Abstract
Objective
To establish normal reference values for tissue oxygen delivery and consumption in preterm infants and demonstrate the usefulness of the integrated evaluation of hemodynamics (IEH) in preterm infants with compromised systemic circulation (CSC).
Methods
This study included 32 stable preterm infants and 6 infants (selected cases) who underwent IEH. IEH is a multimodal approach which integrates clinical parameters: data obtained from near-infrared spectroscopy (NIRS) and targeted neonatal echocardiography (TNE).
Results
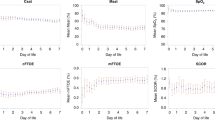
Thirty-two hemodynamically stable preterm infants underwent 57 IEH studies. The mean (10th and 90th percentiles) were 0.23 (0.14 and 0.29) for cerebral fractional oxygen extraction (crFOE), 0.2 (0.13 and 0.24) for renal fractional oxygen extraction (rnFOE), and 0.22 (0.19 and 0.27) for mesenteric fractional oxygen extraction (msFOE). The time to full clinical recovery in all sick infants after the change of management was between 4 and 48 h.
Conclusion
IEH was useful in targeting the management of preterm infants with CSC.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Elsayed YN, Fraser D. Integrated evaluation of neonatal hemodynamics program optimizing organ perfusion and performance in critically ill neonates, Part 1: Understanding physiology of neonatal hemodynamics. Neonatal Netw. 2016;35:143–150.
Elsayed YN, Fraser D. Integrated evaluation of neonatal hemodynamics, Part 2: Systematic bedside assessment. Neonatal Netw. 2016;35:192–203.
Elsayed YN, Amer R, Seshia MM. The impact of integrated evaluation of hemodynamics using targeted neonatal echocardiography with indices of tissue oxygenation: a new approach. J Perinatol. 2017;37:527–35.
Mertens L, Seri I, Marek J, Arlettaz R, Barker P, McNamara P, et al. Targeted neonatal echocardiography in the neonatal intensive care unit: practice guidelines and recommendations for training. Eur J Echocardiogr. 2011;12:715–36.
Limperopoulos C, Gauvreau KK, O’Leary H, Moore M, Bassan H, Eichenwald EC. et al. Cerebral hemodynamic changes during intensive care of preterm infants. Pediatrics. 2008;122:e1006–13 [Internet].
Liem KD, Greisen G. Monitoring of cerebral haemodynamics in newborn infants. Early Hum Dev. 2010;86:155–8 [Internet].
Scheeren TWL, Saugel B. Journal of clinical monitoring and computing 2016 end of year summary: monitoring cerebral oxygenation and autoregulation. J Clin Monit Comput. 2017;31:241–6.
Amer R, Kalash R, Seshia MM, Elsayed YN. The impact of integrated evaluation of hemodynamics on management of preterm infants with late-onset compromised systemic circulation. Am J Perinatol. 2017;34:1011–9.
El-Khuffash AF, McNamara PJ. Neonatologist-performed functional echocardiography in the neonatal intensive care unit. Semin Fetal Neonatal Med. 2011;16:50–60.
Zubrow AB, Hulman S, Kushner H, Falkner B. Determinants of blood pressure in infants admitted to neonatal intensive care units: a prospective multicenter study. Philadelphia Neonatal Blood Pressure Study Group. J Perinatol. 1995;15:470–9.
Pichler G, Binder C, Avian A, Beckenbach E, Schmölzer GM, Urlesberger B. Reference ranges for regional cerebral tissue oxygen saturation and fractional oxygen extraction in neonates during immediate transition after birth. J Pediatr. 2013;163:1558–63.
Greisen G, Leung T, Wolf M. Has the time come to use near-infrared spectroscopy as a routine clinical tool in preterm infants undergoing intensive care? Philos Trans R Soc A Math Phys Eng Sci. 2011;369:4440–51.
Caille V, Squara P. Oxygen uptake-to-delivery relationship: a way to assess adequate flow. Crit Care. 2006;10(Suppl. 3):S4.
Andersen CC, Stark MJ. Haemoglobin transfusion threshold in very preterm newborns: a theoretical framework derived from prevailing oxygen physiology. Med Hypotheses. 2012;78:71–4 [Internet].
Lauscher P, Lauscher S, Kertscho H, Habler O, Meier J. Hyperoxia reversibly alters oxygen consumption and metabolism. Science. 2012;2012:410321. abstract [Internet].
Lister G, Walter TK, Versmold HT, Dallman PR, Rudolph AM. Oxygen delivery in lambs: cardiovascular and hematologic development. Am J Physiol. 1979;237:H668–75.
Wilkening RB, Meschia G. Fetal oxygen uptake, oxygenation, and acid-base balance as a function of uterine blood flow. Am J Physiol. 1983;244:H749–55 [Internet].
Noori S, Seri I. Evidence-based versus pathophysiology-based approach to diagnosis and treatment of neonatal cardiovascular compromise. Semin Fetal Neonatal Med. 2015;20:238–45 [Internet].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Elsayed, Y.N., Louis, D., Ali, Y.H. et al. Integrated evaluation of hemodynamics: a novel approach for the assessment and management of preterm infants with compromised systemic circulation. J Perinatol 38, 1337–1343 (2018). https://doi.org/10.1038/s41372-018-0188-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-018-0188-6
This article is cited by
-
Renal tissue oxygenation and development of AKI in preterm neonates born < 32 weeks’ gestational age in the first week of age
Journal of Perinatology (2024)
-
A new physiologic-based integrated algorithm in the management of neonatal hemodynamic instability
European Journal of Pediatrics (2022)
-
A new intestinal ultrasound integrated approach for the management of neonatal gut injury
European Journal of Pediatrics (2022)
-
Perioperative management of arteriovenous malformation guided by integrated evaluation of hemodynamics
European Journal of Pediatrics (2021)
-
The perfusion index histograms predict patent ductus arteriosus requiring treatment in preterm infants
European Journal of Pediatrics (2021)