Abstract
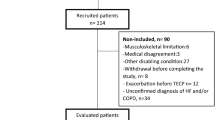
Our aim was to conduct a sex-disaggregated analysis of pulmonary and systemic vascular function in healthy individuals both at rest and during submaximal exercise. Healthy individuals underwent right-heart catheterization at rest and during submaximal cycling. Hemodynamic data were collected in a control state and with moderate exercise. Pulmonary and systemic vascular variables including: compliance, resistance, and elastance were calculated, indexed to body surface area (BSA), adjusted for age and compared between male and female sex. Thirty-six individuals (18M/18F; 54 ± 7 vs. 58 ± 6 years, p = 0.04) were included. When adjusted for age and indexed to BSA, total pulmonary resistance (TPulmR) (516 ± 73 vs. 424 ± 118 WU m−2, p = 0.03) and pulmonary arterial elastance (PEa) (0.41 ± 0.1 vs. 0.32 ± 0.1 mmHg ml−1 m2, p = 0.03) were higher in females vs. males. Both pulmonary (Cpa) and systemic compliance (Csa) were lower in females vs. males however lost significance with adjustment for age. Systemic arterial elastance (SEa) was higher in females (1.65 ± 0.29 vs. 1.31 ± 0.24 mmHg ml−1, p = 0.05). Secondary analyses demonstrated significant correlations between age and PVR (r = 0.33, p = 0.05), TPulmR (r = 0.35, p = 0.04), Cpa (r = −0.48, p < 0.01), and PEa (r = 0.37, p = 0.03). During exercise, there were greater increases in TPulmR (p = 0.02) and PEa (p = 0.01) in females vs. males. In conclusion, TPulmR and PEa are significantly higher at rest and exercise in females vs. males. Cpa and Csa were lower in females, however this may have been confounded by age. Our results are consistent with the notion that indices of pulmonary and systemic vascular load are higher, related to both older age and female sex, independent of heart failure.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Ogawa T, Spina RJ, Martin WH 3rd, Kohrt WM, Schechtman KB, Holloszy JO, et al. Effects of aging, sex, and physical training on cardiovascular responses to exercise. Circulation. 1992;86:494–503.
Weiss EP, Spina RJ, Holloszy JO, Ehsani AA. Gender differences in the decline in aerobic capacity and its physiological determinants during the later decades of life. J Appl Physiol. 2006;101:938–44.
Ho JE, Lyass A, Lee DS, Vasan RS, Kannel WB, Larson MG, et al. Predictors of new-onset heart failure: differences in preserved versus reduced ejection fraction. Circ Heart Fail. 2013;6:279–86.
Redfield MM, Jacobsen SJ, Borlaug BA, Rodeheffer RJ, Kass DA. Age- and gender-related ventricular-vascular stiffening: a community-based study. Circulation. 2005;112:2254–62.
Lau ES, Panah LG, Zern EK, Liu EE, Farrell R, Schoenike MW, et al. Arterial stiffness and vascular load in HFpEF: differences among women and men. J Card Fail. 2022;2:202–11.
Coutinho T, Borlaug BA, Pellikka PA, Turner ST, Kullo IJ. Sex differences in arterial stiffness and ventricular-arterial interactions. J Am Coll Cardiol. 2013;61:96–103.
Scantlebury DC, Borlaug BA. Why are women more likely than men to develop heart failure with preserved ejection fraction? Curr Opin Cardiol. 2011;26:562–8.
Lam CS, Roger VL, Rodeheffer RJ, Borlaug BA, Enders FT, Redfield MM. Pulmonary hypertension in heart failure with preserved ejection fraction: a community-based study. J Am Coll Cardiol. 2009;53:1119–26.
Borlaug BA, Redfield MM. Diastolic and systolic heart failure are distinct phenotypes within the heart failure spectrum. Circulation. 2011;123:2006–13.
Esfandiari S, Wright SP, Goodman JM, Sasson Z, Mak S. Pulmonary artery wedge pressure relative to exercise work rate in older men and women. Med Sci Sports Exerc. 2017;49:1297–304.
Wright SP, Esfandiari S, Gray T, Fuchs FC, Chelvanathan A, Chan W, et al. The pulmonary artery wedge pressure response to sustained exercise is time-variant in healthy adults. Heart. 2016;102:438–43.
Wright SP, Granton JT, Esfandiari S, Goodman JM, Mak S. The relationship of pulmonary vascular resistance and compliance to pulmonary artery wedge pressure during submaximal exercise in healthy older adults. J Physiol. 2016;594:3307–15.
Tampakakis E, Shah SJ, Borlaug BA, Leary PJ, Patel HH, Miller WL, et al. Pulmonary effective arterial elastance as a measure of right ventricular afterload and its prognostic value in pulmonary hypertension due to left heart disease. Circ Heart Fail. 2018;11:e004436.
Chemla D, Hebert JL, Coirault C, Salmeron S, Zamani K, Lecarpentier Y. Matching dicrotic notch and mean pulmonary artery pressures: implications for effective arterial elastance. Am J Physiol. 1996;271:H1287–95.
Wyka K, Mathews P, Clark W. Foundations of respiratory care. Albany: Thomas Learning; 2002.
Wright SP, Sless RT, Mak S. Does increased arterial stiffness cause heart failure with preserved ejection fraction in women? J Card Fail. 2022;28:212–4.
Tedford RJ, Hassoun PM, Mathai SC, Girgis RE, Russell SD, Thiemann DR, et al. Pulmonary capillary wedge pressure augments right ventricular pulsatile loading. Circulation. 2012;125:289–97.
Lam CS, Borlaug BA, Kane GC, Enders FT, Rodeheffer RJ, Redfield MM. Age-associated increases in pulmonary artery systolic pressure in the general population. Circulation. 2009;119:2663–70.
Beale AL, Nanayakkara S, Segan L, Mariani JA, Maeder MT, van Empel V, et al. Sex differences in heart failure with preserved ejection fraction pathophysiology: a detailed invasive hemodynamic and echocardiographic analysis. JACC Heart Fail. 2019;7:239–49.
Muthurangu V, Atkinson D, Sermesant M, Miquel ME, Hegde S, Johnson R, et al. Measurement of total pulmonary arterial compliance using invasive pressure monitoring and MR flow quantification during MR-guided cardiac catheterization. Am J Physiol Heart Circ Physiol. 2005;289:H1301–6.
Segers P, Brimioulle S, Stergiopulos N, Westerhof N, Naeije R, Maggiorini M, et al. Pulmonary arterial compliance in dogs and pigs: the three-element windkessel model revisited. Am J Physiol. 1999;277:H725–31.
Hadinnapola C, Li Q, Su L, Pepke-Zaba J, Toshner M. The resistance-compliance product of the pulmonary circulation varies in health and pulmonary vascular disease. Physiol Rep. 2015;3:1–9.
Brimioulle S, Wauthy P, Ewalenko P, Rondelet B, Vermeulen F, Kerbaul F, et al. Single-beat estimation of right ventricular end-systolic pressure-volume relationship. Am J Physiol Heart Circ Physiol. 2003;284:H1625–30.
Author information
Authors and Affiliations
Contributions
RTS, SPW and SM contributed to the acquisition, analysis, or interpretation of data for the work. RTS drafted the manuscript. SPW, RFB, FHV and SM critically revised the manuscript. All gave final approval and agree to be accountable for all aspects of work ensuring integrity and accuracy.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sless, R.T., Wright, S.P., Bentley, R.F. et al. Sex differences in pulmonary and systemic vascular function at rest and during exercise in healthy middle-aged adults. J Hum Hypertens 37, 746–752 (2023). https://doi.org/10.1038/s41371-023-00822-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-023-00822-0
This article is cited by
-
Journal of Human Hypertension special issue on sex and gender differences in hypertension
Journal of Human Hypertension (2023)