD38, CD40, SLAMF-7 and CCR4). Clin Microbiol Infect. 2018;24:S83–94.
Schmader K. Herpes zoster. Clin Geriatr Med. 2016;32:539–53.
Pandit A, Leblebjian H, Hammond SP, Laubach JP, Richardson PG, Baden LR, et al. Safety of live-attenuated measles-mumps-rubella and herpes zoster vaccination in multiple myeloma patients on maintenance lenalidomide or bortezomib after autologous hematopoietic cell transplantation. Bone Marrow Transplant. 2018;53:942–5.
Winston DJ, Mullane KM, Cornely OA, Boeckh MJ, Brown JW, Pergam SA, et al. Inactivated varicella zoster vaccine in autologous haemopoietic stem-cell transplant recipients: an international, multicentre, randomised, double-blind, placebo-controlled trial. Lancet. 2018;391:2116–27.
Cunningham AL, Lal H, Kovac M, Chlibek R, Hwang SJ, Diez-Domingo J, et al. Efficacy of the herpes zoster subunit vaccine in adults 70 years of age or older. N Engl J Med. 2016;375:1019–32.
Dagnew AF, Ilhan O, Lee WS, Woszczyk D, Kwak JY, Bowcock S, et al. Immunogenicity and safety of the adjuvanted recombinant zoster vaccine in adults with haematological malignancies: a phase 3, randomised, clinical trial and post-hoc efficacy analysis. Lancet Infect Dis. 2019;19:988–1000.
Centers for Disease Control and Prevention, National Center for Immunization and Respiratory Diseases, Department of Health and Human Services. Vaccine Information Statement (Interim), Hepatitis A Vaccine (7/28/2020), 42 U.S.C. § 300aa-26. https://www.cdc.gov/vaccines/hcp/vis/vis-statements/hep-a.html. Accessed 28 Jul 2020.
Terrault NA, Lok ASF, McMahon BJ, Chang KM, Hwang JP, Jonas MM, et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance. Hepatology. 2018;67:1560–99.
Lee S, Kim HW, Kim KH. Antibodies against hepatitis A and hepatitis B virus in intravenous immunoglobulin products. J Korean Med Sci. 2016;31:1937–42.
Hwang JP, Somerfield MR, Alston-Johnson DE, Cryer DR, Feld JJ, Kramer BS, et al. Hepatitis B virus screening for patients with cancer before therapy: American Society of Clinical Oncology Provisional Clinical Opinion Update. J Clin Oncol. 2015;33:2212–20.
Lampertico P, Agarwal K, Berg T, Buti M, Janssen HLA, Papatheodoridis G, et al. European Association for the Study of the Liver. EASL 2017 Clinical Practice Guidelines on the management of hepatitis B virus infection. J Hepatol. 2017;67:370–98.
Sarmati L, Andreoni M, Antonelli G, Arcese W, Bruno R, Coppola N, et al. Recommendations for screening, monitoring, prevention, prophylaxis and therapy of hepatitis B virus reactivation in patients with haematologic malignancies and patients who underwent haematologic stem cell transplantation-a position paper. Clin Microbiol Infect. 2017;23:935–40.
Duncan JD, Urbanowicz RA, Tarr AW, Ball JK. Hepatitis C virus vaccine: challenges and prospects. Vaccines. 2020;8:1–23.
Kontio M, Jokinen S, Paunio M, Peltola H, Davidkin I. Waning antibody levels and avidity: implications for MMR vaccine-induced protection. J Infect Dis. 2012;206:1542–8.
Ljungman P, Lewensohn-Fuchs I, Hammarstrom V, Aschan J, Brandt L, Bolme P, et al. Long-term immunity to measles, mumps, and rubella after allogeneic bone marrow transplantation. Blood. 1994;84:657–63.
Ljungman P, Cordonnier C, Einsele H, Englund J, Machado CM, Storek J, et al. Vaccination of hematopoietic cell transplant recipients. Bone Marrow Transplant. 2009;44:521–6.
Simell B, Lahdenkari M, Reunanen A, Kayhty H, Vakevainen M. Effects of ageing and gender on naturally acquired antibodies to pneumococcal capsular polysaccharides and virulence-associated proteins. Clin Vaccin Immunol. 2008;15:1391–7.
Geno KA, Gilbert GL, Song JY, Skovsted IC, Klugman KP, Jones C, et al. Pneumococcal capsules and their types: past, present, and future. Clin Microbiol Rev. 2015;28:871–99.
Bahuaud M, Bodilis H, Malphettes M, Maugard Landre A, Matondo C, Bouscary D, et al. Immunogenicity and persistence of the 13-valent pneumococcal conjugate vaccine (PCV13) in patients with untreated smoldering multiple myeloma (SMM): a pilot study. Heliyon. 2017;3:e00441.
Bonten MJ, Huijts SM, Bolkenbaas M, Webber C, Patterson S, Gault S, et al. Polysaccharide conjugate vaccine against pneumococcal pneumonia in adults. N Engl J Med. 2015;372:1114–25.
Hinge M, Ingels HA, Slotved HC, Molle I. Serologic response to a 23-valent pneumococcal vaccine administered prior to autologous stem cell transplantation in patients with multiple myeloma. APMIS. 2012;120:935–40.
Mustafa SS, Shah D, Bress J, Jamshed S. Response to PCV13 vaccination in patients with multiple myeloma versus healthy controls. Hum Vaccines Immunother. 2019;15:452–4.
Pasiarski M, Sosnowska-Pasiarska B, Grywalska E, Stelmach-Goldys A, Kowalik A, Gozdz S, et al. Immunogenicity and safety of the 13-valent pneumococcal conjugate vaccine in patients with monoclonal gammopathy of undetermined significance—relationship with selected immune and clinical parameters. Clin Interv Aging. 2019;14:1741–9.
Karlsson J, Roalfe L, Hogevik H, Zancolli M, Andreasson B, Goldblatt D, et al. Poor correlation between pneumococcal IgG and IgM titers and opsonophagocytic activity in vaccinated patients with multiple myeloma and Waldenstrom’s macroglobulinemia. Clin Vaccin Immunol. 2016;23:379–85.
Lode H, Schmoele-Thoma B, Gruber W, Ahlers N, Fernsten P, Baker S, et al. Dose-ranging study of a single injection of pneumococcal conjugate vaccine (1 x, 2 x, or 4 x) in healthy subjects aged 70 years or older. Vaccine. 2011;29:4940–6.
Harboe ZB, Dalby T, Weinberger DM, Benfield T, Molbak K, Slotved HC, et al. Impact of 13-valent pneumococcal conjugate vaccination in invasive pneumococcal disease incidence and mortality. Clin Infect Dis. 2014;59:1066–73.
Andrews NJ, Waight PA, George RC, Slack MP, Miller E. Impact and effectiveness of 23-valent pneumococcal polysaccharide vaccine against invasive pneumococcal disease in the elderly in England and Wales. Vaccine. 2012;30:6802–8.
High NJ, Fan F, Schwartzman JD. Chapter 97—haemophilus influenzae. Molecular medical microbiology, 2nd ed. vol. 3. Amsterdam: Academic Press; 2015. pp 1709–28.
Nix EB, Hawdon N, Gravelle S, Biman B, Brigden M, Malik S, et al. Risk of invasive Haemophilus influenzae type b (Hib) disease in adults with secondary immunodeficiency in the post-Hib vaccine era. Clin Vaccine Immunol. 2012;19:766–71.
Palazzo M, Shah GL, Copelan O, Seier K, Devlin SM, Maloy M, et al. Revaccination after autologous hematopoietic stem cell transplantation is safe and effective in patients with multiple myeloma receiving lenalidomide maintenance. Biol Blood Marrow Transplant. 2018;24:871–6.
Feldman C, Anderson R. Meningococcal pneumonia: a review. Pneumonia. 2019;11:3.
Bennett DE, Meyler KL, Cafferkey MT, Cunney RJ. Diversity of meningococci associated with invasive meningococcal disease in the Republic of Ireland over a 19 year period, 1996–2015. PloS ONE. 2020;15:e0228629.
Kristinsson SY, Gridley G, Hoover RN, Check D, Landgren O. Long-term risks after splenectomy among 8,149 cancer-free American veterans: a cohort study with up to 27 years follow-up. Haematologica. 2014;99:392–8.
Einarsdottir S, Ljungman P, Kaijser B, Nicklasson M, Horal P, Norder H, et al. Humoral immunity to tetanus, diphtheria and polio in adults after treatment for hematological malignancies. Vaccine. 2020;38:1084–8.
Ljungman P, Wiklund-Hammarsten M, Duraj V, Hammarstrom L, Lonnqvist B, Paulin T, et al. Response to tetanus toxoid immunization after allogeneic bone marrow transplantation. J Infect Dis. 1990;162:496–500.
Parkkali T, Ruutu T, Stenvik M, Kuronen T, Kayhty H, Hovi T, et al. Loss of protective immunity to polio, diphtheria and Haemophilus influenzae type b after allogeneic bone marrow transplantation. APMIS. 1996;104:383–8.
Suzuki N, Mizue N, Hori T, Hatakeyama N, Kudoh T, Tsutsumi H. Pertussis in adolescence after unrelated cord blood transplantation. Bone Marrow Transplant. 2003;32:967.
Nordoy T, Husebekk A, Aaberge IS, Jenum PA, Samdal HH, Flugsrud LB, et al. Humoral immunity to viral and bacterial antigens in lymphoma patients 4-10 years after high-dose therapy with ABMT. Serological responses to revaccinations according to EBMT guidelines. Bone Marrow Transplant. 2001;28:681–7.
Renaud L, Schraen S, Fouquet G, Guidez S, Demarquette H, Nudel M, et al. Response to pneumococcal vaccination in multiple myeloma. Cancer Med. 2019;8:3822–30.
Cordonnier C, Einarsdottir S, Cesaro S, Di Blasi R, Mikulska M, Rieger C, et al. Vaccination of haemopoietic stem cell transplant recipients: guidelines of the 2017 European Conference on Infections in Leukaemia (ECIL 7). Lancet Infect Dis. 2019;19:e200–12.
Inazawa N, Hori T, Nojima M, Saito M, Igarashi K, Yamamoto M, et al. Virus reactivations after autologous hematopoietic stem cell transplantation detected by multiplex PCR assay. J Med Virol. 2017;89:358–62.
Rubin LG, Levin MJ, Ljungman P, Davies EG, Avery R, Tomblyn M, et al. 2013 IDSA clinical practice guideline for vaccination of the immunocompromised host. Clin Infect Dis. 2014;58:309–18.
Gueller S, Allwinn R, Mousset S, Martin H, Wieters I, Herrmann E, et al. Enhanced immune response after a second dose of an AS03-adjuvanted H1N1 influenza A vaccine in patients after hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2011;17:1546–50.
Cordonnier C, Labopin M, Chesnel V, Ribaud P, De La Camara R, Martino R, et al. Randomized study of early versus late immunization with pneumococcal conjugate vaccine after allogeneic stem cell transplantation. Clin Infect Dis. 2009;48:1392–401.
Frerichs KA, Bosman PWC, Nijhof IS, Zweegman S, van de Donk N. Cytomegalovirus reactivation in a patient with extensively pretreated multiple myeloma during daratumumab treatment. Clin Lymphoma Myeloma Leuk. 2019;19:e9–11.
Hartkamp A, Mulder AH, Rijkers GT, van Velzen-Blad H, Biesma DH. Antibody responses to pneumococcal and haemophilus vaccinations in patients with B-cell chronic lymphocytic leukaemia. Vaccine. 2001;19:1671–7.
Noonan K, Rudraraju L, Ferguson A, Emerling A, Pasetti MF, Huff CA, et al. Lenalidomide-induced immunomodulation in multiple myeloma: impact on vaccines and antitumor responses. Clin Cancer Res. 2012;18:1426–34.
Maltezou HC, Poland GA. Immunization of healthcare personnel in Europe: time to move forward with a common program. Vaccine. 2020;8:3187–90.
Government of Canada. Immunization of workers: Canadian Immunization Guide for Health Professionals. 2019. https://www.canada.ca/en/public-health/services/publications/healthy-living/canadian-immunization-guide-part-3-vaccination-specific-populations/page-11-immunization-workers.html#p3c10t1. Accessed 31 Mar 2020.
U.S. Department of Health and Human Services (HHS), Office of Infectious Disease and HIV/AIDS Policy. 2020. https://www.vaccines.gov/basics/safety/side_effects. Accessed 29 Feb 2020.
Plotkin SA, Offit PA, DeStefano F, Larson HJ, Arora NK, Zuber PLF, et al. The science of vaccine safety: summary of meeting at Wellcome Trust. Vaccine. 2020;38:1869–80.
Acknowledgements
This work was supported in part by the Austrian Forum against Cancer. We thank NCCN® for permission to reproduce the figure on “recommendations for vaccination for patients with autologous or allogeneic stem cell transplantation” from the NCCN® Guidelines Version 1.2020: Prevention and Treatment of Cancer-Related Infections.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ludwig, H., Boccadoro, M., Moreau, P. et al. Recommendations for vaccination in multiple myeloma: a consensus of the European Myeloma Network. Leukemia 35, 31–44 (2021). https://doi.org/10.1038/s41375-020-01016-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41375-020-01016-0
This article is cited by
-
Cytokine-responsive T- and NK-cells portray SARS-CoV-2 vaccine-responders and infection in multiple myeloma patients
Leukemia (2024)
-
Monitoring, prophylaxis, and treatment of infections in patients with MM receiving bispecific antibody therapy: consensus recommendations from an expert panel
Blood Cancer Journal (2023)
-
Effects of heat-sensitive moxibustion plus Chinese medication on the expression of serum inflammatory indicators and microRNAs in patients with multiple myeloma after chemotherapy
Journal of Acupuncture and Tuina Science (2023)
-
Impfungen in der Hämatologie und Onkologie
best practice onkologie (2023)
-
Management of patients with multiple myeloma and COVID-19 in the post pandemic era: a consensus paper from the European Myeloma Network (EMN)
Leukemia (2023)