Abstract
Background
Failure to reach full oral feeding remains a significant barrier for premature infants to discharge home. Postmenstrual age (PMA) at first oral feeding is significantly associated with the length of hospital stay (LOS).
Methods
Single-center QI to introduce oral feeding to infants on high-flow nasal cannula (HFNC) by reducing the flow to 2 L during feeds.
Global aim
To reduce PMA at first oral feeding and reduce the LOS.
SMART aim
To introduce oral feeds in 40% of infants who are on ≤4 L HFNC by the end of 12 months.
Results
Over 12 months, SMART aim reached with 100% enrollment. PMA at first oral feeding decreased from a median of 42.4w ((IQR) (40,46.6) to 37.8w (35.8,43.2), PMA at discharge decreased from 47w (44.6,50.7) to 42.6w (41.3,48.8).
Conclusion
Allowing oral feeding in infants while on HFNC is feasible. This approach can significantly reduce PMA at first and full oral feeding.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
American Academy of Pediatrics Committee on Fetus and Newborn. Hospital discharge of the high-risk neonate. Pediatrics. 2008;122:1119–26.
Bakewell-Sachs S, Medoff-Cooper B, Escobar GJ, Silber JH, Lorch SA. Infant functional status: the timing of physiologic maturation of premature infants. Pediatrics. 2009;123:e878–86.
Edwards L, Cotten CM, Smith PB, Goldberg R, Saha S, Das A, et al. Inadequate oral feeding as a barrier to discharge in moderately preterm infants. J Perinatol. 2019;39:1219–28.
Jadcherla SR, Wang M, Vijayapal AS, Leuthner SR. Impact of prematurity and co-morbidities on feeding milestones in neonates: A retrospective study. J Perinatol. 2010;30:201–8.
Brumbaugh JE, Colaizy TT, Saha S, Van Meurs KP, Das A, Walsh MC, et al. Oral feeding practices and discharge timing for moderately preterm infants. Early Hum Dev. 2018;120:46–52.
Anderson E, Gregoski MJ, Gehle D, Head WT, Hardy KT, Chapman A, et al. Severity of respiratory disease is correlated with time of first oral feeding and need for a gastrostomy tube at discharge in premature infants born at <30 weeks of gestation. Pediatr Pul. 2022;57:193–9.
de Jesus Brito S, Tsopanoglou SP, Galvão EL, de Deus FA, de Lima VP. Can high-flow nasal cannula reduce the risk of bronchopulmonary dysplasia compared with CPAP in preterm infants? A systematic review and meta-analysis. BMC Pediatr. 2021;21:1–9.
Healy LI, Corcoran P, Murphy BP. High-flow nasal cannulae, bronchopulmonary dysplasia and retinopathy of prematurity. Ir Med J. 2019;112:1–7.
Hoffman SB, Terrell N, Driscoll CH, Davis NL. Impact of high-flow nasal cannula use on neonatal respiratory support patterns and length of stay. Respir Care. 2016;61:1299–304.
Canning A, Fairhurst R, Chauhan M, Weir KA. Oral feeding for infants and children receiving nasal continuous positive airway pressure and high-flow nasal cannula respiratory supports: a survey of practice. Dysphagia. 2020;35:443–54.
Leibel SL, Castro M, McBride T, Hassall K, Sarmiento K, Ye XY, et al. Comparison of continuous positive airway pressure versus High flow nasal cannula for Oral feeding Preterm infants (CHOmP): randomized pilot study. J Matern-Fetal Neonatal Med. 2022;35:951–7.
Jadcherla SR, Bhandari V “pressure” to feed the preterm newborn: Associated with “positive” outcomes? Vol. 82, Pediatric Research. Nature Publishing Group; 2017. p. 899–900.
Dalgleish SR, Kostecky LL, Blachly N. Eating in “SINC”: Safe individualized nipple-feeding competence, a quality improvement project to explore infant-driven oral feeding for very premature infants requiring noninvasive respiratory support. Neonatal Netw. 2016;35:217–27.
Tubbs-Cooley HL, Pickler RH, Meinzen-Derr JK. Missed oral feeding opportunities and preterm infants’ time to achieve full oral feedings and neonatal intensive care unit discharge. Am J Perinatol. 2015;32:1–8.
Gentle SJ, Meads C, Ganus S, Barnette E, Munkus K, Carlo WA, et al. Improving time to independent oral feeding to expedite hospital discharge in preterm infants. Pediatrics. 2022;149:e2021052023.
Ludwig S, Waitzman K. Changing feedings documentation to reflect infant-driven feeding practice. Newborn Infant Nurs Rev. 2007;7:156–60.
Canning A, Clarke S, Thorning S, Chauhan M, Weir KA. Oral feeding for infants and children receiving nasal continuous positive airway pressure and high flow nasal cannula: a systematic review. BMC Pediatr. 2021;21:83. https://doi.org/10.1186/s12887-021-02531-4. Published 2021 Feb 17.
Dumpa V, Kamity R, Ferrara L, Akerman M, Hanna N. The effects of oral feeding while on nasal continuous positive airway pressure (NCPAP) in preterm infants. J Perinatol. 2020;40:909–15.
Shetty S, Hunt K, Douthwaite A, Athanasiou M, Hickey A, Greenough A. High-flow nasal cannula oxygen and nasal continuous positive airway pressure and full oral feeding in infants with bronchopulmonary dysplasia. Arch Dis Child Fetal Neonatal Ed. 2016;101:F408–11.
Wilkinson D, Andersen C, O’Donnell CP, De Paoli AG, Manley BJ. High flow nasal cannula for respiratory support in preterm infants. Cochrane Database OF Systematic Reviews. 2016;2016 Update in: Cochrane Database Syst Rev. 2023;2023.
Luo K, Huang Y, Xiong T, Tang J. High-flow nasal cannula versus continuous positive airway pressure in primary respiratory support for preterm infants: A systematic review and meta-analysis. Front Pediatr. 2022;10:1–13.
Greene Z, O’Donnell CPF, Walshe M Oral stimulation for promoting oral feeding in preterm infants. Cochrane Database Syst Rev. 2016;2016.
Greene Z, O’Donnell CPF, Walshe M Oral stimulation for promoting oral feeding in preterm infants. Cochrane Database Syst Rev. 2023; 2023.
Elsewadi BF, Samson N, Nadeau C, Vanhaverbeke K, Nguyen N, Alain C, et al. Safety of bottle-feeding under nasal respiratory support in preterm lambs with and without tachypnoea. Front Physiol. 2022;12:1–11.
Ferrara L, Bidiwala A, Sher I, Pirzada M, Barlev D, Islam S, et al. Effect of nasal continuous positive airway pressure on the pharyngeal swallow in neonates. J Perinatol. 2017;37:398–403.
Shimzu D, Araki S, Kawamura M, Kuwamura M, Suga S, Miyake F, et al. Impact of hgh flow nasal cannula oxygen on oral feeding chronic lung disease. J Occup Environ Hyg. 2019;41:131–8.
Acknowledgements
Fig. 2 is created by biorender.com. We used the SQUIRE guideline to outline our manuscript, as the Journal of Perinatology Author Guidelines suggested. Openai.com used with rephrasing function by HYA for originally written texts. Study data were collected and managed using REDCap electronic data capture tools hosted at University Hospital. REDCap 13.5.3-2023 Vanderbilt University. Available from https://project-redcap.org/UL1TR002548.
Author information
Authors and Affiliations
Contributions
MB and RMR provided leadership and supervision in designing the QI study. HYA led the study in the unit and wrote the manuscript. SR performed all initial oral feeding safety evaluations on HFNC for each infant enrolled in the new protocol. CN (nurse practitioner), MP (bedside nurse), and TF (bedside nurse) provided valuable study support with our clinical colleagues in the NICU. RMR performed the statistical analyses and created the control charts. MB and RMR contributed to major revisions of the manuscript. SR, CN, MP, and TF revised and contributed to the manuscript. All authors read and agreed to the last version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Institutional Review Board
IRB exempted the study.
Supplemental Materials
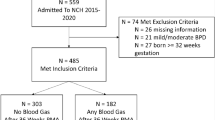
Detailed diagram for infants that were not analyzed, the bedside daily feeding evaluation forms, PDSA summary table, table with infants who needed g tube at discharge.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yildiz Atar, H., Ryan, R.M., Ricciardi, S. et al. Introduction of oral feeding in premature infants on high flow nasal cannula in a level IV neonatal intensive care unit: a quality improvement initiative. J Perinatol (2024). https://doi.org/10.1038/s41372-024-01917-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41372-024-01917-3