Abstract
In this cohort study, we determined time to blood pressure (BP) control and its predictors among hypertensive PLHIV enrolled in integrated hypertension-HIV care based on the World Health Organization (WHO) HEARTS strategy at Mulago Immunosuppression Clinic in Uganda. From August 2019 to March 2020, we enrolled hypertensive PLHIV aged \(\ge\)18 years and initiated Amlodipine 5 mg mono-therapy for BP (140–159)/(90–99) mmHg or Amlodipine 5 mg/Valsartan 80 mg duo-therapy for BP ≥ 160/90 mmHg. Patients were followed with a treatment escalation plan until BP control, defined as BP < 140/90 mmHg. We used Cox proportional hazards models to identify predictors of time to BP control. Of 877 PLHIV enrolled (mean age 50.4 years, 62.1% female), 30% received mono-therapy and 70% received duo-therapy. In the monotherapy group, 66%, 88% and 96% attained BP control in the first, second and third months, respectively. For patients on duo-therapy, 56%, 83%, 88% and 90% achieved BP control in the first, second, third, and fourth months, respectively. In adjusted Cox proportional hazard analysis, higher systolic BP (aHR 0.995, 95% CI 0.989-0.999) and baseline ART tenofovir/lamivudine/efavirenz (aHR 0.764, 95% CI 0.637–0.917) were associated with longer time to BP control, while being on ART for >10 years was associated with a shorter time to BP control (aHR 1.456, 95% CI 1.126–1.883). The WHO HEARTS strategy was effective at achieving timely BP control among PLHIV. Additionally, monotherapy anti-hypertensive treatment for stage I hypertension is a viable option to achieve BP control and limit pill burden in resource limited HIV care settings.
Similar content being viewed by others
Background
Effective antiretroviral therapy (ART) has improved survival in persons living with HIV (PLHIV) [1]. This has resulted from improved programmatic HIV care world over, most importantly in sub-Saharan Africa (SSA) where the burden of disease is highest [2, 3]. With increased life expectancy, the burden of hypertension and associated cardiovascular disease in PLHIV has increased [4,5,6].
To address the care of hypertension in programmatic HIV settings, the Joint United Nations Program on HIV/AIDS (UNAIDS) adopted the strategy of integrating hypertension screening and treatment into already established HIV care systems [7,8,9]. Prospectively, multiple countries including in SSA have adopted this approach. Common challenges in these settings have been lack of basic hypertension medication, lack of training on hypertension care for frontline HIV care givers as well as limited diagnostic capabilities for secondary hypertension and complications [9,10,11].
The 8th Joint National Committee (JNC 8) and the European Cardiology Society guidelines for the management of hypertension recommend the initiation of hypertension treatment with preferably two agents at small doses with preference given to thiazide diuretics, calcium channel blockers and Angiotensin-converting enzyme inhibitors or Angiotensin receptor blockers in black populations. The target for treatment is optimized blood pressure control within a month, and failure of which is the recommendation to titrate medication doses and number of agents [12, 13].
To integrate hypertension care in routine HIV services at Mulago National Referral Hospital, Immunosuppression (ISS) clinic, we adapted a treatment protocol for hypertension based on the World Health Organization (WHO) HEARTS technical package for hypertension treatment [14]. The HEARTS-based treatment protocol guided clinicians on the stepwise titration of hypertension medications from either low dose monotherapy or duo-therapy depending on the patient’s baseline blood pressures [15].
In this study, we sought to determine the time to blood pressure control and its predictors among adult hypertensive PLHIV who received integrated treatment for hypertension and HIV based on the adapted WHO HEARTS protocol. Additionally, we aimed to determine if monotherapy for patients with stage I hypertension was a viable option to control blood pressure and limit pill burden in the HIV clinical setting.
Methods
Study setting and design
This was a prospective cohort study at the Mulago ISS clinic located within Mulago National Referral Hospital complex in Kampala, Uganda. The clinic provides comprehensive HIV services to over 16,500 PLHIV. Since August 2019, the clinic has been providing integrated HIV and hypertension care.
Study participants and inclusion criteria
Between August 2019 and March, 2020, we enrolled consented PLHIV \(\ge\)18 years newly diagnosed treatment-naïve hypertensive patients while in HIV care. Patients were followed-up for 12 months up to March 2021. A diagnosis of hypertension was based on two repeat blood pressure (BP) measurements of systolic BP ≥ 140 or diastolic BP ≥ 90 mmHg or both, at least a week apart, after a five-minute rest in a sitting position in a clinic setting in accordance with the American Heart Association guidelines [16]
Intervention
The hypertension and HIV integration implementation package was earlier published and included, healthy lifestyle counseling, use of a simplified, stepwise hypertension treatment protocol, access to hypertension medicines to patients at no cost, prescribing of hypertension medicines by non-physician health workers and established systems for monitoring integrated care[15] (Fig. 1).
Three hypertension medicines were available for prescription by health workers: Amlodipine 5 mg and 10 mg, Valsartan- 80 mg and 160 mg and Hydrochlorothiazide- 12.5 mg and 25 mg.
Patients with baseline BP between (140–159)/(90–99) mmHg were initiated on Amlodipine 5 mg monotherapy while those with baseline blood pressures of ≥160/90 mmHg were started on Amlodipine 5 mg and Valsartan 80 mg duo-therapy. Patients were reviewed at the clinic monthly until they attained BP control defined as a blood pressure less than 140/90 mmHg. During each clinic visit, single BP readings were taken after 5 min rest following the same baseline protocol and titration of hypertension medications was effected as shown in Fig. 2. After attaining BP control, patients received three-month refills of both hypertension and ART medications [15, 17].
The choice of medications used in the hypertension protocol was guided by the evidence on effectiveness from the CREOLE trial [18] and was further influenced by a subsidy from the medication local supplier.
Data collection
We collected clinical, demographic and anthropometric data at baseline including sex, age, weight, height, blood pressure, current and previous ART regimens, history of diabetes mellitus (DM), smoking history, latest viral loads, baseline CD4 cell counts at the start of ART and duration on ART from hard copy patient files as primary data sources. Prospectively, blood pressure was measured during monthly reviews and later three monthly for patients who achieved both blood pressure control and HIV viral suppression.
Statistical analyses
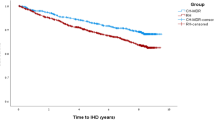
We described baseline characteristics using means and standard deviations for continuous variables including age and baseline CD4, and frequencies and percentages for categorical variables; sex, body mass index (BMI), duration on ART, smoking history, history of diabetes mellitus (DM) and latest viral loads. We compared baseline characteristics of patients who were started on one hypertension medicine and those that were started on two hypertension medicines using the Fisher’s exact test and the Pearson chi-square test at a 5% significance level. We calculated proportions of PLHIV with controlled blood pressure in each treatment arm at each month of follow up and estimated the closest time to BP control using the Kaplan Meier survival estimates considering the treatment protocol as one composite intervention.
We tested the proportional hazards assumption using scaled Schoenfeld residuals and it was met (p > 0.05). We therefore used Hazard ratios (HR) from the univariate and multivariable cox proportional hazards models to determine the predictors of time to first BP control at a 5% significance level. In our models, we included covariates known to influence blood pressure i.e., age, sex, BMI, smoking, immunological status (viral load suppression and CD4+ cell count) as well as ART regimens and duration on ART[19,20,21]
Results
Baseline characteristics
A total of 877 patients were enrolled in the study. Of these, 236 (30%) started treatment with Amlodipine 5 mg monotherapy and 641 (70%) started with Amlodipine 5 mg/Valsartan 80 mg duo-therapy. The mean age of study participants was 50.4 (SD = 9.5) and majority, 545 (62.1%) were female. There were no significant differences in sex and age between the two groups. Mean baseline systolic blood pressures for the monotherapy and duo-therapy groups were 145 (SD = 10.8) mmHg and 162 (SD = 17.7) mmHg respectively. Majority (69%) of the duo-therapy patients had baseline blood pressure between (160–179)/(100–109) with 22% and 8% having baseline blood pressure between (180–199)/(110–119) and (≥200)/(≥120) respectively. More than a third of the patients were overweight 339 (38.7%) followed by normal weight 283 (32.3%) and obese 224 (25.5%) with the minority being underweight 31 (3.5%). Of the enrolled patients, 396 (45.1%) had been on ART for <5 years, 395 (45.0%) between 5 and 10 years and 86 (9.8%) for more than 10 years. When evaluated for history of diagnosed diabetes mellitus, 177 (20.2%) reported having diabetes mellitus. There was no significant difference in frequency of smoking, ART combinations, most recent viral loads and baseline CD4 cell counts between the patients started on monotherapy versus duo-therapy (Table 1).
Blood pressure control at the different steps of the treatment protocol
Among the patients initiated on monotherapy (N = 236), 156 (66%) attained BP control within a month of treatment. Among the 80 patients with uncontrolled BP after the first month, 52 (22%) were controlled in the second month and 18 (8%) in the third month. Cumulatively, 66% of the patients were controlled in the first month, 88% by the second month and 96% by the third month. Only 7 (3%) patients failed to attain BP control after five months of follow up and 2(1%) did not complete follow up because they were transferred out to get care from another clinic (Table 2).
For the patients started on duo-therapy (N = 641), 362 (56%) attained BP control within the first month. Among the 279 patients who failed to attain BP control after the first month, 173(27%) attained BP control after the second month, 34 (5%) in the third month and 15 (2%) in the fourth month. Cumulatively 56% patients achieved blood pressure control in the first month, 83% by the second month, 88% by the third month and 90% by the fourth month. After four months of follow up, 40 (7%) patients had not yet attained BP control and 17 (3%) did not complete the follow up duration (2 patients lost to follow up, 4 patients died, 10 patients transferred out, 1 stopped medication due to persistent lower limb edema) (Table 2).
Overall, probability of blood pressure control per month of follow up among all enrolled patients considering the treatment protocol as one composite intervention
The probability of blood pressure control was 30%, 50%, 70%, 80% and 85% at one, two, three, four and five months of follow up respectively (Fig. 3).
Socio-demographic and clinical predictors to time to blood pressure control evaluating the tested treatment protocol as one composite intervention
We determined a high mean baseline systolic blood pressure (adjusted hazard ratio (aHR) 0.995, 95% Confidence Interval (95% CI): 0.989, 0.999, P value (p): 0.045), having a baseline ART regimen as tenofovir/ lamivudine/efavirenz (aHR: 0.764, 95% CI: 0.637, 0.917, p = 0.004) was associated with longer time to blood pressure control. Being on ART for more than 10 years was associated with a shorter time to blood pressure control (aHR: 1.456 95% CI; 1.126, 1.883) (Table 3).
Discussion
In resource limited settings where fixed dose combination antihypertensive drugs, trained human resource as well as availability of facilities for blood pressure monitoring are scarce, adherence to universally agreed upon guidelines in the treatment of hypertension is challenging [9, 22, 23]. Because of the increasing burden of non-communicable diseases (NCDs) worldwide, the WHO developed a HEARTS technical package aimed at providing country ministries of Health with a strategic approach in improving cardiovascular disease (CVD) management in primary care settings [14]. We adopted this model and tailored it to our study clinic setting in Uganda evaluating its effectiveness by determining time to blood pressure control in patients started on monotherapy and those on duo-therapy [15].
More than half of the patients in each treatment group attained blood pressure control four weeks after starting treatment, with approximately 90% achieving BP control by the third month, irrespective of the anti-hypertensive regimen they received. Time to blood pressure control has been evaluated in different world settings comparing the efficacy of monotherapy versus duo-therapy anti-hypertensive treatment. In a large retrospective database cohort in the USA, up to about 55% of patients on monotherapy and 60% of those on fixed dose combination drugs were controlled by 400 days [24]. In another Malaysian cohort largely on monotherapy, BP control was achieved in 47% and 65% at 6 and 12 months respectively [25]. Our protocol was implemented in a real world setting with integrated adherence support for both ART and hypertension treatment. This ongoing routine adherence counseling could have influenced the high rates of BP control observed in our study as compared to the rates in the above cohorts.
Hypertension is one of the most attributable traditional risk factors responsible for atherosclerotic CVD in person living with HIV [26]. Our study population exhibited a high prevalence of CVD risk factors underlining the need for more effective blood pressure control. A large percentage of the patients were overweight and obese with a mean age of 50 years. Additionally, majority had been exposed to ART for more than five years. Long term exposure to ART including nucleoside reverse transcriptase inhibitors (NRTIs) and protease inhibitors (PIs) has also been linked to heightened CVD risk [27, 28].
Multiple studies have evaluated the contribution of conventional risk factors to hypertension in PLHIV and determined that most factors cut across both HIV infected and uninfected populations. Additionally, multiple studies have found an increased risk of hypertension with longevity on anti-retroviral therapy [29,30,31,32]. However, the association of these factors to BP control is largely understudied in PLHIV [19, 33, 34]. In our study, we determined that patients who had been on ART for ≥10 years tended to have a shorter time to blood pressure control. This could be attributed to transferred adherence to anti-hypertensive therapy following years of ART adherence counseling.
We had some limitations in execution of this study. This was an intervention in a single HIV clinic site and hence the results may not be generalizable to the general HIV positive population. This is because hypertension in different regions of sub-Saharan Africa may be driven by different factors such as diet, physical activity as well as environment. Additionally, during the time of intervention, availability of hypertension drugs as well as emphasis on patient education on lifestyle modification was ensured as part of the WHO HEARTS model that was being tested which may lead to overestimation of the success of the rates of BP control as compared to other public health care settings in Africa with frequent drug stockouts as well as limited personnel. Despite the limitations, we demonstrated that this simplified protocol was effective in attaining timely BP control and minimizing pill burden in a pragmatic resource limited setting.
Conclusions
In this study, an adapted WHO HEART treatment protocol attained timely BP control among hypertensive PLHIV. Additionally, we demonstrated that on initiation of Amlodipine 5mg-monotherapy in PLHIV with stage I hypertension and Amlodipine 5 mg/Valsartan 40 mg duo-therapy in patients with ≥ stage 2 hypertension, there was reasonably high rates of blood pressure control in the first month. The use of monotherapy anti-hypertensive treatment can be a viable undertaking in similar clinical settings to limit treatment cost and pill burden. Larger multi-center studies should be conducted to increase generalizability of the results.
Summary
What is known about the topic
-
Persons living with HIV have a high prevalence of hypertension.
-
Controlled hypertension reduces cardiovascular disease mortality and morbidity.
-
Integrated management of HIV and hypertension improves hypertension control and sustains HIV control among hypertensive persons living with HIV.
What this study adds
-
The WHO HEARTS strategy was effective at achieving timely BP control among Persons living with HIV.
-
The monotherapy anti-hypertensive treatment for stage I hypertension is a viable option to achieve BP control and limit pill burden in resource limited HIV care settings.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Global HIV & AIDS statistics — 2020 fact sheet | UNAIDS [Internet]. https://www.unaids.org/en/resources/fact-sheet Accessed 21 May 2021.
Fisher KA, Patel SV, Mehta N, Stewart A, Medley A, Dokubo EK, et al. Lessons learned from programmatic gains in HIV service delivery during the COVID-19 Pandemic — 41 PEPFAR-Supported Countries, 2020. Morb Mortal Wkly Rep. 2022;71:447–52.
Global HIV Programme. Available from: https://www.who.int/teams/global-hiv-hepatitis-and-stis-programmes/hiv/treatment. Accessed 10 Oct 2022.
Jespersen NA, Axelsen F, Dollerup J, Nørgaard M, Larsen CS. The burden of non-communicable diseases and mortality in people living with HIV (PLHIV) in the pre-, early- and late-HAART era. HIV Med. 2021;22:478–90.
Haacker M, Bärnighausen T, Atun R. HIV and the growing health burden from noncommunicable diseases in Botswana: modelling study. J Glob Health. 2019;9:010428.
Yang Z, Zhu Z, Lizarondo L, Xing W, Han S, Hu H, et al. Experience of chronic noncommunicable disease in people living with HIV: a systematic review and meta-aggregation of qualitative studies. BMC Public Health. 2021;21:1–19.
A program of Resolve to Save Lives INTEGRATING HYPERTENSION AND HIV MANAGEMENT A practical Differentiated Service Delivery toolkit INTEGRATING HYPERTENSION AND HIV MANAGEMENT 2. [Online]. Available: https://www.resolvetosavelives.org.
Unaids, Responding to the Challenge of Non-communicable Diseases, https://doi.org/10.1097/QAD.0000000000001888.
Vorkoper S, Kupfer LE, Anand N, Patel P, Beecroft B, Tierney WM, et al. Building on the HIV chronic care platform to address noncommunicable diseases in sub-Saharan Africa: a research agenda. AIDS. 2018;32:S107–13.
McCombe G, Lim J, Van Hout MC, Lazarus JV, Bachmann M, Jaffar S, et al. Integrating care for diabetes and hypertension with HIV care in sub-saharan africa: a scoping review. Int J Integr Care. 2022;22:6.
Kintu A, Sando D, Okello S, Mutungi G, Guwatudde D, Menzies NA, et al. Integrating care for non-communicable diseases into routine HIV services: key considerations for policy design in sub-Saharan Africa. J Int AIDS Soc. 2020;23:e25508.
https://www.escardio.org/Education/ESC-Education-by-Topic/Hypertension Hypertension.
The JNC 8 Hypertension Guidelines: An In-Depth Guide [Internet]. https://www.ajmc.com/view/the-jnc-8-hypertension-guidelines-an-in-depth-guide Accessed 10 Oct 2022.
HEARTS: technical package for cardiovascular disease management in primary health care: Risk-based CVD management [Internet]. https://www.who.int/publications/i/item/9789240001367 Accessed 30 Nov 2022.
Muddu M, Semitala FC, Kimera I, Mbuliro M, Ssennyonjo R, Kigozi SP, et al. Improved hypertension control at six months using an adapted WHO HEARTS-based implementation strategy at a large urban HIV clinic in Uganda. BMC Health Serv Res. 2022;22:1–14.
Muntner P, Shimbo D, Carey RM, Charleston JB, Gaillard T, Misra S, et al. Measurement of blood pressure in humans: a scientific statement from the american heart association. Hypertension. 2019;73:E35–66.
Kimera ID, Namugenyi C, Schwartz JI, Musimbaggo DJ, Ssenyonjo R, Atukunda P, et al. Integrated multi-month dispensing of antihypertensive and antiretroviral therapy to sustain hypertension and HIV control. J Hum Hypertens. 2023;37:213–9.
Ojji DB, Mayosi B, Francis V, Badri M, Cornelius V, Smythe W, et al. Comparison of dual therapies for lowering blood pressure in black Africans. N. Engl J Med. 2019;380:2429–39.
Fahme SA, Bloomfield GS, Peck R. Hypertension in HIV-infected adults. Hypertension. 2018;72:44–55.
Xu Y, Chen X, Wang K. Global prevalence of hypertension among people living with HIV: a systematic review and meta-analysis. J Am Soc Hypertens. 2017;11:530–40.
Ryscavage P, Still W, Nyemba V, Stafford K. Prevalence of systemic hypertension among HIV-infected and HIV-uninfected young adults. Open Forum Infect Dis. 2017;4:S59–S59.
Adeyemi O, Lyons M, Njim T, Okebe J, Birungi J, Nana K, et al. Integration of non-communicable disease and HIV/AIDS management: a review of healthcare policies and plans in East Africa. BMJ Glob Health. 2021;6:e004669.
Wald DS, Law M, Morris JK, Bestwick JP, Wald NJ. Combination therapy versus monotherapy in reducing blood pressure: meta-analysis on 11,000 participants from 42 trials. Am J Med. 2009;122:290–300.
Egan BM, Bandyopadhyay D, Shaftman SR, Wagner CS, Zhao Y, Yu-Isenberg KS. Initial monotherapy and combination therapy and hypertension control the first year. Hypertension. 2012;59:1124–31.
Cheong AT, Mohd Said S, Muksan N. Time to achieve first blood pressure control after diagnosis among hypertensive patients at primary health care clinics: a preliminary study. Asia Pac J Public Health. 2015;27:NP485–94.
Shah ASV, Stelzle D, Ken Lee K, Beck EJ, Alam S, et al. Global burden of atherosclerotic cardiovascular disease in people living with HIV: systematic review and meta-analysis. Circulation. 2018;138:1100–12.
Jarwani B. Cardiovascular disease and antiretroviral therapy. J Glob Infect Dis. 2019;11:91.
Bavinger C, Bendavid E, Niehaus K, Olshen RA, Olkin I, Sundaram V, et al. Risk of cardiovascular disease from antiretroviral therapy for hiv: a systematic review. PLoS One. 2013;8:e59551.
Thiébaut R, El-Sadr WM, Friis-Møller N, Rickenbach M, Reiss P, Monforte AD, et al. Predictors of hypertension and changes of blood pressure in HIV-infected patients. Antivir Ther. 2005;10:811–23.
Jackson IL, Lawrence SM, Igwe CN, Ukwe CV, Okonta MJ. Prevalence and control of hypertension among people living with HIV receiving care at a Nigerian hospital. PAMJ. 2022; 41:153.
Kwarisiima D, Atukunda M, Owaraganise A, Chamie G, Clark T, Kabami J, et al. Hypertension control in integrated HIV and chronic disease clinics in Uganda in the SEARCH study. BMC Public Health. 2019;19:1–10.
Debiso AT, Debiso AT. Incidence and predictors of systemic hypertension among cohort of HIV/AIDS infected patients in health facilities of South Ethiopia. Adv Infect Dis. 2020;10:47–63.
Nduka CU, Stranges S, Sarki AM, Kimani PK, Uthman OA. Evidence of increased blood pressure and hypertension risk among people living with HIV on antiretroviral therapy: a systematic review with meta-analysis. J Hum Hypertens. 2016;30:355–62.
Nkeh-Chungag BN, Goswami N, Engwa GA, Sewani-Rusike CR, Mbombela V, Webster I, et al. Relationship between endothelial function, antiretroviral treatment and cardiovascular risk factors in hiv patients of african descent in South Africa: a cross-sectional study. J Clin Med. 2021;10:1–14.
Acknowledgements
The authors acknowledge the support of Makerere University Joint AIDS program, RTSL and the Mulago ISS clinic towards the study implementation.
Funding
This study was funded by resolve to Save Lives (RTSL) under the Learning, Implementation, Networking, Knowledge sharing and Support (LINKS) community grants for improving cardiovascular health. However, the funder was not involved in the design of the study, data collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
WA, FCS, IDK, FM and MM conceptualized the study, WA, IDK and MM wrote the protocol, IDK, CN, RS, MM performed data extraction, data analysis and interpretation. WA, FM, IDK and MM wrote the manuscript and RK, FM, GM, IS, JIS and ARK provided critical revisions of the manuscript. All authors reviewed and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by The AIDS Support Organization (TASO) research ethics committee [Number: 040/19/Ug-REC-009], and the Uganda National Council of Science and Technology [HS 2644]. All study participants provided informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Amutuhaire, W., Semitala, F.C., Kimera, I.D. et al. Time to blood pressure control and predictors among patients receiving integrated treatment for hypertension and HIV based on an adapted WHO HEARTS implementation strategy at a large urban HIV clinic in Uganda. J Hum Hypertens (2024). https://doi.org/10.1038/s41371-024-00897-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41371-024-00897-3